Frequency and Clinical Review of the Aberrant Obturator Artery: A Cadaveric Study
Abstract
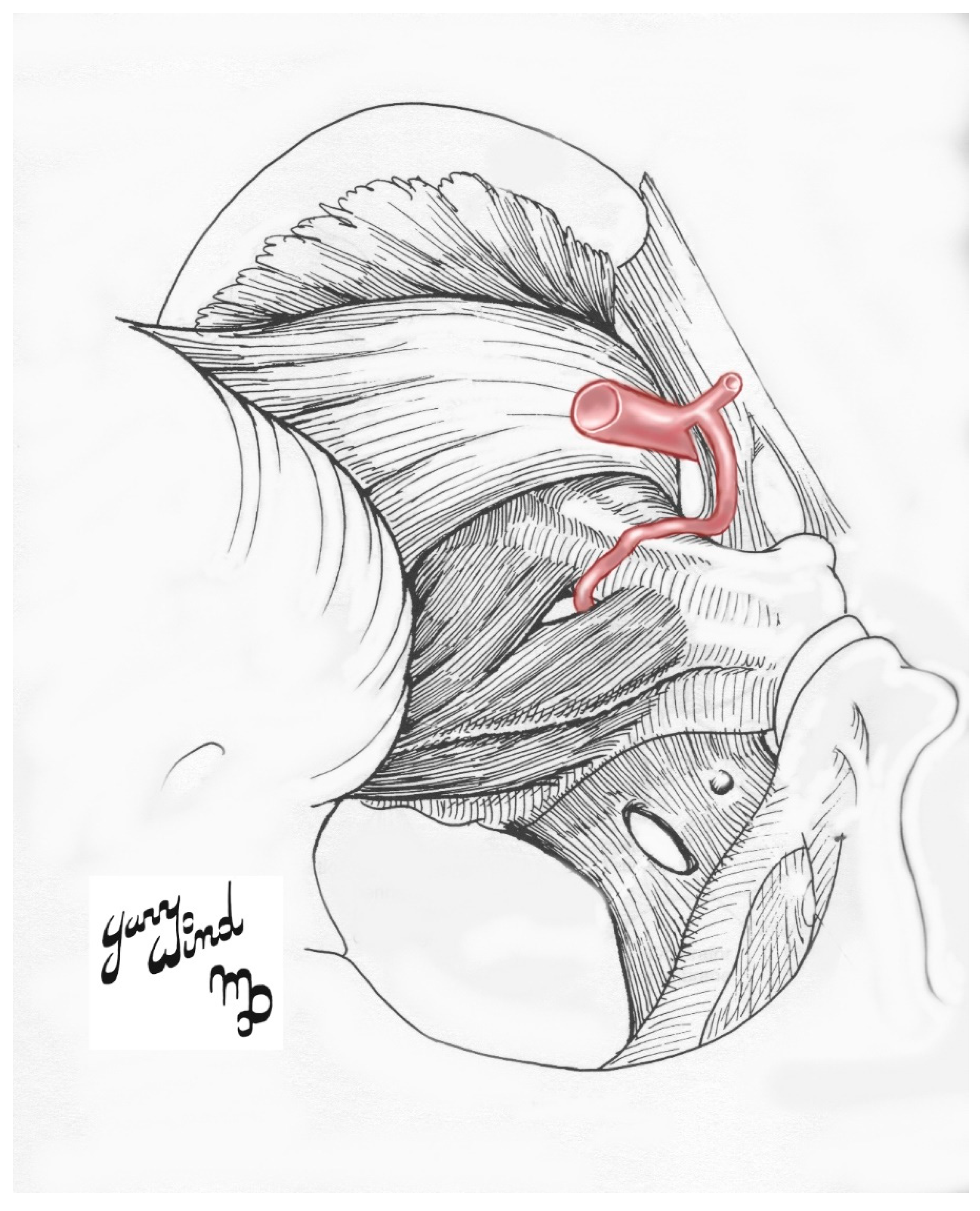
1. Introduction
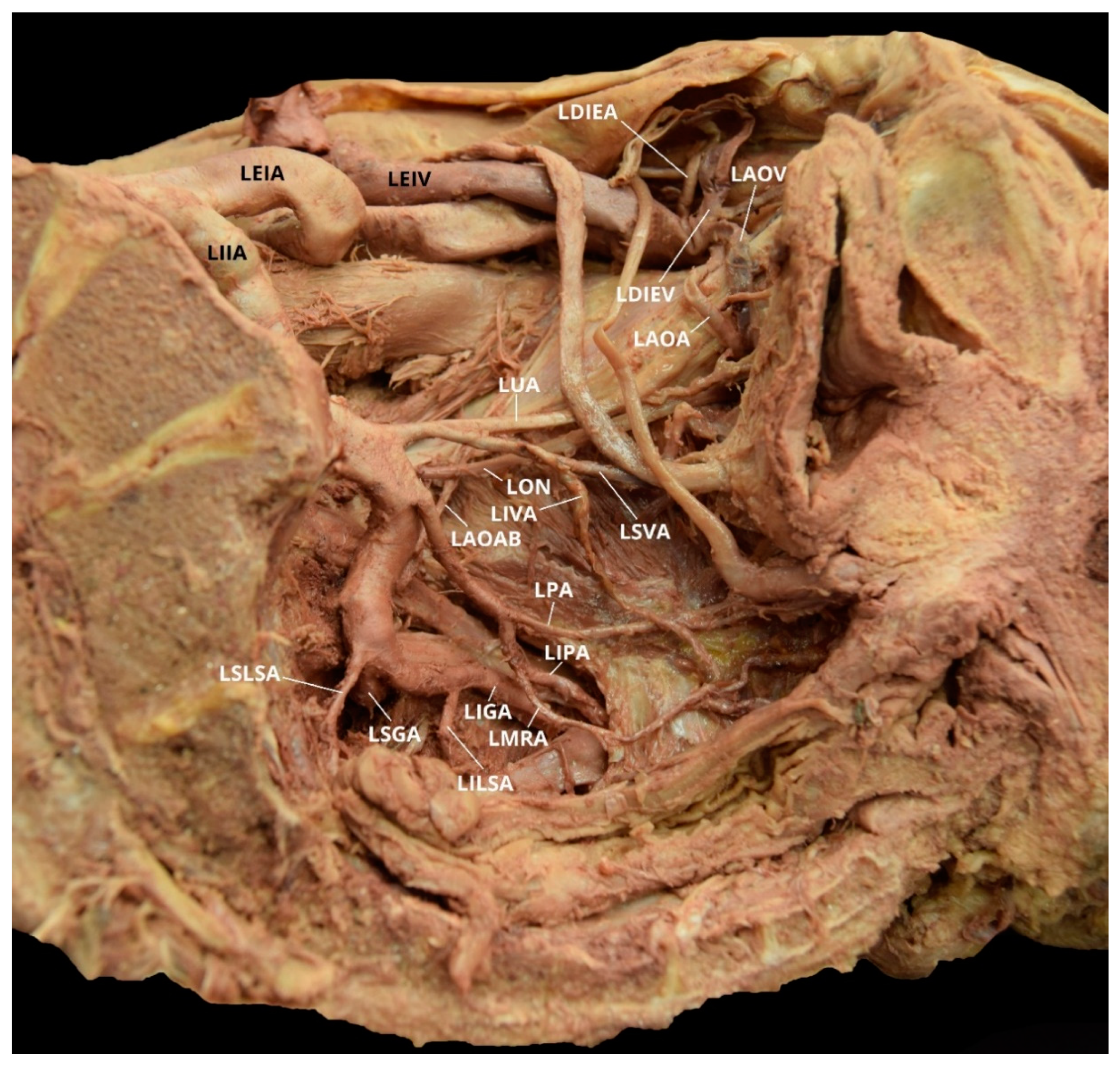
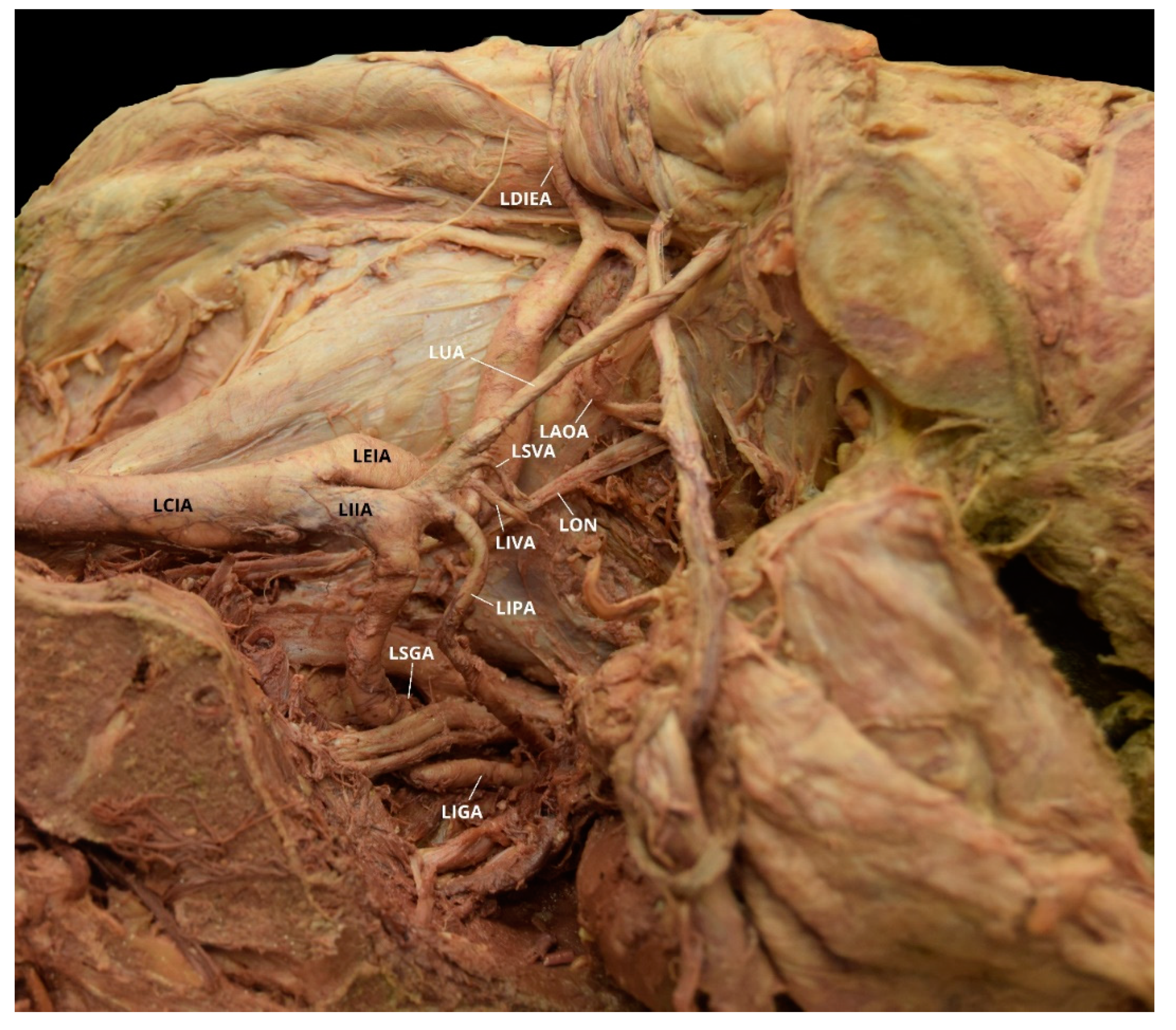
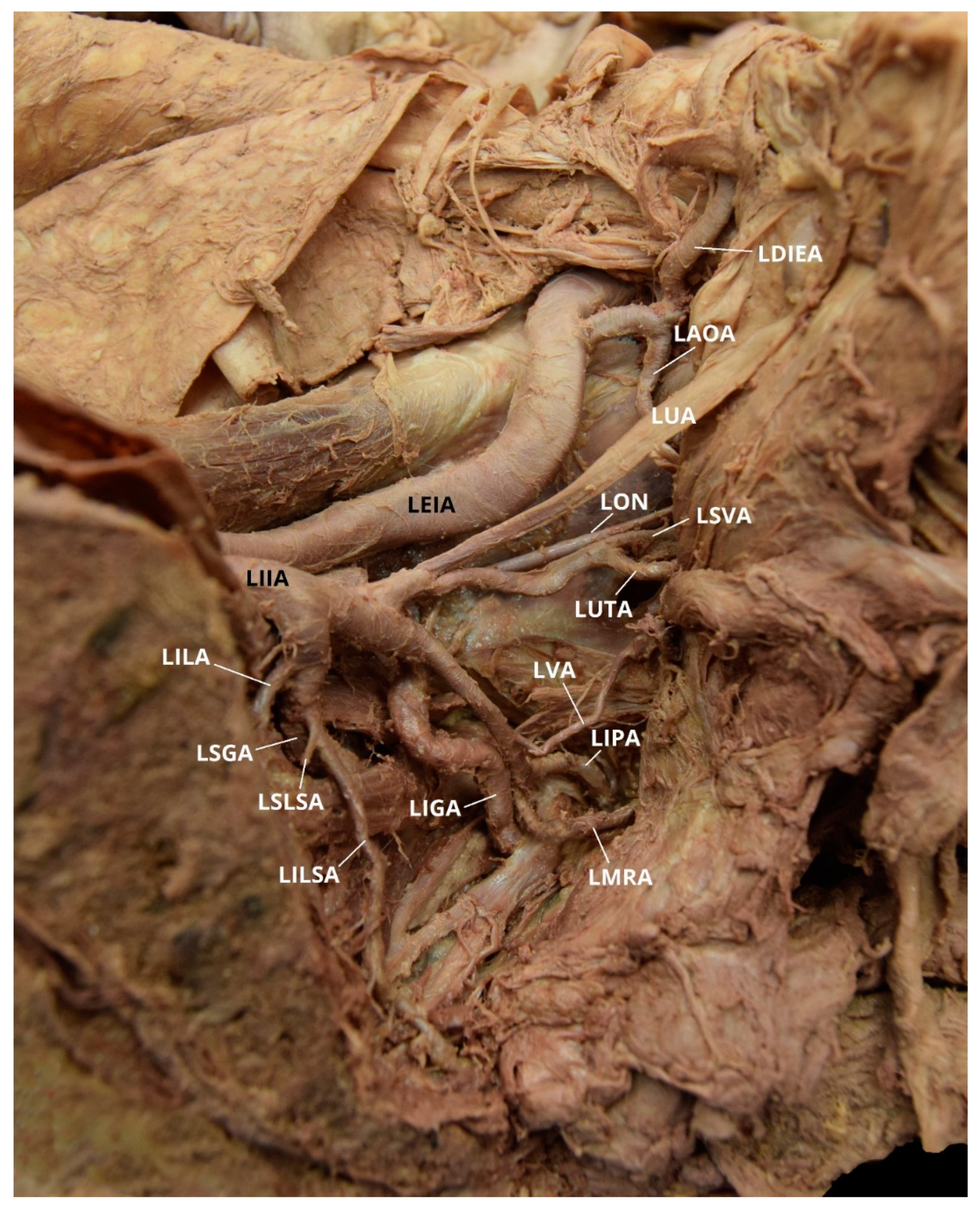
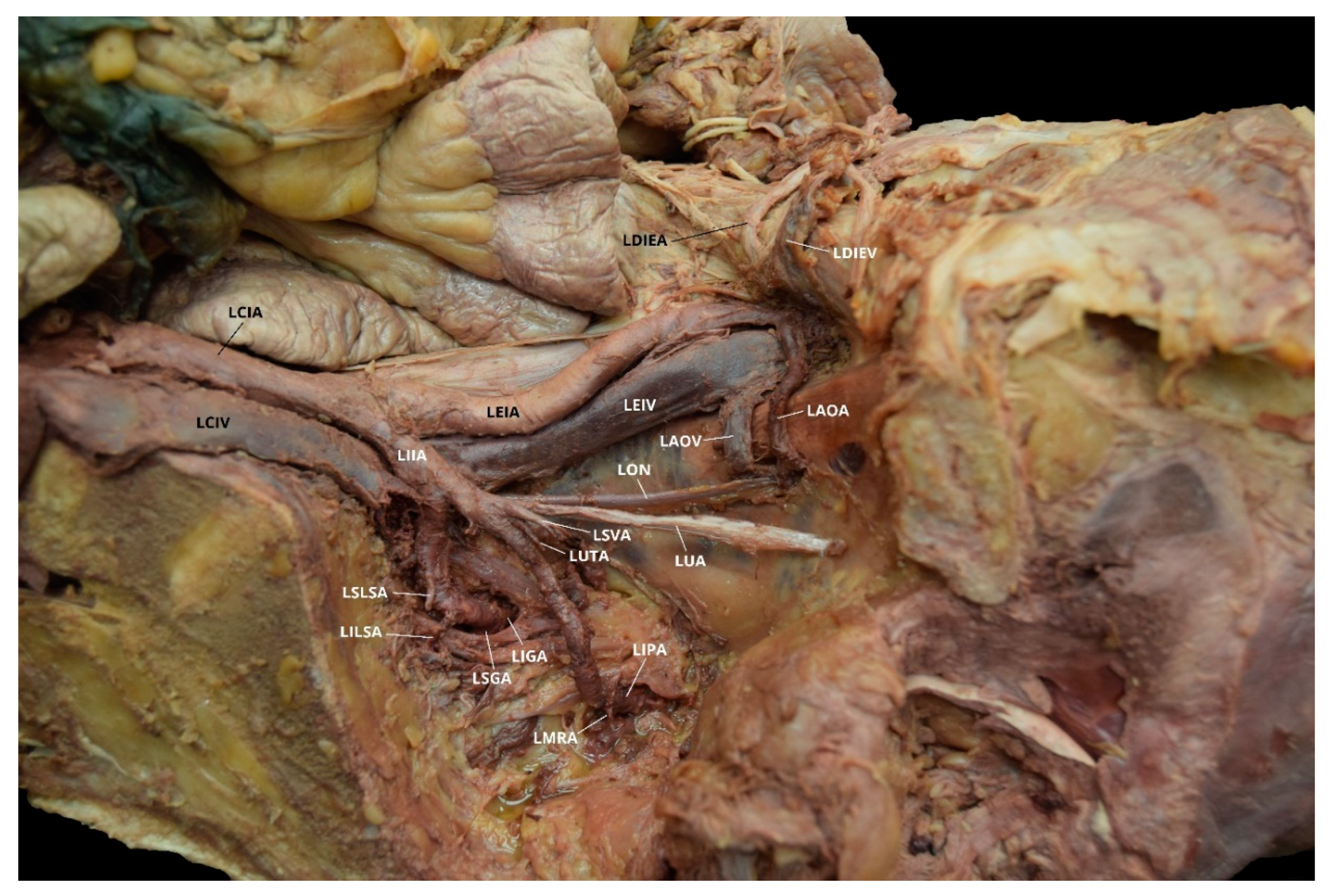
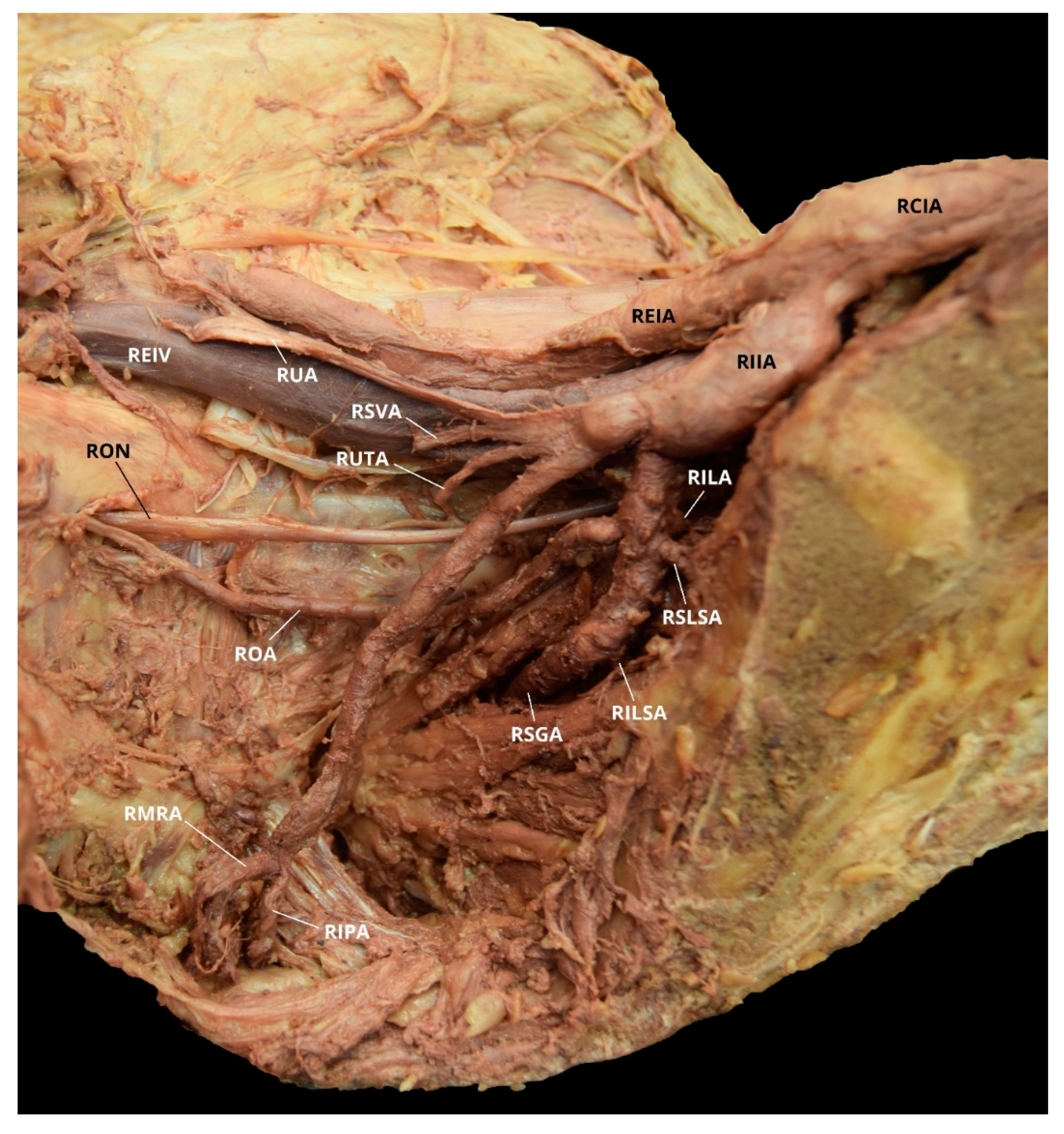
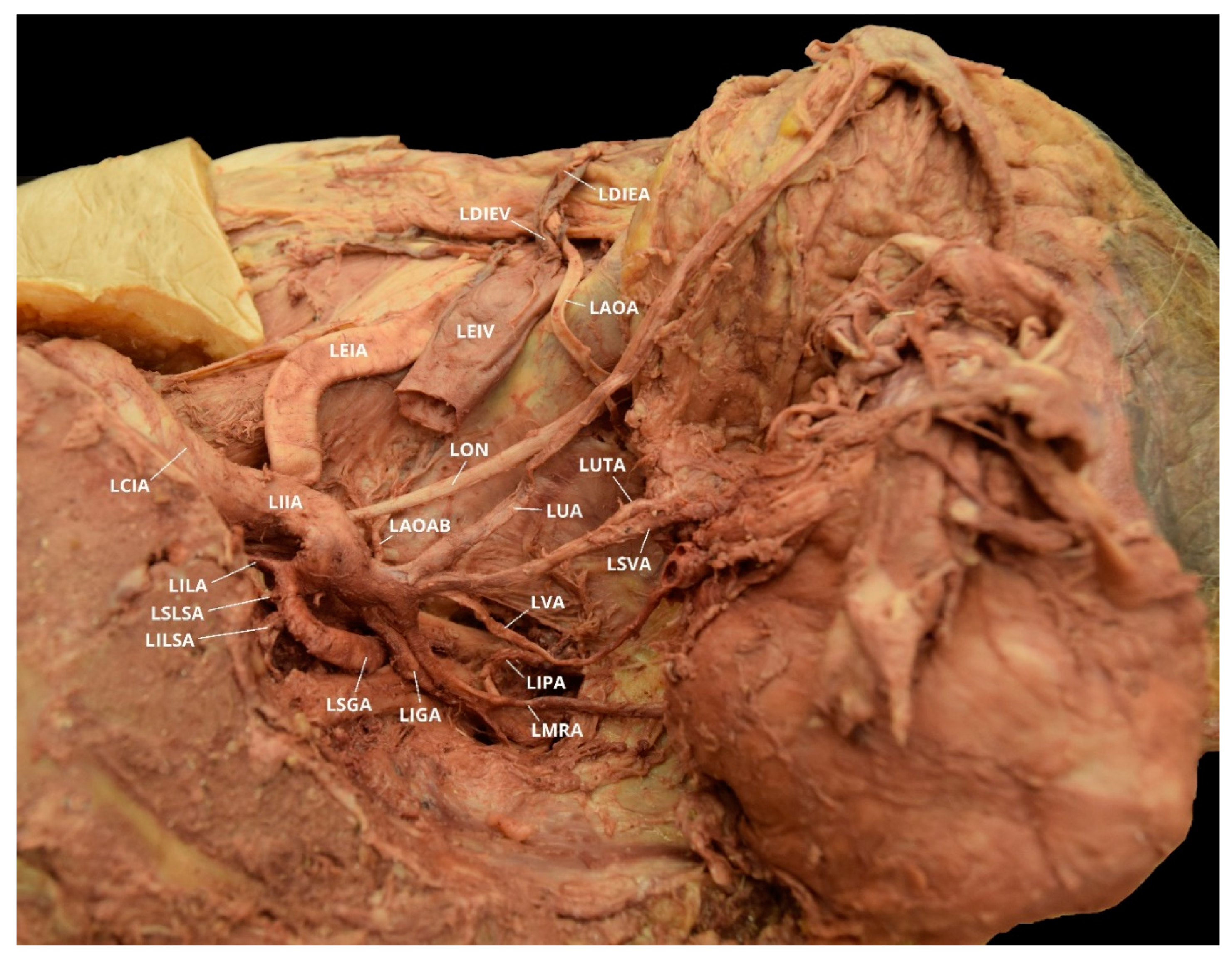
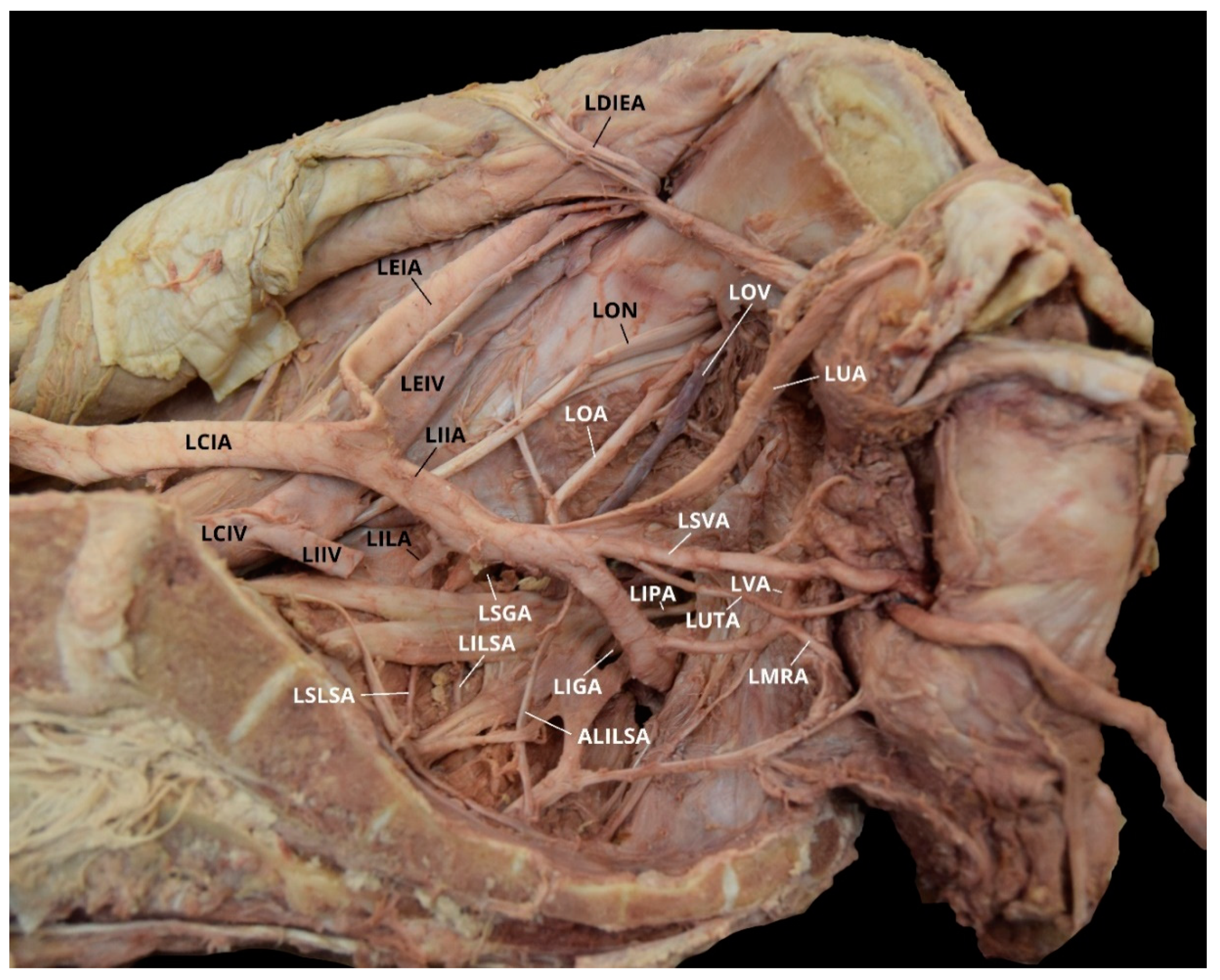
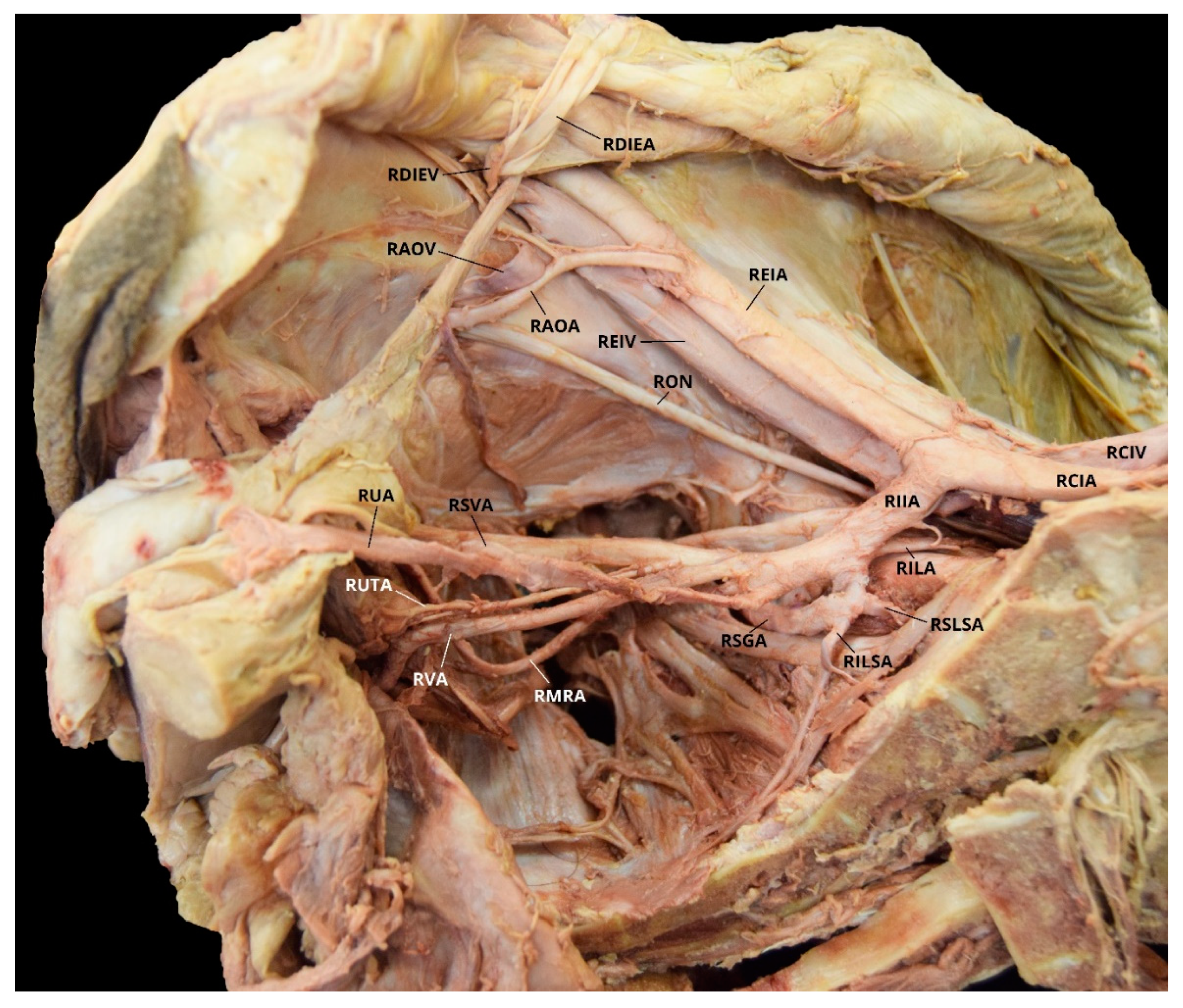
2. Case Descriptions
3. Discussion
3.1. Obturator Artery
3.2. Aberrant Obturator Artery
3.3. Embryonic Development
3.4. Clinical Significance
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Bilhim, T.; Pereira, J.A.; Fernandes, L.; Tinto, H.R.; Pisco, J.M. Angiographic Anatomy of the Male Pelvic Arteries. Am. J. Roentgenol. 2014, 203, 373–382. [Google Scholar] [CrossRef]
- Bergman, R.A.; Thompson, S.A.; Afifi, A.K.; Saadeh, F.A. Compendium of Human Anatomic Variation: Catalog, Atlas and World Literature; Urban and Schwarzenberg: Baltimore, MD, USA, 1988; p. 86. [Google Scholar]
- Lee, E.Y.; Kim, J.Y.; Kim, H.N.; Sohn, H.-J.; Seo, J.H. Variant Origin of Obturator Artery: A Branch of Inferior Epigastric Artery from External Iliac Artery. Korean J. Phys. Anthropol. 2013, 26, 125–130. [Google Scholar] [CrossRef][Green Version]
- Requarth, J.A.; Miller, P.R. Aberrant obturator artery is a common arterial variant that may be a source of unidentified hemorrhage in pelvic fracture patients. J. Trauma. 2011, 70, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Pai, M.M.; Krishnamurthy, A.; Prabhu, L.V.; Pai, M.V.; Kumar, S.A.; Hadimani, G.A. Variability in the origin of the obturator artery. Clin. Sao Paulo 2009, 64, 897–901. [Google Scholar] [CrossRef]
- Kawai, K.; Honma, S.; Koizumi, M.; Kodama, K. Inferior epigastric artery arising from the obturator artery as a terminal branch of the internal iliac artery and consideration of its rare occurrence. Ann. Anat. 2008, 190, 541–548. [Google Scholar] [CrossRef]
- Pick, J.W.; Barry, J.; Anson, B.J.; Ashley, F.L. The origin of the obturator artery: Study of 640 body halves. Am. J. Anat. 1942, 70, 317–343. [Google Scholar] [CrossRef]
- Sañudo, J.; Mirapeix, R.; Rodriguez-Niedenführ, M.; Maranillo, E.; Parkin, I.; Vázquez, T. Obturator artery revisited. Int. Urogynecol. J. 2011, 22, 1313–1318. [Google Scholar] [CrossRef] [PubMed]
- Mamatha, H.; D’Souza, A.S.; Ankolekar, V.; Bangera, H. An anomalous origin of obturator artery: A case report. Indian J. Basic Appl. Med. Res. 2014, 3, 293–295. [Google Scholar]
- Sakthivel; Priyadarshini, S. Variability of origin of obturator artery and its clinical significance. Int. J. Anat. Res. 2015, 3, 1704–1709. [Google Scholar] [CrossRef]
- Sonje, P.D.; Vatsalaswamy, P. Study of Variations in the Origin of Obturator Artery. Indian J. Vasc. Endovasc. Surg. 2016, 131–135. [Google Scholar] [CrossRef]
- Suryavanshi, S.; Bhagel, P.; Sharma, D. Variability in the Origin of the Obturator Artery: A Descriptive Cross-Sectional Cadaveric Study. IJSS J. Surg. 2016, 2, 16–19. [Google Scholar]
- Tunstall, R. Internal iliac arteries. In Bergman’s Comprehensive Encyclopedia of Human Anatomic Variations, 1st ed.; Tubbs, S., Shoja, M.M., Loukas, M., Eds.; John & Wiley & Sons, Inc.: Hoboken, NJ, USA, 2016; pp. 694–721. [Google Scholar]
- Cerda, A. Symmetric Bilateral Aberrant Obturator Artery. A Case Rep. 2016, 34, 1083–1086. [Google Scholar]
- Baena, G.; Rojas, S.; Peña, E. Corona mortis: Anatomical and clinical relevance and occurrence in a sample of the Colombian population. Int. J. Morphol. 2015, 33, 130–136. [Google Scholar] [CrossRef][Green Version]
- Lau, H.; Lee, F. A prospective endoscopic study of retro pubic vascular anatomy in 121 patients undergoing endoscopic extra peritoneal inguinal hernio-plasty. Surg. Endosc. 2003, 17, 1376–1379. [Google Scholar] [CrossRef]
- Daeubler, B.; Anderson, S.; Leunig, M.; Triller, J. Hemorrhage secondary to pelvic fracture: Coil embolization of an aberrant obturator artery. J. Endovasc. Ther. 2003, 10, 676–680. [Google Scholar] [CrossRef]
- Darmanis, S.; Lewis, A.; Mansoor, A.; Bircher, M. Corona mortis: An anatomical study with clinical implications in approaches to the pelvis and acetabulum. Clin. Anat. 2007, 20, 433–439. [Google Scholar] [CrossRef]
- Kashyap, S.; Diwan, Y.; Mahajan, S.; Diwan, D.; Lal, M.; Chauhan, R. The Majority of Corona Mortia Are Small Calibre Venous Blood Vessels: A Cadaveric Study of North Indians. Hip Pelvis 2019, 31, 40–47. [Google Scholar] [CrossRef]
- Astarci, P.; Alexandrescu, V.; Hammer, F.; Elkhoury, G.; Noirhomme, P.; Rubay, J.; Poncelet, A.; Lacroix, V.; Glineur, D.; Verhelst, R. Late Presentation of Bleeding from a Traumatic Obturator Artery Aneurysm, Successfully Treated by Endovascular Means. EJVES Extra 2005, 10, 77–80. [Google Scholar] [CrossRef]
- Biswas, S.; Bandopadhyay, M.; Adhikari, A.; Kundu, P.; Roy, R. Variation of origin of obturator artery in eastern indian population—A study. J. Anat. Soc. India 2010, 59, 168–172. [Google Scholar] [CrossRef]
- Prabaharr, P.S. The incidence of aberrant obturator artery in South Indian population—A cadaveric study. Univ. J. Pre. Paraclin. Sci. 2019, 5, 1–3. [Google Scholar]
- Rajive, A.V.; Pillay, M. A study of variations in the origin of obturator artery and its clinical significance. J. Clin. Diagn. Res. 2015, 9, AC12–AC15. [Google Scholar] [PubMed]
- Smith, J.C.; Gregorius, J.C.; Breazeale, B.H.; Watkins, G.E. The Corona Mortis, a Frequent Vascular Susceptible to Blunt Pelvic Trauma: Identification at Routine Multidetector CT. J. Vasc. Interv. Radiol. 2009, 20, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Tantchev, L.S.; Gorchev, G.A.; Tomov, S.T.; Radionova, Z.V. Aberrant obturator vessels in minimally invasive pelvic lymph node dissection. Gynecol. Surg. 2013, 10, 273–278. [Google Scholar] [CrossRef]
- Yamaki, K.; Saga, T.; Doi, Y.; Aida, K.; Yoshizuka, M. A statistical study of the branching of the human internal iliac artery. Kurume Med. J. 1998, 45, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Al-Talalwah, W.; Al-Hashim, Z.; Al Dorzi, S.; Al Hifzi, H.; Yasky, A.; Al Mousa, H.; Soames, R. The clinical significance of the obturator artery in origin variability. Indian J. Sci. Res. 2016, 7, 61–65. [Google Scholar]
- Dehmukh, V.; Sign, S.; Sirohi, N.; Baruhee, D. Variation in the Obturator Vasculature During Routine Anatomy Dissection of a Cadaver. Sultan Qaboos Univ. Med. J. 2016, 16, e256–e258. [Google Scholar] [CrossRef]
- Goke, K.; Pires, L.A.S.; Leite, T.F.O.; Chagas, C.A.A. Rare origin of the obturator artery from the external iliac artery with two obturator veins. J. Vasc. Bras. 2016, 15, 250–253. [Google Scholar] [CrossRef]
- Parsons, F.G.; Keith, A. Sixth annual report of the Committee of Collective Investigation of the Anatomical Society of Great Britian and Ireland (1895–1896). J. Anat. Physiol. 1897, 31, 31–44. [Google Scholar]
- Braithwaite, J.L. Variations in origin of parietal branches of internal iliac artery. J. Anat. 1952, 86, 423–430. [Google Scholar]
- Leite, T.F.O.; Pires, L.A.S.; Goke, K.; Silva, J.G.; Chagas, C.A.A. Corona Mortis: Anatomical and surgical description on 60 cadaveric hemipelvises. Rev. Col. Bras. Cir. 2017, 44, 553–559. [Google Scholar] [CrossRef]
- Rusu, M.C.; Ilie, A.C.; Brezean, I. Human anatomic variations: Common, external iliac, origin of the obturator, inferior epigastric and medial circumflex femoral arteries, and deep femoral artery course on the medial side of the femoral vessels. Surg. Radiol. Anat. 2017, 39, 1285–1288. [Google Scholar] [CrossRef] [PubMed]
- Jusoh, A.R.; Abd Rahman, N.; Abd Latiff, A.; Othman, F.; Das, S.; Abd Ghafar, N.; Suhaimi, F.H.; Hussan, F.; Sulaiman, I.M. The anomalous origin and branches of the obturator artery with its clinical implications. Rom. J. Morphol. Embryol. 2010, 51, 163–166. [Google Scholar] [PubMed]
- Buchanan, A.M. Manual of Anatomy, Systematic and Practical, Including Embryology; CV Mosby Company: St Louis, MO, USA, 1914; Volume 1, p. 436. [Google Scholar]
- Naguib, N.; Nour-Eldin, N.; Hammerstingl, R.; Lehnert, T.; Floeter, J.; Zangos, S.; Vogl, T.J. Three dimensional reconstructed contrast-enhanced MR angiography for internal iliac artery branch visualization before uterine artery embolization. J. Vasc. Interv. Radiol. 2008, 19, 1569–1575. [Google Scholar] [CrossRef] [PubMed]
- Deaver, J.B. Surgical Anatomy: A Treatise on Human Anatomy in Its Application to the Practice of Medicine and Surgery; P. Blakiston’s Son & Co.: Philadelphia, PA, USA, 1903. [Google Scholar] [CrossRef]
- Nayak, S.B.; Shetty, S.D.; Shetty, P.; Deepthinath, R.; George, B.M.; Mishra, S.; Sirasanagandla, S.R.; Jumar, N.; Abhinitha, P. Presence of abnormal obturator artery and an abnormal venous plexus at the anterolateral pelvic wall. OA Case Rep. 2014, 3, 49–50. [Google Scholar]
- Sakthivelavan, S.; Sendiladibban, S.D.; Aristotle, S.; Sivanandan, A.V. Corona mortis—A case report with surgical implications distally. Int. J. Anat. Var. 2010, 3, 103–105. [Google Scholar]
- Kumar, D.; Rath, G. Anomalous origin of obturator artery from the internal iliac artery. Int. J. Morphol. 2007, 25, 639–641. [Google Scholar] [CrossRef]
- Berberoğlu, M.; Uz, A.; Ozmen, M.M.; Bozkurt, M.C.; Erkuran, C.; Taner, S.; Tekin, A.; Tekdemir, I. Corona mortis: An anatomic study in seven cadavers and an endoscopic study in 28 patients. Surg. Endosc. 2001, 15, 72–75. [Google Scholar]
- Standring, S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 39th ed.; Elsevier: Amsterdam, The Netherlands, 2005; p. 1044. [Google Scholar]
- Adachi, B. Das Arteriensystem der Japaner; Die Kaiserlich Japanische Universitat zu Kyoto: Kyoto, Japan, 1928. [Google Scholar]
- Jastchinski, S. Die Abweighchungen der arteriaobturatoria. Int. Mschr. Anat. Physiol. 1891, 8, 111–127. [Google Scholar]
- Mahato, N.K. Retro-pubic vascular anomalies: A study of abnormal obturator vessels. Eur. J. Anat. 2009, 13, 121–126. [Google Scholar]
- Herskowitz, M.; Walsh, J.; Lilly, M.; McFarland, K. Importance of Both Internal and External Iliac Artery Interrogation in Pelvic Trauma as Evidenced by Hemorrhage from Bilateral Corona Mortis with Unilateral Aberrant Origin off the External Iliac Artery. Case Rep. Radiol. 2019, 6734816, 1–4. [Google Scholar] [CrossRef]
- Quian, J.; Sharpey, W.; Thomson, A.; Cleland, J.G. Quain’s Elements of Anatomy; Thomson, A., Schaefer, E.A., Thane, G.D., Eds.; James Walton: London, UK, 1867; Volume 1, p. 455. [Google Scholar]
- Bilgiç, S.; Sahin, B. Rare arterial variation: A common trunk from the external iliac artery for the obturator, inferior epigastric and profunda femoris arteries. Surg. Radiol. Anat. 1997, 19, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Jakubowicz, M.; Czarniawska-Grzesinska, M. Variability in origin and topotraphy of the inferior epigastric and obturator arteries. Folia Morphol. 1996, 2, 121–126. [Google Scholar]
- Ram, K.S.; Gupta, T.; Chawla, K.; Aggarwal, A.; Gupta, R.; Sahni, D. Corona Mortis—A Case Report. J. Anat. Sci. 2015, 23, 28–30. [Google Scholar]
- Al-Talalwah, W. A new concept and classification of corona mortis and its clinical significance. Chin. J. Traumatol. 2017, 19, 251–254. [Google Scholar] [CrossRef]
- Petrenko, V.M. Development of the obturator artery in human prenatal ontogenesis. Morfologia 2000, 118, 51–53. [Google Scholar] [PubMed]
- Al-Talalwah, W.; Soames, R. Internal iliac artery classification and its clinical significance: Original Communication. Rev. Argent. Anat. Clin. 2014, 6, 63–71. [Google Scholar] [CrossRef]
- Cunningham, F.G.; Leveno, K.J.; Bloom, S.L.; Hauth, J.C.; Gilstrap, L.C.; Wenstrom, K.D. Williams Obstetrics, 22nd ed.; McGraw–Hill Professional: New York, NY, USA, 2005; pp. 7–8. [Google Scholar]
- Gilroy, A.M.; Hermey, D.C.; DiBenedetto, L.M.; Marks, S.C., Jr.; Page, D.W.; Lei, Q.F. Variability of the obturator vessels. Clin. Anat. 1997, 10, 328–332. [Google Scholar] [CrossRef]
- Nigam, V.K.; Nigam, S. Essentials of Abdominal Wall Hernias; International Publishing House Pvt. Ltd.: New Delhi, India, 2008; p. 84. [Google Scholar]
- Rusu, M.; Cergan, R.; Motoc, A.; Folescu, R.; Pop, E. Anatomical considerations on the corona mortis. Surg. Radiol. Anat. 2010, 32, 17–24. [Google Scholar] [CrossRef]
- Ates, M.; Kinaci, E.; Kose, E.; Soyer, V.; Sarici, B.; Cuglan, S.; Korkmaz, F.; Dirican, A. Corona mortis: In vivo anatomical knowledge and the risk of injury in totally extraperitoneal inguinal hernia repair. Hernia 2016, 20, 659–665. [Google Scholar] [CrossRef]
- Sanna, B.; Henry, B.M.; Vikse, J.; Skinningsrud, B.; Pękala, J.R.; Walocha, J.A.; Cirocchi, R.; Tomaszewski, K.A. The prevalence and morphology of the corona mortis (Crown of death): A meta-analysis with implications in abdominal wall and pelvic surgery. Inj. Int. J. Care Inj. 2018, 49, 302–308. [Google Scholar] [CrossRef]
- Henning, P.; Brenner, B.; Brunner, K.; Zimmermann, H. Hemodynamic Instability Following an Avulsion of the Corona Mortis Artery Secondary to a Benign Pubic Ramus Fracture. J. Trauma Acute Care Surg. 2007, 62, E14–E17. [Google Scholar] [CrossRef] [PubMed]
- Ten Broek, R.P.G.; Bezemer, J.; Timmer, F.A.; Mollen, R.M.H.G.; Boekhoudt, F.D. Massive haemorrhage following minimally displaced pubic ramus fractures. Eur. J. Trauma Emerg. Surg. 2014, 40, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Loffroy, R.; Yeguiayan, J.M.; Guiu, B.; Cercueil, J.; Krausé, D. Stable fracture of the pubic rami: A rare cause of life-threatening bleeding from the inferior epigastric artery managed with transcatheter embolization. Can. J. Emerg. Med. 2008, 10, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Wilson, C.J.; Edwards, R. Massive extraperitoneal hemorrhage after soft tissue trauma to the pubic branch of the inferior epigastric artery. J. Trauma Acute Care Surg. 2000, 48, 779–780. [Google Scholar] [CrossRef]
- Okcu, G.; Erkan, S.; Yercan, H.S.; Ozic, U. The incidence and location of corona mortis: A study of 75 cadavers. Acta Orthop. Scand. 2004, 75, 53–55. [Google Scholar] [CrossRef]



| Group | Description of IIA Divisions |
|---|---|
| A | Two branches: (1) SGA and (2) a common trunk of IGA and IPA (common gluteal-pudendal trunk) |
| B | Two branches: (1) IPA and (2) a common gluteal trunk of SGA and IGA |
| C | Three branches: (1) SGA, (2) IGA, and (3) IPA |
| D | Two branches: (1) a common trunk of SGA and IPA and (2) IGA |
| Type | Description of OA Variation |
|---|---|
| A | The OA arises from anterior division of the IIA |
| B | The OA arises from the DIEA |
| C | The OA is a branch of the posterior division of the IIA |
| D | The OA arises from the IIA, above its final branching |
| E | The OA arises from the EIA |
| F | The OA arises from the FA |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granite, G.; Meshida, K.; Wind, G. Frequency and Clinical Review of the Aberrant Obturator Artery: A Cadaveric Study. Diagnostics 2020, 10, 546. https://doi.org/10.3390/diagnostics10080546
Granite G, Meshida K, Wind G. Frequency and Clinical Review of the Aberrant Obturator Artery: A Cadaveric Study. Diagnostics. 2020; 10(8):546. https://doi.org/10.3390/diagnostics10080546
Chicago/Turabian StyleGranite, Guinevere, Keiko Meshida, and Gary Wind. 2020. "Frequency and Clinical Review of the Aberrant Obturator Artery: A Cadaveric Study" Diagnostics 10, no. 8: 546. https://doi.org/10.3390/diagnostics10080546
APA StyleGranite, G., Meshida, K., & Wind, G. (2020). Frequency and Clinical Review of the Aberrant Obturator Artery: A Cadaveric Study. Diagnostics, 10(8), 546. https://doi.org/10.3390/diagnostics10080546






