Differences in Dynamics of Lung Computed Tomography Patterns between Survivors and Deceased Adult Patients with COVID-19
Abstract
:1. Introduction
Purpose of the Article
2. Materials and Methods
2.1. Patients
2.2. Methods
2.3. Statistical Analysis
3. Results
3.1. Clinical Information
3.2. CT Manifestations of Coronavirus Infection
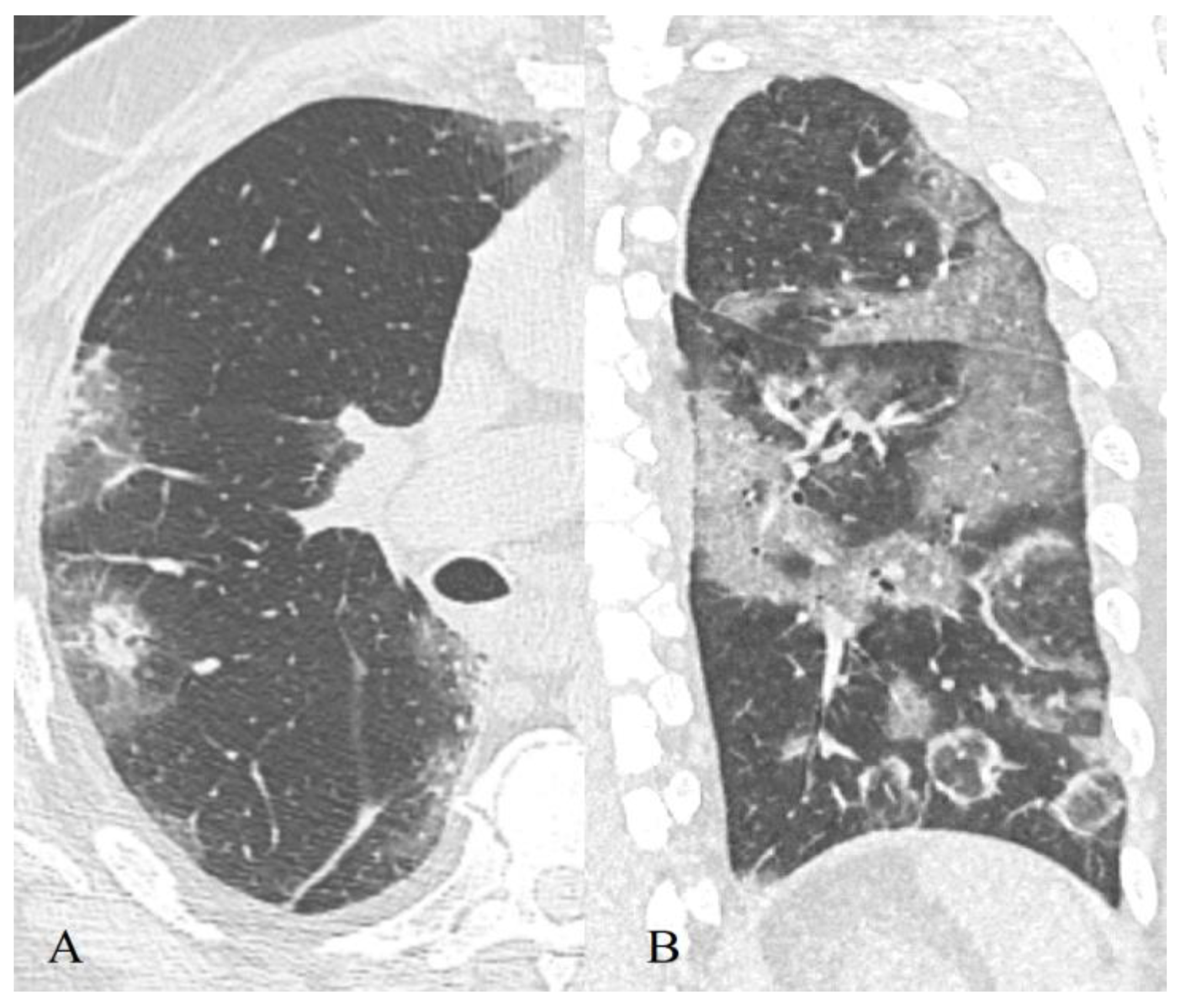
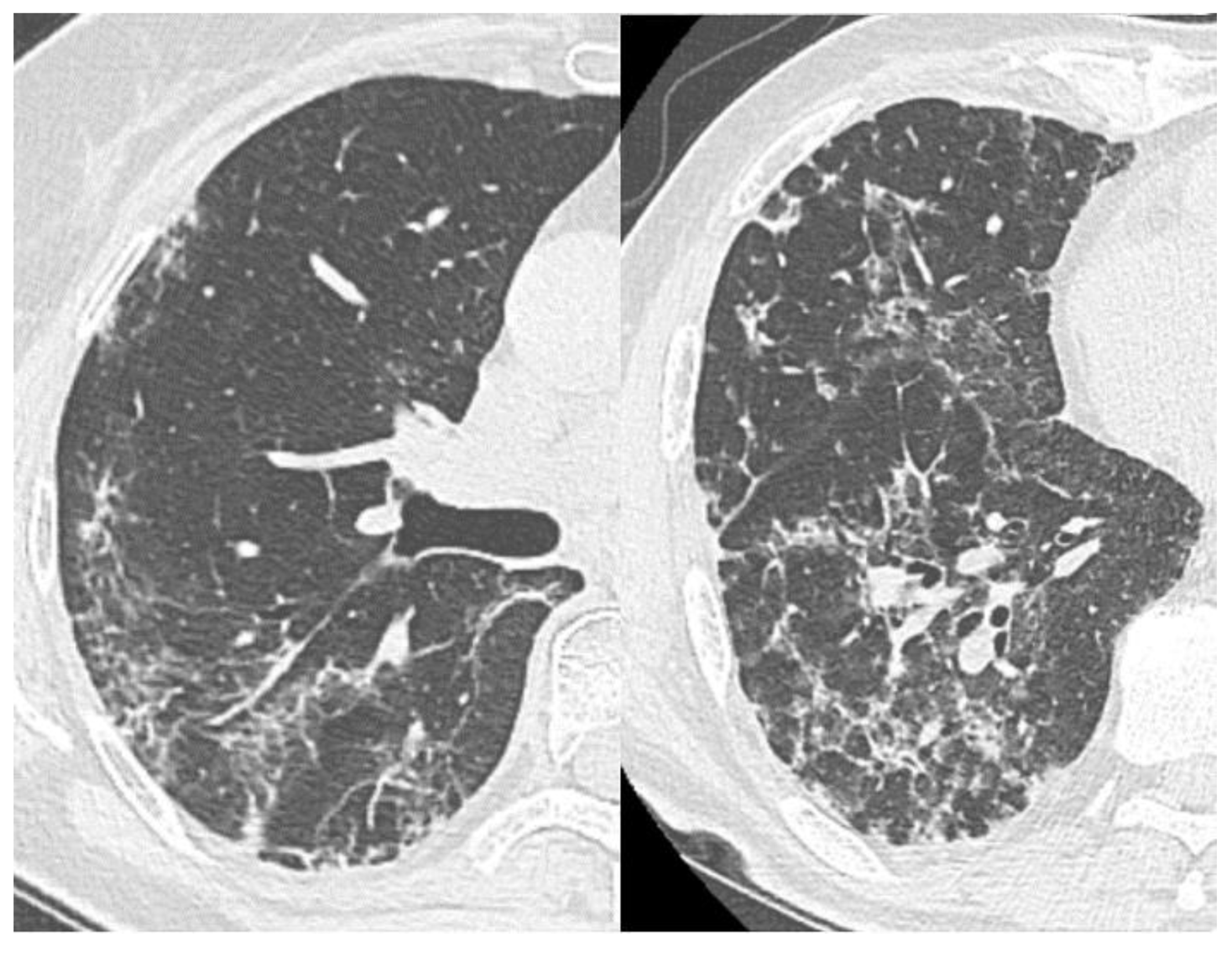
3.2.1. Ground-Glass Opacity
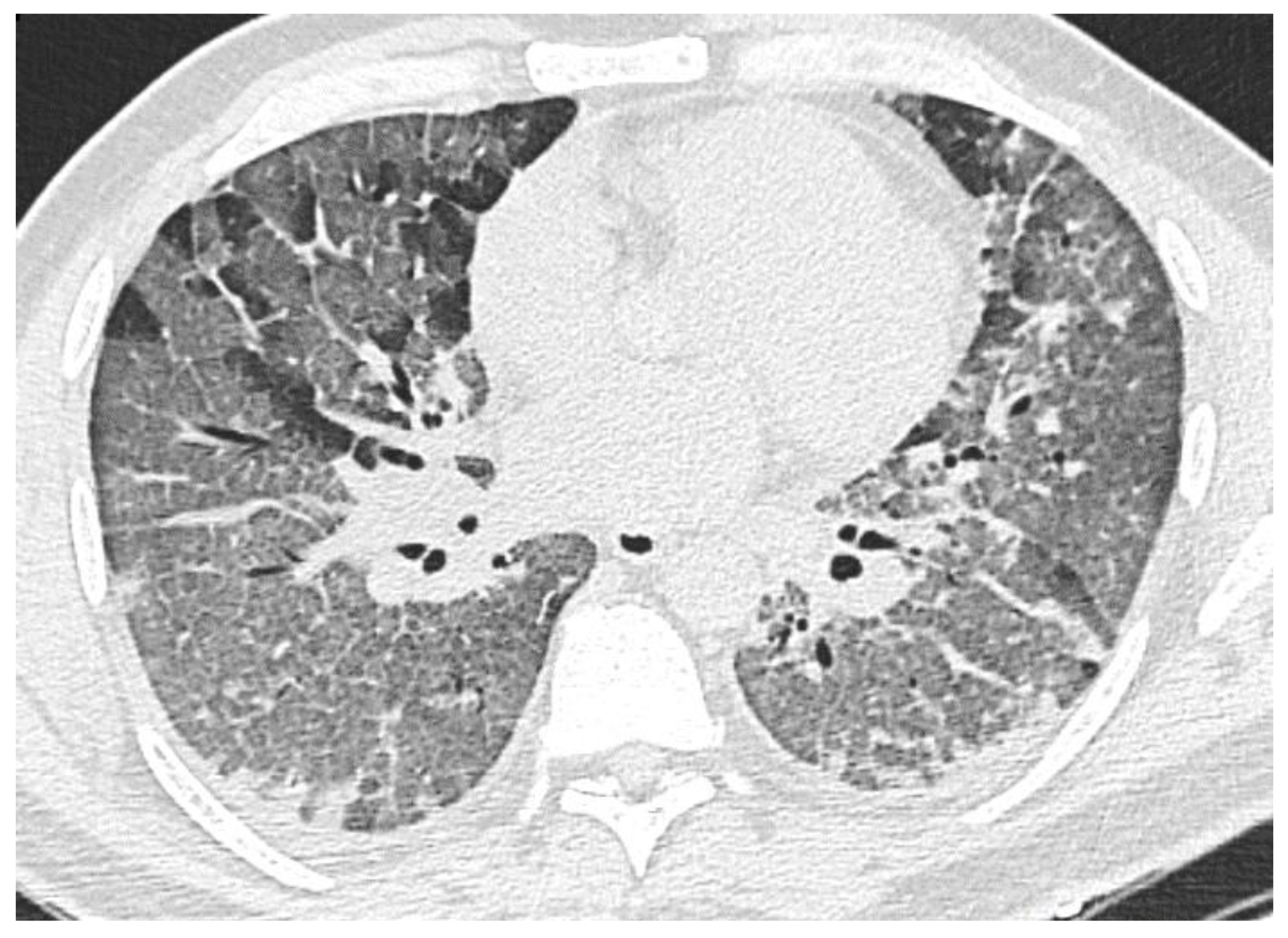
3.2.2. Consolidation
3.2.3. “Crazy Paving” Pattern
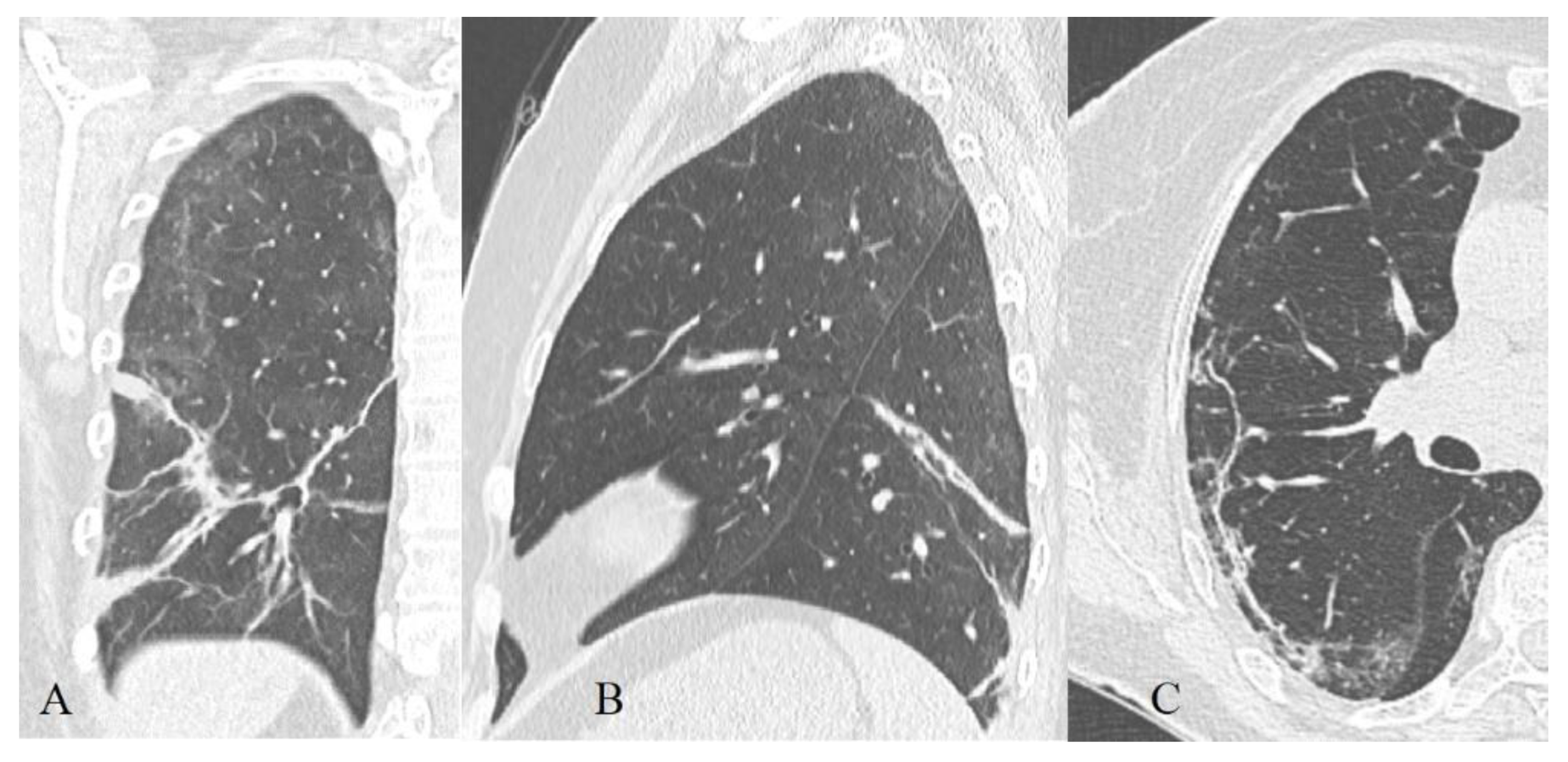
3.2.4. Reticular Interstitial Pattern, Pleuroparenchymal Bands
3.2.5. Localization, Shape, and Volume of the Lesion
3.2.6. Hydrothorax, Hydropericardium, Lymphadenopathy
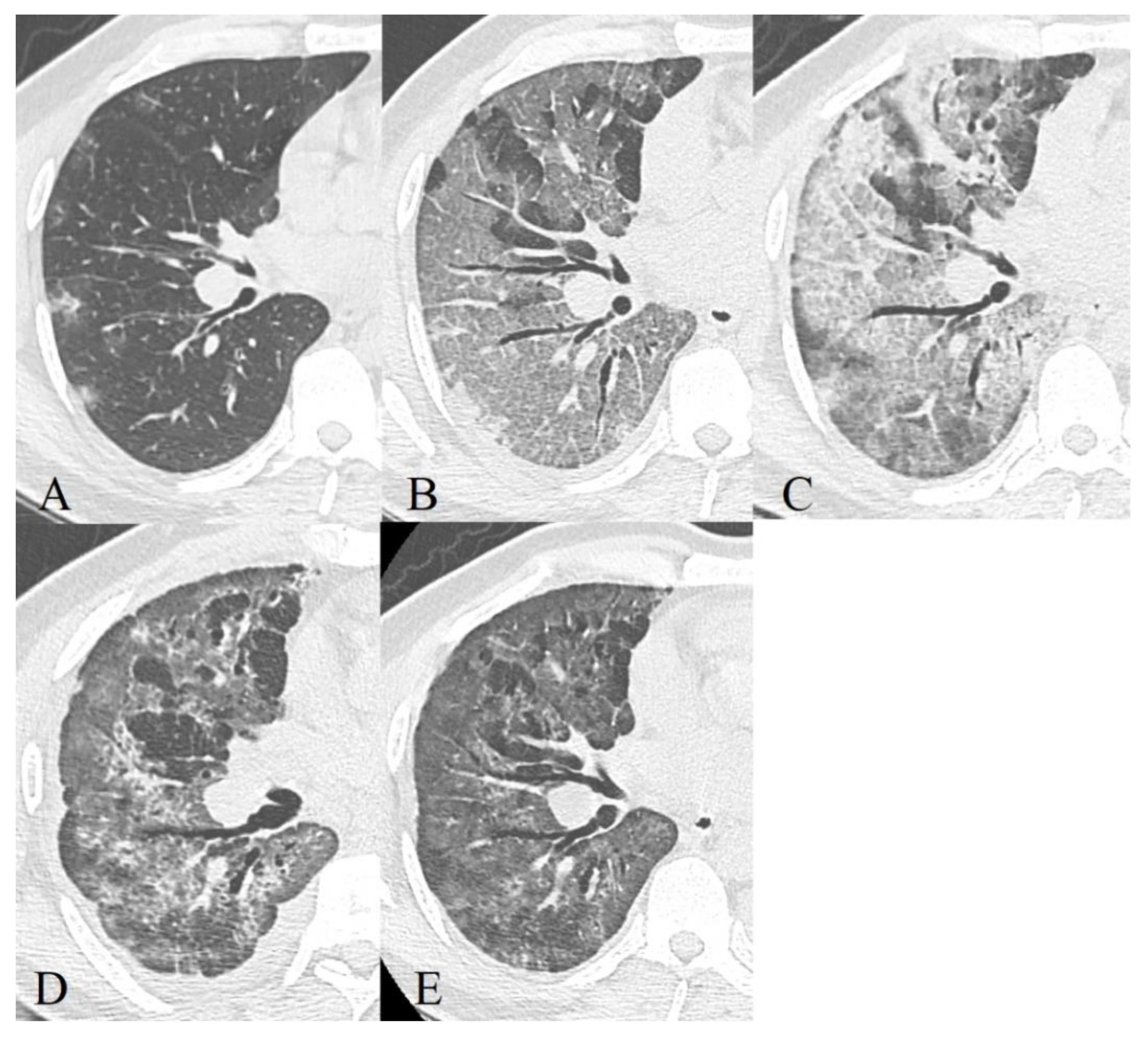
3.3. Dynamics of CT Changes over Time
- Early or initial (0–4 days): normal CT scan or the presence of areas of the GGO type;
- Progressive (5–8 days): an increase in the volume of the GGO type lesions (the frequency of isolated registration is ~40%) and the appearance of CP zones; a combination of GGO and consolidations (in ~43%), GGO and RC (in ~58%); the presence of only consolidations (in ~12%) [43];
- Peak (9–13 days): a significant decrease in the frequency of isolated GGO type changes with a predominance of a combination of GGO and RC (the combination of GGO and consolidations occurred in 30% of cases and already showed a downward trend, in 13% of cases there was a development of pleural effusion, compared to 2.3% during the previous phase) [43];
- Resolution (>14 days): an increase in the volume of the air pulmonary parenchyma with the appearance and predominant contribution of RC, parenchymal bands, and subpleural lines, a reversible halo (signs of organizing pneumonia). At the same time, there is a decrease in the contribution of the combination of GGO and consolidations to the overall CT picture (~9%), with the beginning of a downward trend in the contribution of the combination of GGO and RC (~66%). The contribution of the isolated GGO pattern remained unchanged in comparison with the previous phase (~22%) [43] since consolidation was probably resolved into GGO.
- Early or initial (0–4 days): GGO type changes dominated in both cohorts, but almost 67% of deceased CT studies had CP pattern in this phase of disease, almost half of studies demonstrated mixed GGO-consolidation changes;
- Progressive (5–8 days): an increase in the volume of the GGO, appearance and increase CP (56% of recovered patient’s studies, 73%—deceased), consolidations (57% of recovered patient’s studies, 87%—deceased) type lesions in both cohorts, RC presented in half of the studies;
- Peak (9–13 days): predominance of a combination of GGO (87%), consolidations (67%), and RC (54%) in recovered patients and the combination of CP (87%), consolidations (77%) and RC (65%)—in deceased. RC demonstrated ascending trend in both cohorts, consolidations—in recovered patients, CP—in deceased, the contribution of GGO decreased in both;
- Resolution (>14 days): predominant contribution of consolidations and RC in both cohorts, at the same time there is a decrease in the contribution of GGO, but CP contribution decreased more slowly in deceased than in recovered patients.
3.3.1. Severity of Lung Damage
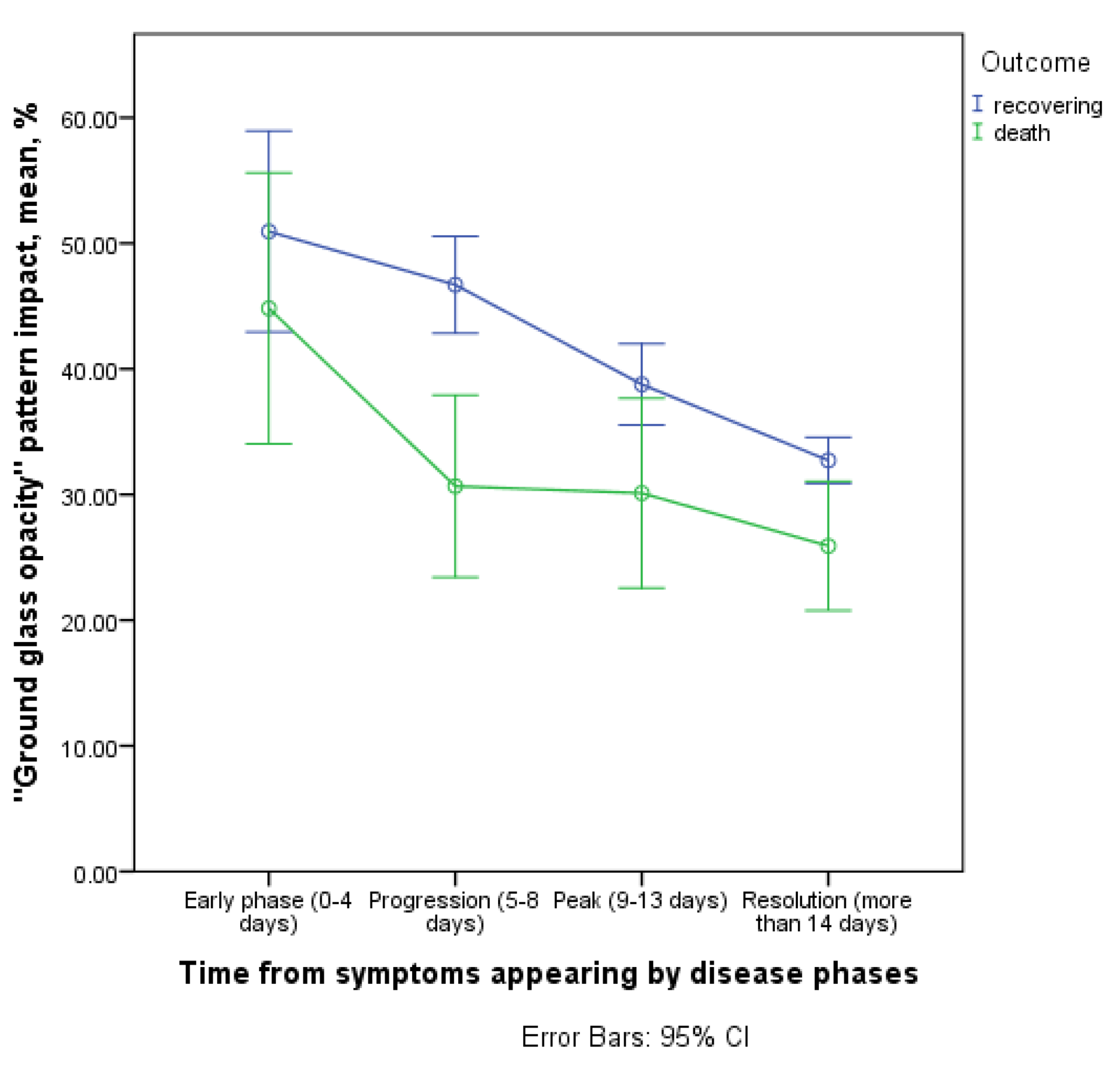
3.3.2. Contribution of the ‘GGO’ Pattern to CT Picture in the Affected Areas
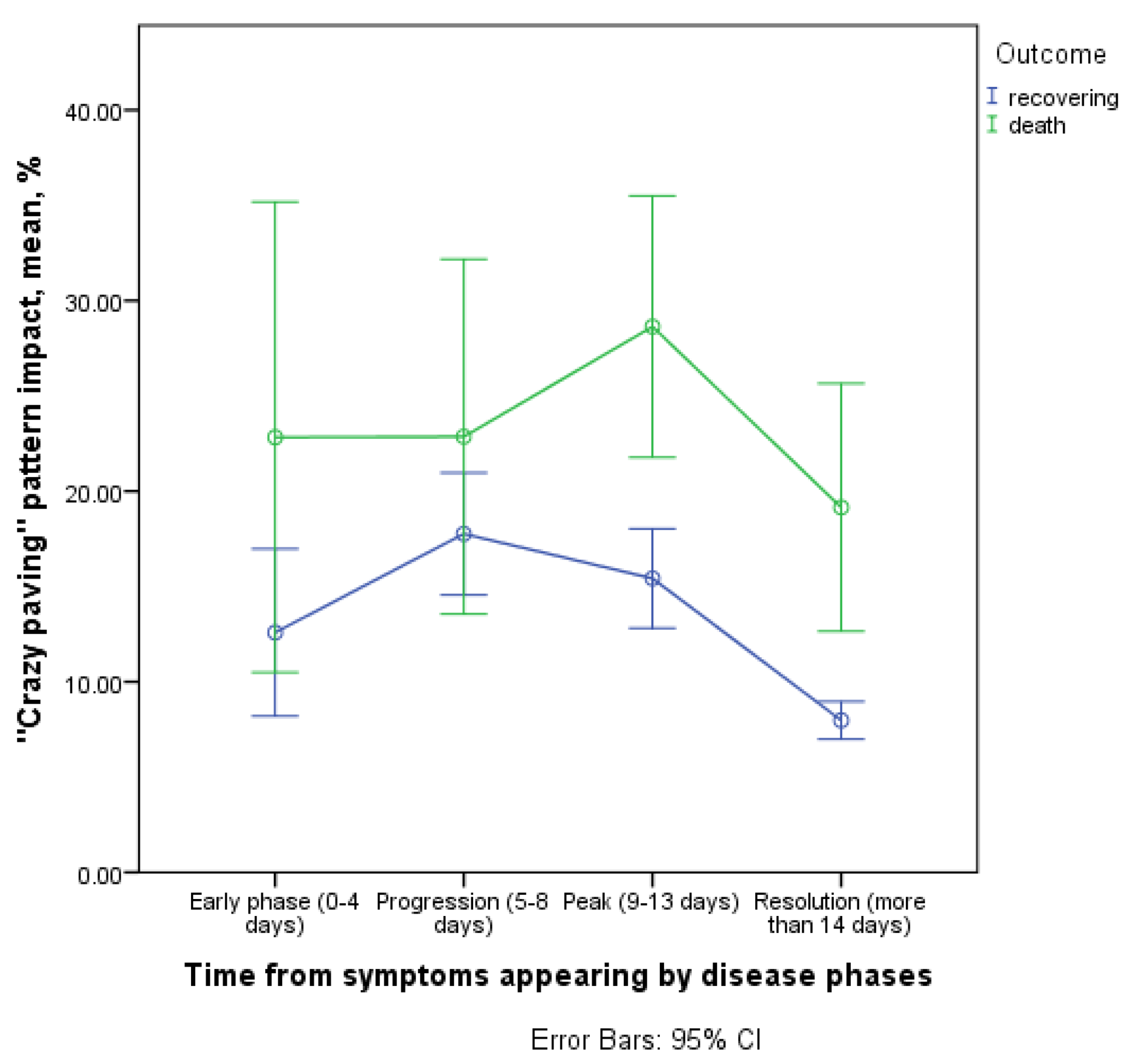
3.3.3. Contribution of the ‘Crazy Paving’ Pattern to CT Picture in the Affected Areas
3.3.4. Contribution of the Consolidation Pattern to CT Picture in the Affected Areas
3.3.5. Contribution of Reticular Changes to CT Picture in the Affected Areas
3.3.6. Contribution of Linear Bands to CT Picture in the Affected Areas
3.3.7. Dominant Patterns on Admission Day, Frequency of Pattern Detection
4. Discussion
5. Limitations of Our Study
- Some combinations of radiological patterns were in the ‘gray’ zone, which makes it possible that certain patterns were not registered correctly, as in many other analyzed articles.
- The volume of lung lesion was registered visually, according to scales that are not devoid of shortcomings and subjectivity.
- The sample of fatal cases was relatively small, which reduced the sensitivity of the statistical analysis.
- This study does not include data from pathomorphological studies, which makes our arguments about the mechanisms of development of certain patterns purely hypothetical.
- There may have been a hidden mutual influence of factors (confounding), which may distort the results of our observational study.
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 Pathophysiology: A Review. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280.e8. [Google Scholar] [CrossRef]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High Expression of ACE2 Receptor of 2019-NCoV on the Epithelial Cells of Oral Mucosa. Int. J. Oral Sci. 2020, 12, 8. [Google Scholar] [CrossRef]
- Wichmann, D.; Sperhake, J.-P.; Lütgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schröder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients With COVID-19. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef]
- Black, J.R.M.; Bailey, C.; Przewrocka, J.; Dijkstra, K.K.; Swanton, C. COVID-19: The Case for Health-Care Worker Screening to Prevent Hospital Transmission. Lancet 2020, 395, 1418–1420. [Google Scholar] [CrossRef]
- Li, X.; Ma, X. Acute Respiratory Failure in COVID-19: Is It “Typical” ARDS? Crit. Care 2020, 24, 1–5. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The Incubation Period of Coronavirus Disease 2019 (CoVID-19) from Publicly Reported Confirmed Cases: Estimation and Application. Ann. Intern. Med. 2020, 172, 577–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, L.; Zhu, J.; Wang, X.; Yang, J.; Liu, X.F.; Xu, X.K. Characterizing COVID-19 Transmission: Incubation Period, Reproduction Rate, and Multiple-Generation Spreading. Front. Phys. 2021, 8, 1–6. [Google Scholar] [CrossRef]
- van Kampen, J.J.A.; van de Vijver, D.A.M.C.; Fraaij, P.L.A.; Haagmans, B.L.; Lamers, M.M.; Okba, N.; van den Akker, J.P.C.; Endeman, H.; Gommers, D.A.M.P.J.; Cornelissen, J.J.; et al. Duration and Key Determinants of Infectious Virus Shedding in Hospitalized Patients with Coronavirus Disease-2019 (COVID-19). Nat. Commun. 2021, 12, 267. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, L.; Ledda, A.; Wymant, C.; Zhao, L.; Ledda, V.; Abeler, L.; Kendall, M.; Nurtay, A.; Cheng, H.; Ng, T.; et al. The Timing of COVID-19 Transmission. MedRxiv 2020. Preprint. [Google Scholar] [CrossRef]
- Yu, X.; Yang, R. COVID-19 Transmission through Asymptomatic Carriers Is a Challenge to Containment. Influenza Other Respir. Viruses 2020, 14, 474–475. [Google Scholar] [CrossRef] [Green Version]
- Rodrigues, J.C.L.; Hare, S.S.; Edey, A.; Devaraj, A.; Jacob, J.; Johnstone, A.; McStay, R.; Nair, A.; Robinson, G. An Update on COVID-19 for the Radiologist—A British Society of Thoracic Imaging Statement. Clin. Radiol. 2020, 75, 323–325. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Y.; Yang, Z.; Ai, T.; Wu, S.; Xia, L. Association of “Initial CT” Findings with Mortality in Older Patients with Coronavirus Disease 2019 (COVID-19). Eur. Radiol. 2021, 31, 567–568. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical Course and Outcomes of Critically Ill Patients with SARS-CoV-2 Pneumonia in Wuhan, China: A Single-Centered, Retrospective, Observational Study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive Study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Izcovich, A.; Ragusa, M.A.; Tortosa, F.; Lavena Marzio, M.A.; Agnoletti, C.; Bengolea, A.; Ceirano, A.; Espinosa, F.; Saavedra, E.; Sanguine, V.; et al. Prognostic Factors for Severity and Mortality in Patients Infected with COVID-19: A Systematic Review. PLoS ONE 2020, 15, e0241955. [Google Scholar] [CrossRef]
- Goyal, P.; Choi, J.J.; Pinheiro, L.C.; Schenck, E.J.; Chen, R.; Jabri, A.; Satlin, M.J.; Campion, T.R.; Nahid, M.; Ringel, J.B.; et al. Clinical Characteristics of Covid-19 in New York City. N. Engl. J. Med. 2020, 382, 2372–2374. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical Course and Risk Factors for Mortality of Adult in Patients With COVID-19 In Wuhan, China: A Retrospective Cohort Study. J. Med. Study Res. 2020, 3, 1–2. [Google Scholar] [CrossRef]
- WHO COVID-19 Dashboard. Available online: https://covid19.who.int/ (accessed on 5 October 2021).
- Brogna, B.; Bignardi, E.; Brogna, C.; Capasso, C.; Gagliardi, G.; Martino, A.; Musto, L.A. Covid-19 Pneumonia in Vaccinated Population: A Six Clinical and Radiological Case Series. Medicina 2021, 57, 891. [Google Scholar] [CrossRef]
- Kim, H.; Hong, H.; Yoon, S.H. Diagnostic Performance of CT and Reverse Transcriptase-Polymerase Chain Reaction for Coronavirus Disease 2019: A Meta-Analysis. Radiology 2020, 296, E145–E155. [Google Scholar] [CrossRef]
- Grassi, R.; Cappabianca, S.; Urraro, F.; Granata, V.; Giacobbe, G.; Magliocchetti, S.; Cozzi, D.; Fusco, R.; Galdiero, R.; Picone, C.; et al. Evolution of Ct Findings and Lung Residue in Patients with Covid-19 Pneumonia: Quantitative Analysis of the Disease with a Computer Automatic Tool. J. Pers. Med. 2021, 11, 641. [Google Scholar] [CrossRef]
- Ciampi, Q.; Antonini-Canterin, F.; Barbieri, A.; Barchitta, A.; Benedetto, F.; Cresti, A.; Miceli, S.; Monte, I.; Petrella, L.; Trocino, G.; et al. Reshaping of Italian Echocardiographic Laboratories Activities during the Second Wave of Covid-19 Pandemic and Expectations for the Post-Pandemic Era. J. Clin. Med. 2021, 10, 3466. [Google Scholar] [CrossRef]
- Yang, R.; Li, X.; Liu, H.; Zhen, Y.; Zhang, X.; Xiong, Q.; Luo, Y.; Gao, C.; Zeng, W. Chest CT Severity Score: An Imaging Tool for Assessing Severe COVID-19. Radiol. Cardiothorac. Imaging 2020, 2, e200047. [Google Scholar] [CrossRef] [Green Version]
- Kondakov, A.; Berdalin, A.; Lelyuk, V.; Gubskiy, I.; Golovin, D. Risk Factors of In-Hospital Mortality in Non-Specialized Tertiary Center Repurposed for Medical Care to COVID-19 Patients in Russia. Diagnostics 2021, 11, 1687. [Google Scholar] [CrossRef]
- Koo, H.J.; Lim, S.; Choe, J.; Choi, S.; Sung, H.; Do, K. Radiographic and CT Features of Viral Pneumonia. RadioGraphics 2018, 38, 719–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaller, T.; Hirschbühl, K.; Burkhardt, K.; Braun, G.; Trepel, M.; Märkl, B.; Claus, R. Postmortem Examination of Patients with COVID-19. J. Am. Med. Assoc. 2020, 323, 2518–2520. [Google Scholar] [CrossRef] [PubMed]
- Barton, L.M.; Duval, E.J.; Stroberg, E.; Ghosh, S.; Mukhopadhyay, S. COVID-19 Autopsies, Oklahoma, USA. Am. J. Clin. Pathol. 2020, 153, 725–733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cai, W.; Yang, J.; Fan, G.; Xu, L.; Zhang, B.; Liu, R. Chest CT Findings of Coronavirus Disease 2019 (COVID-19). J. Coll. Physicians Surg. Pak. 2020, 30, S53–S55. [Google Scholar] [CrossRef]
- Ojha, V.; Mani, A.; Pandey, N.N.; Sharma, S.; Kumar, S. CT in Coronavirus Disease 2019 (COVID-19): A Systematic Review of Chest CT Findings in 4410 Adult Patients. Eur. Radiol. 2020, 30, 6129–6138. [Google Scholar] [CrossRef]
- Ye, Z.; Zhang, Y.; Wang, Y.; Huang, Z.; Song, B. Chest CT Manifestations of New Coronavirus Disease 2019 (COVID-19): A Pictorial Review. Eur. Radiol. 2020, 30, 4381–4389. [Google Scholar] [CrossRef] [Green Version]
- Song, F.; Shi, N.; Shan, F.; Zhang, Z.; Shen, J.; Lu, H.; Ling, Y.; Jiang, Y.; Shi, Y. Emerging 2019 Novel Coronavirus (2019-NCoV) Pneumonia. Radiology 2020, 295, 210–217. [Google Scholar] [CrossRef] [Green Version]
- Inui, S.; Fujikawa, A.; Jitsu, M.; Kunishima, N.; Watanabe, S.; Suzuki, Y.; Umeda, S.; Uwabe, Y. Chest CT Findings in Cases from the Cruise Ship Diamond Princess with Coronavirus Disease (COVID-19). Radiol. Cardiothorac. Imaging 2020, 2, e200110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, H.; Han, X.; Jiang, N.; Cao, Y.; Alwalid, O.; Gu, J.; Fan, Y.; Zheng, C. Radiological Findings from 81 Patients with COVID-19 Pneumonia in Wuhan, China: A Descriptive Study. Lancet Infect. Dis. 2020, 20, 425–434. [Google Scholar] [CrossRef]
- Pan, Y.; Guan, H.; Zhou, S.; Wang, Y.; Li, Q.; Zhu, T.; Hu, Q.; Xia, L. Initial CT Findings and Temporal Changes in Patients with the Novel Coronavirus Pneumonia (2019-NCoV): A Study of 63 Patients in Wuhan, China. Eur. Radiol. 2020, 30, 3306–3309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, M.-Y.; Lee, E.Y.P.; Yang, J.; Yang, F.; Li, X.; Wang, H.; Lui, M.M.; Lo, C.S.-Y.; Leung, B.; Khong, P.-L.; et al. Imaging Profile of the COVID-19 Infection: Radiologic Findings and Literature Review. Radiol. Cardiothorac. Imaging 2020, 2, e200034. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansell, D.M.; Bankier, A.A.; MacMahon, H.; McLoud, T.C.; Müller, N.L.; Remy, J. Fleischner Society: Glossary of Terms for Thoracic Imaging. Radiology 2008, 246, 697–722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henkel, M.; Weikert, T.; Marston, K.; Schwab, N.; Sommer, G.; Haslbauer, J.; Franzeck, F.; Anastasopoulos, C.; Stieltjes, B.; Michel, A.; et al. Lethal COVID-19: Radiologic-Pathologic Correlation of the Lungs. Radiol. Cardiothorac. Imaging 2020, 2, e200406. [Google Scholar] [CrossRef]
- Kanne, J.P.; Little, B.P.; Chung, J.H.; Elicker, B.M.; Ketai, L.H. Essentials for Radiologists on COVID-19: An Update-Radiology Scientific Expert Panel. Radiology 2020, 296, E113–E114. [Google Scholar] [CrossRef] [Green Version]
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef] [Green Version]
- Zhou, S.; Zhu, T.; Wang, Y.; Xia, L. Imaging Features and Evolution on CT in 100 COVID-19 Pneumonia Patients in Wuhan, China. Eur. Radiol. 2020, 30, 5446–5454. [Google Scholar] [CrossRef]
- Sanli, D.E.T.; Yildirim, D.; Sanli, A.N.; Turkmen, S.; Erozan, N.; Husmen, G.; Altundag, A.; Tuzuner, F. A Practical Approach to Imaging Characteristics and Standardized Reporting of COVID-19: A Radiologic Review. Mil. Med. Res. 2021, 8, 1–10. [Google Scholar] [CrossRef]
- Pan, F.; Zheng, C.; Ye, T.; Li, L.; Liu, D.; Li, L.; Hesketh, R.L.; Yang, L. Different Computed Tomography Patterns of Coronavirus Disease 2019 (COVID-19) between Survivors and Non-Survivors. Sci. Rep. 2020, 10, 1–9. [Google Scholar] [CrossRef]
- Li, K.; Wu, J.; Wu, F.; Guo, D.; Chen, L.; Fang, Z.; Li, C. The Clinical and Chest CT Features Associated with Severe and Critical COVID-19 Pneumonia. Investig. Radiol. 2020, 55, 327–331. [Google Scholar] [CrossRef] [PubMed]
- Pershina, E.S.; Cherniaev, A.L.; Samsonova, M.V.; Varyasin, V.V.; Omarova, Z.R.; Pereshivailov, S.O.; Berezhnaia, E.E.; Parshin, V.V.; Mikhailichenko, K.Y.; Shilova, A.S.; et al. Comparison of the CT Patterns and Pulmonary Histology in Patients with COVID-19. Med. Vis. 2020, 24, 37–53. [Google Scholar] [CrossRef]
- Brogna, B.; Bignardi, E.; Brogna, C.; Volpe, M.; Lombardi, G.; Rosa, A.; Gagliardi, G.; Capasso, P.F.M.; Gravino, E.; Maio, F.; et al. A Pictorial Review of the Role of Imaging in the Detection, Management, Histopathological Correlations, and Complications of Covid-19 Pneumonia. Diagnostics 2021, 11, 437. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; Liu, S.; Zhao, P.; Liu, H.; Zhu, L.; et al. Pathological Findings of COVID-19 Associated with Acute Respiratory Distress Syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef]
- Pogatchnik, B.P.; Swenson, K.E.; Sharifi, H.; Bedi, H.; Berry, G.J.; Guo, H.H. Radiology–Pathology Correlation Demonstrating Organizing Pneumonia in a Patient Who Recovered from COVID-19. Am. J. Respir. Crit. Care Med. 2020, 202, 598–599. [Google Scholar] [CrossRef]
- Copin, M.-C.; Parmentier, E.; Duburcq, T.; Poissy, J.; Mathieu, D. Time to Consider Histologic Pattern of Lung Injury to Treat Critically Ill Patients with COVID-19 Infection. Intensive Care Med. 2020, 46, 1124–1126. [Google Scholar] [CrossRef] [Green Version]
- Gattinoni, L.; Chiumello, D.; Caironi, P.; Busana, M.; Romitti, F.; Brazzi, L.; Camporota, L. COVID-19 Pneumonia: Different Respiratory Treatments for Different Phenotypes? Intensive Care Med. 2020, 46, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Barisione, E.; Grillo, F.; Ball, L.; Bianchi, R.; Grosso, M.; Morbini, P.; Pelosi, P.; Patroniti, N.A.; de Lucia, A.; Orengo, G.; et al. Fibrotic Progression and Radiologic Correlation in Matched Lung Samples from COVID-19 Post-Mortems. Virchows Arch. 2021, 478, 471–485. [Google Scholar] [CrossRef] [PubMed]
- Castro, C.Y. ARDS and Diffuse Alveolar Damage: A Pathologist’s Perspective. Semin. Thorac. Cardiovasc. Surg. 2006, 18, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Sarmiento, X.; Guardiola, J.J.; Almirall, J.; Mesalles, E.; Mate, J.L.; Soler, M.; Klamburg, J. Discrepancy between Clinical Criteria for Diagnosing Acute Respiratory Distress Syndrome Secondary to Community Acquired Pneumonia with Autopsy Findings of Diffuse Alveolar Damage. Respir. Med. 2011, 105, 1170–1175. [Google Scholar] [CrossRef] [Green Version]
- Oikonomou, A.; Hansell, D.M. Organizing Pneumonia: The Many Morphological Faces. Eur. Radiol. 2002, 12, 1486–1496. [Google Scholar] [CrossRef]
- Beasley, M.B.; Franks, T.J.; Galvin, J.R.; Gochuico, B.; Travis, W.D. Acute Fibrinous and Organizing Pneumonia. Arch. Pathol. Lab. Med. 2002, 126, 1064–1070. [Google Scholar] [CrossRef]
- Kashiwabara, K.; Kohshi, S.I. Additional Computed Tomography Scans in the Prone Position to Distinguish Early Interstitial Lung Disease from Dependent Density on Helical Computed Tomography Screening Patient Characteristics. Respirology 2006, 11, 482–487. [Google Scholar] [CrossRef]
- Carsana, L.; Sonzogni, A.; Nasr, A.; Rossi, R.S.; Pellegrinelli, A.; Zerbi, P.; Rech, R.; Colombo, R.; Antinori, S.; Corbellino, M.; et al. Pulmonary Post-Mortem Findings in a Series of COVID-19 Cases from Northern Italy: A Two-Centre Descriptive Study. Lancet Infect. Dis. 2020, 20, 1135–1140. [Google Scholar] [CrossRef]
- Yu, M.; Xu, D.; Lan, L.; Tu, M.; Liao, R.; Cai, S.; Cao, Y.; Xu, L.; Liao, M.; Zhang, X.; et al. Thin-Section Chest CT Imaging of COVID-19 Pneumonia: A Comparison Between Patients with Mild and Severe Disease. Radiol. Cardiothorac. Imaging 2020, 2, e200126. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.-C.; Luo, H.; Liu, S.; Huang, S.; Zhou, Z.; Yu, Q.; Zhang, S.; Zhao, Z.; Yu, Y.; Yang, Y.; et al. Dynamic Evolution of COVID-19 on Chest Computed Tomography: Experience from Jiangsu Province of China. Eur. Radiol. 2020, 30, 6194–6203. [Google Scholar] [CrossRef]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A.; et al. Chest CT Score in COVID-19 Patients: Correlation with Disease Severity and Short-Term Prognosis. Eur. Radiol. 2020, 30, 6808–6817. [Google Scholar] [CrossRef]
- Zhang, J.; Meng, G.; Li, W.; Shi, B.; Dong, H.; Su, Z.; Huang, Q.; Gao, P. Relationship of Chest CT Score with Clinical Characteristics of 108 Patients Hospitalized with COVID-19 in Wuhan, China. Respir. Res. 2020, 21, 180. [Google Scholar] [CrossRef]
- Li, K.; Chen, D.; Chen, S.; Feng, Y.; Chang, C.; Wang, Z.; Wang, N.; Zhen, G. Predictors of Fatality Including Radiographic Findings in Adults with COVID-19. Respir. Res. 2020, 21, 146. [Google Scholar] [CrossRef] [PubMed]
- Ruch, Y.; Kaeuffer, C.; Ohana, M.; Labani, A.; Fabacher, T.; Bilbault, P.; Kepka, S.; Solis, M.; Greigert, V.; Lefebvre, N.; et al. CT Lung Lesions as Predictors of Early Death or ICU Admission in COVID-19 Patients. Clin. Microbiol. Infect. 2020, 26, 1417.e5–1417.e8. [Google Scholar] [CrossRef] [PubMed]
- Li, K.; Fang, Y.; Li, W.; Pan, C.; Qin, P.; Zhong, Y.; Liu, X.; Huang, M.; Liao, Y.; Li, S. CT Image Visual Quantitative Evaluation and Clinical Classification of Coronavirus Disease (COVID-19). Eur. Radiol. 2020, 30, 4407–4416. [Google Scholar] [CrossRef] [Green Version]
- Leonardi, A.; Scipione, R.; Alfieri, G.; Petrillo, R.; Dolciami, M.; Ciccarelli, F.; Perotti, S.; Cartocci, G.; Scala, A.; Imperiale, C.; et al. Role of Computed Tomography in Predicting Critical Disease in Patients with Covid-19 Pneumonia: A Retrospective Study Using a Semiautomatic Quantitative Method. Eur. J. Radiol. 2020, 130, 109202. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; He, G.; Yang, X.; Chen, J.; Wu, J.; Ma, M.; Lu, W.; Li, Q.; Cheng, T.; Huang, X. Dynamic Changes of Chest CT Follow-up in Coronavirus Disease-19 (COVID-19) Pneumonia: Relationship to Clinical Typing. BMC Med. Imaging 2020, 20, 92. [Google Scholar] [CrossRef]
- Liu, X.; Zhou, H.; Zhou, Y.; Wu, X.; Zhao, Y.; Lu, Y.; Tan, W.; Yuan, M.; Ding, X.; Zou, J.; et al. Temporal Radiographic Changes in COVID-19 Patients: Relationship to Disease Severity and Viral Clearance. Sci. Rep. 2020, 10, 10263. [Google Scholar] [CrossRef]
- Zhao, W.; Zhong, Z.; Xie, X.; Yu, Q.; Liu, J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. Am. J. Roentgenol. 2020, 214, 1072–1077. [Google Scholar] [CrossRef]
- Zhang, N.; Xu, X.; Zhou, L.-Y.; Chen, G.; Li, Y.; Yin, H.; Sun, Z. Clinical Characteristics and Chest CT Imaging Features of Critically Ill COVID-19 Patients. Eur. Radiol. 2020, 30, 6151–6160. [Google Scholar] [CrossRef]
- McKleroy, W.; Lyn-Kew, K. 500 Million Alveoli from 30,000 Feet: A Brief Primer on Lung Anatomy. Lung Innate Immun. Inflamm. Methods Mol. Biol. 2018, 1809, 3–15. [Google Scholar]








| Risk Factor | NR | ND | OR | |
|---|---|---|---|---|
| Gender (m vs. f) | Male | 314 | 37 | 1.97 * (95% CI 1.07–3.62) |
| Female | 268 | 16 | ||
| Gender (m vs. f, aged 59 or more) | Male | 125 | 25 | 1.83 (95% CI 0.92–3.62) |
| Female | 137 | 15 | ||
| Gender (m vs. f, under 59 years old) | Male | 189 | 12 | 8.32 * (95% CI 1.07–64.75) |
| Female | 131 | 1 | ||
| Body mass index | <25 | 124 | 11 | 0.78 (95% CI 0.38–1.60) |
| ≥25 | 420 | 29 | ||
| Body mass index | <30 | 323 | 27 | 0.70 (95% CI 0.36–1.39) |
| ≥30 | 221 | 13 | ||
| Current smoking | Yes | 51 | 5 | 1.17 (95% CI 0.44–3.08) |
| No | 525 | 44 | ||
| Alcohol abuse (self-reported) | Yes | 5 | 3 | 7.13 * (95% CI 1.65–30.72) |
| No | 570 | 48 | ||
| CT-Pattern | Early Phase | Progressive Phase | Peak Phase | Resolution Phase | ||||
|---|---|---|---|---|---|---|---|---|
| %R | %D | %R | %D | %R | %D | %R | %D | |
| Ground glass opacity | 81.8 | 94.4 | 93.1 | 87.0 | 87.3 | 83.3 | 86.1 | 83.8 |
| Crazy paving | 38.7 | 66.7 | 56.0 | 72.7 | 50.2 | 86.7 | 36.3 | 61.8 |
| Consolidations | 48.0 | 47.4 | 56.9 | 87.0 | 67.3 | 76.7 | 71.6 | 91.7 |
| Reticular interstitial changes | 36.5 | 55.6 | 53.0 | 47.8 | 53.8 | 64.5 | 71.1 | 61.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akopyan, G.B.; Berdalin, A.B.; Gubskiy, I.L.; Lelyuk, V.G. Differences in Dynamics of Lung Computed Tomography Patterns between Survivors and Deceased Adult Patients with COVID-19. Diagnostics 2021, 11, 1937. https://doi.org/10.3390/diagnostics11101937
Akopyan GB, Berdalin AB, Gubskiy IL, Lelyuk VG. Differences in Dynamics of Lung Computed Tomography Patterns between Survivors and Deceased Adult Patients with COVID-19. Diagnostics. 2021; 11(10):1937. https://doi.org/10.3390/diagnostics11101937
Chicago/Turabian StyleAkopyan, Gevorg B., Alexander B. Berdalin, Ilya L. Gubskiy, and Vladimir G. Lelyuk. 2021. "Differences in Dynamics of Lung Computed Tomography Patterns between Survivors and Deceased Adult Patients with COVID-19" Diagnostics 11, no. 10: 1937. https://doi.org/10.3390/diagnostics11101937
APA StyleAkopyan, G. B., Berdalin, A. B., Gubskiy, I. L., & Lelyuk, V. G. (2021). Differences in Dynamics of Lung Computed Tomography Patterns between Survivors and Deceased Adult Patients with COVID-19. Diagnostics, 11(10), 1937. https://doi.org/10.3390/diagnostics11101937







