Hiatal Hernias Revisited—A Systematic Review of Definitions, Classifications, and Applications
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akerlund, A.I. Hernia diaphragmatica hiatus oesophagei vom anatomischen und rontgenologischen gesichtspunkt. Acta Radiol. 1926, 6, 3–22. [Google Scholar] [CrossRef]
- Guthrie, D.; Jones, F.H. The frequency and diagnosis of hiatal hernia. Ann. Surg. 1940, 111, 971–978. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harrington, S.W. The Surgical Treatment of the More Common Type of Diaphragmatic Hernia: Report of 404 Cases. Ann. Surg. 1945, 122, 546–568. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stapleton, J.G. Oesophageal hiatus hernia. Can. Med. Assoc. J. 1947, 57, 13–16. [Google Scholar] [PubMed] [PubMed Central]
- Trueman, K.R. Diagnosis and treatment of para-oesophageal hiatus hernia. Can. Med. Assoc. J. 1947, 56, 149–153. [Google Scholar] [PubMed] [PubMed Central]
- Allison, P.R. Peptic ulcer of the oesophagus. Thorax 1948, 3, 20–42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Olsen, A.M.; Harrington, S.W. Esophageal hiatal hernias of the short esophagus type; etiologic and therapeutic considerations. J. Thorac. Surg. 1948, 17, 189–209. [Google Scholar] [CrossRef] [PubMed]
- Merendino, K.A.; Varco, R.L.; Wangensteen, O.H. Displacement of the Esophagus into a New Diaphragmatic Orifice in the Repair of Paraesophageal and Esophageal Hiatus Hernia. Ann. Surg. 1949, 129, 185–197. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stephens, H.B. The problem of the acquired short esophagus; report of 18 patients. Calif. Med. 1949, 71, 385–390. [Google Scholar] [PubMed] [PubMed Central]
- Kaplan, S. Oesophageal hiatus hernia. A clinical study of 45 cases. Postgrad. Med. J. 1951, 27, 165–177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Sweet, R.H. Esophageal hiatus hernia of the diaphragm; the anatomical characteristics, technic of repair, and results of treatment in 111 consecutive cases. Ann. Surg. 1952, 135, 1–13. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barrett, N.R. Hiatus hernia. Proc. R. Soc. Med. 1952, 45, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Macdougall, J.T.; Abbott, A.C. Sliding hiatus hernia; a review of cases. Can. Med. Assoc. J. 1957, 77, 752–756. [Google Scholar] [PubMed] [PubMed Central]
- Barrett, N.R. Hiatus hernia. Br. Med. J. 1960, 2, 247–252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Collis, J.L. A review of surgical results in hiatus hernia. Thorax 1961, 16, 114–119. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Paulson, D.L.M.; Shaw, R.R.M.; Kee, J.L.M. Esophageal hiatal diaphragmatic hernia and its complications. Ann. Surg. 1962, 155, 957–970. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Borgeskov, S.; Pedersen, O.T.; Frederiksen, T. Oesophageal Hiatal Hernia: A Radiological Follow-up. Thorax 1964, 19, 327–331. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Edwards, D.A.W.; Phillips, S.F.; Rowlands, E.N. Clinical and Radiological Results of Repair of Hiatus Hernia. Br. Med. J. 1964, 2, 714–718. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Brindley, G.V. Surgical Treatment of Complications of Esopliageal Hiatal Hernia. Ann. Surg. 1965, 161, 723–731. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Clagett, O.T. Present concepts regarding the surgical treatment of oesophageal hiatal hernia. Ann. R. Coll. Surg. Engl. 1966, 38, 195–209. [Google Scholar] [PubMed] [PubMed Central]
- Krupp, S.; Rossetti, M. Surgical treatment of hiatal hernias by fundoplication and gastropexy (Nissen repair). Ann. Surg. 1966, 164, 927–934. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zellos, S. Surgical treatment of hiatal hernia, with particular reference to the transthoracic subdiaphragmatic approach. Thorax 1966, 21, 295–304. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Skinner, D.B.; Belsey, R.H. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J. Thorac. Cardiovasc. Surg. 1967, 53, 33–54. [Google Scholar] [CrossRef] [PubMed]
- Hill, L.D. An effective operation for hiatal hernia: An eight year appraisal. Ann. Surg. 1967, 166, 681–692. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nissen, R.; Pfeifer, K. Aktuelle Probleme in der Chirurgie: Zwerchfellhernien; Verlag Hans Huber Bern: Bern, Switzerland, 1967; pp. 31–72. [Google Scholar]
- Borrie, J. Surgical treatment of hiatal hernia: A 10-year survey. Thorax 1967, 22, 344–350. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Hamelmann, H. Hiatal hernias in adults. Langenbecks Arch. Chir. 1968, 322, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Allison, P.R. Hiatus hernia: (a 20-year retrospective survey). Ann. Surg. 1973, 178, 273–276. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hoffman, E.; Sumner, M.C. A clinical and radiological review of 204 hiatal hernia operations. Thorax 1973, 28, 379–385. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- Mokka, R.E.; Laitinen, S.; Punto, L.; Kairaluoma, M.I.; Pokela, R.; Kärkölä, P.; Huttunen, R.; Larmi, T.K. Hiatal hernia repair. Ann. Chir. Gynaecol. 1976, 65, 369–375. [Google Scholar] [PubMed]
- Jacobsson, S.I. Hiatal hernia. Follow-up of a ten-year material. Acta Chir. Scand. Suppl. 1976, 464, 1–28. [Google Scholar] [PubMed]
- Maher, J.W.; Hollenbeck, J.I.; Woodward, E.R. An analysis of recurrent esophagitis following posterior gastropexy. Ann. Surg. 1978, 187, 227–230. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rossetti, M. Indication et tactique chirurgicales dans le reflux et la hernie hiatale [Surgical indications and tactics in reflux and hiatal hernia]. Rev. Med. Suisse Rom. 1982, 102, 753–756. (In French) [Google Scholar] [PubMed]
- Pearson, F.G.; Cooper, J.D.; Ilves, R.; Todd, T.R.; Jamieson, W.R. Massive hiatal hernia with incarceration: A report of 53 cases. Ann. Thorac. Surg. 1983, 35, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Hallissey, M.T.; Ratliff, D.A.; Temple, J.G. Paraoesophageal hiatus hernia: Surgery for all ages. Ann. R. Coll. Surg. Engl. 1992, 74, 23–25. [Google Scholar] [PubMed] [PubMed Central]
- Kuster, G.G.; Gilroy, S. Laparoscopic technique for repair of paraesophageal hiatal hernias. J. Laparoendosc. Surg. 1993, 3, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Menguy, R. Le traitement chirugical des hernies hiatales par roulement avec volvulus intrathoracique de la totalité de l’estomac [Surgical treatment of paraesophageal hiatal hernia with total intrathoracic volvulus of the stomach]. Chirurgie 1994, 120, 439–442; discussion 442–443. (In French) [Google Scholar] [PubMed]
- Jamieson, G.G.; Watson, D.I.; Britten-Jones, R.; Mitchell, P.C.; Anvari, M. Laparoscopic Nissen fundoplication. Ann. Surg. 1994, 220, 137–145. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oddsdottir, M.; Franco, A.L.; Laycock, W.S.; Waring, J.P.; Hunter, J.G. Laparoscopic repair of paraesophageal hernia. New access, old technique. Surg. Endosc. 1995, 9, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Myers, G.A.; Harms, B.A.; Starling, J.R. Management of paraesophageal hernia with a selective approach to antireflux surgery. Am. J. Surg. 1995, 170, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Hill, L.D.; Kozarek, R.A.; Kraemer, S.J.; Aye, R.W.; Mercer, C.D.; Low, D.E.; Pope, C.E., 2nd. The gastroesophageal flap valve: In vitro and in vivo observations. Gastrointest. Endosc. 1996, 44, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Perdikis, G.; Hinder, R.A.; Filipi, C.J.; Walenz, T.; McBride, P.J.; Smith, S.L.; Katada, N.; Klingler, P.J. Laparoscopic paraesophageal hernia repair. Arch. Surg. 1997, 132, 586–589; discussion 590–591. [Google Scholar] [CrossRef] [PubMed]
- Edye, M.B.; Canin-Endres, J.; Gattorno, F.; Salky, B.A. Durability of laparoscopic repair of paraesophageal hernia. Ann. Surg. 1998, 228, 528–535. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Altorki, N.K.; Yankelevitz, D.; Skinner, D.B. Massive hiatal hernias: The anatomic basis of repair. J. Thorac. Cardiovasc. Surg. 1998, 115, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Maziak, D.E.; Todd, T.R.; Pearson, F.G. Massive hiatus hernia: Evaluation and surgical management. J. Thorac. Cardiovasc. Surg. 1998, 115, 53–60; discussion 61–62. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.S.; Dunnegan, D.L.; Soper, N.J. Clinical and radiologic assessment of laparoscopic paraesophageal hernia repair. Surg. Endosc. 1999, 13, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Swanstrom, L.L.; Jobe, B.A.; Kinzie, L.R.; Horvath, K.D. Esophageal motility and outcomes following laparoscopic paraesophageal hernia repair and fundoplication. Am. J. Surg. 1999, 177, 359–363. [Google Scholar] [CrossRef] [PubMed]
- Luketich, J.D.; Raja, S.; Fernando, H.C.; Campbell, W.; Christie, N.A.; Buenaventura, P.O.; Weigel, T.L.; Keenan, R.J.; Schauer, P.R. Laparoscopic repair of giant paraesophageal hernia: 100 consecutive cases. Ann. Surg. 2000, 232, 608–618. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dahlberg, P.S.; Deschamps, C.; Miller, D.L.; Allen, M.S.; Nichols, F.C.; Pairolero, P.C. Laparoscopic repair of large paraesophageal hiatal hernia. Ann. Thorac. Surg. 2001, 72, 1125–1129. [Google Scholar] [CrossRef] [PubMed]
- Champion, J.K.; Rock, D. Laparoscopic mesh cruroplasty for large paraesophageal hernias. Surg. Endosc. 2003, 17, 551–553. [Google Scholar] [CrossRef] [PubMed]
- Leeder, P.C.; Smith, G.; Dehn, T.C. Laparoscopic management of large paraesophageal hiatal hernia. Surg. Endosc. 2003, 17, 1372–1375. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.J.; Tan, B.B.; Yee, J.; Orringer, M.B.; Iannettoni, M.D. A 25-year experience with open primary transthoracic repair of paraesophageal hiatal hernia. J. Thorac. Cardiovasc. Surg. 2004, 127, 843–849. [Google Scholar] [CrossRef] [PubMed]
- Andujar, J.J.; Papasavas, P.K.; Birdas, T.; Robke, J.; Raftopoulos, Y.; Gagné, D.J.; Caushaj, P.F.; Landreneau, R.J.; Keenan, R.J. Laparoscopic repair of large paraesophageal hernia is associated with a low incidence of recurrence and reoperation. Surg. Endosc. 2004, 18, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Targarona, E.M.; Novell, J.; Vela, S.; Cerdán, G.; Bendahan, G.; Torrubia, S.; Kobus, C.; Rebasa, P.; Balague, C.; Garriga, J.; et al. Mid term analysis of safety and quality of life after the laparoscopic repair of paraesophageal hiatal hernia. Surg. Endosc. 2004, 18, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Zaninotto, G.; Portale, G.; Costantini, M.; Rizzetto, C.; Guirroli, E.; Ceolin, M.; Salvador, R.; Rampado, S.; Prandin, O.; Ruol, A.; et al. Long-term results (6–10 years) of laparoscopic fundoplication. J. Gastrointest. Surg. 2007, 11, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Boushey, R.P.; Moloo, H.; Burpee, S.; Schlachta, C.M.; Poulin, E.C.; Haggar, F.; Trottier, D.C.; Mamazza, J. Laparoscopic repair of paraesophageal hernias: A Canadian experience. Can. J. Surg. 2008, 51, 355–360. [Google Scholar] [PubMed] [PubMed Central]
- Luketich, J.D.; Nason, K.S.; Christie, N.A.; Pennathur, A.; Jobe, B.A.; Landreneau, R.J.; Schuchert, M.J. Outcomes after a decade of laparoscopic giant paraesophageal hernia repair. J. Thorac. Cardiovasc. Surg. 2010, 139, 395–404, 404.e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mittal, S.K.; Bikhchandani, J.; Gurney, O.; Yano, F.; Lee, T. Outcomes after repair of the intrathoracic stomach: Objective follow-up of up to 5 years. Surg. Endosc. 2011, 25, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Pallabazzer, G.; Santi, S.; Parise, P.; Solito, B.; Giusti, P.; Rossi, M. Giant hiatal hernias: Direct hiatus closure has an acceptable recurrence rate. Updates Surg. 2011, 63, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Carrott, P.W.; Hong, J.; Kuppusamy, M.; Kirtland, S.; Koehler, R.P.; Low, D.E. Repair of giant paraesophageal hernias routinely produces improvement in respiratory function. J. Thorac. Cardiovasc. Surg. 2012, 143, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Lugaresi, M.; Mattioli, S.; Aramini, B.; D’Ovidio, F.; Di Simone, M.P.; Perrone, O. The frequency of true short oesophagus in type II-IV hiatal hernia. Eur. J. Cardiothorac. Surg. 2013, 43, e30–e36. [Google Scholar] [CrossRef] [PubMed]
- Bjelović, M.; Babic, T.; Gunjić, D.; Veselinović, M.; Spica, B. Laparoscopic repair of hiatal hernias: Experience after 200 consecutive cases. Srp. Arh. Celok. Lek. 2014, 142, 424–430. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Latzko, M.; Borao, F.; Squillaro, A.; Mansson, J.; Barker, W.; Baker, T. Laparoscopic repair of paraesophageal hernias. JSLS J. Soc. Laparosc. Robot. Surg. 2014, 18, e2014.00009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chang, C.G.; Thackeray, L. Laparoscopic Hiatal Hernia Repair in 221 Patients: Outcomes and Experience. JSLS J. Soc. Laparosc. Robot. Surg. 2016, 20, e2015.00104. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Stringham, J.R.; Phillips, J.V.; McMurry, T.L.; Lambert, D.L.; Jones, D.R.; Isbell, J.M.; Lau, C.L.; Kozower, B.D. Prospective study of giant paraesophageal hernia repair with 1-year follow-up. J. Thorac. Cardiovasc. Surg. 2017, 154, 743–751. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mertens, A.C.; Tolboom, R.C.; Zavrtanik, H.; Draaisma, W.A.; Broeders, I.A.M.J. Morbidity and mortality in complex robot-assisted hiatal hernia surgery: 7-year experience in a high-volume center. Surg. Endosc. 2019, 33, 2152–2161. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.; Boyan, W.; Decker, J.; Almagno, V.; Binenbaum, S.; Matharoo, G.; Squillaro, A.; Borao, F. Emergent Repair of Paraesophageal Hernias and the Argument for Elective Repair. JSLS J. Soc. Laparosc. Robot. Surg. 2019, 23, e2019.00015. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dara, V.; Croo, A.; Peirsman, A.; Pattyn, P. Necessity of fundoplication and mesh in the repair of the different types of paraesophageal hernia. Acta Gastroenterol. Belg. 2019, 82, 251–256. [Google Scholar] [PubMed]
- Sorial, R.K.; Ali, M.; Kaneva, P.; Fiore, J.F., Jr.; Vassiliou, M.; Fried, G.M.; Feldman, L.S.; Ferri, L.E.; Lee, L.; Mueller, C.L. Modern era surgical outcomes of elective and emergency giant paraesophageal hernia repair at a high-volume referral center. Surg. Endosc. 2020, 34, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, K.H.; Breithaupt, W.; Varga, G.; Babic, B.; Schulz, T.; Meining, A. Primary laparoscopic fundoplication in selected patients with gastroesophageal reflux disease. Dis. Esophagus 2022, 35, doab032. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Luna, M.R.; Pizzicannella, M.; Fiorillo, C.; Almuttawa, A.; Lapergola, A.; Mutter, D.; Marrescaux, J.; Dallemagne, B.; Perretta, S. Impact of surgical repair on type IV paraesophageal hernias (PEHs). Surg. Endosc. 2022, 36, 5467–5475. [Google Scholar] [CrossRef] [PubMed]
- D’Elia, M.A.; Ahmadi, N.; Jarrar, A.; Neville, A.; Mamazza, J. Paraesophageal hernia repair in elderly patients: Outcomes from a 10-year retrospective study. Can. J. Surg. 2022, 65, E121–E127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Amundson, J.R.; Kuchta, K.; Wu, H.; VanDruff, V.N.; Haggerty, S.P.; Linn, J.; Ujiki, M.B. A 13-year experience with biologic and biosynthetic absorbable mesh reinforced laparoscopic paraesophageal hernia repair. Surg. Endosc. 2023, 37, 7271–7279. [Google Scholar] [CrossRef] [PubMed]
- Salvador, R.; Vittori, A.; Capovilla, G.; Riccio, F.; Nezi, G.; Forattini, F.; Provenzano, L.; Nicoletti, L.; Moletta, L.; Costantini, A.; et al. Antireflux Surgery’s Lifespan: 20 Years After Laparoscopic Fundoplication. J. Gastrointest. Surg. 2023, 27, 2325–2335. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Giulini, L.; Razia, D.; Latorre-Rodríguez, A.R.; Shacker, M.; Csucska, M.; Mittal, S.K. Surgical Repair of Large Hiatal Hernias: Insight from a High-Volume Center. J. Gastrointest. Surg. 2023, 27, 2308–2315. [Google Scholar] [CrossRef] [PubMed]
- Furnée, E.J.; Draaisma, W.A.; Gooszen, H.G.; Hazebroek, E.J.; Smout, A.J.; Broeders, I.A. Tailored or routine addition of an antireflux fundoplication in laparoscopic large hiatal hernia repair: A comparative cohort study. World J. Surg. 2011, 35, 78–84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dallemagne, B.; Kohnen, L.; Perretta, S.; Weerts, J.; Markiewicz, S.; Jehaes, C. Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann. Surg. 2011, 253, 291–296. [Google Scholar] [CrossRef]
- Stylopoulos, N.; Rattner, D.W. The history of hiatal hernia surgery: From Bowditch to laparoscopy. Ann. Surg. 2005, 241, 185–193. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gyawali, C.P.; Kahrilas, P.J.; Savarino, E.; Zerbib, F.; Mion, F.; Smout, A.J.P.M.; Vaezi, M.; Sifrim, D.; Fox, M.R.; Vela, M.F.; et al. Modern diagnosis of GERD: The Lyon Consensus. Gut 2018, 67, 1351–1362. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kahrilas, P.J.; Kim, H.C.; Pandolfino, J.E. Approaches to the diagnosis and grading of hiatal hernia. Best. Pract. Res. Clin. Gastroenterol. 2008, 22, 601–616. [Google Scholar] [CrossRef] [PubMed]
- DeMeester, T.R. Etiology and Natural History of Gastroesophageal Reflux Disease and Predictors of progressive Disease. In Shackelford’s Surgery of the Alimentary Tract, 8th ed.; Yeo, C.J., DeMeester, S.R., Fadden, D.W.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 204–220. [Google Scholar]
- Fuchs, K.H.; DeMeester, T.R.; Otte, F.; Broderick, R.C.; Breithaupt, W.; Varga, G.; Musial, F. Severity of GERD and disease progression. Dis. Esophagus 2021, 34, doab006. [Google Scholar] [CrossRef] [PubMed]
- DeMeester, T.R.; Johnson, L.F.; Joseph, G.J.; Toscano, M.S.; Hall, A.W.; Skinner, D.B. Patterns of gastroesophageal reflux in health and disease. Ann. Surg. 1976, 184, 459–470. [Google Scholar] [CrossRef]
- Costantini, M.; Crookes, P.F.; Bremner, R.M.; Hoeft, S.F.; Ehsan, A.; Peters, J.H.; Bremner, C.G.; DeMeester, T.R. Value of physiologic assessment of foregut symptoms in a surgical practice. Surgery 1993, 114, 780–786. [Google Scholar] [PubMed]
- Tack, J.; Caenepeel, P.; Arts, J.; Lee, K.J.; Sifrim, D.; Janssens, J. Prevalence of acid reflux functional dyspepsia and its association with symptom profile. Gut 2005, 54, 1370–1376. [Google Scholar] [CrossRef] [PubMed]
- Rydberg, L.; Ruth, M.; Abrahamsson, H.; Lundell, L. Tailoring antireflux surgery: A randomized clinical trial. World J. Surg. 1999, 23, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Fibbe, C.; Layer, P.; Keller, J.; Strate, U.; Emmermann, A.; Zornig, C. Esophageal motility in reflux disease before and after fundoplication: A prospective, randomized, clinical, and manometric study. Gastroenterology 2001, 121, 5–14. [Google Scholar] [CrossRef]
- Dallemagne, B.; Weertz, J.; Markiewicz, S.; Dewandre, J.M.; Wahlen, C.; Monami, B.; Jehaes, C. Clinical results of laparoscopic fundoplication ten years after surgery. Surg. Endosc. 2006, 20, 159–165. [Google Scholar] [CrossRef]
- Frantzides, C.T.; Madan, A.K.; Carlson, M.A.; Stavropoulos, G.P. A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs simple cruroplasty for large hiatal hernia. Arch. Surg. 2002, 137, 649–652. [Google Scholar] [CrossRef]
- Granderath, F.A.; Schweiger, U.M.; Kamolz, T.; Pasiut, M.; Haas, C.F.; Pointner, R. Laparoscopic antireflux surgery with routine mesh-hiatoplasty in the treatment of gastroesophageal reflux disease. J. Gastrointest. Surg. 2002, 6, 347–353. [Google Scholar] [CrossRef]
- Bonavina, L.; DeMeester, T.; Fockens, P.; Dunn, D.; Saino, G.; Bona, D.; Lipham, J.; Bemelman, W.; Ganz, R.A. Laparoscopic sphincter augmentation device eliminates reflux symptoms and normalizes esophageal acid exposure: One- and 2-year results of a feasibility trial. Ann. Surg. 2010, 252, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Jobe, B.A.; Richter, J.E.; Hoppo, T.; Peters, J.H.; Bell, R.; Dengler, W.C.; DeVault, K.; Fass, R.; Gyawali, C.P.; Kahrilas, P.J.; et al. Preoperative diagnostic workup before antireflux surgery: An evidence and experience-based consensus of the Esophageal Diagnostic Advisory Panel. J. Am. Coll. Surg. 2013, 217, 586–597. [Google Scholar] [CrossRef]
- Linke, G.R.; Gehrig, T.; Hogg, L.V.; Göhl, A.; Kenngott, H.; Schäfer, F.; Fischer, L.; Gutt, C.N.; Müller-Stich, B.P. Laparoscopic mesh-augmented hiatoplasty without fundoplication as a method to treat large hiatal hernias. Surg. Today 2014, 44, 820–826. [Google Scholar] [CrossRef] [PubMed] [PubMed Central][Green Version]
- DeMeester, S.R. Laparoscopic paraesophageal hernia repair: Critical steps and adjunct techniques to minimize recurrence. Surg. Laparosc. Endosc. Percutan Tech. 2013, 23, 429–435. [Google Scholar] [CrossRef]
- Gerdes, S.; Schoppmann, S.F.; Bonavina, L.; Boyle, N.; Müller-Stich, B.P.; Gutschow, C.A.; Hiatus Hernia Delphi Collaborative Group. Management of paraesophageal hiatus hernia: Recommendations following a European expert Delphi consensus. Surg. Endosc. 2023, 37, 4555–4565. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fuchs, K.H.; Babic, B.; Breithaupt, W.; Dallemagne, B.; Fingerhut, A.; Furnee, E.; Granderath, F.; Horvath, O.P.; Kardos, P.; Pointner, R.; et al. EAES recommendations for the management of Gastroesophageal reflux Disease. Surg. Endosc. 2014, 28, 1753–1773. [Google Scholar] [CrossRef] [PubMed]
- Tolone, S.; Savarino, E.; Zaninotto, G.; Gyawali, C.P.; Frazzoni, M.; de Bortoli, N.; Frazzoni, L.; Del Genio, G.; Bodini, G.; Furnari, M.; et al. High-resolution manometry is superior to endoscopy and radiology in assessing and grading sliding hiatal hernia: A comparison with surgical in vivo evaluation. United Eur. Gastroenterol. J. 2018, 6, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Granderath, F.A.; Schweiger, U.M.; Pointner, R. Laparoscopic antireflux surgery: Tailoring the hiatal closure to the size of hiatal surface area. Surg. Endosc. 2007, 21, 542–548. [Google Scholar] [CrossRef]
- Grubnik, V.V.; Malynovskyy, A.V. Laparoscopic repair of hiatal hernias: New classification supported by long-term results. Surg. Endosc. 2013, 27, 4337–4346. [Google Scholar] [CrossRef] [PubMed]
- Köckerling, F.; Zarras, K.; Adolf, D.; Kraft, B.; Jacob, D.; Weyhe, D.; Schug-Pass, C. What Is the Reality of Hiatal Hernia Management? A Registry Analysis. Front. Surg. 2020, 7, 584196. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
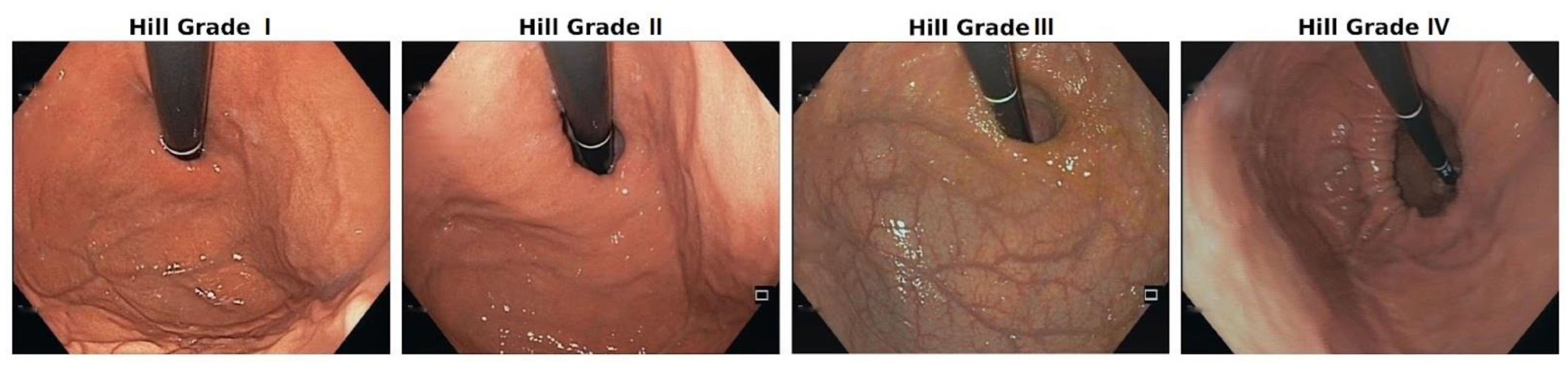
- Kafetzis, I.; Fuchs, K.H.; Sodmann, P.; Troya, J.; Zoller, W.; Meining, A.; Hann, A. Efficient artificial intelligence-based assessment of the gastroesophageal valve with Hill classification through active learning. Sci. Rep. 2024, 14, 18825. [Google Scholar] [CrossRef] [PubMed]

| Number | Definition of Element for Typing | Further Explanations for the Definition |
|---|---|---|
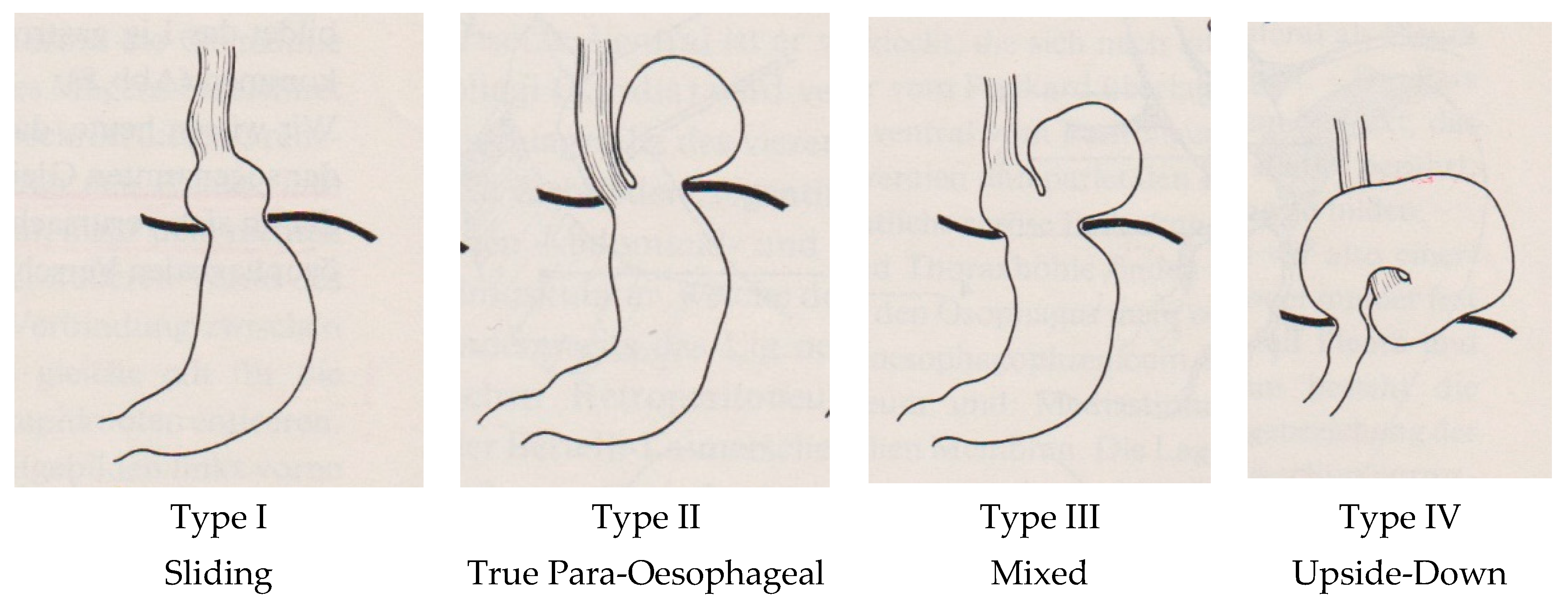
| 1 | True para-oesophageal hernia Akerlund 1926 [1] | The cardia remains at the level of the diaphragm. The hernia develops by rolling up through a small defect in the phreno-oesophageal membrane next to the oesophagus into the mediastinum. |
| 2 | Short oesophagus by congenital predisposition | This phenomenon was described in early experiences with HH and a short oesophagus; this element was only described in the 1930s and 1940s publications, and then it was dropped. |
| 3 | Short oesophagus acquired Collis | The association between oesophagitis and oesophageal shortening was recognised in the 1950s. |
| 4 | Sliding hernia in chest, which develops from small to larger hernias Akerlund 1926 [1] | The proximal stomach is sliding into the mediastinum; thus, the cardia is leaving the level of the diaphragm via the circumferential weakening of the phreno-oesophageal membrane. |
| 5 | Mixed type of hernia Akerlund 1926 [1] | This hernia develops from a sliding hernia with a limited size, in which the stomach migrates into the chest, with the complete proximal part of the stomach (cardia, fundus, and corpus) in the chest. With this process, the oesophagus can shorten. |
| 6 | Other intra-abdominal organs slide into the intrathoracic hernia Skinner and Belsey 1967 [23] | The development of the hernia is huge, causing, under favourable conditions, a migration of the colon, spleen, and/or pancreas into the chest. |
| 7 | Upside-down stomach Skinner and Belsey 1967 [23] | This is a further development of a true para-oesophageal hernia through a small defect in the phreno-oesophageal membrane, causing a further rolling up of the stomach in the chest. Since the cardia remains attached to the diaphragm, the stomach rotates around this fixation upside-down in the mediastinum. |
| Method of Data Demonstration | n Patients | Number of Publications | Publication in References |
|---|---|---|---|
| All types | 8904 | 27 | [10,13,15,17,18,21,33,36,38,41,55,62,64,70,74,75] |
| Selective PEH | 3829 | 33 | [34,35,37,39,40,42,43,44,45,46,47,48,49,50,51,52,53,54,56,57,58,59,60,61,62,63,65,66,67,68,69,71,72,73] |
| Total | 12,733 | 60 | [10,13,15,17,18,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75] |
| Application of Typing | Type I | Type II | Type III | Type IV |
|---|---|---|---|---|
| Typing of complete HH cohort: 8904 patients | 7441 | 413 | 965 | 85 |
| Distribution percentage | 83.6% | 4.3% | 10.8% | 0.9% |
| Typing of selective PEH cohort: 3829 patients | - | 348 | 2951 | 530 |
| Distribution percentage | - | 9.1% | 77.1% | 13.8% |
| Comparison percentage of PEH among the complete HH cohort/n = 1463) (exclusion Type I) | - | 413 28.3% | 965 65.9% | 85 5.8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuchs, K.H.; Kafetzis, I.; Hann, A.; Meining, A. Hiatal Hernias Revisited—A Systematic Review of Definitions, Classifications, and Applications. Life 2024, 14, 1145. https://doi.org/10.3390/life14091145
Fuchs KH, Kafetzis I, Hann A, Meining A. Hiatal Hernias Revisited—A Systematic Review of Definitions, Classifications, and Applications. Life. 2024; 14(9):1145. https://doi.org/10.3390/life14091145
Chicago/Turabian StyleFuchs, Karl Hermann, Ioannis Kafetzis, Alexander Hann, and Alexander Meining. 2024. "Hiatal Hernias Revisited—A Systematic Review of Definitions, Classifications, and Applications" Life 14, no. 9: 1145. https://doi.org/10.3390/life14091145
APA StyleFuchs, K. H., Kafetzis, I., Hann, A., & Meining, A. (2024). Hiatal Hernias Revisited—A Systematic Review of Definitions, Classifications, and Applications. Life, 14(9), 1145. https://doi.org/10.3390/life14091145





