Early Diagnosis of Pancreatic Cancer: The Key for Survival
Abstract
1. Introduction
- ductal adenocarcinoma and its subtypes: 85–90%
- intraductal papillary mucinous neoplasms (IPMN) with an associated invasive carcinoma: 2–3%
- mucinous cystic neoplasms (MCN) with an associated invasive carcinoma: 1%
- acinar cell carcinoma: <1%
- pancreato-blastoma: <1%
- serous cystadenocarcinoma: <1%
- intraductal papillary mucinous neoplasms (IPMNs)
- mucinous cystic neoplasms (MCNs)
- solid-pseudopapillary neoplasms (SPNs)
- serous cystic neoplasms (SCNs).
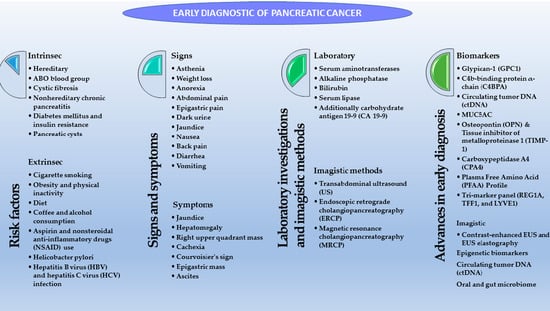
2. Risk Factors for PC
- Patients with associated genetic syndromes (Peutz-Jeghers, ataxia-telangiectasia, Li-Fraumeni); hereditary pancreatitis or ovarian, breast, nonpolyposis colon (Lynch II) cancer; familial atypical multiple mole melanoma syndrome or adenomatous polyposis [19].
- Patients having familial PC history, for which a molecular basis has not yet been discovered [19].
3. Clinical Manifestations of PC and Impediments Regarding Early Diagnosis
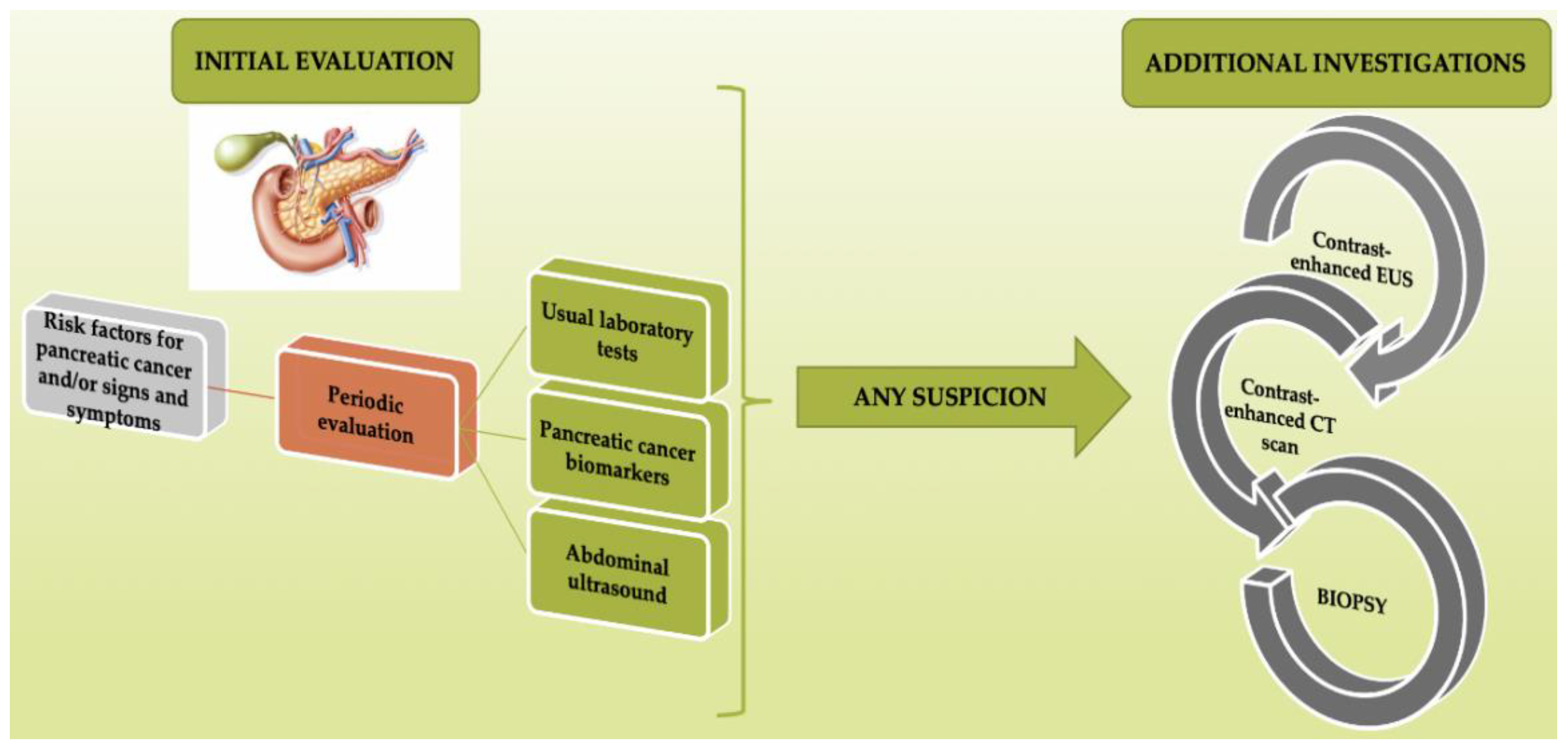
4. Diagnosis of PC in Early Stages
- The detection of deeply localized tumors that are difficult to identify by transabdominal ultrasound.
- The possibility of obtaining tissue samples by FNA biopsy. The samples then undergo a pathology examination to establish a certain diagnosis. The sensibility of this diagnostic method is approximately 92% [71].
- Higher sensibility when compared with transabdominal US, CT, or MRI in the detection of intraductal papillary mucinous neoplasms < 1 cm in size.
- Higher sensibility when compared with CT in the detection of lymph node metastases and vascular invasion [71].
5. Advances in the Early Diagnosis of PC
5.1. Endoscopic Methods
5.2. Genomic Biomarkers
5.2.1. Epigenetic Biomarkers
5.2.2. Circulating Tumor Deoxyribonucleic Acid (ctDNA)
5.2.3. MicroRNAs (miRNAs)
5.2.4. Stool-Based Tests
5.3. Proteomic Biomarkers
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kim, V.M.; Ahuja, N. Early detection of pancreatic cancer. Chin. J. Cancer Res. 2015, 27, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.; Naito, Y.; Cope, L.; Naranjo-Suarez, S.; Saunders, T.; Hong, S.M.; Goggins, M.G.; Herman, J.M.; Wolfgang, C.L.; Iacobuzio-Donahue, C.A. Functional p38 MAPK Identified by Biomarker Profiling of Pancreatic Cancer Restrains Growth through JNK Inhibition and Correlates with Improved Survival. Clin. Cancer Res. 2014, 20, 6200–6211. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef] [PubMed]
- WHO. GLOBOCAN Database. Available online: https://gco.iarc.fr/today/home (accessed on 15 June 2020).
- Eissa, M.A.L.; Lerner, L.; Abdelfatah, E.; Shankar, N.; Canner, J.K.; Hasan, N.M.; Yaghoobi, V.; Huang, B.; Kerner, Z.; Takaesu, F.; et al. Promoter methylation of ADAMTS1 and BNC1 as potential biomarkers for early detection of pancreatic cancer in blood. Clin. Epigenetics 2019, 11, 59. [Google Scholar] [CrossRef]
- Cancer Stat Facts: Pancreatic Cancer. Available online: https://seer.cancer.gov/statfacts/html/pancreas.html (accessed on 17 July 2020).
- Distler, M.; Rückert, F.; Hunger, M.; Kersting, S.; Pilarsky, C.; Saeger, H.D.; Grützmann, R. Evaluation of survival in patients after pancreatic head resection for ductal adenocarcinoma. BMC Surg. 2013, 13, 12. [Google Scholar] [CrossRef]
- Kenner, B.J.; Go, V.L.W.; Chari, S.T.; Goldberg, A.E.; Rothschild, L.J. Early Detection of Pancreatic Cancer: The Role of Industry in the Development of Biomarkers. Pancreas 2017, 46, 1238–1241. [Google Scholar] [CrossRef]
- Jemal, A.; Siegel, R.; Ward, E.; Hao, Y.; Xu, J.; Thun, M.J. Cancer statistics, 2009. CA Cancer J. Clin. 2009, 59, 225–249. [Google Scholar] [CrossRef]
- Wolfgang, C.L.; Herman, J.M.; Laheru, D.A.; Klein, A.P.; Erdek, M.A.; Fishman, E.K.; Hruban, R.H. Recent progress in pancreatic cancer. CA Cancer J. Clin. 2013, 63, 318–348. [Google Scholar] [CrossRef]
- Lennon, A.M.; Wolfgang, C.L.; Canto, M.I.; Klein, A.P.; Herman, J.M.; Goggins, M.; Fishman, E.K.; Kamel, I.; Weiss, M.J.; Diaz, L.A.; et al. The early detection of pancreatic cancer: What will it take to diagnose and treat curable pancreatic neoplasia? Cancer Res. 2014, 74, 3381–3389. [Google Scholar] [CrossRef]
- Klimstra, D.S. Nonductal neoplasms of the pancreas. Mod. Pathol. 2007, 20, S94–S112. [Google Scholar] [CrossRef]
- Haeberle, L.; Esposito, I. Pathology of pancreatic cancer. Transl. Gastroenterol. Hepatol. 2019, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Mogoanta, S.S.; Costache, A.; Mutiu, G.; Bungau, S.G.; Ghilusi, M.; Grosu, F.; Vasile, M.; Vilcea, I.D.; Gherghinescu, M.C.; Mogoanta, L.; et al. A nonfunctional neuroendocrine tumor of the pancreas—A case report. Rom. J. Morphol. Embryol. 2015, 56, 511–519. [Google Scholar] [PubMed]
- Basturk, O.; Hong, S.M.; Wood, L.D.; Adsay, N.V.; Albores-Saavedra, J.; Biankin, A.V.; Brosens, L.A.; Fukushima, N.; Goggins, M.; Hruban, R.H.; et al. Revised Classification System and Recommendations From the Baltimore Consensus Meeting for Neoplastic Precursor Lesions in the Pancreas. Am. J. Surg. Pathol. 2015, 39, 1730–1741. [Google Scholar] [CrossRef]
- Reddy, S.; Cameron, J.L.; Scudiere, J.; Hruban, R.H.; Fishman, E.K.; Ahuja, N.; Pawlik, T.M.; Edil, B.H.; Schulick, R.D.; Wolfgang, C.L. Surgical Management of Solid-Pseudopapillary Neoplasms of the Pancreas (Franz or Hamoudi Tumors): A Large Single-Institutional Series. J. Am. Coll. Surg. 2009, 208, 950–959. [Google Scholar] [CrossRef] [PubMed]
- Wargo, J.A.; Fernandez-del-Castillo, C.; Warshaw, A.L. Management of pancreatic serous cystadenomas. Adv. Surg. 2009, 43, 23–34. [Google Scholar] [CrossRef]
- Mario, C.; Marilisa, F.; Kryssia, I.R.C.; Pellegrino, C.; Ginevra, C.; Chiara, M.; Alberto, B.; Antonio, N.; Gioacchino, L.; Tiziana, M.; et al. Epidemiology and risk factors of pancreatic cancer. Acta Biomed. 2018, 89, 141–146. [Google Scholar] [CrossRef]
- Olson, S.H.; Kurtz, R.C. Epidemiology of pancreatic cancer and the role of family history. J. Surg. Oncol. 2013, 107, 1–7. [Google Scholar] [CrossRef]
- Schneider, R.; Slater, E.P.; Sina, M.; Habbe, N.; Fendrich, V.; Matthäi, E.; Langer, P.; Bartsch, D.K. German national case collection for familial pancreatic cancer (FaPaCa): Ten years experience. Fam. Cancer 2011, 10, 323–330. [Google Scholar] [CrossRef]
- Ghiorzo, P. Genetic predisposition to pancreatic cancer. World J. Gastroenterol. 2014, 20, 10778–10789. [Google Scholar] [CrossRef]
- Vincent, A.; Herman, J.; Schulick, R.; Hruban, R.H.; Goggins, M. Pancreatic cancer. Lancet 2011, 378, 607–620. [Google Scholar] [CrossRef]
- Solomon, S.; Das, S.; Brand, R.; Whitcomb, D.C. Inherited pancreatic cancer syndromes. Cancer J. 2012, 18, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Couch, F.J.; Johnson, M.R.; Rabe, K.G.; Brune, K.; de Andrade, M.; Goggins, M.; Rothenmund, H.; Gallinger, S.; Klein, A.; Petersen, G.M.; et al. The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2007, 16, 342–346. [Google Scholar] [CrossRef]
- Jones, S.; Hruban, R.H.; Kamiyama, M.; Borges, M.; Zhang, X.; Parsons, D.W.; Lin, C.-H.J.; Palmisano, E.; Brune, K.; Jaffee, E.M.; et al. Exomic sequencing identifies PALB2 as a pancreatic cancer susceptibility gene. Science 2009, 324, 217. [Google Scholar] [CrossRef] [PubMed]
- Slater, E.P.; Langer, P.; Niemczyk, E.; Strauch, K.; Butler, J.; Habbe, N.; Neoptolemos, J.P.; Greenhalf, W.; Bartsch, D.K. PALB2 mutations in European familial pancreatic cancer families. Clin. Genet. 2010, 78, 490–494. [Google Scholar] [CrossRef]
- Tischkowitz, M.D.; Sabbaghian, N.; Hamel, N.; Borgida, A.; Rosner, C.; Taherian, N.; Srivastava, A.; Holter, S.; Rothenmund, H.; Ghadirian, P.; et al. Analysis of the gene coding for the BRCA2-Interacting protein PALB2 in familial and sporadic pancreatic cancer. Gastroenterology 2009, 137, 1183–1186. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.P. Genetic susceptibility to pancreatic cancer. Mol. Carcinog. 2012, 51, 14–24. [Google Scholar] [CrossRef]
- Aggarwal, G.; Rabe, K.G.; Petersen, G.M.; Chari, S.T. New-onset diabetes in pancreatic cancer: A study in the primary care setting. Pancreatology 2012, 12, 156–161. [Google Scholar] [CrossRef]
- Batabyal, P.; Vander Hoorn, S.; Christophi, C.; Nikfarjam, M. Association of diabetes mellitus and pancreatic adenocarcinoma: A meta-analysis of 88 studies. Ann. Surg. Oncol. 2014, 21, 2453–2462. [Google Scholar] [CrossRef]
- Vesa, C.M.; Popa, L.; Popa, A.R.; Rus, M.; Zaha, A.A.; Bungau, S.; Tit, D.M.; Aron, R.A.C.; Zaha, D.C. Current Data Regarding the Relationship between Type 2 Diabetes Mellitus and Cardiovascular Risk Factors. Diagnostics 2020, 10, 314. [Google Scholar] [CrossRef]
- Li, D.; Tang, H.; Hassan, M.M.; Holly, E.A.; Bracci, P.M.; Silverman, D.T. Diabetes and risk of pancreatic cancer: A pooled analysis of three large case–control studies. Cancer Causes Control 2011, 22, 189–197. [Google Scholar] [CrossRef]
- Liao, K.F.; Lai, S.W.; Li, C.I.; Chen, W.C. Diabetes mellitus correlates with increased risk of pancreatic cancer: A population-based cohort study in Taiwan. J. Gastroenterol. Hepatol. 2012, 27, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Rosato, V.; Li, D.; Silverman, D.; Petersen, G.M.; Bracci, P.M.; Neale, R.E.; Muscat, J.; Anderson, K.; Gallinger, S.; et al. Diabetes, antidiabetic medications, and pancreatic cancer risk: An analysis from the International Pancreatic Cancer Case-Control Consortium. Ann. Oncol. 2014, 25, 2065–2072. [Google Scholar] [CrossRef] [PubMed]
- Permert, J.; Ihse, I.; Jorfeldt, L.; von Schenck, H.; Arnquist, H.J.; Larsson, J. Improved glucose metabolism after subtotal pancreatectomy for pancreatic cancer. Br. J. Surg. 1993, 80, 1047–1050. [Google Scholar] [CrossRef] [PubMed]
- Gullo, L.; Pezzilli, R.; Morselli-Labate, A.M.; Italian Pancreatic Cancer Study Group. Diabetes and the risk of pancreatic cancer. N. Engl. J. Med. 1994, 331, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.; Wright, D. Diabetes mellitus as a risk factor for pancreatic cancer. A meta-analysis. JAMA 1995, 273, 1605–1609. [Google Scholar] [CrossRef]
- Huxley, R.; Ansary-Moghaddam, A.; de González, A.B.; Barzi, F.; Woodward, M. Type-II diabetes and pancreatic cancer: A meta-analysis of 36 studies. Br. J. Cancer 2005, 92, 2076–2083. [Google Scholar] [CrossRef]
- Lowenfels, A.B.; Maisonneuve, P. Epidemiology and risk factors for pancreatic cancer. Best Pract. Res. Clin. Gastroenterol. 2006, 20, 197–209. [Google Scholar] [CrossRef]
- Nkondjock, A.; Ghadirian, P.; Johnson, K.C.; Krewski, D.; Canadian Cancer Registries Epidemiology Research Group. Dietary intake of lycopene is associated with reduced pancreatic cancer risk. J. Nutr. 2005, 135, 592–597. [Google Scholar] [CrossRef]
- Sivasankarapillai, V.S.; Nair, R.M.K.; Rahdar, A.; Bungau, S.; Zaha, D.C.; Aleya, L.; Tit, D.M. Overview of the anticancer activity of Withaferin A, an active constituent of the Indian Ginseng Withania somnifera. Environ. Sci. Pollut. Res. 2020, 27, 26025–26035. [Google Scholar] [CrossRef]
- Lynch, S.M.; Vrieling, A.; Lubin, J.H.; Kraft, P.; Mendelsohn, J.B.; Hartge, P.; Canzian, F.; Steplowski, E.; Arslan, A.A.; Gross, M.; et al. Cigarette smoking and pancreatic cancer: A pooled analysis from the pancreatic cancer cohort consortium. Am. J. Epidemiol. 2009, 170, 403–413. [Google Scholar] [CrossRef]
- Vrieling, A.; Bueno-de-Mesquita, H.B.; Boshuizen, H.C.; Michaud, D.S.; Severinsen, M.T.; Overvad, K.; Olsen, A.; Tjønneland, A.; Clavel-Chapelon, F.; Boutron-Ruault, M.C.; et al. Cigarette smoking, environmental tobacco smoke exposure and pancreatic cancer risk in the European Prospective Investigation into Cancer and Nutrition. Int. J. Cancer. 2010, 126, 2394–2403. [Google Scholar] [CrossRef]
- Wang, Y.T.; Gou, Y.W.; Jin, W.W.; Xiao, M.; Fang, H.Y. Association between alcohol intake and the risk of pancreatic cancer: A dose–response meta-analysis of cohort studies. BMC Cancer 2016, 16, 212. [Google Scholar] [CrossRef] [PubMed]
- Michaud, D.S.; Vrieling, A.; Jiao, L.; Mendelsohn, J.B.; Steplowski, E.; Lynch, S.M.; Wactawski-Wende, J.; Arslan, A.A.; Bueno-de-Mesquita, H.B.; Fuchs, C.S.; et al. Alcohol intake and pancreatic cancer: A pooled analysis from the pancreatic cancer cohort consortium (PanScan). Cancer Causes Control 2010, 21, 1213–1225. [Google Scholar] [CrossRef]
- Davoodi, S.H.; Malek-Shahabi, T.; Malekshahi-Moghadam, A.; Shahbazi, R.; Esmaeili, S. Obesity as an important risk factor for certain types of cancer. Iran. J. Cancer Prev. 2013, 6, 186–194. [Google Scholar] [PubMed]
- de Gonzalez, A.B.; Sweetland, S.; Spencer, E. A meta-analysis of obesity and the risk of pancreatic cancer. Br. J. Cancer 2003, 89, 519–523. [Google Scholar] [CrossRef]
- Calle, E.E.; Rodriguez, C.; Walker-Thurmond, K.; Thun, M.J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N. Engl. J. Med. 2003, 348, 1625–1638. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Greenwood, D.C.; Chan, D.S.; Vieira, R.; Vieira, A.R.; Rosenblatt, D.A.N.; Cade, J.E.; Burley, V.J.; Norat, T. Body mass index, abdominal fatness and pancreatic cancer risk: A systematic review and non-linear dose-response meta-analysis of prospective studies. Ann. Oncol. 2012, 23, 843–852. [Google Scholar] [CrossRef]
- Lightsey, D.; National Council Against Health Fraud and Quackwatch. Comment on ‘Red and processed meat consumption and risk of pancreatic cancer: Meta-analysis of prospective studies’. Br. J. Cancer 2012, 107, 754–755. [Google Scholar] [CrossRef] [PubMed]
- Stolzenberg-Solomon, R.Z.; Cross, A.J.; Silverman, D.T.; Schairer, C.; Thompson, F.E.; Kipnis, V.; Subar, A.F.; Hollenbeck, A.; Schatzkin, A.; Sinha, R. Meat and meat-mutagen intake and pancreatic cancer risk in the NIH-AARP cohort. Cancer Epidemiol. Biomark. Prev. 2007, 16, 2664–2675. [Google Scholar] [CrossRef]
- Beaney, A.J.; Banim, P.J.; Luben, R.; Lentjes, M.A.; Khaw, K.T.; Hart, A.R. Higher Meat Intakes Are Positively Associated With Higher Risks of Developing Pancreatic Cancer in an Age-dependent Manner and Are Modified by Plasma Anti-oxidants: A Prospective Cohort Study (EPIC-Norfolk) Using Data From Food Diaries. Pancreas 2017, 46, 672–678. [Google Scholar] [CrossRef]
- Beatty, J.K.; Akierman, S.V.; Motta, J.P.; Muise, S.; Workentine, M.L.; Harrison, J.J.; Bhargava, A.; Beck, P.L.; Rioux, K.P.; McKnight, G.W.; et al. Giardia duodenalis induces pathogenic dysbiosis of human intestinal microbiota biofilms. Int. J. Parasitol. 2017, 47, 311–326. [Google Scholar] [CrossRef] [PubMed]
- Michaud, D.S.; Izard, J. Microbiota, oral microbiome, and pancreatic cancer. Cancer J. 2014, 20, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Hujoel, P.P.; Drangsholt, M.; Spiekerman, C.; Weiss, N.S. An exploration of the periodontitis-cancer association. Ann. Epidemiol. 2003, 13, 312–316. [Google Scholar] [CrossRef]
- Joshipura, K.J.; Douglass, C.W.; Garcia, R.I.; Valachovic, R.; Willett, W.C. Validity of a self-reported periodontal disease measure. J. Public Health Dent. 1996, 56, 205–212. [Google Scholar] [CrossRef]
- Stolzenberg-Solomon, R.Z.; Blaser, M.J.; Limburg, P.J.; Perez-Perez, G.; Taylor, P.R.; Virtamo, J.; Albanes, D.; ATBC Study. Helicobacter pylori seropositivity as a risk factor for pancreatic cancer. J. Natl. Cancer Inst. 2001, 93, 937–941. [Google Scholar] [CrossRef]
- Yu, G.; Murphy, G.; Michel, A.; Weinstein, S.J.; Männistö, S.; Albanes, D.; Pawlita, M.; Stolzenberg-Solomon, R.Z. Seropositivity to Helicobacter pylori and risk of pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2013, 22, 2416–2419. [Google Scholar] [CrossRef]
- Risch, H.A.; Yu, H.; Lu, L.; Kidd, M.S. ABO Blood Group. Helicobacter pylori seropositivity, and risk of pancreatic cancer: A case-control study. J. Natl. Cancer Inst. 2010, 102, 502–505. [Google Scholar] [CrossRef]
- Shin, E.J.; Canto, M.I. Pancreatic cancer screening. Gastroenterol. Clin. N. Am. 2012, 41, 143–157. [Google Scholar] [CrossRef]
- De La Cruz, M.S.; Young, A.P.; Ruffin, M.T. Diagnosis and management of pancreatic cancer. Am. Fam. Physician 2014, 89, 626–632. [Google Scholar]
- Porta, M.; Fabregat, X.; Malats, N.; Guarner, L.; Carrato, A.; de Miguel, A.; Ruiz, L.; Jariod, M.; Costafreda, S.; Coll, S.; et al. Exocrine pancreatic cancer: Symptoms at presentation and their relation to tumour site and stage. Clin. Transl. Oncol. 2005, 7, 189–197. [Google Scholar] [CrossRef]
- Mahadevan, D.; Von Hoff, D.D. Tumor-stroma interactions in pancreatic ductal adenocarcinoma. Mol. Cancer Ther. 2007, 6, 1186–1197. [Google Scholar] [CrossRef] [PubMed]
- Canto, M.I.; Goggins, M.; Yeo, C.J.; Griffin, C.; Axilbund, J.E.; Brune, K.; Ali, S.Z.; Jagannath, S.; Petersen, G.M.; Fishman, E.K.; et al. Screening for pancreatic neoplasia in high-risk individuals: An EUS-based approach. Clin. Gastroenterol. Hepatol. 2004, 2, 606–621. [Google Scholar] [CrossRef]
- Zakharova, O.P.; Karmazanovsky, G.G.; Egorov, V.I. Pancreatic adenocarcinoma: Outstanding problems. World J. Gastrointest. Surg. 2012, 4, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Brentnall, T.A.; Bronner, M.P.; Byrd, D.R.; Haggitt, R.C.; Kimmey, M.B. Early diagnosis and treatment of pancreatic dysplasia in patients with a family history of pancreatic cancer. Ann. Intern. Med. 1999, 131, 247–255. [Google Scholar] [CrossRef]
- Canto, M.I.; Goggins, M.; Hruban, R.H.; Petersen, G.M.; Giardiello, F.M.; Yeo, C.; Fishman, E.K.; Brune, K.; Axilbund, J.; Griffin, C.; et al. Screening for early pancreatic neoplasia in high-risk individuals: A prospective controlled study. Clin. Gastroenterol. Hepatol. 2006, 4, 766–781. [Google Scholar] [CrossRef]
- McWilliams, R.R.; Petersen, G.M.; Rabe, K.G.; Holtegaard, L.M.; Lynch, P.J.; Bishop, M.D.; Highsmith, W.E., Jr. Cystic fibrosis transmembrane conductance regulator (CFTR) gene mutations and risk for pancreatic adenocarcinoma. Cancer 2009, 116, 203–209. [Google Scholar] [CrossRef]
- Poley, J.W.; Kluijt, I.; Gouma, D.J.; Harinck, F.; Wagner, A.; Aalfs, C.; van Eijck, C.H.; Cats, A.; Kuipers, E.J.; Nio, Y.; et al. The yield of first-time endoscopic ultrasonography in screening individuals at a high risk of developing pancreatic cancer. Am. J. Gastroenterol. 2009, 104, 2175–2181. [Google Scholar] [CrossRef]
- Vasen, H.F.; Wasser, M.; van Mil, A.; Tollenaar, R.A.; Konstantinovski, M.; Gruis, N.A.; Bergman, W.; Hes, F.J.; Hommes, D.W.; Offerhaus, G.J.; et al. Magnetic resonance imaging surveillance detects early-stage pancreatic cancer in carriers of a p16-Leiden mutation. Gastroenterology 2011, 140, 850–856. [Google Scholar] [CrossRef]
- Raut, C.P.; Grau, A.M.; Staerkel, G.A.; Kaw, M.; Tamm, E.P.; Wolff, R.A.; Vauthey, J.N.; Lee, J.E.; Pisters, P.W.T.; Evans, D.B. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration in patients with presumed pancreatic cancer. J. Gastrointest. Surg. 2003, 7, 118–128. [Google Scholar] [CrossRef]
- Gheonea, D.I.; Săftoiu, A. Beyond conventional endoscopic ultrasound: Elastography, contrast enhancement and hybrid techniques. Curr. Opin. Gastroenterol. 2011, 27, 423–429. [Google Scholar] [CrossRef]
- Kaur, S.; Baine, M.J.; Jain, M.; Sasson, A.R.; Batra, S.K. Early diagnosis of pancreatic cancer: Challenges and new developments. Biomark. Med. 2012, 6, 597–612. [Google Scholar] [CrossRef] [PubMed]
- Poruk, K.E.; Gay, D.Z.; Brown, K.; Mulvihill, J.D.; Boucher, K.M.; Scaife, C.L.; Firpo, M.A.; Mulvihill, S.J. The Clinical Utility of CA 19-9 in Pancreatic Adenocarcinoma: Diagnostic and Prognostic Updates. Curr. Mol. Med. 2013, 13, 340–351. [Google Scholar] [PubMed]
- Gheorghe, G.; Ilie, M.; Socea, B.; Stanescu, A.M.A.; Bratu, O.G.; Iancu, M.A.; Olariu, M.C.; Ciobanu, G.; Diaconu, C.C. Budd-Chiari syndrome. Arch. Balk. Med. Union 2019, 54, 345–350. [Google Scholar] [CrossRef]
- Bratu, O.G.; Cherciu, A.I.; Bumbu, A.; Lupu, S.; Marcu, D.R.; Ionita, R.F.; Manea, M.; Furau, C.; Diaconu, C.C.; Mischianu, D.L.D. Retroperitoneal tumors—Treatment and prognosis of tumor recurrence. Rev. Chim. 2019, 70, 191–194. [Google Scholar] [CrossRef]
- Gold, D.V.; Newsome, G.; Liu, D.; Goldenberg, D.M. Mapping PAM4 (clivatuzumab), a monoclonal antibody in clinical trials for early detection and therapy of pancreatic ductal adenocarcinoma, to MUC5AC mucin. Mol. Cancer 2013, 12, 143. [Google Scholar] [CrossRef]
- Vicentini, C.; Fassan, M.; D’Angelo, E.; Corbo, V.; Silvestris, N.; Nuovo, G.J.; Scarpa, A. Clinical application of microRNA testing in neuroendocrine tumors of the gastrointestinal tract. Molecules 2014, 19, 2458–2468. [Google Scholar] [CrossRef]
- Bettegowda, C.; Sausen, M.; Leary, R.J.; Kinde, I.; Wang, Y.; Agrawal, N.; Bartlett, B.R.; Wang, H.; Luber, B.; Alani, R.M.; et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci. Transl. Med. 2014, 6, 224ra224. [Google Scholar] [CrossRef]
- Long, E.E.; Van Dam, J.; Weinstein, S.; Jeffrey, B.; Desser, T.; Norton, J.A. Computed tomography, endoscopic, laparoscopic, and intra-operative sonography for assessing resectability of pancreatic cancer. Surg. Oncol. 2005, 14, 105–113. [Google Scholar] [CrossRef]
- Beinfeld, M.T.; Wittenberg, E.; Gazelle, G.S. Cost-effectiveness of whole-body CT screening. Radiology 2005, 234, 415–422. [Google Scholar] [CrossRef]
- Rösch, T.; Lorenz, R.; Braig, C.; Feuerbach, S.; Siewert, J.R.; Schusdziarra, V.; Classen, M. Endoscopic ultrasound in pancreatic tumor diagnosis. Gastrointest. Endosc. 1991, 37, 347–352. [Google Scholar] [CrossRef]
- Lee, E.S.; Lee, J.M. Imaging diagnosis of pancreatic cancer: A state-of-the-art review. World J. Gastroenterol. 2014, 20, 7864–7877. [Google Scholar] [CrossRef]
- DeWitt, J.; Devereaux, B.; Chriswell, M.; McGreevy, K.; Howard, T.; Imperiale, T.F.; Ciaccia, D.; Lane, K.A.; Maglinte, D.; Kopecky, K.; et al. Comparison of endoscopic ultrasonography and multidetector computed tomography for detecting and staging pancreatic cancer. Ann. Intern. Med. 2004, 141, 753–763. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.H.; Cha, S.W.; Cho, Y.D. EUS elastography: Advances in diagnostic EUS of the pancreas. Korean J. Radiol. 2012, 13, S12–S16. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, M.; Hookey, L.C.; Bories, E.; Pesenti, C.; Monges, G.; Delpero, J.R. Endoscopic ultrasound elastography: The first step towards virtual biopsy? Preliminary results in 49 patients. Endoscopy 2006, 38, 344–348. [Google Scholar] [CrossRef]
- Ahuja, N.; Sharma, A.R.; Baylin, S.B. Epigenetic Therapeutics: A New Weapon in the War Against Cancer. Annu. Rev. Med. 2016, 67, 73–89. [Google Scholar] [CrossRef]
- Schuebel, K.E.; Chen, W.; Cope, L.; Glöckner, S.C.; Suzuki, H.; Yi, J.M.; Chan, T.A.; Neste, L.V.; Criekinge, W.V.; van den Bosch, S.; et al. Comparing the DNA Hypermethylome with Gene Mutations in Human Colorectal Cancer. PLoS Genet. 2007, 3, e157. [Google Scholar] [CrossRef]
- Jeschke, J.; Van Neste, L.; Glöckner, S.C.; Dhir, M.; Calmon, M.F.; Deregowski, V.; Van Criekinge, W.; Vlassenbroeck, I.; Koch, A.; Chan, T.A.; et al. Biomarkers for detection and prognosis of breast cancer identified by a functional hypermethylome screen. Epigenetics 2012, 7, 701–709. [Google Scholar] [CrossRef]
- Zaha, D.C.; Jurca, C.M.; Bungau, S.; Cioca, G.; Popa, A.; Sava, C.; Endres, L.; Vesa, C.M. Luminal Versus Non-luminal Breast Cancer CDH1 Immunohistochemical Expression. Rev. Chim. 2019, 70, 465–469. [Google Scholar] [CrossRef]
- Yi, J.M.; Guzzetta, A.A.; Bailey, V.J.; Downing, S.R.; Van Neste, L.; Chiappinelli, K.B.; Keeley, B.P.; Stark, A.; Herrera, A.; Wolfgang, C.; et al. Novel methylation biomarker panel for the early detection of pancreatic cancer. Clin. Cancer Res. 2013, 19, 6544–6555. [Google Scholar] [CrossRef]
- Bacalbasa, N.; Balescu, I.; Balalau, C.; Vilcu, M.; Brezean, I. Does sentinel node biopsy play a role in pancreatic adenocarcinoma? Arch. Balk. Med. Union 2019, 54, 334–338. [Google Scholar] [CrossRef]
- Vila-Navarro, E.; Vila-Casadesús, M.; Moreira, L.; Duran-Sanchon, S.; Sinha, R.; Ginés, À.; Fernández-Esparrach, G.; Miquel, R.; Cuatrecasas, M.; Castells, A.; et al. MicroRNAs for detection of pancreatic neoplasia: Biomarker discovery by next-generation sequencing and validation in 2 independent cohorts. Ann. Surg. 2017, 265, 1226–1234. [Google Scholar] [CrossRef]
- Słotwiński, R.; Lech, G.; Słotwińska, S.M. MicroRNAs in pancreatic cancer diagnosis and therapy. Cent. Eur. J. Immunol. 2018, 43, 314–324. [Google Scholar] [CrossRef] [PubMed]
- Vila-Navarro, E.; Duran-Sanchon, S.; Vila-Casadesus, M.; Moreira, L.; Gines, A.; Cuatrecasas, M.; Lozano, J.J.; Bujanda, L.; Castells, A.; Gironella, M. Novel Circulating miRNA Signatures for Early Detection of Pancreatic Neoplasia. Clin. Transl. Gastroenterol. 2019, 10, e00029. [Google Scholar] [CrossRef]
- A Stool DNA Test (Cologuard) for Colorectal Cancer Screening. JAMA 2014, 312, 2566. [CrossRef] [PubMed]
- Kisiel, J.B.; Yab, T.C.; Taylor, W.R.; Chari, S.T.; Petersen, G.M.; Mahoney, D.W.; Ahlquist, D.A. Stool DNA testing for the detection of pancreatic cancer: Assessment of methylation marker candidates. Cancer 2011, 118, 2623–2631. [Google Scholar] [CrossRef] [PubMed]
- Ansari, D.; Torén, W.; Zhou, Q.; Hu, D.; Andersson, R. Proteomic and genomic profiling of pancreatic cancer. Cell Biol. Toxicol. 2019, 35, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Sogawa, K.; Takano, S.; Iida, F.; Satoh, M.; Tsuchida, S.; Kawashima, Y.; Yoshitomi, H.; Sanda, A.; Kodera, Y.; Takizawa, H.; et al. Identification of a novel serum biomarker for pancreatic cancer, C4b-binding protein α-chain (C4BPA) by quantitative proteomic analysis using tandem mass tags. Br. J. Cancer 2016, 115, 949–956. [Google Scholar] [CrossRef]
- Sun, L.; Burnett, J.; Guo, C.; Xie, Y.; Pan, J.; Yang, Z.; Ran, Y.; Sun, D. CPA4 is a promising diagnostic serum biomarker for pancreatic cancer. Am. J. Cancer Res. 2016, 6, 91–96. [Google Scholar]
- Melo, S.A.; Luecke, L.B.; Kahlert, C.; Fernandez, A.F.; Gammon, S.T.; Kaye, J.; LeBleu, V.S.; Mittendorf, E.A.; Weitz, J.; Rahbari, N.; et al. Glypican1 identifies cancer exosomes and facilitates early detection of cancer. Nature 2015, 523, 177–182. [Google Scholar] [CrossRef]
- Kaur, S.; Smith, L.M.; Patel, A.; Menning, M.; Watley, D.C.; Malik, S.S.; Krishn, S.R.; Mallya, K.; Aithal, A.; Sasson, A.R.; et al. A Combination of MUC5AC and CA19-9 Improves the Diagnosis of Pancreatic Cancer: A Multicenter Study. Am. J. Gastroenterol. 2017, 112, 172–183. [Google Scholar] [CrossRef]
- Poruk, K.E.; Firpo, M.A.; Scaife, C.L.; Adler, D.G.; Emerson, L.L.; Boucher, K.M.; Mulvihill, S.J. Serum osteopontin and tissue inhibitor of metalloproteinase 1 as diagnostic and prognostic biomarkers for pancreatic adenocarcinoma. Pancreas 2013, 42, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Fukutake, N.; Ueno, M.; Hiraoka, N.; Shimada, K.; Shiraishi, K.; Saruki, N.; Ito, T.; Yamakado, M.; Ono, N.; Imaizumi, A.; et al. A Novel Multivariate Index for Pancreatic Cancer Detection Based On the Plasma Free Amino Acid Profile. PLoS ONE 2015, 10, e0132223. [Google Scholar] [CrossRef] [PubMed]
- Radon, T.P.; Massat, N.J.; Jones, R.; Alrawashdeh, W.; Dumartin, L.; Ennis, D.; Duffy, S.W.; Kocher, H.M.; Pereira, S.P.; Guarner, L.; et al. Identification of a three-biomarker panel in urine for early detection of pancreatic adenocarcinoma. Clin. Cancer Res. 2015, 21, 3512–3521. [Google Scholar] [CrossRef] [PubMed]
- Verna, E.C.; Hwang, C.; Stevens, P.D.; Rotterdam, H.; Stavropoulos, S.N.; Sy, C.D.; Prince, M.A.; Chung, W.K.; Fine, R.L.; Chabot, J.A.; et al. Pancreatic cancer screening in a prospective cohort of high-risk patients: A comprehensive strategy of imaging and genetics. Clin. Cancer Res. 2010, 16, 5028–5037. [Google Scholar] [CrossRef]
- Humphris, J.L.; Johns, A.L.; Simpson, S.H.; Cowley, M.J.; Pajic, M.; Chang, D.K.; Nagrial, A.M.; Chin, V.T.; Chantrill, L.A.; Pinese, M.; et al. Clinical and pathologic features of familial pancreatic cancer. Cancer 2014, 120, 3669–3675. [Google Scholar] [CrossRef]
- Wagner, M.; Redaelli, C.; Lietz, M.; Seiler, C.A.; Friess, H.; Büchler, M.W. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br. J. Surg. 2004, 91, 586–594. [Google Scholar] [CrossRef]
- Griffin, J.F.; Poruk, K.E.; Wolfgang, C.L. Pancreatic cancer surgery: Past, present, and future. Chin. J. Cancer Res. 2015, 27, 332–348. [Google Scholar] [CrossRef]
| Intrinsic Risk Factors | Extrinsic Risk Factors |
|---|---|
| Hereditary | Cigarette smoking |
| AB0 blood group | Obesity and physical inactivity |
| Cystic fibrosis | Diet |
| Nonhereditary chronic pancreatitis | Coffee and alcohol consumption |
| Diabetes mellitus and insulin resistance | Aspirin and nonsteroidal anti-inflammatory drugs use |
| Pancreatic cysts | Helicobacter pylori infection |
| Hepatitis B and C virus (HBV and HCV) infections |
| Symptoms | Signs |
|---|---|
| Asthenia | Jaundice |
| Weight loss | Hepatomegaly |
| Anorexia | Right upper quadrant mass |
| Abdominal pain | Cachexia |
| Epigastric pain | Courvoisier’s sign |
| Dark urine | Epigastric mass |
| Jaundice | Ascites |
| Nausea | |
| Back pain | |
| Diarrhea | |
| Vomiting | |
| Steatorrhea | |
| Thrombophlebitis |
| Initial Testing | 2nd Step | 3rd Step | ||
|---|---|---|---|---|
| Jaundice or epigastric pain | Serum aminotransferases, alkaline phosphatase, bilirubin, serum lipase, and additionally carbohydrate antigen 19-9 (CA 19-9). These laboratory tests raise suspicion of an upper abdominal cavity pathology, CA19-9 being the most widely used biomarker for PC, with 44.2% sensitivity and 84.8% specificity [74]. | Jaundice | Transabdominal US or ERCP or MRCP in patients with high suspicion for choledocholithiasis. | 1. To confirm the presence of the mass and to assess disease extent: CT scan or MRI. 2. Positive diagnosis: BIOPSY–percutaneous biopsy, endoscopic ultrasound-guided biopsy. |
| Epigastric pain and weight loss | Abdominal CT | |||
| Proteomic Biomarkers | |||
|---|---|---|---|
| In Tissue | In Cell Lines | In Pancreatic Juice | In Serum/Plasma |
| Actinin-4 Annexin A2 Bcl-2 Cathepsin D CD34 CEACAM5 COX-2 Galectin-1 H1.3 hENT1 IGFBP2 IGFBP3 Integrin 1 Ki-67 Laminin β1 LGALS3BP MUC5AC P27 P53 Plasminogen S100A4 Survivin TGF-β1 VEGF | ApoE CD9 Fibronectin receptor Perlecan S100A6 S100A8 S100A9 SDF4 SMAD4 | A1BG Caldecrin DJ-1 FGB Lithostathine I α MMP-9 L1CAM Plasminogen S100A8 S100A9 | CA 19-9 DKK1 Exosomal glypican-1 HSP-27 IL-11 MIC-1 Xylitol+ 1,5-anhydro-D-glucitol + histidine + inositol CA 19-9 + MUC5AC CA 19-9 + CA 242 CA 19-9 + IGF-1 + albumin CA 19-9 + CEA + CA 125 + CA 242 CA 19-9 + 5MC + H2AZ + H2A1.1 + H3K4Me2 CA 19-9 + CEA + HGF + OPN + ctDNA CA 19-9 + THBS2 |
| Biomarker(s) | Sample Origin | Main Findings and Observations–Usefulness in PC Diagnosis | Ref. |
|---|---|---|---|
| C4BPA | Serum | Higher sensitivity than CA19-9, particularly in the early stages of PDAC, also higher specificity for PDAC. | [99] |
| CPA4 | Serum + tissue biopsy | Very well expressed in the tissues and serum of patients with PC, useful in staging the disease because it is associated with lymph node metastasis. | [100] |
| GPC1 | Serum | Correlation with tumor staging, can be identified in circulating exosome of patients with PC, but it is not found in healthy subjects. | [101] |
| MUC5AC | Serum + tissue biopsy | In combination with CA 19-9, it can be useful in improving sensitivity; it is undetectable in healthy pancreas tissue. | [102] |
| OPNT + TIMP-1 | Serum | Combined with CA 19-9, it can improve the sensitivity for PC, therefore being useful in early detection; it is also undetectable in healthy individuals. | [103] |
| PFAA profile | Serum | Strong correlations with disease stage, can distinguish healthy individuals from ones suffering from PC. | [104] |
| LYVE1, REG1A, TFF1 | Urine | High accuracy, of over 90%. PC early stage is detectable using this biomarkers panel. | [105] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gheorghe, G.; Bungau, S.; Ilie, M.; Behl, T.; Vesa, C.M.; Brisc, C.; Bacalbasa, N.; Turi, V.; Costache, R.S.; Diaconu, C.C. Early Diagnosis of Pancreatic Cancer: The Key for Survival. Diagnostics 2020, 10, 869. https://doi.org/10.3390/diagnostics10110869
Gheorghe G, Bungau S, Ilie M, Behl T, Vesa CM, Brisc C, Bacalbasa N, Turi V, Costache RS, Diaconu CC. Early Diagnosis of Pancreatic Cancer: The Key for Survival. Diagnostics. 2020; 10(11):869. https://doi.org/10.3390/diagnostics10110869
Chicago/Turabian StyleGheorghe, Gina, Simona Bungau, Madalina Ilie, Tapan Behl, Cosmin Mihai Vesa, Ciprian Brisc, Nicolae Bacalbasa, Vladiana Turi, Raluca Simona Costache, and Camelia Cristina Diaconu. 2020. "Early Diagnosis of Pancreatic Cancer: The Key for Survival" Diagnostics 10, no. 11: 869. https://doi.org/10.3390/diagnostics10110869
APA StyleGheorghe, G., Bungau, S., Ilie, M., Behl, T., Vesa, C. M., Brisc, C., Bacalbasa, N., Turi, V., Costache, R. S., & Diaconu, C. C. (2020). Early Diagnosis of Pancreatic Cancer: The Key for Survival. Diagnostics, 10(11), 869. https://doi.org/10.3390/diagnostics10110869