Knee Capsule Anatomy: An MR Imaging and Cadaveric Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
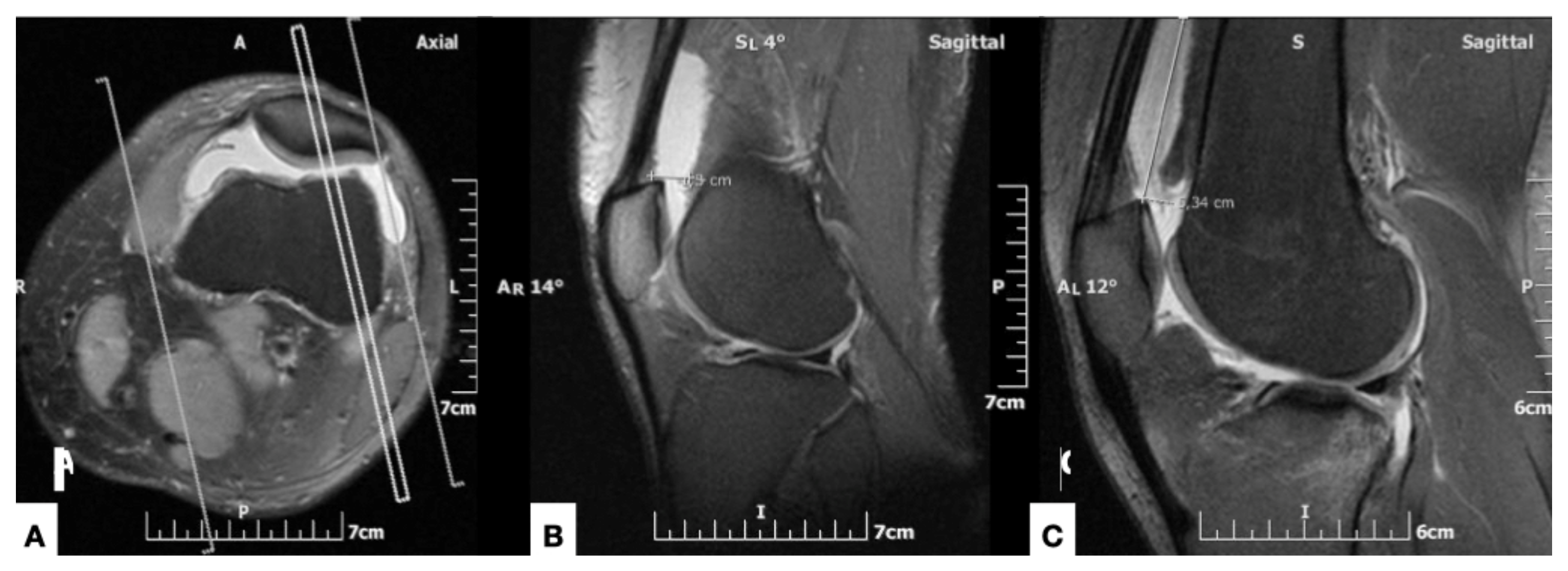
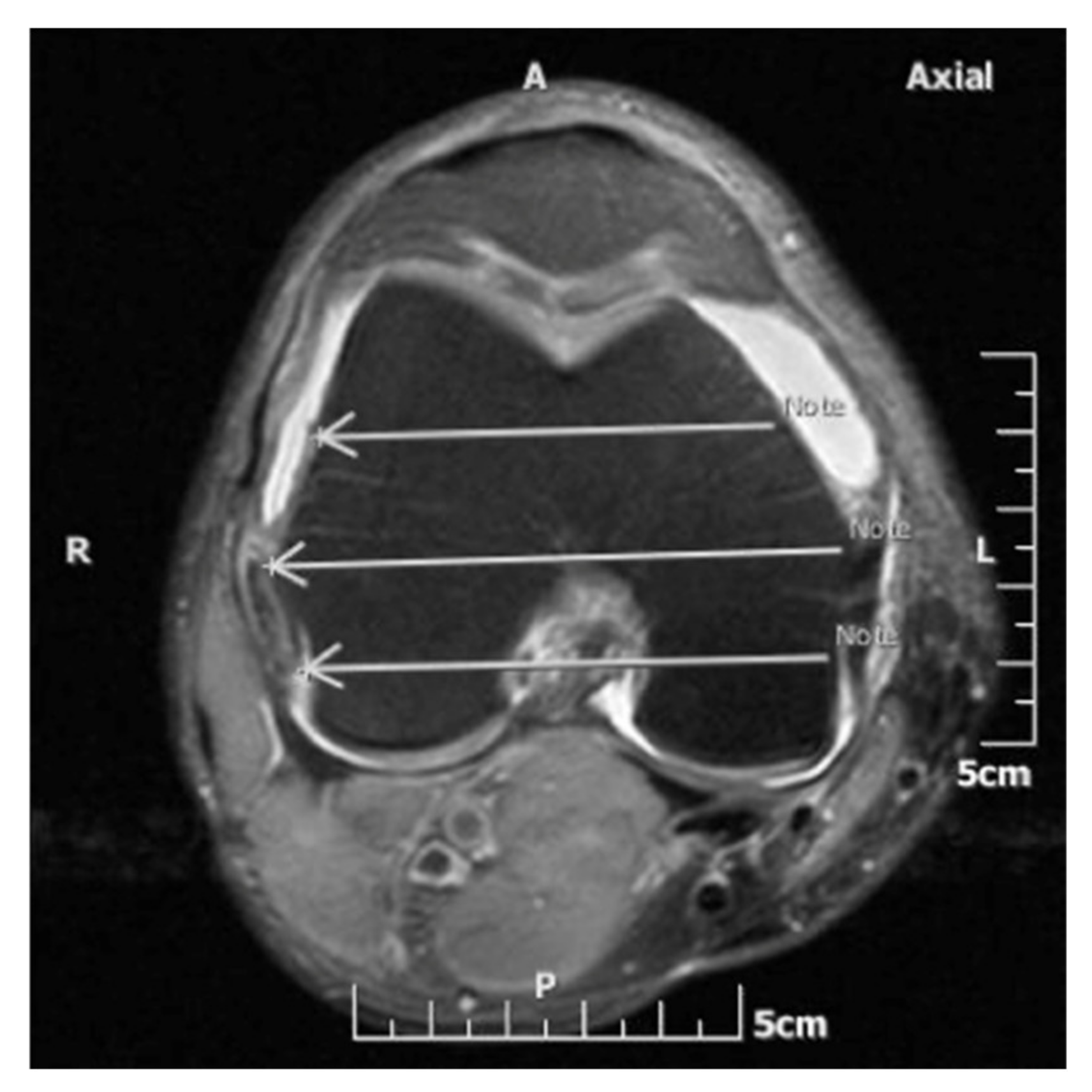
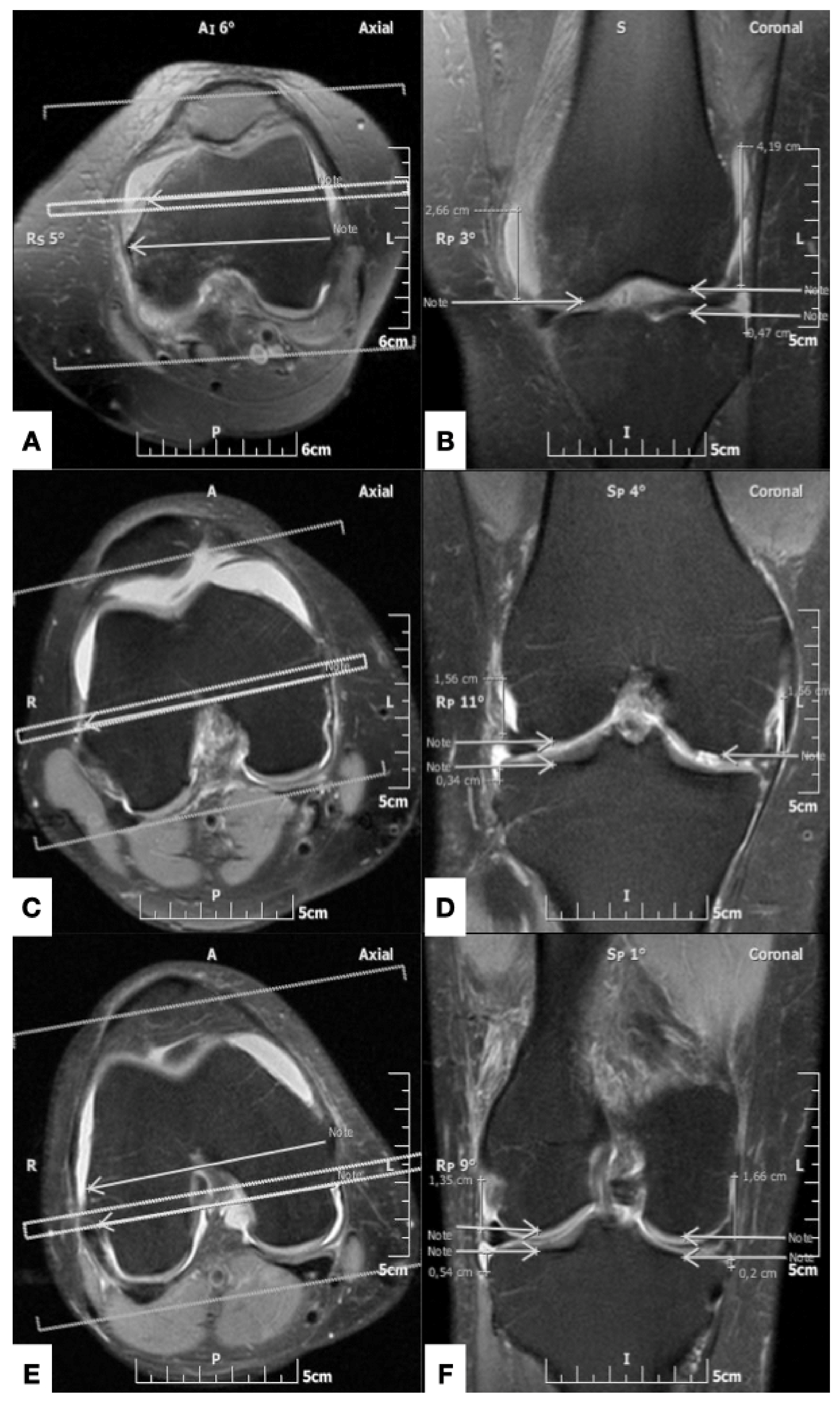
2.2. MR Imaging Protocol and Analysis
2.3. Cadaveric Dissection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Anglen, J.O. Early outcome of hybrid external fixation for fracture of the distal tibia. J. Orthop. Trauma. 1999, 13, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Borrione, F.; Jouvre, J.; Louis, R. External fixation of the tibia. Basic concepts and prospective evaluation. Surg. Radiol. Anat. 1988, 10, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Checketts, R.; Otterburn, M.; MacEachern, A. Pin tract infection: Definition, incidence and prevention. Int. J. Orthop. Trauma 1993, 3, 16–19. [Google Scholar]
- Hutson, J.; Zych, G. Infections in periarticular fractures of the lower extremity treated with tensioned wire hybrid fixators. J. Orthop. Trauma 1998, 12, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.; Johnson, C.; Appleton, P.; Rodriguez, E. Lateral femoral traction pin entry: Risk to the femoral artery and other medial neurovascular structures. J. Orthop. Surg. Res. 2010, 5, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McElvany, M.; Benninger, B.; Smith, S.; Mirza, A.; Marshall, L.; Friess, D. Are Distal Femoral Traction Pins Intra-Articular? A Cadaveric Study. J. Orthop. Trauma 2013, 27, e250–e253. [Google Scholar] [CrossRef] [PubMed]
- Mahan, J.; Seligson, D.; Hemry, S.; Al, E. Factors in pin tract infection. Orthopedics 1991, 14, 305–308. [Google Scholar] [PubMed]
- DeCoster, T.; Crawford, M.; Kraut, M. Safe extracapsular placement of proximal tibia transfixation pins. J. Orthop. Trauma 1999, 13, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Hyman, J.; Moore, T. Anatomy of the distal knee joint and pyarthrosis following external fixation. J. Orthop. Trauma 1999, 13, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Reid, J.; Van Slyke, M.; Moulton, M.; Mann, T. Safe placement of proximal tibial transixation wires with respect to intracapsular penetration. J. Orthop. Trauma 2001, 15, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Stevens, M.; DeCoster, T.; Gracia, F.; Sell, J. Septic knee from Ilizarov transfixation tibial pin. Iowa. Orthop. J. 1995, 15, 217–220. [Google Scholar] [PubMed]
- Vora, A.; Haddad, S.; Kadakia, A.; Lazarus, M.L.; Merk, B.R. Extracapsular placement of distal tibial transfixation wires. J. Bone. Joint. Surg. 2004, 86, 988–993. [Google Scholar] [CrossRef] [PubMed]
- Lowery, K.; Dearden, P.; Sherman., K.; Mahadevan, V.; Sharma, H. Cadaveric analysis of capsular attachments of the distal femur related to pin and wire placement. Injury 2015, 46, 970–974. [Google Scholar] [CrossRef] [PubMed]
- Szwedowski, D.; Herman, K.; Grabowski, R.; Dallo, I.; Domżalski, M. The influence of the variety of the infrapatellar branch of the saphenous nerve on the risk of iatrogenic injuries during arthroscopic procedures in the knee joint. Transl. Res. Anat. 2021, 23, 100120. [Google Scholar]
- Jelev, L.; Krastev, N.; Malinova, L. An aberrant deep muscle crossing popliteal fossa and concomitant popliteal vein variation. A review of the related muscle and venous variations. Transl. Res. Anat. 2021, 25, 100146. [Google Scholar]
- Luyckx, T.; Beckers, L.; Colyn, W.; Bellemans, J. The Adductor Ratio: A New Tool for Joint Line Reconstruction in Revision TKA. Knee. Surg. Sport. Traumatol. Arthosc. 2014, 22, 3028–3033. [Google Scholar] [CrossRef] [PubMed]
- Stavlas, P.; Polyzois, D. Septic arthritis of the major joints of the lower limb after periarticular external fixation application: Are conventional safe corridors enough to prevent it? Injury 2005, 36, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Matziolis, G.; Roehner, E.; Windisch, C.; Wagner, A. The volume of the human knee joint. Arch. Orthop. Trauma Surg. 2015, 135, 1401–1403. [Google Scholar] [CrossRef] [PubMed]



| Anatomical Plane | Cadaver (n = 20) Mean ± SD | MR Imaging (n = 50) Mean ± SD | Univariate Hazard Ratio (95% CI) | p Value |
|---|---|---|---|---|
| Lateral | ||||
| Anterior | 6.47 ± 1.14 | 6.50 ± 1.39 | (−0.87 to 0.82) | ns |
| Middle | 2.92 ± 1.42 | 2.74 ± 1.66 | (−0.66 to 1.03) | ns |
| Posterior | 2.07 ± 1.03 | 1.52 ± 0.96 | (−0.28 to 1.40) | ns |
| Medial | ||||
| Anterior | 5.21 ±1.60 | 4.57 ± 1.60 | −0.19 to 1.46 | ns |
| Middle | 1.62 ± 1.00 | 1.74 ± 1.14 | −0.94 to 0.70 | ns |
| Posterior | 2.08 ± 1.01 | 1.99 ± 1.14 | −0.73 to 0.91 | ns |
| Anatomical plane | Cadaver (n = 20) Mean ± SD | MR Imaging (n = 50) Mean ± SD | Univariate Hazard Ratio (95% CI) | p Value |
|---|---|---|---|---|
| Lateral | ||||
| Anterior | 1.45 ± 2.40 | 0.09 ± 0.15 | (0.85 to 1.86) | <0.0001 |
| Middle | 0.91 ± 0.25 | 0.34 ± 0.19 | (0.06 to 1.09) | <0.05 |
| Posterior | 0.96 ± 0.24 | 0.62 ± 0.53 | (−0.17 to 0.83) | ns |
| Medial | ||||
| Anterior | 0.92 ± 0.25 | 0.11 ± 0.23 | (0.57 to 1.06) | <0.0001 |
| Middle | 0.94 ± 0.25 | 0.26 ± 0.37 | (0.43 to 0.92) | <0.0001 |
| Posterior | 0.98 ± 0.23 | 0.34 ± 0.58 | (0.40 to 0.89) | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zibis, A.H.; Vassalou, E.E.; Raoulis, V.A.; Lampridis, V.; Klontzas, M.E.; Fyllos, A.; Stavlas, P.; Karantanas, A.H. Knee Capsule Anatomy: An MR Imaging and Cadaveric Study. Diagnostics 2021, 11, 1965. https://doi.org/10.3390/diagnostics11111965
Zibis AH, Vassalou EE, Raoulis VA, Lampridis V, Klontzas ME, Fyllos A, Stavlas P, Karantanas AH. Knee Capsule Anatomy: An MR Imaging and Cadaveric Study. Diagnostics. 2021; 11(11):1965. https://doi.org/10.3390/diagnostics11111965
Chicago/Turabian StyleZibis, Aristeidis H., Evangelia E. Vassalou, Vasileios A. Raoulis, Vasileios Lampridis, Michail E. Klontzas, Apostolos Fyllos, Panagiotis Stavlas, and Apostolos H. Karantanas. 2021. "Knee Capsule Anatomy: An MR Imaging and Cadaveric Study" Diagnostics 11, no. 11: 1965. https://doi.org/10.3390/diagnostics11111965
APA StyleZibis, A. H., Vassalou, E. E., Raoulis, V. A., Lampridis, V., Klontzas, M. E., Fyllos, A., Stavlas, P., & Karantanas, A. H. (2021). Knee Capsule Anatomy: An MR Imaging and Cadaveric Study. Diagnostics, 11(11), 1965. https://doi.org/10.3390/diagnostics11111965








