1. Introduction
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) is the gold standard technique for diagnosing solid pancreatic masses. The pathological assessment was originally based on cytological findings, which provide 85–97% sensitivity, 88–98% specificity, and 78–96% diagnostic accuracy [
1,
2,
3]. However, histopathological assessments provide more information regarding tissue architecture and immunohistological staining, thus facilitating a more accurate and precise diagnosis than that obtainable with cytological assessment [
4]. In addition, histopathological findings, including immunostaining, are essential for diagnosing various diseases, such as lymphoma, autoimmune pancreatitis, and other rare tumors. Large-caliber 19-gauge needles have been used to obtain sufficient biopsy samples for histopathological assessment [
5,
6,
7] although this technique has some technical issues related to the stiff shaft and unsharpened tip. To overcome these issues, third-generation FNA needles, including Franseen needles, were recently developed [
8]. Franseen needles have three symmetric heels at the tip and their unique shape helps obtain a sufficient sample for histopathological assessment in most cases, even if the needle is a conventional caliber (22-gauge, 22G). Several studies have indicated that using a Franseen needle during EUS-guided fine needle biopsy (EUS-FNB) provides various benefits [
9,
10,
11], although the feasibility of using Franseen needles might be limited for smaller lesions. Therefore, this study aimed to evaluate the feasibility of histopathological assessment for small pancreatic lesions using a 22G Franseen needle during EUS-FNB.
2. Materials and Methods
2.1. Patients
This retrospective single-center study was conducted at the University of Toyama Hospital and included all patients who underwent EUS-FNB for solid pancreatic lesions between June 2018 and April 2020. During this period, a 22G Franseen needle (Acquire; Boston Scientific, Marlborough, MA, USA) was routinely used as the first biopsy needle at our institution. The patient and lesion characteristics, final diagnosis, diagnostic ability, and adverse events of EUS-FNB using a 22G Franseen needle were investigated. The severity of adverse events was defined according to the American Society for Gastrointestinal Endoscopy classification [
12]. This retrospective study protocol was approved by the institutional review board of our institution (R2020096) on 25 August 2020, and registered in the University Hospital Medical Information Network clinical trials registry (UMIN000041511). All patients had provided informed consent for the EUS-FNB procedure.
2.2. Procedural Technique
The EUS was performed as an in-patient procedure using a curved linear echoendoscope (GF-UCT260; Olympus Corporation, Tokyo, Japan) connected to an ultrasound scanning system (EU-ME2; Olympus Corporation, Tokyo, Japan). The patients underwent EUS-FNB under conscious sedation with midazolam, and their vital signs were monitored. Two experienced endosonographers (I.Y. and K.T.) performed the EUS-FNB using a 22G Franseen needle (Acquire; Boston Scientific) in all cases, as previously reported [
13]. The lesion was punctured via the stomach or duodenum under guidance from real-time EUS imaging, and color Doppler imaging was used to confirm that the puncture path would not disrupt any major vessels or the main pancreatic duct. The stylet was then removed, a 20 mL syringe was attached to the needle, and 10 mL of negative pressure was applied. Several movements were made within the lesion and the suction was slowly released after the movements were completed. The needle was then withdrawn into the sheath and the entire system was withdrawn from the biopsy channel. The aspirated material was expelled onto glass slides by carefully reinserting the stylet into the needle. All patients were observed for ≥24 h after the procedure.
The specimen was macroscopically evaluated, and the whitish portions (macroscopically visible core) were collected and placed on a small piece of filter paper. The sample was then placed in formalin solution for histological examination and the remaining material was smeared on glass slides for cytological examination. As our institution does not have an on-site pathologist or cytologist, punctures were repeated up to three times until a whitish material was macroscopically observed. If the third puncture was not successful, the lesion was diagnosed based on only the cytological examination.
2.3. Definition
In this study, the diagnosis based on the EUS-FNB specimen was determined using the histological and cytological findings. The “histological diagnosis” only considered the histological findings (without cytology) and included pancreatic cancer, neuroendocrine neoplasm (NEN), metastatic tumor, and solid pseudopapillary neoplasm (SPN). The cytological diagnosis was classified as definite, suspected malignancy (including NEN and SPN), or benign, based on the Bethesda system. Cases judged as “definite” or “suspicious” by cytological diagnosis were defined as malignant. The final diagnosis was based on: (1) definite evidence of malignancy from a surgical specimen, (2) a diagnosis of malignancy based on the EUS-FNB findings and clinical/imaging follow-up compatible with malignant disease, or (3) no evidence of malignancy based on the EUS-FNB findings and clinical/imaging follow-up of ≥6 months.
2.4. Endpoints
The primary endpoint was the diagnostic accuracy of EUS-FNB for small pancreatic lesions (diameter of <10 mm). The diagnostic histopathological results of small pancreatic lesions were compared with those of other lesions (>10 mm). We also analyzed factors that were associated with the accuracy of the histopathological diagnosis using EUS-FNB.
2.5. Statistical Analyses
Continuous variables were presented as median (range) and categorical variables were presented as number (percentage). Univariate and multivariate analyses were performed to identify the factors influencing the accuracy of the histopathological diagnosis using EUS-FNB. The univariate analyses were performed using the chi-squared test or Fisher’s exact test for categorical variables and the Mann-Whitney U-test for continuous variables. The multivariate analysis was performed using a logistic regression model, and factors with a univariate p-value of <0.05 were entered into the multivariate model. All analyses were performed using JMP® software (version 15; SAS Institute, Inc., Cary, NC, USA).
4. Discussion
Franseen needles have emerged as a preferable alternative to conventional needles as they can easily obtain larger tissue samples than conventional needles. For example, relative to a conventional needle, a Franseen needle of the same gauge provides approximately 5× the median area of tissue sample for histopathological evaluation [
10]. In this context, larger samples preserve tissue architecture and can provide a more accurate and easier pathological diagnosis, relative to smaller samples. We have also reported that a macroscopic on-site evaluation of the macroscopically visible core can help determine the required number of needle punctures, even without rapid on-site cytological evaluation (ROSE) [
7], which can reduce the burden on endosonographers and pathologists. Furthermore, obtaining a sufficient core sample can enable genetic analysis and molecular profiling [
8,
14], which can contribute to personalized treatment selection. Several studies have already confirmed the efficacy of the Franseen needle [
15,
16,
17]. A meta-analysis of 15 studies with 1024 patients revealed that, relative to FNA needles and in the absence of ROSE, FNB needles provided better diagnostic adequacy for solid pancreatic lesions and required fewer needle passes to establish the diagnosis [
18]. Our previous study also revealed that use of a Franseen needle provided sufficient tissue samples for histological interpretation in 96% of cases with a single needle pass and in 100% of cases with 3 needle passes [
16].
Several studies have addressed factors that affect the diagnostic accuracy of EUS-FNA. Uehara et al. [
19] reported that the diagnostic accuracy of EUS-FNA was not associated with lesion size, lesion location, or needle size, based on their retrospective study, and concluded that EUS-FNA was useful for diagnosing small pancreatic lesions (<10 mm). However, Agarwal et al. [
20] reported that the diagnostic accuracy of EUS-FNA was lower for suspicious pancreatic lesions that were <20 mm, relative to lesions that were >21 mm. Haba et al. [
21] also reported that a low diagnostic accuracy was independently associated with a nonpancreatic cancer final diagnosis, pancreatic head lesion location, lesion size of <20 mm, and absence of ROSE. Furthermore, they found that lesion size and ROSE had the greatest influence on diagnostic accuracy. Kurita et al. [
22] also reported that the diagnostic accuracy of EUS-FNA was significantly lower for small pancreatic tumors (<5 mm) accompanied by chronic pancreatitis and pancreatic cancer. Thus, small lesion size appears to be associated with lower diagnostic accuracy, although those studies used conventional FNA needles and the pathological diagnosis was mainly based on cytological assessment. Therefore, it is unclear whether EUS-FNB using a Franseen needle is feasible for histopathological assessment of small pancreatic lesions.
The present study revealed that the overall accuracy of EUS-FNB (combining cytology and histology) was 98.7% for all lesions, and the accuracy was still high (94.3%) for lesions that were <10 mm. Nevertheless, the diagnostic accuracy based on the histological examination alone was only 64.3% for small lesions (<10 mm), although the accuracy increased to 97.2% for lesions that were >10 mm (
p < 0.001). In addition, lower diagnostic accuracy was associated with age <70 years and a non-pancreatic cancer final diagnosis, although these factors were not significant in the multivariate analysis, and only lesion size was an independent predictor of histopathological diagnosis accuracy. This may be related to cases with small lesions (<10 mm) often involving younger patients (<70 years old) and patients with non-NEN tumors (
Table 7).
A detailed examination of the EUS-FNB results for lesions that were <10 mm revealed some interesting findings. First, sufficient samples could not be obtained for the histopathological diagnosis in all 4 cases that had lesions of <5 mm although the histopathological diagnosis was accurate in 9 out of 10 cases (90%) that had lesions measuring in the range of 6–10 mm. Thus, a lesion size of <5 mm, rather than <10 mm, may influence the accuracy of the histopathological diagnosis, which may be related to the difficulty of visualizing and puncturing these small lesions. Nevertheless, cytological diagnosis was possible in all 4 cases with lesion sizes of <5 mm, which would suggest that the needle punctured the lesion correctly. Therefore, we conclude that the histopathological diagnosis is likely more difficult than the cytopathological diagnosis in cases with such small lesions. However, combining the cytologic and histopathologic information provided by the biopsy may enhance the diagnostic accuracy in such cases.
Interestingly, all 4 cases with lesions of <5 mm had a cytological diagnosis of NEN, which might have contributed to the failed histopathological diagnosis. However, the diagnostic accuracy of EUS-FNA is generally considered lower for pancreatic cancer than for other pathologies [
22]. This may be because pancreatic cancer often involves an intense stromal desmoplastic reaction [
23], which may make it difficult to aspirate the sample during FNB and to histopathologically diagnose the limited number of cancer cells in abundant desmoplastic tissue from a small specimen.
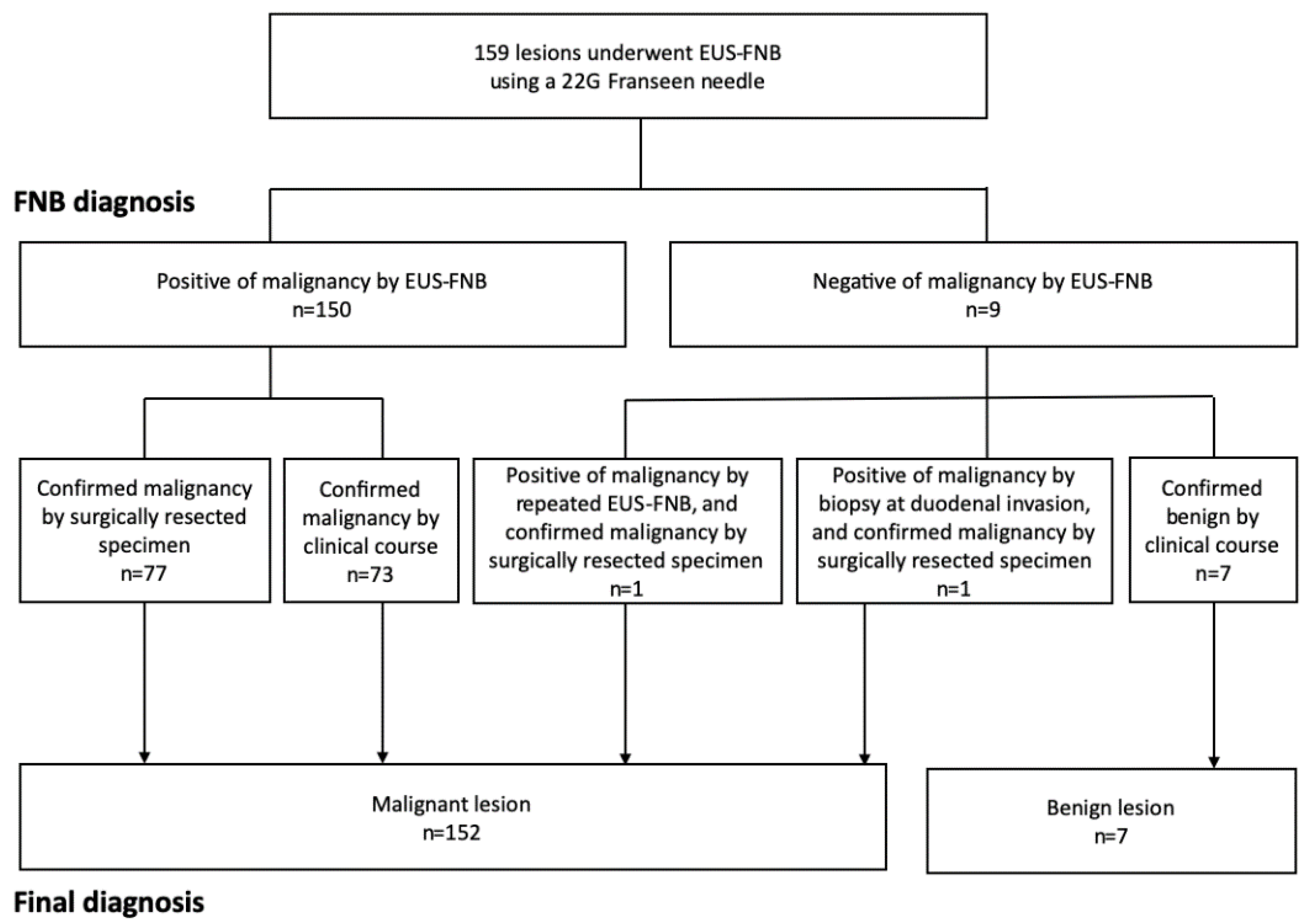
The present study has some limitations. First, the retrospective single-center study design and small number of patients are associated with risks of bias. However, during the study period, we routinely performed EUS-FNB with a Franseen needle for all patients with solid pancreatic masses, regardless of lesion size and location. Nevertheless, large prospective studies are needed to validate our findings. Second, the final diagnoses were confirmed based on the surgical specimen in 79 out of 159 patients, while the EUS-FNB findings and clinical course were used to confirm the diagnoses for the other 80 patients (73 malignant lesions and 7 benign lesions). It is possible that the 7 patients who were diagnosed with benign tumors might actually have had low-grade malignancy, although they did not exhibit any signs of malignancy during a ≥6-month follow-up. Third, the study, including the assessment of diagnostic accuracy, is limited by a very small number of biopsies of lesions of <5 mm.
In conclusion, the diagnostic accuracy for small lesions (<10 mm), especially for lesions of <5 mm, based on the histological examination alone, was significantly lower than for other lesions (>10 mm). Furthermore, multivariate analysis revealed that only lesion size was an independent predictor of histopathological diagnosis accuracy.