Physical Inactivity and Cardiovascular Health in Aging Populations: Epidemiological Evidence and Policy Implications from Riyadh, Saudi Arabia
Abstract
1. Introduction
1.1. Aim of the Study
1.2. Research Question
- What is the association between physical inactivity and key cardiovascular disease (CVD) risk factors (e.g., hypertension, diabetes, obesity) in older adults in Riyadh?
- What are the demographic and socioeconomic determinants of physical inactivity among older adults in this population?
- How do existing policy recommendations align with the specific barriers to physical activity in Riyadh, and what strategies can be proposed to address these barriers?
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Sample and Sampling
2.4. Inclusion Criteria
- Age: Participants aged 60 years or older were selected to focus on the elderly population, where the risk of cardiovascular diseases and physical inactivity tends to be higher.
- Medical Status: Individuals diagnosed with or at risk for cardiovascular diseases, as determined by their medical records or clinical evaluation, were included to ensure the study’s relevance to cardiovascular health.
- Hospital Attendance: Only patients attending the hospital for routine medical care, follow-ups, or cardiovascular-related issues were considered.
- Consent: Participants were required to provide informed consent. In cases where participants were unable to consent independently (e.g., due to mild cognitive impairment), consent was obtained from their legal guardians or caregivers.
2.5. Exclusion Criteria
- Severe Cognitive or Communication Impairments: Individuals unable to comprehend the study procedures or respond to the questionnaire due to severe cognitive decline, dementia, or language barriers were excluded.
- Terminal Illnesses: Patients with terminal conditions or those receiving palliative care were excluded, as their health status could significantly confound the study results.
- Non-Compliance: Individuals unwilling or unable to complete the questionnaire or participate in anthropometric measurements were excluded.
2.6. Sampling Technique
- Screening: Medical records and patient appointment schedules were reviewed to identify potential participants who met the inclusion criteria.
- Invitation: Eligible individuals were approached in person, and the study objectives and procedures were explained in detail.
- Voluntary Participation: Participation was entirely voluntary, and individuals were given sufficient time to decide whether to join the study.
2.7. Justification for Sample Size
2.8. Data Collection Tools
2.8.1. Structured Questionnaire
- Demographic Information: Questions on age, gender, marital status, education level, occupation (if applicable), and socioeconomic status.
- Lifestyle Factors: Inquiries about dietary habits, smoking history, alcohol consumption, and sleep patterns.
- Medical History: Questions on participants’ past and current medical conditions, particularly related to cardiovascular diseases (e.g., hypertension, hyperlipidemia, diabetes, and prior cardiovascular events such as myocardial infarction or stroke).
- Family History: Information on the prevalence of cardiovascular diseases and related conditions among first-degree relatives.
2.8.2. Physical Activity Scale for the Elderly (PASE)
- Leisure-Time Activities: Walking, swimming, dancing, and other recreational activities.
- Household Activities: Light and heavy housework, gardening, and yard work.
- Occupational Activities: Physical tasks associated with any part-time or volunteer work.
- A pilot test was conducted with 15 older adults in Riyadh to assess comprehension and clarity. Minor adjustments were made in wording to reflect local activities, such as including references to indoor walking in shopping malls—a common alternative to outdoor exercise due to extreme weather conditions.
- Bilingual administration: The PASE was offered in both English and Arabic, with trained research assistants available to clarify questions for participants with literacy challenges.
- Expert review: The adapted questionnaire was reviewed by local geriatric and public health specialists to ensure its relevance to the Saudi Arabian context.
2.8.3. Medical Record Review
- Blood Pressure: Most recent systolic and diastolic blood pressure readings.
- Lipid Profile: Levels of total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides.
- Blood Glucose Levels: Fasting blood glucose and HbA1c readings for participants with or without diabetes.
- Body Mass Index (BMI): Pre-recorded height and weight measurements used to calculate BMI.
- Cardiovascular Diagnoses: Documentation of any diagnosed cardiovascular conditions (e.g., coronary artery disease, heart failure, or arrhythmias).
2.8.4. Anthropometric Measurements
- Weight and Height: Measured using a calibrated digital scale and stadiometer, respectively. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2).
- Waist Circumference: Measured at the midpoint between the lower rib and the iliac crest using a non-stretchable measuring tape. This measurement was used to assess central obesity, a critical risk factor for cardiovascular diseases.
- Hip Circumference: Taken at the widest part of the hips to calculate the waist-to-hip ratio, another indicator of cardiovascular risk.
2.9. Data Collection Procedure
2.10. Recruitment of Participants
2.11. Administration of the Structured Questionnaire
2.12. Assessment of Physical Activity
- Low physical activity: PASE score ≤ 60 (sedentary lifestyle, minimal activity)
- Moderate physical activity: PASE score 61–100 (occasional structured activity, moderate household chores)
- High physical activity: PASE score > 100 (frequent structured exercise, active daily routines)
- Handgrip strength measurement (via a dynamometer)
- Gait speed testing (as a functional mobility indicator)
- Muscle mass estimation (via bioelectrical impedance analysis or DXA scans)
2.13. Anthropometric Measurements Procedure
2.14. Medical Record Review Procedure
2.15. Quality Control Measures
2.16. Data Analysis
2.17. Data Normality
2.18. Path Analysis Details
2.19. Ethical Considerations
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Di Cesare, M.; Perel, P.; Taylor, S.; Kabudula, C.; Bixby, H.; Gaziano, T.A.; McGhie, D.V.; Mwangi, J.; Pervan, B.; Narula, J.; et al. The Heart of the World. Glob. Heart 2024, 19, 11. [Google Scholar] [CrossRef]
- Qu, C.; Liao, S.; Zhang, J.; Cao, H.; Zhang, H.; Zhang, N.; Yan, L.; Cui, G.; Luo, P.; Zhang, Q.; et al. Burden of Cardiovascular Disease among Elderly: Based on the Global Burden of Disease Study 2019. Eur. Heart J. Qual. Care Clin. Outcomes 2024, 10, 143–153. [Google Scholar] [CrossRef] [PubMed]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical Activity in Older Age: Perspectives for Healthy Ageing and Frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Alfaraidhy, M.A.; Regan, C.; Forman, D.E. Cardiac Rehabilitation for Older Adults: Current Evidence and Future Potential. Expert Rev. Cardiovasc. Ther. 2022, 20, 13–34. [Google Scholar] [CrossRef] [PubMed]
- Warren, T.Y.; Barry, V.; Hooker, S.P.; Sui, X.; Church, T.S.; Blair, S.N. Sedentary Behaviors Increase Risk of Cardiovascular Disease Mortality in Men. Med. Sci. Sport. Exerc. 2010, 42, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Zhang, M.; Wang, C.; Yuan, Y.; Liang, J. Association between Sedentary Behavior, Physical Activity, and Cardiovascular Disease-Related Outcomes in Adults—A Meta-Analysis and Systematic Review. Front. Public Health 2022, 10, 1018460. [Google Scholar] [CrossRef]
- Luo, Y.; Liu, J.; Zeng, J.; Pan, H. Global Burden of Cardiovascular Diseases Attributed to Low Physical Activity: An Analysis of 204 Countries and Territories between 1990 and 2019. Am. J. Prev. Cardiol. 2024, 17, 100633. [Google Scholar] [CrossRef]
- Singam, N.S.V.; Fine, C.; Fleg, J.L. Cardiac Changes Associated with Vascular Aging. Clin. Cardiol. 2020, 43, 92–98. [Google Scholar] [CrossRef]
- Mahmood, S.S.; Levy, D.; Vasan, R.S.; Wang, T.J. The Framingham Heart Study and the Epidemiology of Cardiovascular Disease: A Historical Perspective. Lancet 2014, 383, 999–1008. [Google Scholar] [CrossRef]
- Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Physical Activity, All-Cause and Cardiovascular Mortality, and Cardiovascular Disease. Med. Sci. Sport. Exerc. 2019, 51, 1270–1281. [Google Scholar] [CrossRef] [PubMed]
- Tucker, W.J.; Fegers-Wustrow, I.; Halle, M.; Haykowsky, M.J.; Chung, E.H.; Kovacic, J.C. Exercise for Primary and Secondary Prevention of Cardiovascular Disease. J. Am. Coll. Cardiol. 2022, 80, 1091–1106. [Google Scholar] [CrossRef]
- Collado-Mateo, D.; Lavín-Pérez, A.M.; Peñacoba, C.; Del Coso, J.; Leyton-Román, M.; Luque-Casado, A.; Gasque, P.; Fernández-del-Olmo, M.Á.; Amado-Alonso, D. Key Factors Associated with Adherence to Physical Exercise in Patients with Chronic Diseases and Older Adults: An Umbrella Review. Int. J. Environ. Res. Public Health 2021, 18, 2023. [Google Scholar] [CrossRef] [PubMed]
- Kanavaki, A.M.; Rushton, A.; Efstathiou, N.; Alrushud, A.; Klocke, R.; Abhishek, A.; Duda, J.L. Barriers and Facilitators of Physical Activity in Knee and Hip Osteoarthritis: A Systematic Review of Qualitative Evidence. BMJ Open 2017, 7, e017042. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Rosenbaum, S.; Stubbs, B.; Gorczynski, P.; Yung, A.R.; Vancampfort, D. Motivating Factors and Barriers towards Exercise in Severe Mental Illness: A Systematic Review and Meta-Analysis. Psychol. Med. 2016, 46, 2869–2881. [Google Scholar] [CrossRef] [PubMed]
- McMaughan, D.J.; Oloruntoba, O.; Smith, M.L. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front. Public Health 2020, 8, 231. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Liu, Z.; Fu, Y.; Zhang, H.; Wu, J.; Lai, C.; Xue, E.; Gao, Q.; Shao, J. Social Determinants of Intrinsic Capacity: A National Cohort Study. Am. J. Prev. Med. 2024, 66, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.R.; Sudati, I.P.; Konzen, V.D.M.; de Campos, A.C.; Wibelinger, L.M.; Correa, C.; Miguel, F.M.; Silva, R.N.; Borghi-Silva, A. COVID-19 and the Impact on the Physical Activity Level of Elderly People: A Systematic Review. Exp. Gerontol. 2022, 159, 111675. [Google Scholar] [CrossRef]
- Zhao, J.; Ke, Z.; Huang, R.; Wen, X.; Liu, W.; Wang, S.; Zhang, X.; Zhuang, X.; Pan, L.; Liao, L. Physical Activity and the Risk of Developing 8 Age-Related Diseases: Epidemiological and Mendelian Randomization Studies. Eur. Rev. Aging Phys. Act. 2024, 21, 24. [Google Scholar] [CrossRef] [PubMed]
- Gelius, P.; Messing, S.; Goodwin, L.; Schow, D.; Abu-Omar, K. What Are Effective Policies for Promoting Physical Activity? A Systematic Review of Reviews. Prev. Med. Reports 2020, 18, 101095. [Google Scholar] [CrossRef] [PubMed]
- Chamradova, K.; Batalik, L.; Winnige, P.; Dosbaba, F.; Hartman, M.; Batalikova, K.; Janikova, A.; Nehyba, S.; Felsoci, M.; Pepera, G.; et al. Effects of Home-Based Exercise with Telehealth Guidance in Lymphoma Cancer Survivors Entering Cardio-Oncology Rehabilitation: Rationale and Design of the Tele@home Study. Cardio-Oncology 2024, 10, 46. [Google Scholar] [CrossRef]
- Lutz, A.H.; Forman, D.E. Cardiac Rehabilitation in Older Adults: Apropos yet Significantly Underutilized. Prog. Cardiovasc. Dis. 2022, 70, 94–101. [Google Scholar] [CrossRef]
- Heath, G.W.; Parra, D.C.; Sarmiento, O.L.; Andersen, L.B.; Owen, N.; Goenka, S.; Montes, F.; Brownson, R.C. Evidence-Based Intervention in Physical Activity: Lessons from around the World. Lancet 2012, 380, 272–281. [Google Scholar] [CrossRef]
- Van Hoof, J.; Kazak, J.K.; Perek-Białas, J.M.; Peek, S.T.M. The Challenges of Urban Ageing: Making Cities Age-Friendly in Europe. Int. J. Environ. Res. Public Health 2018, 15, 2473. [Google Scholar] [CrossRef] [PubMed]
- Fien, S.; Linton, C.; Mitchell, J.S.; Wadsworth, D.P.; Szabo, H.; Askew, C.D.; Schaumberg, M.A. Characteristics of Community-Based Exercise Programs for Community-Dwelling Older Adults in Rural/Regional Areas: A Scoping Review. Aging Clin. Exp. Res. 2022, 34, 1511–1528. [Google Scholar] [CrossRef] [PubMed]
- den Braver, N.R.; Garcia Bengoechea, E.; Messing, S.; Kelly, L.; Schoonmade, L.J.; Volf, K.; Zukowska, J.; Gelius, P.; Forberger, S.; Woods, C.B.; et al. The Impact of Mass-Media Campaigns on Physical Activity: A Review of Reviews through a Policy Lens. Eur. J. Public Health 2022, 32, iv71–iv83. [Google Scholar] [CrossRef] [PubMed]
- Aerts, N.; Anthierens, S.; Van Bogaert, P.; Peremans, L.; Bastiaens, H. Prevention of Cardiovascular Diseases in Community Settings and Primary Health Care: A Pre-Implementation Contextual Analysis Using the Consolidated Framework for Implementation Research. Int. J. Environ. Res. Public Health 2022, 19, 8467. [Google Scholar] [CrossRef] [PubMed]
- Schultz, W.M.; Kelli, H.M.; Lisko, J.C.; Varghese, T.; Shen, J.; Sandesara, P.; Quyyumi, A.A.; Taylor, H.A.; Gulati, M.; Harold, J.G.; et al. Socioeconomic Status and Cardiovascular Outcomes. Circulation 2018, 137, 2166–2178. [Google Scholar] [CrossRef] [PubMed]
- Canali, S.; Schiaffonati, V.; Aliverti, A. Challenges and Recommendations for Wearable Devices in Digital Health: Data Quality, Interoperability, Health Equity, Fairness. PLoS Digit. Health 2022, 1, e0000104. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Chandrasekaran, A.M.; Bhaumik, S.; Chattopadhyay, K.; Gamage, A.U.; De Silva, P.; Roy, A.; Prabhakaran, D.; Tandon, N. Cost-Effectiveness of Interventions to Control Cardiovascular Diseases and Diabetes Mellitus in South Asia: A Systematic Review. BMJ Open 2018, 8, e017809. [Google Scholar] [CrossRef]
- Jones, M.; Bright, P.; Hansen, L.; Ihnatsenka, O.; Carek, P.J. Promoting Physical Activity in a Primary Care Practice: Overcoming the Barriers. Am. J. Lifestyle Med. 2021, 15, 158–164. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M. Physical Inactivity in Saudi Arabia Revisited: A Systematic Review of Inactivity Prevalence and Perceived Barriers to Active Living. Int. J. Health Sci. 2018, 12, 50–64. [Google Scholar]
- Alharbi, B.F.H.; Baker, P.; Pavey, T.; Alharbi, M.F. Investigating the Beliefs of Saudi Females Regarding Physical Activity: A Qualitative Exploration. Int. J. Qual. Stud. Health Well-Being 2024, 19, 2296696. [Google Scholar] [CrossRef] [PubMed]
- Alqarni, A.; Vennu, V.; Alshammari, S.A.; Bindawas, S.M. Cross-Cultural Adaptation and Validation of the Arabic Version of the Physical Activity Scale for the Elderly among Community-Dwelling Older Adults in Saudi Arabia. Clin. Interv. Aging 2018, 13, 419–427. [Google Scholar] [CrossRef] [PubMed]
- D’Amore, C.; Lajambe, L.; Bush, N.; Hiltz, S.; Laforest, J.; Viel, I.; Hao, Q.; Beauchamp, M. Mapping the Extent of the Literature and Psychometric Properties for the Physical Activity Scale for the Elderly (PASE) in Community-Dwelling Older Adults: A Scoping Review. BMC Geriatr. 2024, 24, 761. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The Moderator–Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations. J. Pers. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013; Volume xvii, p. 507. [Google Scholar]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Koolhaas, C.M.; Dhana, K.; Schoufour, J.D.; Ikram, M.A.; Kavousi, M.; Franco, O.H. Impact of Physical Activity on the Association of Overweight and Obesity with Cardiovascular Disease: The Rotterdam Study. Eur. J. Prev. Cardiol. 2017, 24, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Anindya, K.; Marthias, T.; Zulfikar Biruni, M.; Hage, S.; Ng, N.; Laverty, A.A.; McPake, B.; Millett, C.; Haregu, T.N.; Hulse, E.S.G.; et al. Low Physical Activity Is Associated with Adverse Health Outcome and Higher Costs in Indonesia: A National Panel Study. Front. Cardiovasc. Med. 2022, 9, 972461. [Google Scholar] [CrossRef] [PubMed]
- Syeda, U.S.A.; Battillo, D.; Visaria, A.; Malin, S.K. The Importance of Exercise for Glycemic Control in Type 2 Diabetes. Am. J. Med. Open 2023, 9, 100031. [Google Scholar] [CrossRef] [PubMed]
- Barone Gibbs, B.; Hivert, M.-F.; Jerome, G.J.; Kraus, W.E.; Rosenkranz, S.K.; Schorr, E.N.; Spartano, N.L.; Lobelo, F. Physical Activity as a Critical Component of First-Line Treatment for Elevated Blood Pressure or Cholesterol: Who, What, and How?: A Scientific Statement From the American Heart Association. Hypertension 2021, 78, e26–e37. [Google Scholar] [CrossRef] [PubMed]
- Kraft, P.; Kraft, B. Explaining Socioeconomic Disparities in Health Behaviours: A Review of Biopsychological Pathways Involving Stress and Inflammation. Neurosci. Biobehav. Rev. 2021, 127, 689–708. [Google Scholar] [CrossRef] [PubMed]
- Pampel, F.C.; Krueger, P.M.; Denney, J.T. Socioeconomic Disparities in Health Behaviors. Annu. Rev. Sociol. 2010, 36, 349–370. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.K.; Floegel, T.A.; Li, L.C.; Leese, J.; De Vera, M.A.; Beauchamp, M.R.; Taunton, J.; Liu-Ambrose, T.; Allen, K.D. Tailored Physical Activity Behavior Change Interventions: Challenges and Opportunities. Transl. Behav. Med. 2021, 11, 2174–2181. [Google Scholar] [CrossRef]
- Mendoza-Vasconez, A.S.; Linke, S.; Muñoz, M.; Pekmezi, D.; Ainsworth, C.; Cano, M.; Williams, V.; Marcus, B.H.; Larsen, B.A. Promoting Physical Activity among Underserved Populations. Curr. Sports Med. Rep. 2016, 15, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Meredith, S.J.; Cox, N.J.; Ibrahim, K.; Higson, J.; McNiff, J.; Mitchell, S.; Rutherford, M.; Wijayendran, A.; Shenkin, S.D.; Kilgour, A.H.M.; et al. Factors That Influence Older Adults’ Participation in Physical Activity: A Systematic Review of Qualitative Studies. Age Ageing 2023, 52, afad145. [Google Scholar] [CrossRef] [PubMed]
- Brandt, L.; Liu, S.; Heim, C.; Heinz, A. The Effects of Social Isolation Stress and Discrimination on Mental Health. Transl. Psychiatry 2022, 12, 398. [Google Scholar] [CrossRef] [PubMed]
- Craike, M.; Wiesner, G.; Hilland, T.A.; Bengoechea, E.G. Interventions to Improve Physical Activity among Socioeconomically Disadvantaged Groups: An Umbrella Review. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 43. [Google Scholar] [CrossRef]
- Zimmer, C.; McDonough, M.H.; Hewson, J.; Toohey, A.M.; Din, C.; Crocker, P.R.E.; Bennett, E.V. Social Support among Older Adults in Group Physical Activity Programs. J. Appl. Sport Psychol. 2023, 35, 658–679. [Google Scholar] [CrossRef]
- Shaban, M.; Mohammed, H.H.; Amer, F.G.M.; Elsayed, H.H.; Ali, S.I.; Ibrahim, A.M. Psychometric Evaluation of the Translated Arabic Version of the Geriatrics Health Behavior Questionnaire (GHBQ) for Geriatric Nurses: A Cross-Sectional Study. BMC Nurs. 2024, 23, 552. [Google Scholar] [CrossRef] [PubMed]
- Wattanapisit, A.; Wattanapisit, S.; Wongsiri, S. Overview of Physical Activity Counseling in Primary Care. Korean J. Fam. Med. 2021, 42, 260–268. [Google Scholar] [CrossRef]
- Portegijs, E.; Lee, C.; Zhu, X. Activity-Friendly Environments for Active Aging: The Physical, Social, and Technology Environments. Front. Public Health 2023, 10, 1080148. [Google Scholar] [CrossRef] [PubMed]
- Hong, A.; Welch-Stockton, J.; Kim, J.Y.; Canham, S.L.; Greer, V.; Sorweid, M. Age-Friendly Community Interventions for Health and Social Outcomes: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 2554. [Google Scholar] [CrossRef] [PubMed]
- Shaban, M.; Amer, F.G.M.; Shaban, M.M. The Impact of Nursing Sustainable Prevention Program on Heat Strain among Agricultural Elderly Workers in the Context of Climate Change. Geriatr. Nurs. 2024, 58, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Haldane, V.; Chuah, F.L.H.; Srivastava, A.; Singh, S.R.; Koh, G.C.H.; Seng, C.K.; Legido-Quigley, H. Community Participation in Health Services Development, Implementation, and Evaluation: A Systematic Review of Empowerment, Health, Community, and Process Outcomes. PLoS ONE 2019, 14, e0216112. [Google Scholar] [CrossRef] [PubMed]
- Perry, A.S.; Dooley, E.E.; Master, H.; Spartano, N.L.; Brittain, E.L.; Pettee Gabriel, K. Physical Activity Over the Lifecourse and Cardiovascular Disease. Circ. Res. 2023, 132, 1725–1740. [Google Scholar] [CrossRef]
- Ibrahim, A.M.; Abdel-Aziz, H.R.; Mohamed, H.A.H.; Zaghamir, D.E.F.; Wahba, N.M.I.; Hassan, G.A.; Shaban, M.; EL-Nablaway, M.; Aldughmi, O.N.; Aboelola, T.H. Balancing Confidentiality and Care Coordination: Challenges in Patient Privacy. BMC Nurs. 2024, 23, 564. [Google Scholar] [CrossRef] [PubMed]
- Homoud, M.; Jarrar, O.M. Walkability in Riyadh: A Comprehensive Assessment and Implications for Sustainable Community—Al-Falah Case Study. Sustainability 2024, 16, 8073. [Google Scholar] [CrossRef]
- Ajlan, A.M.; Abed, A.M. Al Transformation Model towards Sustainable Smart Cities: Riyadh, Saudi Arabia as a Case Study. Curr. Urban Stud. 2023, 11, 142–178. [Google Scholar] [CrossRef]
- Alruwaili, M.; Elsayed Ramadan, O.M.; Shaban, M.; Alruwaili, A.; Alsadaan, N.; Ali, S.; Al Thobaity, A.; Salihu, D. An Assessment of Pediatric Nurses Awareness and Perceived Knowledge of Autism Spectrum Disorders: A Gulf State Survey. Perspect. Psychiatr. Care 2023, 2023, 1–9. [Google Scholar] [CrossRef]
- Addas, A. Impact of Neighborhood Safety on Adolescent Physical Activity in Saudi Arabia: Gender and Socio-Economic Perspectives. Front. Public Health 2025, 13, 1520851. [Google Scholar] [CrossRef] [PubMed]
- Katar, I. Promoting Pedestrian Ecomobility in Riyadh City for Sustainable Urban Development. Sci. Rep. 2022, 12, 14808. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazzaa, H.M.; AlMarzooqi, M.A. Descriptive Analysis of Physical Activity Initiatives for Health Promotion in Saudi Arabia. Front. Public Health 2018, 6, 329. [Google Scholar] [CrossRef] [PubMed]
- van Hoof, J.; Marston, H.R.; Kazak, J.K.; Buffel, T. Ten Questions Concerning Age-Friendly Cities and Communities and the Built Environment. Build. Environ. 2021, 199, 107922. [Google Scholar] [CrossRef]
- Chase, J.-A.D. Methodological Challenges in Physical Activity Research With Older Adults. West. J. Nurs. Res. 2013, 35, 76–97. [Google Scholar] [CrossRef]
- Mehrabi, S.; Muñoz, J.E.; Basharat, A.; Boger, J.; Cao, S.; Barnett-Cowan, M.; Middleton, L.E. Immersive Virtual Reality Exergames to Promote the Well-Being of Community-Dwelling Older Adults: Protocol for a Mixed Methods Pilot Study. JMIR Res. Protoc. 2022, 11, e32955. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Categories | n (%) |
|---|---|---|
| Age (years) | 60–64 | 64 (38.1%) |
| 65–69 | 55 (32.5%) | |
| 70–74 | 31 (18.4%) | |
| ≥75 | 18 (11.0%) | |
| Gender | Male | 91 (54.2%) |
| Female | 77 (45.8%) | |
| Education | No formal | 46 (27.3%) |
| High school | 71 (42.5%) | |
| College | 51 (30.2%) | |
| Marital Status | Married | 119 (71.1%) |
| Widowed | 49 (28.9%) | |
| Employment Status | Retired | 105 (62.5%) |
| Employed | 26 (15.3%) | |
| Unemployed | 37 (22.2%) | |
| Smoking Status | Current | 43 (25.8%) |
| Former | 58 (34.7%) | |
| Never | 67 (39.5%) | |
| Household Income | <10,000 SAR | 79 (47.3%) |
| 10,000–20,000 SAR | 59 (35.2%) | |
| >20,000 SAR | 29 (17.5%) |
| Physical Activity Level | n (%) | Mean PASE Score ± SD | Walking Duration (min/day) ± SD | Vigorous Exercise (%) |
|---|---|---|---|---|
| Low | 87 (51.8%) | 42.7 ± 12.3 | 15.2 ± 7.1 | 12.3 |
| Moderate | 49 (29.2%) | 85.4 ± 10.6 | 32.8 ± 10.4 | 34.6 |
| High | 32 (19.0%) | 120.3 ± 15.1 | 52.1 ± 12.7 | 58.7 |
| Risk Factor | Low Activity (%) | Moderate Activity (%) | High Activity (%) | p-Value |
|---|---|---|---|---|
| Hypertension | 78.2 | 63.1 | 41.8 | <0.001 |
| Diabetes | 64.4 | 49.8 | 28.7 | <0.001 |
| Obesity (BMI ≥ 30) | 51.3 | 39.6 | 22.3 | <0.001 |
| Hyperlipidemia | 69.0 | 55.3 | 35.4 | <0.001 |
| History of Stroke | 12.6 | 8.4 | 4.3 | <0.05 |
| Coronary Artery Disease | 28.7 | 18.5 | 9.8 | <0.001 |
| Indicator | Low Activity | Moderate Activity | High Activity | p-Value |
|---|---|---|---|---|
| Systolic BP (mmHg) | 148.7 ± 9.4 | 132.6 ± 8.5 | 125.4 ± 7.2 | <0.001 |
| Diastolic BP (mmHg) | 92.3 ± 7.1 | 85.4 ± 6.2 | 80.1 ± 5.6 | <0.001 |
| Total Cholesterol (mg/dL) | 236.5 ± 18.3 | 202.4 ± 15.8 | 182.7 ± 12.9 | <0.001 |
| HDL Cholesterol (mg/dL) | 38.2 ± 5.1 | 46.7 ± 6.4 | 52.3 ± 7.2 | <0.001 |
| LDL Cholesterol (mg/dL) | 157.3 ± 14.8 | 128.9 ± 12.7 | 112.4 ± 10.3 | <0.001 |
| Blood Glucose (mg/dL) | 161.7 ± 21.4 | 140.2 ± 18.5 | 121.5 ± 15.3 | <0.001 |
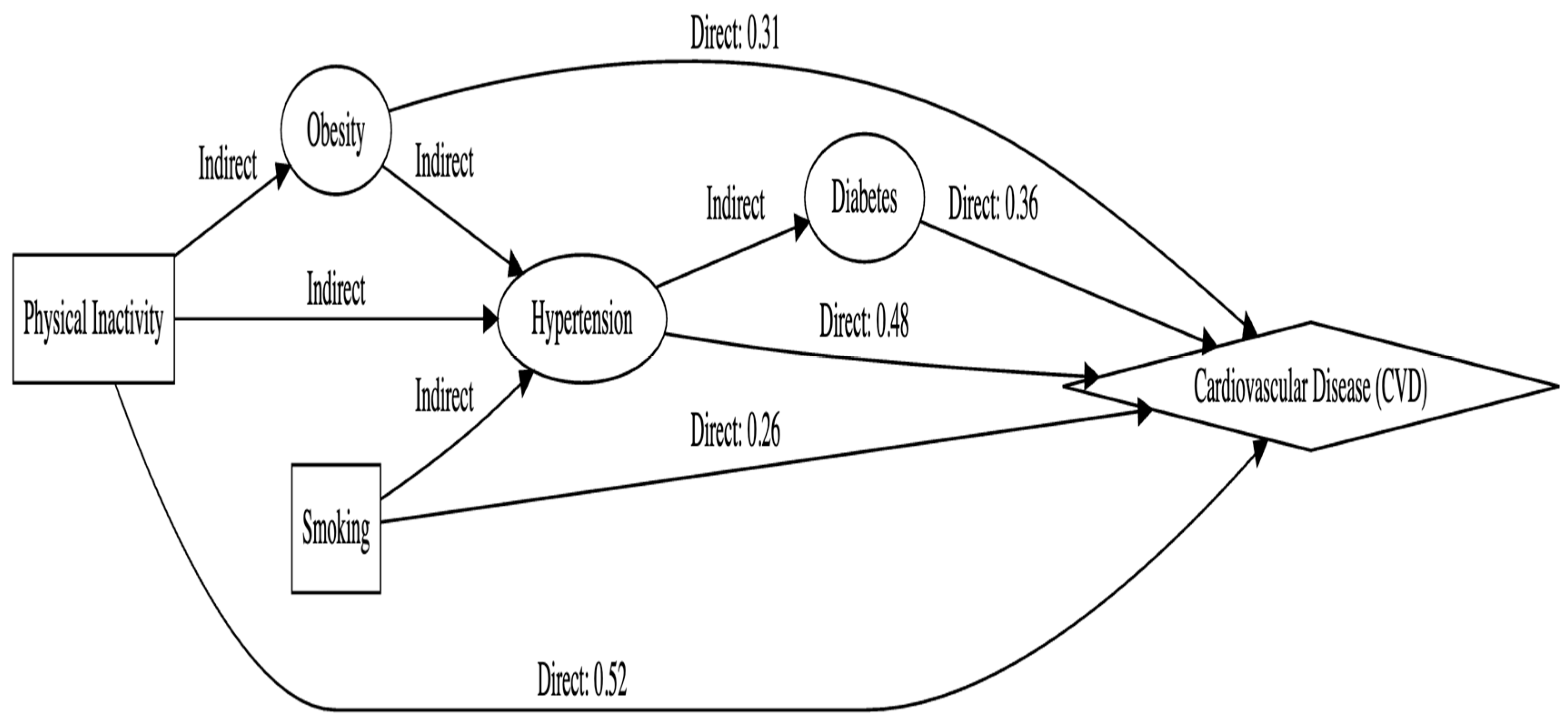
| Variable | Adjusted OR (95% CI) | p-Value |
|---|---|---|
| Physical Inactivity | 1.98 (1.53–2.56) | <0.001 |
| Hypertension | 1.73 (1.34–2.23) | <0.001 |
| Diabetes | 1.52 (1.21–1.91) | <0.001 |
| Obesity | 1.41 (1.12–1.79) | <0.001 |
| Smoking | 1.29 (0.98–1.68) | 0.045 |
| Model Effect Size | R2 = 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alodhialah, A.M.; Almutairi, A.A.; Almutairi, M. Physical Inactivity and Cardiovascular Health in Aging Populations: Epidemiological Evidence and Policy Implications from Riyadh, Saudi Arabia. Life 2025, 15, 347. https://doi.org/10.3390/life15030347
Alodhialah AM, Almutairi AA, Almutairi M. Physical Inactivity and Cardiovascular Health in Aging Populations: Epidemiological Evidence and Policy Implications from Riyadh, Saudi Arabia. Life. 2025; 15(3):347. https://doi.org/10.3390/life15030347
Chicago/Turabian StyleAlodhialah, Abdulaziz M., Ashwaq A. Almutairi, and Mohammed Almutairi. 2025. "Physical Inactivity and Cardiovascular Health in Aging Populations: Epidemiological Evidence and Policy Implications from Riyadh, Saudi Arabia" Life 15, no. 3: 347. https://doi.org/10.3390/life15030347
APA StyleAlodhialah, A. M., Almutairi, A. A., & Almutairi, M. (2025). Physical Inactivity and Cardiovascular Health in Aging Populations: Epidemiological Evidence and Policy Implications from Riyadh, Saudi Arabia. Life, 15(3), 347. https://doi.org/10.3390/life15030347






