Selected Matrix Metalloproteinases (MMP-2, MMP-7) and Their Inhibitor (TIMP-2) in Adult and Pediatric Cancer
Abstract
1. Introduction
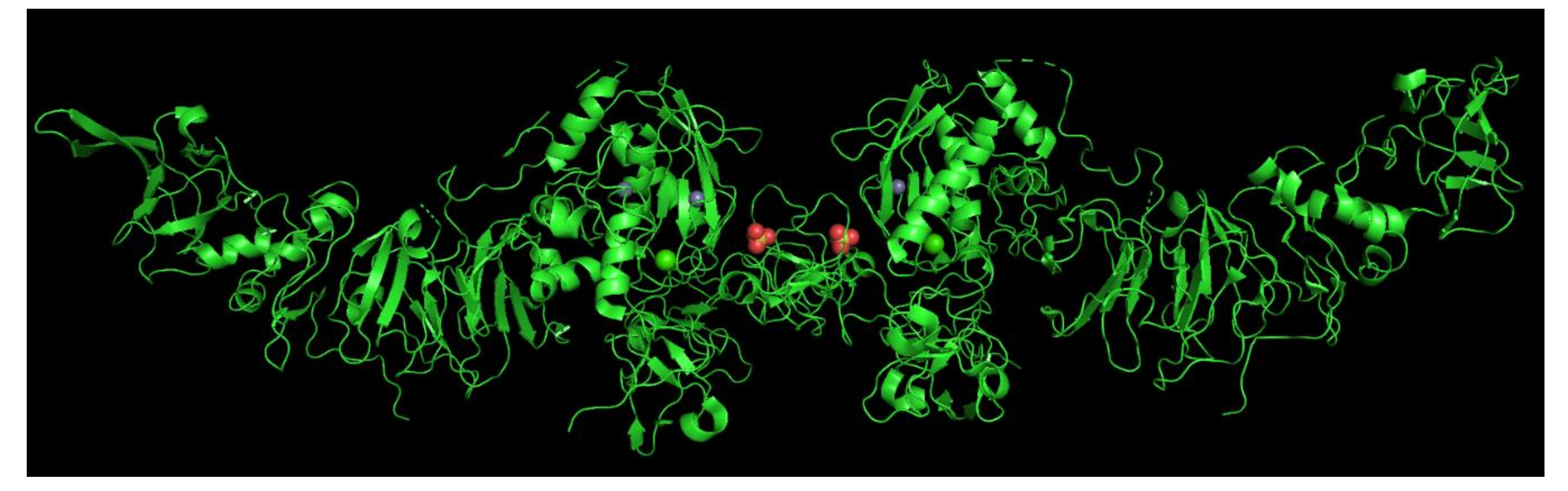
2. MMP—Characteristic and Classification
3. TIMPs—Characteristic and Classification
4. The Involvement of Metalloproteinases and Their Inhibitors in Cancer
4.1. Adult Population—The Involvement of MMPs and TIMP
4.1.1. MMP-2 Involvement in Cancer
4.1.2. TIMP-2 Dual Role in Cancer
4.1.3. MMP-2/TIMP-2 Imbalance in Cancer
4.1.4. MMP-7 Involvement in Cancer
4.2. Pediatric Cancer and MMP-2, MMP-7, and TIMP-2 Involvement
5. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Klemm, F.; Joyce, J.A. Microenvironmental regulation of therapeutic response in cancer. Trends Cell Biol. 2015, 25, 198–213. [Google Scholar] [CrossRef]
- Roy, R.; Yang, J.; Moses, M.A. Matrix metalloproteinases as novel biomarkers and potential therapeutic targets in human cancer. J. Clin. Oncol. 2009, 27, 5287–5297. [Google Scholar] [CrossRef]
- Paiva, K.B.S.; Granjeiro, J.M. Matrix Metalloproteinases in Bone Resorption, Remodeling, and Repair. Prog. Mol. Biol. Transl. 2017, 148, 203–303. [Google Scholar] [CrossRef]
- Rooprai, H.K.; Martin, A.J.; King, A.; Appadu, U.D.; Jones, H.; Selway, R.P.; Gullan, R.W.; Pilkington, G.J. Comparative gene expression profiling of ADAMs, MMPs, TIMPs, EMMPRIN, EGF-R and VEGFA in low grade meningioma. Int. J. Oncol. 2016, 49, 2309–2318. [Google Scholar] [CrossRef]
- Hannocks, M.J.; Zhang, X.; Gerwien, H.; Chashchina, A.; Burmeister, M.; Korpos, E.; Song, J.; Sorokin, L. The gelatinases, MMP-2 and MMP-9, as fine tuners of neuroinflammatory processes. Matrix Biol. 2019, 75–76, 102–113. [Google Scholar] [CrossRef] [PubMed]
- Singh, T.; Adekoya, O.A.; Jayaram, B. Understanding the binding of inhibitors of matrix metalloproteinases by molecular docking, quantum mechanical calculations, molecular dynamics simulations, and a MMGBSA/MMBappl study. Mol. BioSyst. 2015, 11, 1041–1051. [Google Scholar] [CrossRef] [PubMed]
- Tallant, C.; Marrero, A.; Gomis-Rüth, F.X. Matrix metalloproteinases: Fold and function of their catalytic domains. Biochim. Biophys. Acta 2010, 1803, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Klein, T.; Bischoff, R. Physiology and pathophysiology of matrix metalloproteases. J. Amino Acids 2011, 41, 271–290. [Google Scholar] [CrossRef]
- Miekus, N.; Luise, C.; Sippl, W.; Baczek, T.; Schmelzer, C.E.H.; Heinz, A. MMP-14 degrades tropoelastin and elastin. Biochimie 2019, 165, 32–39. [Google Scholar] [CrossRef]
- Nam, D.H.; Lee, K.B.; Ge, X. Functional production of catalytic domains of human MMPs in Escherichia coli periplasm. Methods Mol. Biol. 2018, 1731, 65–72. [Google Scholar] [CrossRef]
- Zhong, S.; Khalil, R.A. A Disintegrin and Metalloproteinase (ADAM) and ADAM with thrombospondin motifs (ADAMTS) family in vascular biology and disease. Biochem. Pharmacol. 2019, 164, 188–204. [Google Scholar] [CrossRef] [PubMed]
- Alipour, H.; Raz, A.; Zakeri, S.; Djadid, N.D. Therapeutic applications of collagenase (metalloproteases): A review. Asian Pac. J. Trop. Biomed. 2016, 6, 975–981. [Google Scholar] [CrossRef]
- Xue, M.; Jackson, C.J. Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring. Adv. Wound Care 2015, 4, 119–136. [Google Scholar] [CrossRef] [PubMed]
- Sorsa, T.; Tjäderhane, L.; Konttinen, Y.T.; Lauhio, A.; Salo, T.; Lee, H.M.; Golub, L.M.; Brown, D.L.; Mäntylä, P. Matrix metalloproteinases: Contribution to pathogenesis, diagnosis and treatment of periodontal inflammation. Ann. Med. 2006, 38, 306–321. [Google Scholar] [CrossRef] [PubMed]
- Sorsa, T.; Gursoy, U.K.; Nwhator, S.; Hernandez, M.; Tervahartiala, T.; Leppilahti, J.; Gursoy, M.; Könönen, E.; Emingil, G.; Pussinen, P.J.; et al. Analysis of matrix metalloproteinases, especially MMP-8, in gingival creviclular fluid, mouthrinse and saliva for monitoring periodontal diseases. Periodontology 2000 2016, 70, 142–163. [Google Scholar] [CrossRef]
- Sorsa, T.; Alassiri, S.; Grigoriadis, A.; Räisänen, I.T.; Pärnänen, P.; Nwhator, S.O.; Gieselmann, D.R.; Sakellari, D. Active MMP-8 (aMMP-8) as a Grading and Staging Biomarker in the Periodontitis Classification. Diagnostics 2020, 10, 61. [Google Scholar] [CrossRef]
- Lauhio, A.; Färkkilä, E.; Pietiläinen, K.H.; Åström, P.; Winkelmann, A.; Tervahartiala, T.; Pirilä, E.; Rissanen, A.; Kaprio, J.; Sorsa, T.A.; et al. Association of MMP-8 with obesity, smoking and insulin resistance. Eur. J. Clin. Investg. 2016, 46, 757–765. [Google Scholar] [CrossRef]
- Rodríguez, D.; Morrison, C.J.; Overall, C.M. Matrix metalloproteinases: What do they not do? New substrates and biological roles identified by murine models and proteomics. Biochim. Biophys. Acta 2010, 1803, 39–54. [Google Scholar] [CrossRef]
- Padala, C.; Tupurani, M.A.; Puranam, K.; Gantala, S.; Shyamala, N.; Kondapalli, M.S.; Gundapaneni, K.K.; Mudigonda, S.; Galimudi, R.K.; Kupsal, K.; et al. Synergistic effect of collagenase-1 (MMP1), stromelysin-1 (MMP3) and gelatinase-B (MMP9) gene polymorphisms in breast cancer. PLoS ONE 2017, 12, e0184448. [Google Scholar] [CrossRef]
- Zhang, X.; Huang, S.; Guo, J.; Zhou, L.; You, L.; Zhang, T.; Zhao, Y. Insights into the distinct roles of MMP-11 in tumor biology and future therapeutics (Review). Int. J. Oncol. 2016, 48, 1783–1793. [Google Scholar] [CrossRef]
- Mora-Gutiérrez, J.M.; Rodríguez, J.A.; Fernández-Seara, M.A.; Orbe, J.; Escalada, F.J.; Soler, M.J.; Roblero, M.F.S.; Riera, M.; Páramo, J.A.; Garcia-Fernandez, N. MMP-10 is Increased in Early Stage Diabetic Kidney Disease and can be Reduced by Renin-Angiotensin System Blockade. Sci. Rep. 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Razai, A.S.; Eckelman, B.P.; Salvesen, G.S. Selective inhibition of matrix metalloproteinase 10 (MMP10) with a single-domain antibody. J. Biol. Chem. 2020, 295, 2464–2472. [Google Scholar] [CrossRef]
- Jabłonska-Trypuc, A.; Matejczyk, M.; Rosochacki, S. Matrix metalloproteinases (MMPs), the main extracellular matrix (ECM) enzymes in collagen degradation, as a target for anticancer drugs. J. Enzyme Inhib. Med. Chem. 2016, 31, 177–183. [Google Scholar] [CrossRef]
- Wielockx, B.; Libert, C.; Wilson, C. Matrilysin (matrix metalloproteinase-7): A new promising drug target in cancer and inflammation? Cytokine Growth Factor Rev. 2004, 15, 111–115. [Google Scholar] [CrossRef]
- Khamis, Z.I.; Iczkowski, K.A.; Man, Y.G.; Bou-Dargham, M.J.; Sang, Q.X.A. Evidence for a Proapoptotic Role of Matrix Metalloproteinase-26 in Human Prostate Cancer Cells and Tissues. J. Cancer 2016, 7, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Itoh, Y. Membrane-type matrix metalloproteinases: Their functions and regulations. Matrix Biol. 2015, 44–46, 207–223. [Google Scholar] [CrossRef]
- Sounni, N.E.; Paye, A.; Host, L.; Noël, A. MT-MMPs as regulators of vessel stability associated with angiogenesis. Front. Pharmacol. 2011, 2, 111. [Google Scholar] [CrossRef]
- Garbacki, N.; Di Valentin, E.; Piette, J.; Cataldo, D.; Crahay, C.; Colige, A. Matrix metalloproteinase 12 silencing: A therapeutic approach to treat pathological lung tissue remodeling? Pulm. Pharmacol. Ther. 2009, 22, 267–278. [Google Scholar] [CrossRef]
- Conlon, G.A.; Murray, G.I. Recent advances in understanding the roles of matrix metalloproteinases in tumour invasion and metastasis. J. Pathol. 2019, 247, 629–640. [Google Scholar] [CrossRef]
- Caterina, J.J.; Skobe, Z.; Shi, J.; Ding, Y.; Simmer, J.P.; Birkedal-Hansen, H.; Bartlett, J.D. Enamelysin (Matrix Metalloproteinase 20)-deficient Mice Display an Amelogenesis Imperfecta Phenotype. J. Biol. Chem. 2002, 277, 49598–49604. [Google Scholar] [CrossRef]
- Manicone, A.M.; Birkland, T.P.; Lin, M.; Betsuyaku, T.; van Rooijen, N.; Lohi, J.; Keski-Oja, J.; Wang, Y.; Skerrett, S.J.; Parks, W.C. Epilysin (MMP-28) Restrains Early Macrophage Recruitment in Pseudomonas aeruginosa Pneumonia. J. Immunol. 2009, 182, 3866–3876. [Google Scholar] [CrossRef]
- Illman, S.A.; Lohi, J.; Keski-Oja, J. Epilysin (MMP-28)—Structure, expression and potential functions. Exp. Dermatol. 2008, 17, 897–907. [Google Scholar] [CrossRef]
- Raeeszadeh-Sarmazdeh, M.; Greene, K.E.; Sankaran, B.; Downey, G.P.; Radisky, D.C.; Radisky, E.S. Directed evolution of the metalloproteinase inhibitor TIMP-1 reveals that its N- and C-terminal domains cooperate in matrix metalloproteinase recognition. J. Biol. Chem. 2019. [Google Scholar] [CrossRef]
- Arpino, V.; Brocka, M.; Gill, S.E. The role of TIMPs in regulation of extracellular matrix proteolysis. Matrix Biol. 2015, 44–46, 247–254. [Google Scholar] [CrossRef]
- Jackson, H.W.; Defamie, V.; Waterhouse, P.; Khokha, R. TIMPs: Versatile Extracellular Regulators in Cancer. Nat. Rev. Cancer 2017, 17, 38–53. [Google Scholar] [CrossRef]
- Okada, Y. Proteinases and Matrix Degradation. In Kelley and Firestein’s Textbook of Rheumatology, 10th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2017; pp. 106–125. [Google Scholar]
- Raeeszadeh-Sarmazdeh, M.; Coban, M.; Sankaran, B.; Radisky, E. Engineering protein therapeutics for cancer based on the natural matrix metalloproteinase inhibitor TIMP-1. Biochem. Mol. Biol. 2020, 34. [Google Scholar] [CrossRef]
- Fischer, T.; Riedl, R. Inhibitory Antibodies Designed for Matrix Metalloproteinase Modulation. Molecules 2019, 24, 2265. [Google Scholar] [CrossRef]
- Zhong, Y.; Lu, Y.T.; Sun, Y.; Shi, Z.H.; Li, N.G.; Tang, Y.P.; Duan, J.A. Recent opportunities in matrix metalloproteinase inhibitor drug design for cancer. Expert. Opin. Drug Discov. 2018, 13, 75–87. [Google Scholar] [CrossRef]
- Sartakhti, J.S.; Manshaei, M.H.; Sadeghi, M. MMP-TIMP Interactions in Cancer Invasion: An Evolutionary Game-Theoretical Framework. J. Theor. Biol. 2017, 412, 17–26. [Google Scholar] [CrossRef]
- Seo, D.W.; Saxinger, W.C.; Guedez, L.; Cantelmo, A.R.; Albini, A.; Stetler-Stevenson, W.G. An integrin-binding N-terminal peptide region of TIMP-2 retains potent angio-inhibitory and anti-tumorigenic activity in vivo. Peptides 2011, 32, 1840–1848. [Google Scholar] [CrossRef]
- Bourboulia, D.; Jensen-Taubman, S.; Stetler-Stevenson, W.G. TIMP-2: An Endogenous Angiogenesis Inhibitor with Distinct Antitumoral Properties. Treat. Strateg. Hematol. 2012, 2, 31–35. [Google Scholar]
- Sounni, N.E.; Rozanov, D.V.; Remacle, A.G.; Golubkov, V.S.; Noel, A.; Strongin, A.Y. Timp-2 binding with cellular MT1-MMP stimulates invasion-promoting MEK/ERK signaling in cancer cells. Int. J. Cancer 2010, 126, 1067–1078. [Google Scholar] [CrossRef]
- Langenskiold, M.; Holmdahl, L.; Falk, P.; Ivarsson, M.L. Increased plasma MMP-2 protein expression in lymph-node positive patients with colorectal cancer. Int. J. Colorectal Dis. 2005, 20, 245–252. [Google Scholar] [CrossRef]
- Hilska, M.; Roberts, P.J.; Collan, Y.U.; Laine, V.J.O.; Kossi, J.; Hirsimaki, P.; Rahkonen, O.; Laato, M. Progostic significance of matrix metalloproteinases-1, -2, -7 and -13 and tissue inhibitors of metalloproteinases-1, -2, -3 and -4 in colorectal cancer. Int. J. Cancer 2007, 121, 714–723. [Google Scholar] [CrossRef]
- Wu, X.; Li, H.; Kang, L.; Li, L.; Wang, W.; Shan, B. Activated Matrix Metalloproteinase-2—A Potential Marker of Prognosis for Epithelial Ovarian Cancer. Gynecol. Oncol. 2002, 84, 126–134. [Google Scholar] [CrossRef]
- Perigny, M.; Bairati, I.; Harvey, I.; Beauchemin, M.; Harel, F.; Plante, M.; Tetu, B. Role of Immunohistochemical Overexpression of Matrix Metalloproteinases MMP-2 and MMP-11 in the Prognosis of Death by Ovarian Cancer. Am. J. Clin. Pathol. 2008, 129, 226–231. [Google Scholar] [CrossRef]
- Davies, B.; Miles, D.W.; Happerfield, L.C.; Naylor, M.S.; Bobrow, L.G.; Rubens, R.D.; Balkwill, F.R. Activity of type IV collagenases in benign and malignant breast disease. Br. J. Cancer. 1993, 67, 1126–1131. [Google Scholar] [CrossRef]
- Iwata, H.; Kobayashi, S.; Iwase, H.; Masaoka, A.; Fujimoto, N.; Okada, Y. Production of Matrix Metalloproteinases and Tissue Inhibitors of Metalloproteinases in Human Breast Carcinomas. Jpn. J. Cancer Res. 1996, 87, 602–611. [Google Scholar] [CrossRef]
- Talvensaari-Mattila, A.; Paakko, P.; Turpeenniemi-Hujanen, T. Matrix Metalloproteinase-2 (MMP-2) is associated with survival in breast carcinoma. Br. J. Cancer 2003, 89, 1270–1275. [Google Scholar] [CrossRef]
- Morgia, G.; Falsaperla, M.; Malaponte, G.; Madonia, M.; Indelicato, M.; Travali, S.; Mazzarino, M.C. Matrix metalloproteinases as diagnostic (MMP-13) and prognostic (MMP-2, MMP-9) markers of prostate cancer. Urol. Res. 2005, 33, 44–50. [Google Scholar] [CrossRef]
- Gerhards, S.; Jung, K.; Koenig, F.; Daniltchenko, D.; Hauptmann, S.; Schnorr, D.; Loening, S.A. Excretion of matrix metalloproteinases 2 and 9 in urine is associated with a high stage and grade of bladder carcinoma. Urology 2001, 57, 675–679. [Google Scholar] [CrossRef]
- Davies, B.; Jonathan, W.; Harpret, W.; Paul, A.; Gordon, W.; Thomas, K.; David, N.; David, T.; Andrew, H.; Frances, B. Levels of Matrix Metalloproteases in Bladder Cancer Correlate with Tumor Grade and Invasion. Cancer Res. 1993, 53, 5365–5369. [Google Scholar] [PubMed]
- Friedberg, M.H.; Glantz, M.J.; Klempner, M.S.; Cole, B.F.; Perides, G. Specific matrix metalloproteinase profiles in the cerebrospinal fluid correlated with the presence of malignant astrocytomas, brain metastases, and carcinomatous meningitis. Cancer 1998, 82, 923–930. [Google Scholar] [CrossRef]
- Sawaya, R.E.; Yamamoto, M.; Gokaslan, Z.L.; Wang, S.W.; Mohanam, S.; Fuller, G.N.; McCutcheon, I.E.; Stetler-Stevenson, W.G.; Nicolsont, G.L.; Rao, J.S. Expression and localization of 72 kDa type IV collagenase (MMP-2) in human malignant gliomas in vivo. Clin. Exp. Metastasis 1996, 14, 35–42. [Google Scholar] [CrossRef]
- Kodate, M.; Kasai, T.; Hashirnoto, H.; Yasumoto, K.; Iwata, Y.; Manabe, H. Expression of matrix metalloproteinase (gelatinase) in T1 adenocarcinoma of the lung. Pathol. Int. 1997, 47, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Ellenrieder, V.; Alber, B.; Lacher, U.; Hendler, S.F.; Menke, A.; Boeck, W.; Wagner, M.; Wilda, M.; Friess, H.; Büchler, M.; et al. Role of MT-MMPs and MMP-2 in pancreatic cancer progression. Int. J. Cancer 1999, 85, 14–20. [Google Scholar] [CrossRef]
- Väisänen, A.; Kallioinen, M.; Taskinen, P.J.; Turpeenniemi-Hujanen, T. Prognostic value of MMP-2 immunoreactive protein (72 kD type IV collagenase) in primary skin melanoma. J. Pathol. 1998, 186, 51–58. [Google Scholar] [CrossRef]
- Giannelli, G.; Bergamini, C.; Marinosci, F.; Fransvea, E.; Quaranta, M.; Lupo, L.; Schiraldi, O.; Antonaci, S. Clinical role of MMP-2/TIMP-2 imbalance in hepatocellular carcinoma. Int. J. Cancer 2002, 97, 425–431. [Google Scholar] [CrossRef]
- Davidson, B.; Goldberg, I.; Kopolovic, J.; Lerner-Geva, L.; Gotlieb, W.H.; Ben-Baruch, G.; Reich, R. MMP-2 and TIMP-2 Expression Correlates with Poor Prognosis in Cervical Carcinoma—A Clinicopathologic Study Using Immunohistochemistry and mRNA in Situ Hybridization. Gynecol. Oncol. 1999, 73, 372–382. [Google Scholar] [CrossRef]
- Talvensaari-Mattila, A.; Turpeenniemi-Hujanen, T. Levels of Circulating TIMP-2 and MMP2-TIMP2 Complex Are Decreased in Squamous Cervical Carcinoma. Obstet. Gynecol. Int. 2010, 179351. [Google Scholar] [CrossRef]
- Shrestha, B.; Bajracharya, D.; Byatnal, A.A.; Kamath, A.; Radhakrishnan, R. May High MMP-2 and TIMP-2 Expressions Increase or Decrease the Aggressivity of Oral Cancer? Pathol. Oncol. Res. 2017, 23, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Kanayama, H.; Yokota, K.; Kurokawa, Y.; Murakami, Y.; Nishitani, M.; Kagawa, S. Prognostic Values of Matrix Metalloproteinase-2 and Tissue Inhibitor of Metalloproteinase-2 Expression in Bladder Cancer. Cancer 1998, 82, 1359–1366. [Google Scholar] [CrossRef]
- Kamat, A.A.; Fletcher, M.; Gruman, L.M.; Mueller, P.; Lopez, A.; Landen, C.N., Jr.; Han, L.; Gershenson, D.M.; Sood, A.K. The Clinical Relevance of Stromal Matrix Metalloproteinase Expression in Ovarian Cancer. Clin. Cancer Res. 2006, 12, 1707–1714. [Google Scholar] [CrossRef]
- Lengyel, E.; Schmalfeldt, B.; Konik, E.; Spathe, K.; Harting, K.; Fenn, A.; Berger, U.; Fridman, R.; Schmitt, M.; Prechtel, D.; et al. Expression of Latent Matrix Metalloproteinase 9 (MMP-9) Predicts Survival in Advanced Ovarian Cancer. Gynecol. Oncol. 2001, 82, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Sakata, K.; Shigemasa, K.; Nagai, N.; Ohama, K. Expression of matrix metalloproteinases (MMP-2, MMP-9, MT1-MMP) and their inhibitors (TIMP-1, TIMP-2) in common epithelial tumors of the ovary. Int. J. Oncol. 2000, 17, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Nakopoulou, L.; Katsarou, S.; Giannopoulou, I.; Alexandrou, P.; Tsirmpa, I.; Panayotopoulou, E.; Mavrommatis, J.; Keramopoulos, A. Correlation of Tissue Inhibitor of Metalloproteinase-2 with Proliferative Activity and Patients’ Survival in Breast Cancer. Mod. Pathol. 2002, 15, 26–34. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mohanam, S.; Wang, S.W.; Rayford, A.; Yamamoto, M.; Sawaya, R.; Nakajima, M.; Liotta, L.A.; Nicolsont, G.L.; Stetler-Stevenson, W.G.; Rao, J.S. Expression of tissue inhibitors of metalloproteinases: Negative regulators of human glioblastoma invasion in vivo. Clin. Exp. Metastasis 1995, 13, 57–62. [Google Scholar] [CrossRef]
- Pulukuri, S.M.; Patibandla, S.; Patel, J.; Estes, N.; Rao, J.S. Epigenetic Inactivation of the Tissue Inhibitor of Metalloproteinase-2 (TIMP-2) Gene in Human Prostate Tumors. Oncogene 2007, 26, 5229–5237. [Google Scholar] [CrossRef]
- Onisto, M.; Riccio, M.P.; Scanapieco, P.; Caenazzo, C.; Griggio, L.; Spina, M.; Stetler-Stevenson, W.G.; Garbisa, S. Gelatinase A/TIMP-2 Imbalance in lymph-node-positive breast carcinomas, as measured by RT-PCR. Int. J. Cancer 1995, 63, 621–626. [Google Scholar] [CrossRef]
- Miao, S.; Zhou, S.Y.; Han, C.S.; Zhang, L.N.; Sun, H.B.; Yang, B. Clinicopathological significance of matrix metalloproteinase-7 protein expression in esophageal cancer: A meta-analysis. Drug Des. Devel. Ther. 2015, 9, 3729–3740. [Google Scholar] [CrossRef]
- Okayama, H.; Kumamoto, K.; Saitou, K.; Hayase, S.; Kofunato, Y.; Sato, Y.; Miyamoto, K.; Nakamura, I.; Ohki, S.; Sekikawa, K.; et al. CD44v6, MMP-7 and nuclear Cdx2 are significant biomarkers for prediction of lymph node metastasis in primary gastric cancer. Oncol. Rep. 2009, 22, 745–755. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yamashita, K.; Azumano, I.; Mai, M.; Okada, Y. Expression and tissue localization of matrix metalloproteinase 7 (matrilysin) in human gastric carcinomas. Implications for vessel invasion and metastasis. Int. J. Cancer (Pred. Oncol.) 1998, 79, 187–194. [Google Scholar] [CrossRef]
- Maurel, J.; Nadal, C.; Garcia-Albeniz, X.; Gallego, R.; Carcereny, E.; Almendro, V.; Mármol, M.; Gallardo, E.; Augé, J.M.; Longarón, R.; et al. Serum matrix metalloproteinase 7 levels identifies poor prognosis advanced colorectal cancer patients. Int. J. Cancer 2007, 121, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- Polistena, A.; Cucina, A.; Dinicola, S.; Stene, C.; Cavallaro, G.; Ciardi, A.; Orlando, G.; Arena, R.; D’ermo, G.; Cavallaro, A.; et al. MMP7 Expression in Colorectal Tumours of Different Stages. In Vivo 2014, 28, 105–110. [Google Scholar] [PubMed]
- Yamamoto, H.; Itoh, F.; Iku, S.; Adachi, Y.; Fukushima, H.; Sasaki, S.; Mukaiya, M.; Hirata, K.; Imai, K. Expression of matrix metalloproteinases and tissue inhibitors of metalloproteinases in human pancreatic adenocarcinomas: Clinicopathologic and prognostic significance of matrilysin expression. J. Clin. Oncol. 2001, 19, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.E.; Humphreys, M.J.; Campbell, F.; Neoptolemos, J.P.; Boyd, M.T. Comprehensive analysis of matrix metalloproteinase and tissue inhibitor expression in pancreatic cancer: Increased expression of matrix metalloproteinase-7 predicts poor survival. Clin. Cancer Res. 2004, 10, 2832–2845. [Google Scholar] [CrossRef]
- Kuhlmann, K.F.D.; Olivier van Till, J.W.; Boermeester, M.A.; de Reuver, P.R.; Tzvetanova, I.D.; Offerhaus, G.J.A.; ten Kate, F.J.W.; Busch, O.R.C.; van Gulik, T.M.; Gouma, D.J.; et al. Evaluation of Matrix Metalloproteinase 7 in Plasma and Pancreatic Juice as a Biomarker for Pancreatic Cancer. Cancer Epidemiol. Biomark. Prev. 2007, 16, 886–891. [Google Scholar] [CrossRef][Green Version]
- Tanimoto, H.; Underwood, L.J.; Shigemasa, K.; Parmley, T.H.; Wang, Y.; Yan, Y.; Clarke, J.; O’Brien, T.J. The Matrix Metalloprotease Pump-1 (MMP-7, Matrilysin): A Candidate Marker/Target for Ovarian Cancer Detection and Treatment. Tumor Biol. 1999, 20, 88–98. [Google Scholar] [CrossRef]
- Liu, D.; Nakano, J.; Ishikawa, S.; Yokomise, H.; Ueno, M.; Kadota, K.; Urushihara, M.; Huang, C.L. Overexpression of matrix metalloproteinase-7 (MMP-7) correlates with tumor proliferation, and a poor prognosis in non-small cell lung cancer. Lung Cancer 2007, 58, 384–391. [Google Scholar] [CrossRef]
- Szarvas, T.; Becker, M.; Vom Dorp, F.; Gethmann, C.; Tötsch, M.; Bánkfalvi, A.; Schmid, K.W.; Romics, I.; Rübben, H.; Ergün, S. Matrix metalloproteinase-7 as a marker of metastasis and predictor of poor survival in bladder cancer. Cancer Sci. 2010, 101, 1300–1308. [Google Scholar] [CrossRef]
- Lynch, C.C.; Hikosaka, A.; Acuff, H.B.; Martin, M.D.; Kawai, N.; Singh, R.K.; Vargo-Gogola, T.C.; Begtrup, J.L.; Peterson, T.E.; Fingleton, B.; et al. MMP-7 promotes prostate cancer-induced osteolysis via the solubilization of RANKL. Cancer Cell 2005, 7, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Kuittinen, O.; Savolainen, E.R.; Koistinen, P.; Möttönen, M.; Turpeenniemi-Hujanen, T. MMP-2 and MMP-9 expression in adult and childhood acute lymphatic leukemia (ALL). Leukemia Res. 2001, 25, 125–131. [Google Scholar] [CrossRef]
- Sawicki, G.; Matsuzaki, A.; Janowska-Wieczorek, A. Expression of the active form of MMP-2 on the surface of leukemic cells accounts for their in vitro invasion. J. Cancer Res. Clin. Oncol. 1998, 124, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Zhang, C.; Chen, R.; Pan, J.; Wang, Y.; Ming, M.; Gui, W.; Wang, D. Clinical implications and prognostic value of EMMPRIN/CD147 and MMP2 expression in pediatric gliomas. Eur. J. Pediatr. 2009, 168, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Onisto, M.; Slongo, M.L.; Gregnanin, L.; Gastaldi, T.; Carli, M.; Rosolen, A. Expression and activity of vascular endothelial growth factor and metalloproteinases in alveolar and embryonal rhabdomyosarcoma cell lines. Int. J. Oncol. 2005, 27, 791–798. [Google Scholar] [PubMed]
- Diomedi-Camassei, F.; Boldrini, R.; Ravà, L.; Donfrancesco, A.; Boglino, C.; Messina, E.; Dominici, C.; Callea, F. Different pattern of matrix metalloproteinases expression in alveolar versus embryonal rhabdomyosarcoma. J. Pediatr. Surg. 2004, 39, 1673–1679. [Google Scholar] [CrossRef] [PubMed]
- Bjørnland, K.; Flatmark, K.; Pettersen, S.; Aaasen, A.O.; Fodstad, O.; Maelandsmo, G.M. Matrix metalloproteinases participate in osteosarcoma invasion. J. Surg. Res. 2005, 127, 151–156. [Google Scholar] [CrossRef]
- Pennanen, H.; Kuittinen, O.; Turpeenniemi-Hujanen, T. Plasma MMP-2-TIMP-2 complex levels measured during follow-up predict a risk of relapse in patients with malignant lymphoma. Eur. J. Haematol. 2008, 80, 46–54. [Google Scholar] [CrossRef]
- Ara, T.; Fukuzawa, M.; Kusafuka, T.; Komoto, Y.; Oue, T.; Inoue, M.; Okada, A. Immunohistochemical expression of MMP-2, MMP-9, and TIMP-2 in neuroblastoma: Association with tumor progression and clinical outcome. J. Pediatr. Surg. 1998, 33, 1272–1278. [Google Scholar] [CrossRef]
- Ara, T.; Fukuzawa, M.; Kusafuka, T.; Komoto, Y.; Oue, T.; Inoue, M.; Okada, A. Determination of imbalance between MMP-2 and TIMP-2 in human neuroblastoma by reverse-transcription polymerase chain reaction and its correlation with tumor progression. J. Pediatr. Surg. 2000, 35, 432–437. [Google Scholar] [CrossRef]
- Sugiura, Y.; Shimada, H.; Seeger, R.C.; Laug, W.E.; DeClerck, Y.A. Matrix Metalloproteinases-2 and -9 Are Expressed in Human Neuroblastoma: Contribution of Stromal Cells to Their Production and Correlation with Metastasis. Cancer Res. 1998, 58, 2209–2216. [Google Scholar]
- Ribatti, D.; Marimpietri, D.; Pastorino, F.; Brignole, C.; Nico, B.; Vacca, A.; Ponzoni, M. Angiogenesis in neuroblastoma. Ann. NY Acad. Sci. 2004, 1028, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Adithi, M.; Nalini, V.; Kandalam, M.; Krishnakumar, S. Expression of matrix metalloproteinases and their inhibitors in retinoblastoma. J. Pediatr. Hematol. Oncol. 2007, 29, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Webb, A.H.; Gao, B.T.; Goldsmith, Z.K.; Irvine, A.S.; Saleh, N.; Lee, R.P.; Lendermon, J.B.; Bheemreddy, R.; Zhang, Q.; Brennan, R.C.; et al. Inhibition of MMP-2 and MMP-9 decreases cellular migration, and angiogenesis in in vitro models of retinoblastoma. BMC Cancer 2017, 17, 1–11. [Google Scholar] [CrossRef]
- De Veas, R.G.; Schweigerer, L.; Medina, M.A. Matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-2 expression in paediatric tumour cells. Effects of tumour cell proliferation modulators on gelatinolytic activity. J. Cancer Res. Clin. Oncol. 1995, 121, 275–278. [Google Scholar] [CrossRef]
- Stolarska, M.; Sałacińska-Łoś, E.; Taran, K.; Trelińska, J.; Kobos, J. Estimation og diagnostic value of TIMP-2 expression in chosen childhood lymphomas and reactive lymphadenopathy. Acta Haematol. Pol. 2008, 39, 477–484. [Google Scholar]
- Pennanen, H.; Kuittinen, O.; Soini, Y.; Turpeenniemi-Hujanen, T. Clinicopathological correlations of TIMP-1 and TIMP-2 in Hodgkin’s lymphoma. Eur. J. Haematol. 2004, 72, 1–9. [Google Scholar] [CrossRef]
- Lynch, C.C.; McDonnell, S. The role of matrilysin (MMP-7) in leukaemia cell invasion. Clin. Exp. Metastasis 2000, 18, 401–406. [Google Scholar] [CrossRef]
- Klein, G.; Vellenga, E.; Fraaije, M.W.; Kamps, W.A.; de Bont, E.S.J.M. The possible role of matrix metalloproteinase (MMP)-2 and MMP-9 in cancer, e.g., acute leukemia. Crit. Rev. Oncol. Hemat. 2004, 50, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Hsu, P.C.; Pei, J.S.; Chen, C.C.; Chang, W.S.; Kuo, C.C.; Cheng, S.P.; Tsai, C.W.; Bau, D.T.; Gong, C.L. Association of Matrix Metallopeptidase-2 Promoter Polymorphisms With the Risk of Childhood Leukemia. Anticancer Res. 2019, 39, 1185–1190. [Google Scholar] [CrossRef]
- Pei, J.S.; Chou, A.K.; Hsu, P.C.; Tsai, C.W.; Chang, W.S.; Wu, M.F.; Wu, M.H.; Hsia, T.C.; Cheng, S.P.; Bau, D.T. Contribution of Matrix Metalloproteinase-7 Genotypes to the Risk of Non-solid Tumor, Childhood Leukemia. Anticancer Res. 2017, 37, 6679–6684. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sakakibara, M.; Koizumi, S.; Saikawa, Y.; Wada, H.; Ichihara, T.; Sato, H.; Horita, S.; Mugishima, H.; Kaneko, Y.; Koike, K. Membrane-Type Matrix Metalloproteinase-1 Expression and Activation of Gelatinase A as Prognostic Markers in Advanced Pediatric Neuroblastoma. Cancer 1999, 85, 231–239. [Google Scholar] [CrossRef]
- Roomi, M.W.; Kalinovsky, T.; Rath, M.; Niedzwiecki, A. In vitro modulation of MMP-2 and MMP-9 in pediatric human sarcoma cell lines by cytokines, inducers and inhibitors. Int. J. Oncol. 2014, 44, 27–34. [Google Scholar] [CrossRef] [PubMed]
| Collagenases | Gelatinases | Stromelysins | |||
|---|---|---|---|---|---|
| MMP-1 | Collagenase-1 Interstitial collagenase | MMP-2 | Gelatinase A 72-kDa type IV collagenase | MMP-3 | Stromelysin-1 |
| MMP-8 | Collagenase-2 Neutrophil collagenase | MMP-9 | Gelatinase B | MMP-10 | Stromelysin-2 |
| MMP-13 | Collagenase-3 | MMP-11 | Stromelysin-3 | ||
| Matrilysins | Membrane-Type MMPs | Other MMPs | |||
| MMP-7 | Matrilysin | MMP-14 | Membrane type-1 MMP | MMP-12 | Macrophage metallo-elastase |
| MMP-26 | Matrilysin-2/endometase | MMP-15 | Membrane type-2 MMP | MMP-20 | Enamelysin |
| MMP-16 | Membrane type-3 MMP | MMP-28 | Epilysin | ||
| MMP-17 | Membrane type-4 MMP | ||||
| MMP-24 | Membrane type-5 MMP | ||||
| MMP-25 | Membrane type-6 MMP | ||||
| MMP/TIMP | Type of the Cancer | Type of the Sample | Main Findings | References |
|---|---|---|---|---|
| MMP-2 | Colorectal cancer | Tumor tissue Plasma | Increased concentration of MMP-2 in tumor tissue, compared with tumor-free tissue MMP-2 plasma level was distinctly elevated in patients with lymph node metastasis compared with those without | Langenskiold et al. [44] |
| Tumor tissue | High expression of MMP-2 in cancer cells was associated with decreased survival of colon cancer patients | Hilska et al. [45] | ||
| Ovarian cancer | Tumor tissue | Significant relationship between activated MMP-2 and invasiveness, metastasis, disease progression; MMP-2 as a potential marker of prognosis | Wu et al. [46] | |
| Ovarian tumors /peritoneal implants | MMP-2 overexpression by cancer cells in peritoneal implants and not in the primary ovarian cancer is predictive of ovarian cancer prognosis | Peringy et al. [47] | ||
| Breast cancer | Tumor tissue | The ratio of active to total MMP-2 was increased in high-grade tumors | Davies et al. [48] | |
| Tumor tissue | Activation of pro-MMP-2 may be an indicator of lymph node metastasis in breast cancer | Iwata et al. [49] | ||
| Tumor tissue | Decreased MMP-2 concentration could serve as a marker for favorable prognosis in breast cancer | Talvensaari-Mattila et al. [50] | ||
| Prostate cancer | Plasma | The level of MMP-2 increased in patients with metastatic prostate cancer compared to BPH/healthy patients | Morgia et al. [51] | |
| Bladder cancer | Urine | Urinary excretion of MMP-2 is associated with higher stage and grade; it may indicate tumor progression and predict relapse of the disease | Gerhards et al. [52] | |
| Tumor tissue | Levels of active MMP-2 increased with tumor grade and invasiveness | Davies et al. [53] | ||
| Central nervous system malignancies | CSF | All patients with positive CSF cytologies had activated MMP-2 | Friedberg et al. [54] | |
| Tumor tissue | Expression of MMP-2 significantly upregulated in malignant gliomas and correlated with progression of human gliomas | Sawaya et al. [55] | ||
| Lung adenocarcinoma | Tumor tissue | MMP-2 positive patients had poorer prognosis | Kodate et al. [56] | |
| Pancreas cancer | Tumor tissue | MMP-2 plays an important role in tumor cell invasion and leads to progression of the disease | Ellenrieder et al [57]. | |
| Primary skin melanoma | Tumor tissue | MMP-2 positive patients had poorer prognosis | Vaisanen et al. [58] | |
| MMP-2/TIMP-2 | HCC | Serum + tumor tissue | MMP-2/TIMP-2 imbalance (and particularly TIMP-2 levels), could become a valuable prognostic factor in patients with HCC | Gianelli et al. [59] |
| Cervical carcinoma | Tumor tissue | Presence of mRNA for both MMP-2 and TIMP-2 is associated with poor survival | Davidson et al. [60] | |
| Serum | Medium level of TIMP-2 and MMP-2/TIMP-2 complex in serum is higher in healthy women, compared to those with a malignant tumor | Talvensaari-Mattila et al. [61] | ||
| Oral cancer | Tumor tissue | A rate of MMP-2/TIMP-2 complex expression is better for characterization of MMP-2 activity | Shretsha et al. [62] | |
| Bladder cancer | Tumor tissue | The expression of MMP-2 and TIMP-2 was higher in invasive tumors, and was strongly associated with poorer survival | Kanayama et al [63]. |
| Type of Cancer | Type of Sample | Result | Study |
|---|---|---|---|
| Esophageal cancer | Tumor tissue | Overexpression of MMP-7 is strictly connected with higher TNM stage, higher invasive grade, presence of lymph nodes metastasis | Miao et al. (meta-analysis) [71] |
| Gastric cancer | Tumor tissue | Overexpression of MMP-7 predicts presence of lymph node metastasis | Okayama et al. [72] |
| Tumor tissue | MMP-7 levels are higher in gastric cancer with vascular invasion compared to the group without invasion | Yamashita et al. [73] | |
| Colorectal cancer | Serum | MMP-7 is an independent prognostic factor for survival in advanced colorectal cancer, possibly even more accurate than LDH | Maurel et al. [74] |
| Serum + Tumor tissue | Overexpression of MMP-7 in advanced cancer, compared to non-metastatic disease Higher level of MMP-7 in serum of stage III/IV patients, compared to patients in I/II stage disease | Polistena et al. [75] | |
| Pancreatic cancer | Tumor tissue | MMP-7 positivity was correlated with poor prognosis | Yamamoto et al. [76] |
| Tumor tissue | MMP-7 level was significantly increased in pancreatic cancer compared with healthy pancreas, and was related with reduced survival | Jones et al. [77] | |
| Plasma + Pancreatic juice | Median plasma MMP-7 levels were significantly higher in carcinoma, compared with chronic pancreatitis Combined MMP-7 and Ca 19-9 levels in plasma give positive predictive value of 100% | Kuhlmann et al. [78] | |
| Ovarian cancer | Tumor tissue | Overexpression of MMP-7 in high-grade ovarian cancer and low malignant potential ovarian tumors; absence of MMP-7 expression in healthy ovary | Tanimoto et al. [79] |
| NSCLC | Tumor tissue | Overall survival significantly lower in patients with overexpression of MMP-7 | Liu et al. [80] |
| Bladder cancer | Tumor tissue + serum | Overexpression of MMP-7 in tissue samples of metastatic bladder cancer, compared to those with localized disease High tissue expression levels are accompanied by elevated serum MMP-7 concentration | Szarvas et al. [81] |
| MMP/TIMP | Type of Cancer | Type of Sample | Result | Study |
|---|---|---|---|---|
| MMP-2 | Acute lymphoblastic leukemia | bone marrow | In pediatric cases positive MMP-2 expression was in relationship with high-risk tumor group and T-cell immunophenotype | Kuittinen et al. [83] |
| Acute myelogenous leukemia | adult cell-lines | Inhibiting the activity of MMP-2 significantly reduced invasiveness of leukemic cells | Sawicki et al. [84] | |
| Central nervous system tumors | tumor tissue | Distinctly positive expression of MMP-2 in anaplastic astrocytoma and glioblastoma compared with healthy brain and low-grade astrocytoma tissue | Gu et al. [85] | |
| Alveolar (ARMS) and embryonal (ERMS) rhabdomyosarcoma | ARMS and ERMS cell lines | ARMS cell line with increased expression of MMP-2 was more invasive compared to ERMS cell line with low levels of MMP-2. | Onisto et al. [86] | |
| ARMS and ERMS tumor samples | ARMS showed stronger MMP-2 expression, compared with ERMS type | Diomedi-Camassei et al. [87] | ||
| Osteosarcoma | cell lines | The most invasive cell line contained the highest amounts of MMP-2 | Bjorland et al. [88] | |
| MMP-2/TIMP-2 | Lymphomas | Plasma | Newly diagnosed lymphoma patients had higher levels of MMP-2/TIMP-2 complex and lower levels of TIMP-2, compared to healthy individuals Patients with highest plasma levels of MMP-2/TIMP-2 complex had a greater chance for relapse of the disease | Pennanen et al. [89] |
| Neuroblastoma | Tumor tissue | Higher levels of MMP-2 mRNA and the ratio of MMP-2/TIMP-2 mRNA were observed in advanced stages and in patients who died from the progression of the disease | Ara et al. [90,91] | |
| Tumor tissue | Higher levels of MMP-2 in stage IV compared to stage I and II | Sugiura et al. [92] | ||
| Tumor tissue | Expression of MMP-2 was increased in advanced stages of the disease | Ribatti et al. [93] | ||
| Retinoblastoma (RB) | Tumor tissue | MMP-2 and TIMP-2 were overexpressed in invasive tumors | Adithi et al. [94] | |
| Cell lines | Higher expression of MMP-2 in poorly differentiated RB compared with moderately/well-differentiated RB Using inhibitors of MMP-2 and MMP-9 results in reduction in cell line migration ability, and significant decrease of cell viability | Webb et al. [95] | ||
| Neuroblastoma RhabdomyosarcomaOsteosarcoma | Cell lines | In neuroblastoma in more aggressive cell lines, MMP-2 expression was twice as high as in less aggressive cells The highest level of MMP-2 was determined for osteosarcoma cell line In neuroblastoma, TIMP-2 was overexpressed in less aggressive line, compared with expression in more aggressive cell line | De Veas et al. [96] | |
| TIMP-2 | Lymphomas | Tumor tissue | TIMP-2 expression exclusively in lymphomas, none in reactive lymph nodes | Stolarska et al. [97] |
| Hodgkin lymphoma | Tumor tissue | TIMP-2 expression correlate with systemic symptoms | Pennanen et al. [98] | |
| MMP-7 | Acute myelogenous leukemia | Cell lines | Only more aggressive cells expressed MMP-7 By inhibiting MMP-7 40% reduction of invasiveness was revealed | Lynch et al. [99] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaczorowska, A.; Miękus, N.; Stefanowicz, J.; Adamkiewicz-Drożyńska, E. Selected Matrix Metalloproteinases (MMP-2, MMP-7) and Their Inhibitor (TIMP-2) in Adult and Pediatric Cancer. Diagnostics 2020, 10, 547. https://doi.org/10.3390/diagnostics10080547
Kaczorowska A, Miękus N, Stefanowicz J, Adamkiewicz-Drożyńska E. Selected Matrix Metalloproteinases (MMP-2, MMP-7) and Their Inhibitor (TIMP-2) in Adult and Pediatric Cancer. Diagnostics. 2020; 10(8):547. https://doi.org/10.3390/diagnostics10080547
Chicago/Turabian StyleKaczorowska, Aleksandra, Natalia Miękus, Joanna Stefanowicz, and Elżbieta Adamkiewicz-Drożyńska. 2020. "Selected Matrix Metalloproteinases (MMP-2, MMP-7) and Their Inhibitor (TIMP-2) in Adult and Pediatric Cancer" Diagnostics 10, no. 8: 547. https://doi.org/10.3390/diagnostics10080547
APA StyleKaczorowska, A., Miękus, N., Stefanowicz, J., & Adamkiewicz-Drożyńska, E. (2020). Selected Matrix Metalloproteinases (MMP-2, MMP-7) and Their Inhibitor (TIMP-2) in Adult and Pediatric Cancer. Diagnostics, 10(8), 547. https://doi.org/10.3390/diagnostics10080547





