Idiopathic Megacolon—Short Review
Abstract
:1. Introduction
2. Clinical Manifestations
3. Etiopathogenic Theories
3.1. Cajal Cells
3.2. Smooth Muscle Cells
3.3. Intramural Tendon Fiber Network
3.4. Pelvic-Perineal Muscle Disorders
3.5. Genetic Appearance
4. Diagnostic Criteria for the Acquired Megacolon
5. Complications
6. Therapeutic Management
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| IM | Idiopathic megacolon |
| HP | Histopathology |
| IHC | Immunohistochemistry |
| CT | Computerized tomography |
| MEN 2B | Multiple Endocrine Neoplasia, Type 2B |
| MSOF | Multiple systems organ failure |
References
- Yinghua, L.; Zhibao, L.; Weijue, X.; Jiangbin, L.; Xiong, H. An unusual cause of idiopathic megacolon in a juvenile. Medicine 2019, 98, e16487. [Google Scholar]
- Gladman, M.A.; Knowles, C.H. Novel concepts in the diagnosis, pathophysiology and management of idiopathic megabowel. Color. Dis. 2008, 10, 531–538. [Google Scholar] [CrossRef]
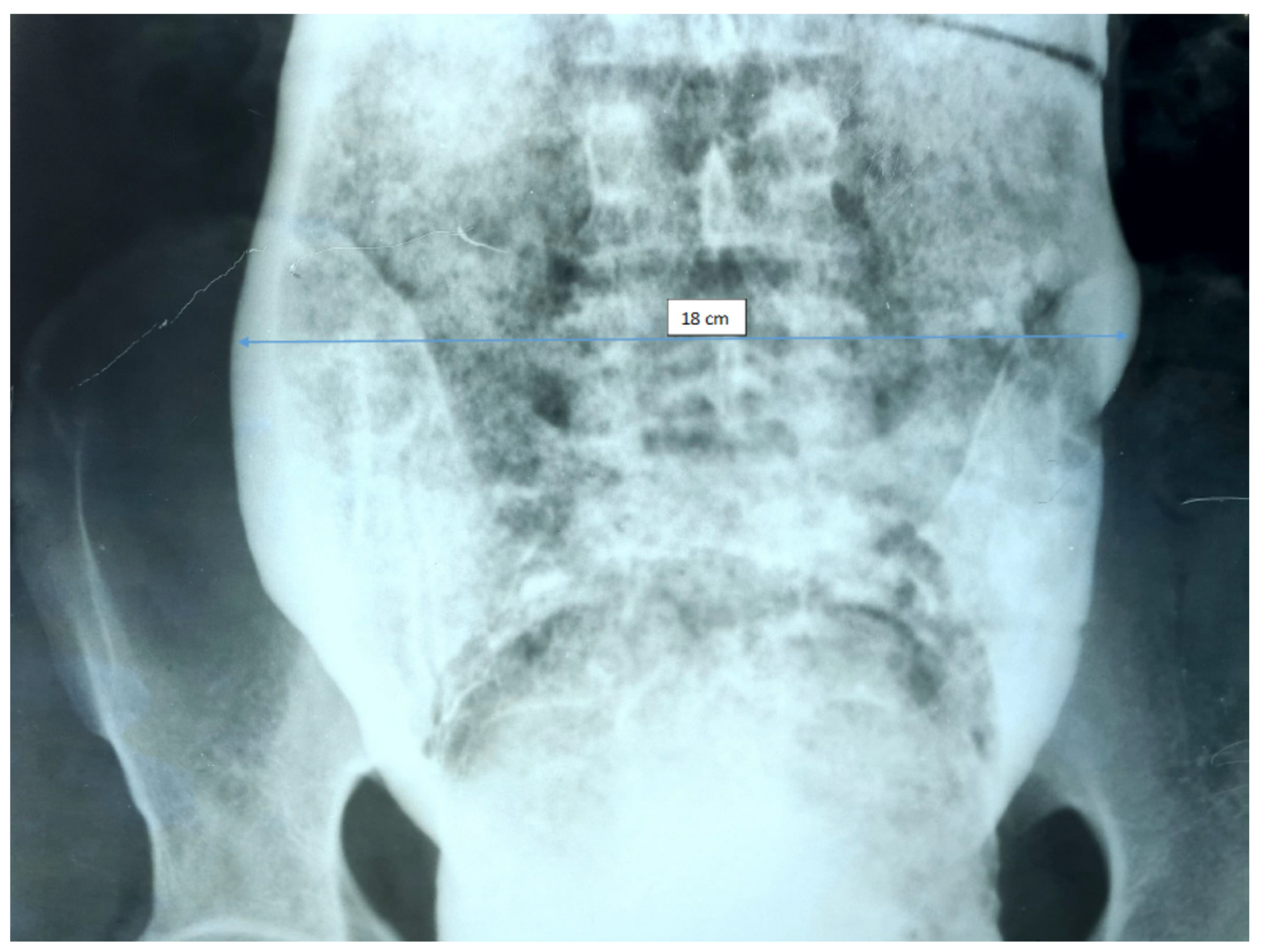
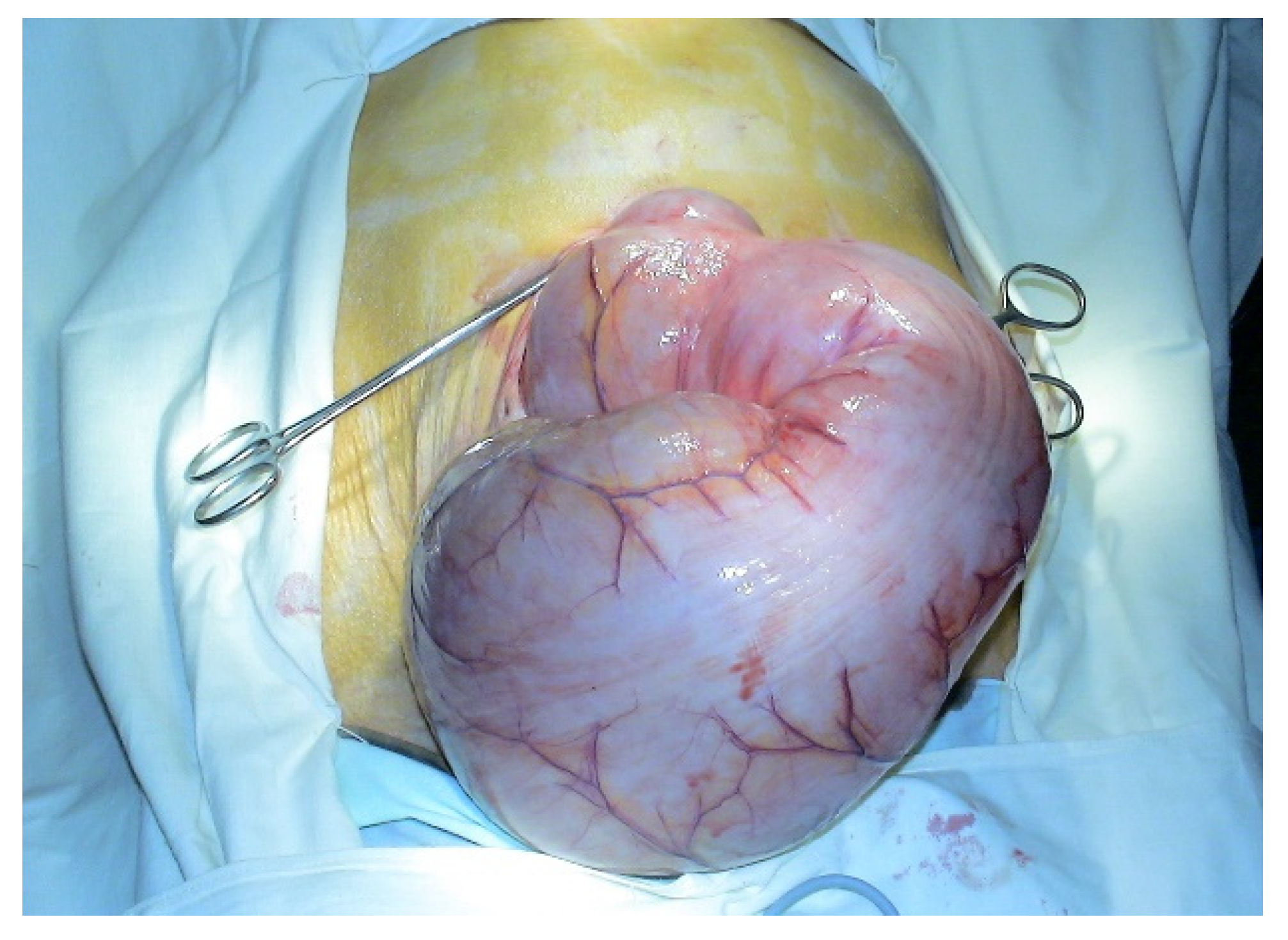
- Fransvea, P.; Cortese, F. A case of idiopathic giant megacolon in an obese patientitle of image. Pan Afr. Med. J. 2018, 31, 206. [Google Scholar] [CrossRef] [PubMed]
- Larentzakis, A.; Kalyva, A.; Kantas, T.; Michalopoulos, N.V.; Zografos, C.G.; Zografos, G.C. Mega-megacolon: A case report. Int. J. Color. Dis. 2020, 35, 1615–1617. [Google Scholar] [CrossRef]
- Wang, X.J.; Camilleri, M. Chronic Megacolon Presenting in Adolescents or Adults: Clinical Manifestations, Diagnosis, and Genetic Associations. Dig. Dis. Sci. 2019, 64, 2750–2756. [Google Scholar] [CrossRef]
- Halder, S.L.; Locke, G.R., 3rd; Schleck, C.D.; Zinsmeister, A.R.; Melton, L.J., 3rd; Talley, N.J. Natural history of functional gastrointestinal disorders: A 12-year longitudinal population-based study. Gastroenterology 2007, 133, 799–807. [Google Scholar] [CrossRef]
- Wang, L.; Zheng, H.; Tian, Y.; Mou, J.; Zhang, L.; Liu, B.; Tong, W. Laparoscopic-assisted colectomy with Duhamel procedure for idiopathic megacolon in adults: A retrospective study. ANZ J. Surg. 2020, 90, 2285–2289. [Google Scholar] [CrossRef]
- Meier-Ruge, W.A.; Müller-Lobeck, H.; Stoss, F.; Bruder, E. The pathogenesis of idiopathic megacolon. Eur. J. Gastroenterol. Hepatol. 2006, 18, 1209–1215. [Google Scholar] [CrossRef]
- Anyaegbuna, C.; Apostolopoulos, A.; Patel, H. Bowel perforation in chronic idiopathic megarectum and megacolon. BMJ Case Rep. 2018, 2018, bcr-2018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gattuso, J.M.; Kamm, M.A. Clinical features of idiopathic megarectum and idiopathic megacolon. Gut 1997, 41, 93–99. [Google Scholar] [CrossRef] [Green Version]
- Krishnamurthy, S.; Schuffler, M.D. Pathology of neuromuscular disorders of the small intestine and colon. Gastroenterology 1987, 93, 610–639. [Google Scholar] [CrossRef]
- Wedel, T.; Spiegler, J.; Soellner, S.; Roblick, U.J.; Schiedeck, T.H.; Bruch, H.P.; Krammer, H.J. Enteric nerves and intestinal cells of Cajal are altered in patients with slow-transit constipation and megacolon. Gastroenterology 2002, 123, 1459–1467. [Google Scholar] [CrossRef] [PubMed]
- Gattuso, J.M.; Hoyle, C.H.V.; Milner, P.; Kamm, M.A.; Burnstock, G. Enteric innervation in idiopathic megarectum and megacolon. Int. J. Color. Dis. 1996, 11, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Min, B.-H.; Son, H.J.; Kim, J.J.; Rhee, J.C.; Lee, S.J.; Rhee, P.-L. Idiopathic proximal hemimegacolon: Radiologic findings and analyses of clinical and physiological characteristics. Abdom. Imaging 2010, 35, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Szymanska, S.; Markiewicz-Kijewska, M.; Pyzlak, M.; Wieckowska-Karkucinska, A.; Kalicinski, P.; Pronicki, M. Familiar Occurrence of Desmosis of the Colon—Report of Two Cases and Literature Review. J. Gen. Pract. 2017, 5, 301. [Google Scholar] [CrossRef]
- Meier-Ruge, W.A.; Holschneider, A.M.; Schärli, A.F. New pathogenetic aspects of gut dysmotility in aplastic and hypoplastic desmosis of early childhood. Pediatr. Surg. Int. 2001, 17, 140–143. [Google Scholar] [CrossRef]
- Siri, S.; Zhao, Y.; Maier, F.; Pierce, D.M.; Feng, B. The Macro- and Micro-Mechanics of the Colon and Rectum I: Experimental Evidence. Bioeng. 2020, 7, 130. [Google Scholar] [CrossRef]
- Gattuso, J.M.; Kamm, M.A.; Talbot, J.C. Pathology of idiopathic megarectumand megacolon. Gut 1997, 41, 252–257. [Google Scholar] [CrossRef]
- Cribb, B.; Ranjan, R.; Henderson, N. A case of perforated chronic idiopathic megacolon. N. Z. Med. J. 2015, 128, 70–72. [Google Scholar]
- Kirgizov, I.V.; Minaev, S.V.; Shishkin, I.; Aprosimova, S.; Ukhina, L. Surgical treatment of idiopathic megarectum in constipated children. J. Pediatr. Surg. 2019, 54, 1379–1383. [Google Scholar] [CrossRef]
- Veress, B.; Ohlsson, B. Spatial relationship between telocytes, interstitial cells of Cajal and the enteric nervous system in the human ileum and colon. J. Cell. Mol. Med. 2020, 24, 3399–3406. [Google Scholar] [CrossRef] [Green Version]
- Núñez Ortiz, A.; Trigo Salado, C.; de la Cruz Ramírez, M.D.; Márquez Galán, J.L.; Herrera Justiniano, J.M.; Leo Carnerero, E. Megacolon in inflammatory bowel disease: Response to infliximab. Rev. Esp. Enferm. Dig. 2020, 112, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Yamagishi, A.; Koyama, N.; Yamashita, N.; Suzuki, M.; Yamada, T.; Kawashima, M.; Yoshida, H. Segmental Hypoganglionosis of the Colon: A Case Report. J. Nippon. Med. Sch. 2021, 88, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Rolle, U.; Piotrowska, A.P.; Nemeth, L.; Puri, P. Altered distribution of interstitialcells of Cajal in Hirschsprung disease. Arch. Pathol. Lab. Med. 2002, 126, 928–933. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.E.; English, W.; Kendall, J.V.; Sheshappanavar, V.; Peroos, S.; West, M.; Cleeve, S.; Knowles, C. Megarectum: Systematic histopathological evaluation of 35 patients and new common pathways in chronic rectal dilatation. J. Clin. Pathol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Washabau, R.J.; Stalis, I.H. Alterations in colonic smooth muscle functionin cats with idiopathic megacolon. Am. J. Vet. Res. 1996, 57, 580–587. [Google Scholar] [PubMed]
- Washabau, R.J.; Holt, D. Pathogenesis, diagnosis, and therapy of felineidiopathic megacolon. Vet. Clin. N. Am. Small Anim. Pract. 1999, 29, 589–603. [Google Scholar]
- Li, M.; Behrenbruch, C.; Wong, A.; An, V. Megacolon following ileostomy reversal due to Clostridium difficile. ANZ J. Surg. 2020, 90, 1769–1770. [Google Scholar] [CrossRef]
- Keller, J.; on behalf of the International Working Group for Disorders of Gastrointestinal Motility and Function; Bassotti, G.; Clarke, J.; Dinning, P.; Fox, M.; Grover, M.; Hellström, P.M.; Ke, M.; Layer, P.; et al. Advances in the diagnosis and classification of gastric and intestinal motility disorders. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 291–308. [Google Scholar] [CrossRef] [Green Version]
- Montedonico, S.; Cáceres, P.; Muñoz, N.; Yáñez, H.; Ramírez, R.; Fadda, B. Histochemical staining for intestinal dysganglionosis: Over 30 years experience with more than 1,500 biopsies. Pediatr. Surg. Int. 2011, 27, 479–486. [Google Scholar] [CrossRef]
- Rollo, B.N.; Zhang, D.; Stamp, L.; Menheniott, T.R.; Stathopoulos, L.; Denham, M.; Dottori, M.; King, S.K.; Hutson, J.M.; Newgreen, D.F. Enteric Neural Cells From Hirschsprung Disease Patients Form Ganglia in Autologous Aneuronal Colon. Cell. Mol. Gastroenterol. Hepatol. 2016, 2, 92–109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gerstenfeld, L.C.; Crawford, D.R.; Boedtker, H.; Doty, P. Expression of type I andIII collagen genes during differentiation of embryonic myoblasts in culture. Mol. Cell. Biol. 1984, 4, 1483–1492. [Google Scholar]
- Lawrance, I.C.; Rogler, G.; Bamias, G.; Breynaert, C.; Florholmen, J.; Pellino, G.; Reif, S.; Speca, S.; Latella, G. Cellular and Molecular Mediators of Intestinal Fibrosis. J. Crohn’s Colitis 2015, 11, 1491–1503. [Google Scholar] [CrossRef] [Green Version]
- Graham, M.F.; Drucker, D.E.R.; Perr, H.A.; Diegelmann, R.F.; Ehrlich, H.P. Heparinmodulates human intestinal smooth muscle cell proliferation, and latticecontraction. Gastroenterology 1987, 93, 801–809. [Google Scholar] [CrossRef]
- Han, J.; Tonkin, D.; Hewett, P. Rare case of wandering spleen causing intra-thoracic megacolon. ANZ J. Surg. 2020, 90, 1192–1193. [Google Scholar] [CrossRef]
- Perr, H.A.; Grider, J.R.; Mills, S.; Konstein, M.; Turner, D.A.; Diegelmann, R.F.; Graham, M. Collagen production by human smooth muscle cells isolatedduring intestinal organogenesis. Anat. Embryol. 1992, 185, 517–527. [Google Scholar] [CrossRef]
- Wallace, A.S.; Burns, A.J. Development of the enteric nervous system, smooth muscle and interstitial cells of Cajal in the human gastrointestinal tract. Cell Tissue Res. 2005, 319, 367–382. [Google Scholar] [CrossRef] [PubMed]
- O’Dwyer, R.H.; Acosta, A.; Camilleri, M.; Burton, D.; Busciglio, I.; Bharucha, A.E. Clinical Features and Colonic Motor Disturbances in Chronic Megacolon in Adults. Dig. Dis. Sci. 2015, 60, 2398–2407. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M.; Wieben, E.; Eckert, D.; Carlson, P.; Hurley O’Dwyer, R.; Gibbons, D.; Acosta, A.; Klee, E.W. Familial chronic megacolon presenting in childhood or adulthood: Seeking the presumed gene association. Neurogastroenterol. Motil. 2019, 31, e13550. [Google Scholar] [CrossRef]
- Brandler, J.B.; Sweetser, S.; Khoshbin, K.; Babameto, M.; Prokop, L.J.; Camilleri, M. Colonic Manifestations and Complications Are Relatively Under-Reported in Systemic Sclerosis: A Systematic Review. Am. J. Gastroenterol. 2019, 114, 1847–1856. [Google Scholar] [CrossRef] [PubMed]
- Downes, T.J.; Cheruvu, M.S.; Karunaratne, T.B.; de Giorgio, R.; Farmer, A.D. Pathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-Obstruction. J. Clin. Gastroenterol. 2018, 52, 477–489. [Google Scholar] [CrossRef]
- Law, N.; Bharucha, A.; Zinsmeister, A. Rectal and colonic distention elicit viscerovisceral reflexes in humans. Am. J. Physiol. Gastrointest. Liver Physiol. 2002, 283, 384–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mollen, R.M.H.G.; Salvioli, B.; Camilleri, M.; Burton, D.; Kost, L.J.; Phillips, S.F.; Pemberton, J.H. The effects of biofeedback on rectal sensation and distal colonic motility in patients with disorders of rectal evacuation: Evidence of an inhibitory rectocolonic reflex in humans? Am. J. Gastroenterol. 1999, 94, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Sohn, G.; Yu, C.S.; Kim, C.W.; Kwak, J.Y.; Jang, T.Y.; Kim, K.H.; Yang, S.S.; Yoon, Y.S.; Lim, S.-B.; Kim, J.C. Surgical Outcomes after Total Colectomy with Ileorectal Anastomosis in Patients with Medically Intractable Slow Transit Constipation. J. Korean Soc. Coloproctology 2011, 27, 180–187. [Google Scholar] [CrossRef] [Green Version]
- Hassan, I.; Pemberton, J.H.; Young-Fadok, T.M.; You, Y.N.; Drelichman, E.R.; Rath-Harvey, D.; Schleck, C.D.; Larson, D.R. Ileorectal Anastomosis for Slow Transit Constipation: Long-Term Functional and Quality of Life Results. J. Gastrointest. Surg. 2006, 10, 1330–1337. [Google Scholar] [CrossRef] [PubMed]
- Arebi, N.; Kalli, T.; Howson, W.; Clark, S.; Norton, C. Systematic review of abdominal surgery for chronic idiopathic constipation. Colorectal Dis. 2011, 13, 1335–1343. [Google Scholar] [CrossRef]
- Kapur, R.P.; Gershon, M.D.; Milla, P.J.; Pachnis, V. The influence of Hox genes and three intercellular signalling pathways on enteric neuromuscular development. Neurogastroenterol. Motil. 2004, 16, 8–13. [Google Scholar] [CrossRef]
- Duluc, I.; Lorentz, O.; Fritsch, C.; Leberquier, C.; Kedinger, M.; Freund, J.-N. Changing intestinal connective tissue interactions alters homeobox gene expression in epithelial cells. J. Cell Sci. 1997, 110, 1317–1324. [Google Scholar] [CrossRef]
- Fehlow, P.; Walther, F.; Miosge, W. An increased incidence of megacolon in psychiatric and neurologic patients. Nervenarzt 1995, 66, 57–59. [Google Scholar]
- Harouna, A.D.; Salahoudine, I.; Mahamoudi, A.; Madi, A.E.; Khattala, K.; Bouabdallah, Y. Neonatal caecal perforation revealing congenital megacolon. Pan Afr. Med. J. 2018, 31, 216. [Google Scholar]
- Camilleri, M. Dysmotility of the small intestinte and colon. In Textbook of Gastroenterology; Yamada, T., Ed.; Wiley-Blackwell: Chichester, UK; Hoboken, NJ, USA, 2009; pp. 1513–1520. [Google Scholar]
- Vijayvargiya, P.; Camilleri, M. Proximal Megacolon in an Adult. Clin. Gastroenterol. Hepatol. 2014, 12, e83–e84. [Google Scholar] [CrossRef]
- Basilisco, G.; Bharucha, A.E. High-resolution anorectal manometry: An expensive hobby or worth every penny? Neurogastroenterol. Motil. 2017, 29, e13125. [Google Scholar] [CrossRef] [PubMed]
- Yoshimaru, K.; Taguchi, T.; Obata, S.; Takemoto, J.; Takahashi, Y.; Iwanaka, T.; Yanagi, Y.; Kuda, M.; Miyoshi, K.; Matsuura, T.; et al. Immunostaining for Hu C/D and CD56 is useful for a definitive histopathological diagnosis of congenital and acquired isolated hypoganglionosis. Virchows Arch. 2017, 470, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Suhardja, T.S.; Simpson, I.; Lim, J.T.-H. Rare case of adult intestinal hypoganglionosis and review of the literature. Clin. J. Gastroenterol. 2021, 14, 1–9. [Google Scholar] [CrossRef]
- Ohkubo, H.; Masaki, T.; Matsuhashi, N.; Kawahara, H.; Yokoyama, T.; Nakajima, A.; Ohkura, Y. Histopathologic findings in patients with idiopathic megacolon: A comparison between dilated and non-dilated loops. Neurogastroenterol. Motil. 2014, 26, 571–580. [Google Scholar] [CrossRef]
- Wedel, T.; Van Eys, G.J.J.M.; Waltregny, D.; Glénisson, W.; Castronovo, V.; Vanderwinden, J.-M. Novel smooth muscle markers reveal abnormalities of the intestinal musculature in severe colorectal motility disorders. Neurogastroenterol. Motil. 2006, 18, 526–538. [Google Scholar] [CrossRef]
- Do, M.Y.; Myung, S.-J.; Park, H.-J.; Chung, J.-W.; Kim, I.-W.; Lee, S.M.; Yu, C.S.; Lee, H.K.; Lee, J.-K.; Park, Y.S.; et al. Novel Classification and Pathogenetic Analysis of Hypoganglionosis and Adult-Onset Hirschsprung’s Disease. Dig. Dis. Sci. 2011, 56, 1818–1827. [Google Scholar] [CrossRef]
- Hlavaty, L.; Sung, L. Idiopathic Megacolon. Am. J. Forensic Med. Pathol. 2017, 38, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Simpson, R.R.; Kennedy, M.L.; Lubowski, D.Z. Idiopathic megacolon causing iliac vein occlusion and hydronephrosis. Aust. N. Z. J. Surg. 2000, 70, 539–542. [Google Scholar] [CrossRef]
- Kabeer, S.; Dvorkin, L.; Carrannante, J.; Linehan, I. A life-threatening complication of undiagnosed congenital idiopathic megacolon. BMJ Case Rep. 2010, 2010, bcr0420102888. [Google Scholar] [CrossRef] [Green Version]
- Evans, J.T.; Delegge, M.H.; Lawrence, C.; Lewin, D. Acute on Chronic Intestinal Pseudo-Obstruction as a Cause of Death in a Previously Healthy Twenty-Year-Old Male. Dig. Dis. Sci. 2006, 51, 647–651. [Google Scholar] [CrossRef]
- Chatelain, D.; Manaouil, C.; Marc, B.; Ricard, J.; Brevet, M.; Montpellier, D.; Defouilloy, C.; Jardé, O. Adult Hirschsprung’s disease diagnosed during forensic autopsy. J. Forensic Sci. 2006, 51, 1160–1163. [Google Scholar] [CrossRef] [PubMed]
- Cuda, T.; Gunnarsson, R.; De Costa, A. Symptoms and diagnostic criteria of acquired Megacolon—A systematic literature review. BMC Gastroenterol. 2018, 18, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mahmood, F.; Ajayi, O.; Ahmed, M.; Akingboye, A.A. Unusual case of cholecystocolonic fistula secondary to megabowel. BMJ Case Rep. 2020, 13, e237836. [Google Scholar] [CrossRef] [PubMed]
- Gladman, M.; Scott, S.M.; Lunniss, P.J.; Williams, N.S. Systematic Review of Surgical Options for Idiopathic Megarectum and Megacolon. Ann. Surg. 2005, 241, 562–574. [Google Scholar] [CrossRef] [PubMed]
- Karling, P.; Abrahamsson, H.; Dolk, A.; Hallböök, O.; Hellström, P.M.; Knowles, C.H.; Kjellström, L.; Lindberg, G.; Lindfors, P.-J.; Nyhlin, H.; et al. Function and dysfunction of the colon and anorectum in adults: Working team report of the Swedish Motility Group (SMoG). Scand. J. Gastroenterol. 2009, 44, 646–660. [Google Scholar] [CrossRef]
- De la Torre, L.; Cogley, K.; Cabrera-Hernández, M.A.; Frias-Mantilla, J.E.; Wehrli, L.A. Transanal proximal rectosigmoidectomy. A new operation for severe chronic idiopathic constipation associated with megarectosigmoid. J. Pediatr. Surg. 2019, 54, 2311–2317. [Google Scholar] [CrossRef] [Green Version]
- Xu, L.; Shek, K.W.; Wong, K.C.; Tong, K.L.; Hau, M.N. Megacolon as the presenting feature of multiple endocrine neoplasia type 2B: A case report. Hong Kong Med. J. 2019, 25, 483–486. [Google Scholar] [CrossRef]
- Gattuso, J.M.; Kamm, M.A.; Morris, G.; Britton, K.E. Gastrointestinal transit in patients with idiopathic megarectum. Dis. Colon Rectum 1996, 39, 1044–1050. [Google Scholar] [CrossRef]
- Tominaga, T.; Nagayama, S.; Takamatsu, M.; Miyanari, S.; Nagasaki, T.; Yamaguchi, T.; Akiyoshi, T.; Konishi, T.; Fujimoto, Y.; Fukunaga, Y.; et al. A case of severe megacolon due to acquired isolated hypoganglionosis after low anterior resection for lower rectal cancer. Clin. J. Gastroenterol. 2020, 13, 328–333. [Google Scholar] [CrossRef] [Green Version]
- Studer, A.S.; Lonergan, A.M.; Le Guillan, S. Megabowel and Giant Fecaloma: A Surgical Condition? J. Gastrointest. Surg. 2019, 23, 1269–1270. [Google Scholar] [CrossRef] [PubMed]
- Súilleabháin, C.B.Ó.; Anderson, J.H.; McKee, R.F.; Finlay, I.G. Strategy for the surgical management of patients with idiopathic megarectum and megacolon. J. Br. Surg. 2002, 88, 1392–1396. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, M.E.P.; Lopez, M.P.J.; Onglao, M.A.S. Idiopathic megacolon and megarectum in an adult treated with laparoscopic modified Duhamel procedure. BMJ Case Rep. 2021, 14, e240209. [Google Scholar] [CrossRef] [PubMed]
- Knowles, C.H.; Grossi, U.; Horrocks, E.J.; Pares, D.; Vollebregt, P.F.; Chapman, M.; Brown, S.R.; Mercer-Jones, M.; Williams, A.B.; Hooper, R.J.; et al. Surgery for constipation: Systematic review and clinical guidance. Color. Dis. 2017, 19, 5–16. [Google Scholar] [CrossRef] [Green Version]
- Szarka, L.A.; Pemberton, J.H. Treatment of megacolon and megarectum. Curr. Treat. Options Gastroenterol. 2006, 9, 343–350. [Google Scholar] [CrossRef]
- Chung, Y.F.A.; Eu, K.W.; Nyam DC, N.K.; Leong AF, P.K.; Ho, Y.H.; Seow-Choen, F. Minimizing recurrence after sigmoid volvulus. J. Br. Surg. 1999, 86, 231–233. [Google Scholar] [CrossRef]
- Williams, N.S.; Fajobi, O.A.; Lunniss, P.J.; Scott, S.M.; Eccersley, A.J.P.; Ogunbiyi, O.A. Vertical reduction rectoplasty: A new treatment for idiopathic megarectum. J. Br. Surg. 2000, 87, 1203–1208. [Google Scholar] [CrossRef]
- Belliveau, P.; Goldberg, S.M.; Rothenberger, D.A.; Nivatvongs, S. Idiopathic acquired megacolon. Dis. Colon Rectum 1982, 25, 118–121. [Google Scholar] [CrossRef]
- Emile, S. Indications and Technical Aspects of Internal Anal Sphincterotomy: Highlighting the Controversies. Dis. Colon Rectum 2017, 60, 128–132. [Google Scholar] [CrossRef]
- Kamm, M.A.; Hawley, P.R.; Lennard-Jones, J.E. Lateral division of the puborectalis muscle in the management of severe constipation. Br. J. Surg. 1988, 75, 661–663. [Google Scholar] [CrossRef]









| Functional Causes | Dietary Factors (Low Residue) Motility Disturbance (Slow Transit Time, Irritable Bowel Syndrome) Sedentary Lifestyle |
|---|---|
| Degeneration of enteric neurons | Chagas disease |
| Structural abnormalities | Anorectal disorders (anal or perianal fissures, thrombosed hemorrhoids) Colonic strictures (diverticulosis, ischemia, radiation therapy) Colonic tumor and obstruction (adenocarcinoma) |
| Smooth muscle and connective tissue disorders | Scleroderma, amyloidosis Toxic megacolon—inflammatory bowel disease (ulcerative colitis, Crohn disease, Cytomegalovirus, Salmonella, medications, etc) |
| Psychogenic conditions | Anxiety, depression, somatization |
| Neurogenic conditions | Cerebrovascular events, sclerosis, Parkinson’s disease, Hirschsprung’s disease, spinal cord tumors |
| Endocrine and metabolic conditions | Hypo- and hyperparathyroidism, diabetes mellitus, hypo- and hypercalcemia, uremia |
| Drugs | Antidepressants, narcotics, psychotropics, sympathomimetics, anticholinergics, diuretics, antacids, non-steroidal anti-inflammatory drugs, calcium channel blockers, etc. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Constantin, A.; Achim, F.; Spinu, D.; Socea, B.; Predescu, D. Idiopathic Megacolon—Short Review. Diagnostics 2021, 11, 2112. https://doi.org/10.3390/diagnostics11112112
Constantin A, Achim F, Spinu D, Socea B, Predescu D. Idiopathic Megacolon—Short Review. Diagnostics. 2021; 11(11):2112. https://doi.org/10.3390/diagnostics11112112
Chicago/Turabian StyleConstantin, Adrian, Florin Achim, Dan Spinu, Bogdan Socea, and Dragos Predescu. 2021. "Idiopathic Megacolon—Short Review" Diagnostics 11, no. 11: 2112. https://doi.org/10.3390/diagnostics11112112
APA StyleConstantin, A., Achim, F., Spinu, D., Socea, B., & Predescu, D. (2021). Idiopathic Megacolon—Short Review. Diagnostics, 11(11), 2112. https://doi.org/10.3390/diagnostics11112112







