An Update on Mitral Valve Aging
Abstract
1. Introduction
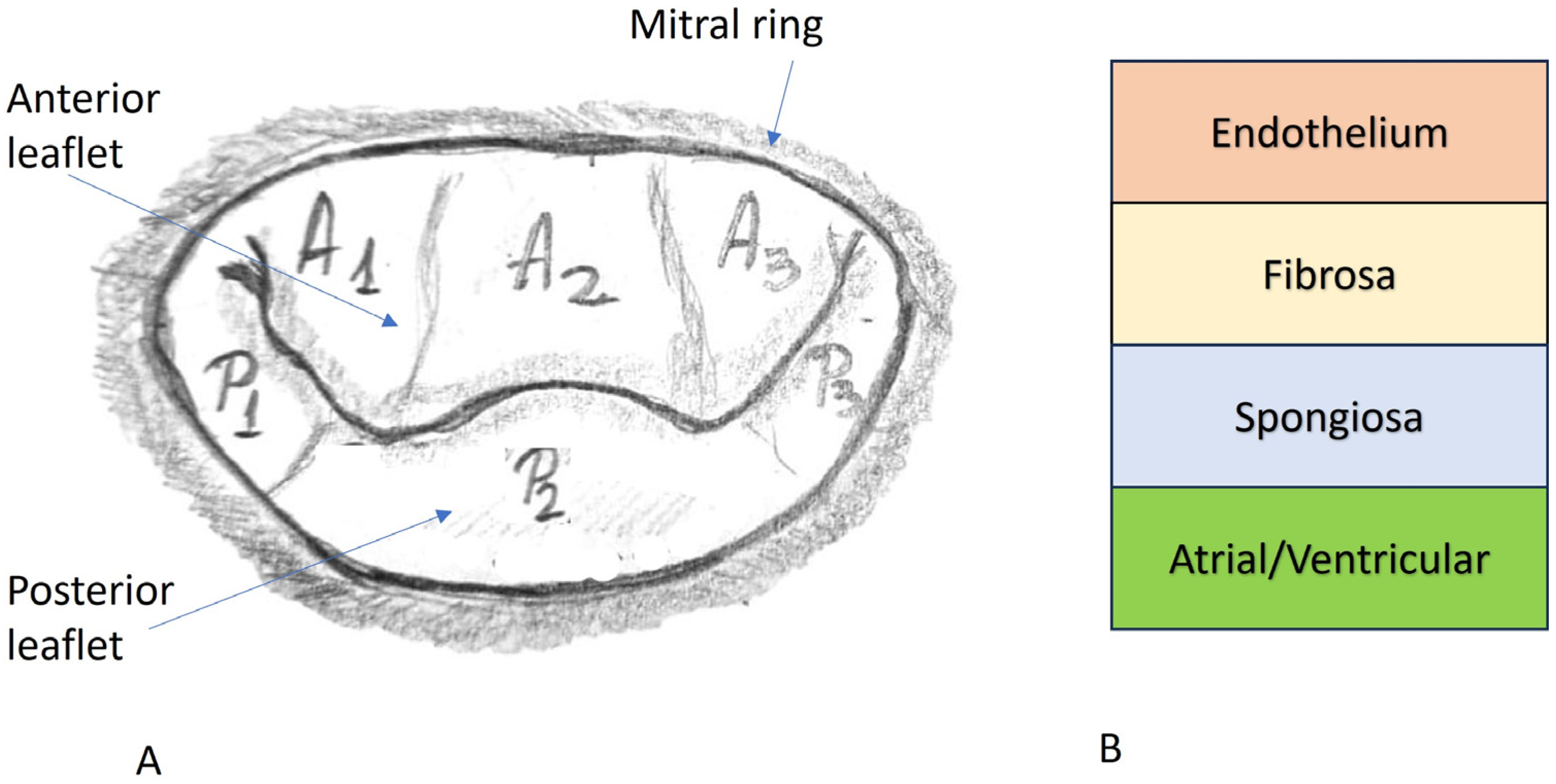
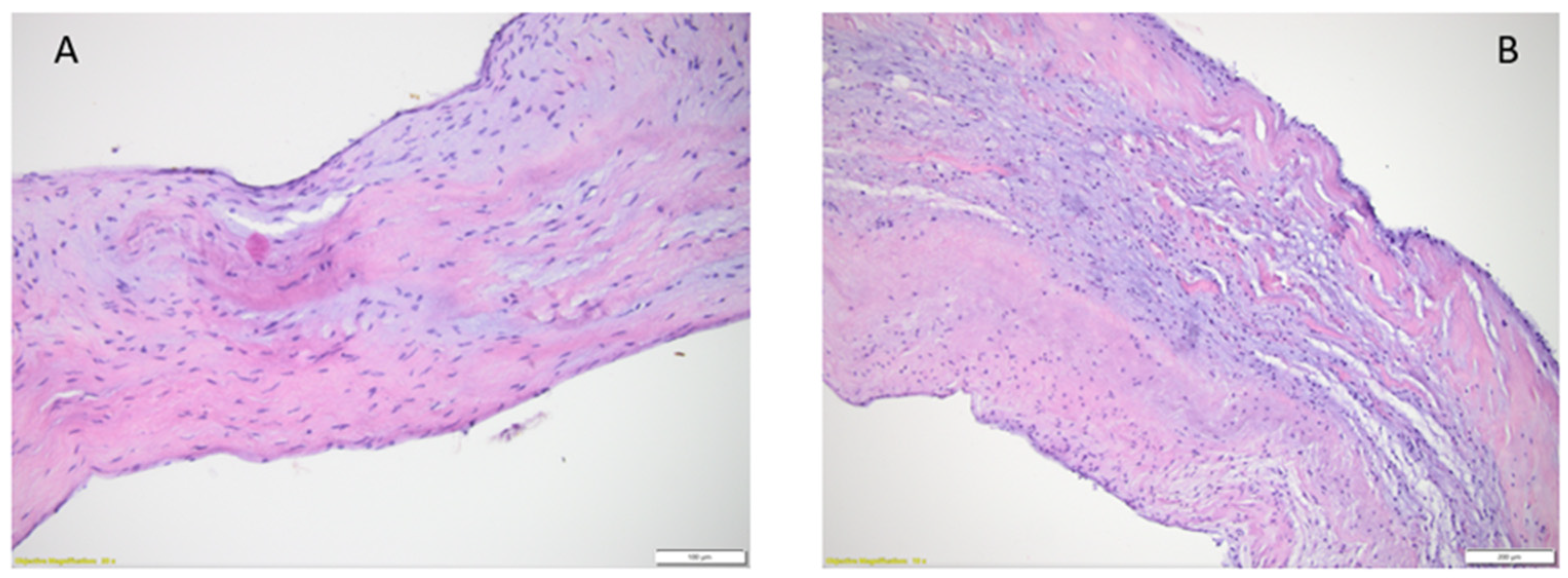
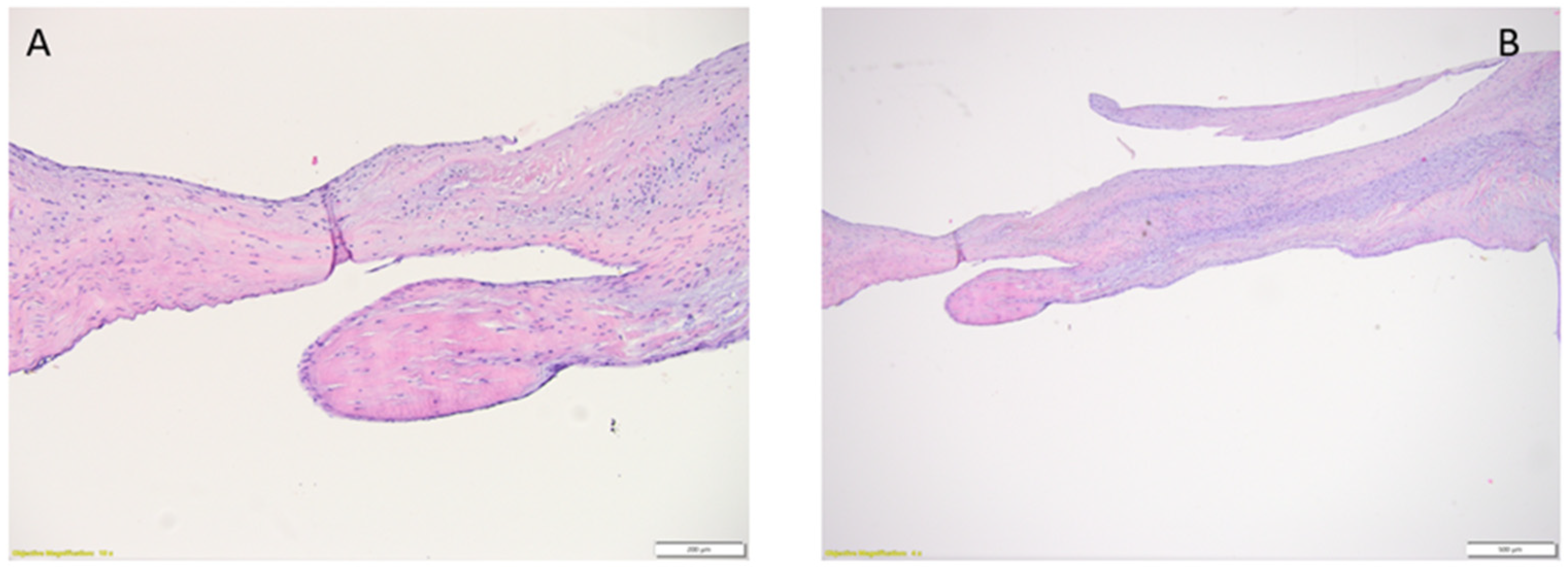
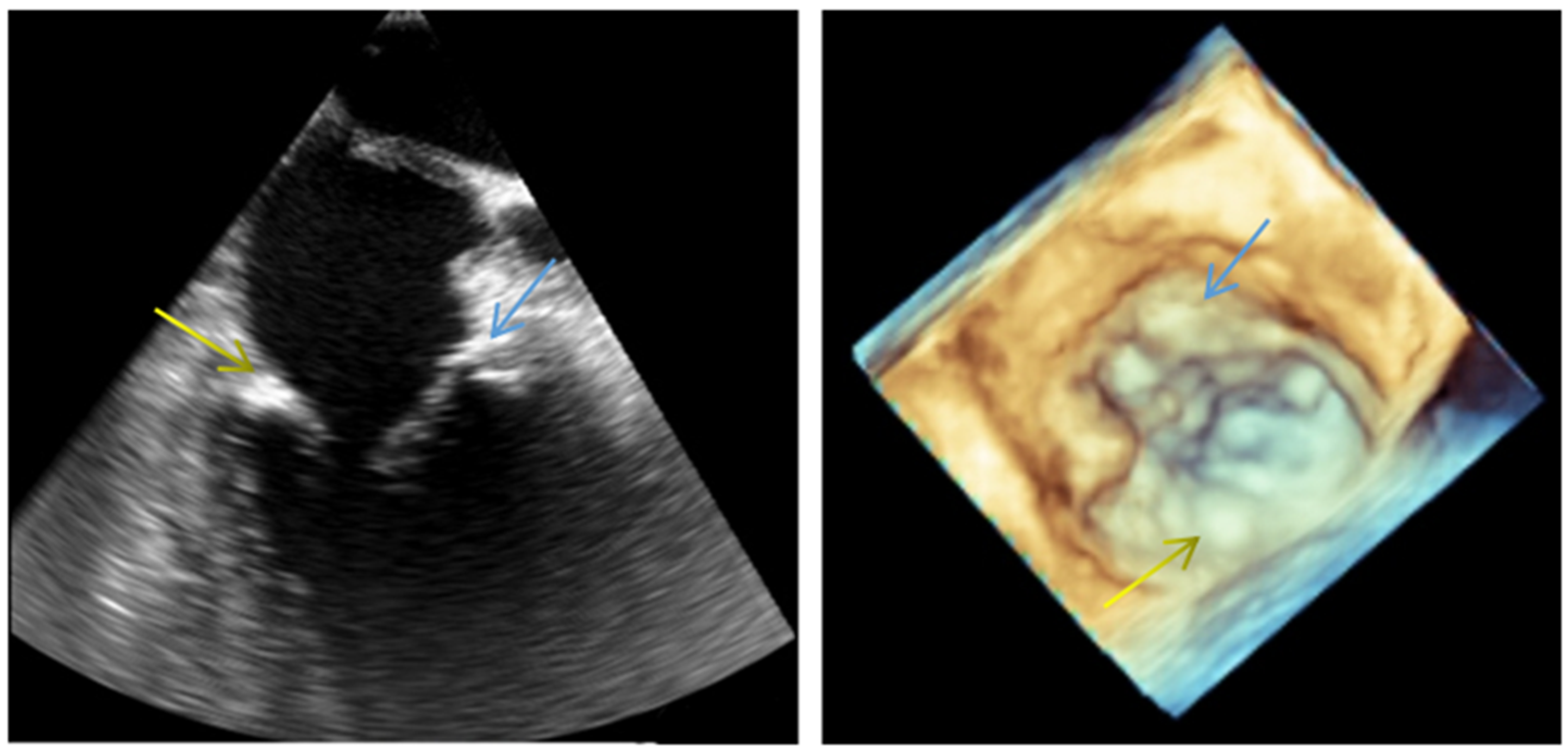
2. Normal Structure of the Mitral Valve
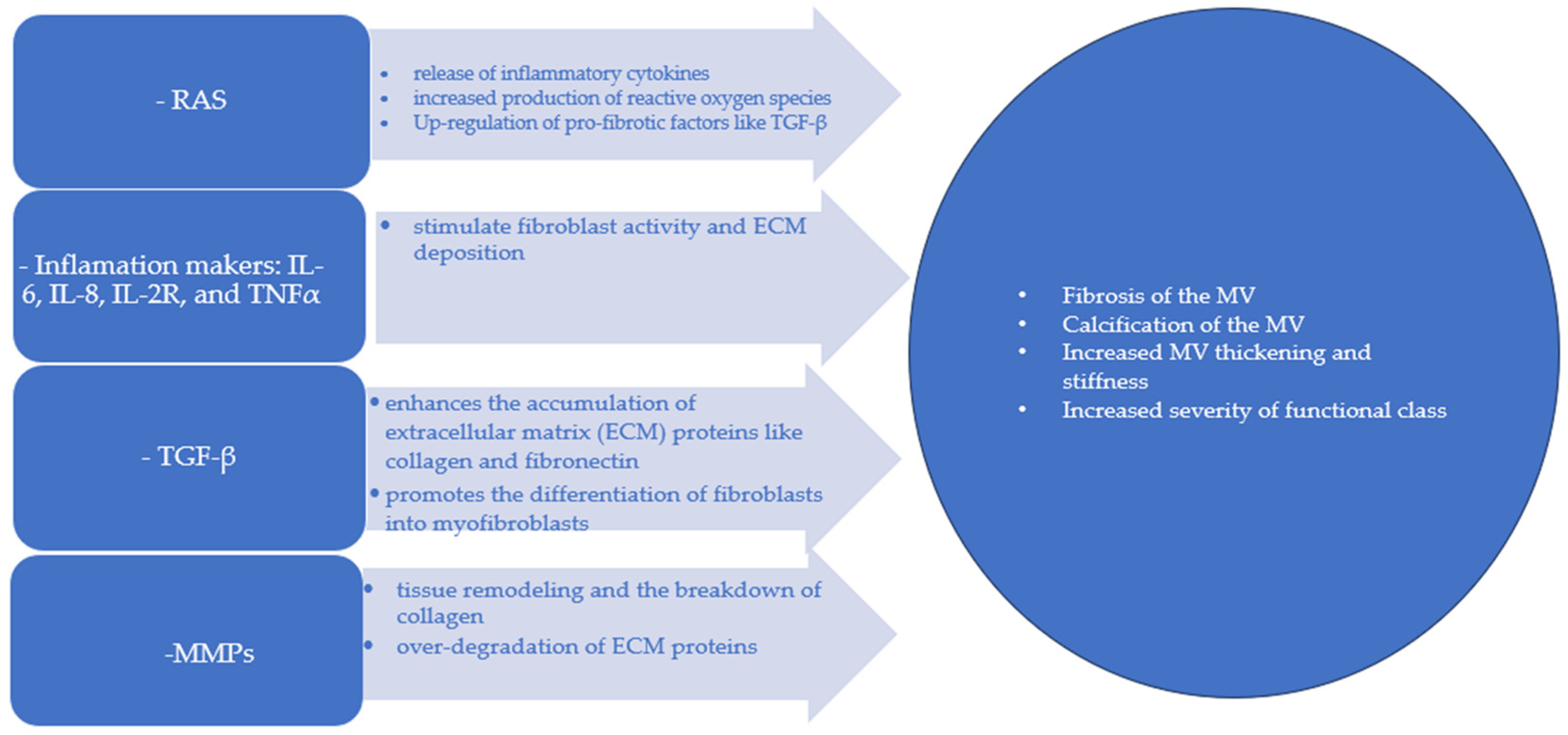
2.1. Mitral Annulus
2.2. Mitral Leaflets
2.3. Chordae Tendineae
2.4. Papillary Muscles and the Ventricular Myocardium
3. Age-Induced Histological Modifications of the Mitral Valve
4. Physiopathology of the Mitral Valve: Age-Induced Modifications
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oosthoek, P.W.; Wenink, A.C.; Wisse, L.J.; Gittenberger-de Groot, A.C. Development of the papillary muscles of the mitral valve: Morphogenetic background of parachute-like asymmetric mitral valves and other mitral valve anomalies. J. Thorac. Cardiovasc. Surg. 1998, 116, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Sanchez Vaca, F.; Bordoni, B. Anatomy, Thorax, Mitral Valve 2023. In StatPearls; StatPearls Publishing: Treasure Island FL, USA, 2024. [Google Scholar] [PubMed]
- Hinton, R.B.; Yutzey, K.E. Heart valve structure and function in development and disease. Annu. Rev. Physiol. 2011, 73, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Perloff, J.K.; Roberts, W.C. The mitral apparatus. Functional anatomy of mitral regurgitation. Circulation 1972, 46, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Angelini, A.; Ho, S.Y.; Anderson, R.H.; Davies, M.J.; Becker, A.E. A histological study of the atrioventricular junction in hearts with normal and prolapsed leaflets of the mitral valve. Br. Heart J. 1988, 59, 712–716. [Google Scholar] [CrossRef]
- Baumgartner, H.; Falk, V.; Bax, J.J.; De Bonis, M.; Hamm, C.; Holm, P.J.; Iung, B.; Lancellotti, P.; Lansac, E.; Rodriguez Muñoz, D.; et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2017, 38, 2739–2791. [Google Scholar] [CrossRef] [PubMed]
- Hollenberg, S.M. Valvular Heart Disease in Adults: Etiologies, Classification, and Diagnosis. FP Essent. 2017, 457, 11–16. [Google Scholar] [PubMed]
- Choong, C.Y.; Abascal, V.M.; Weyman, J.; Levine, R.A.; Gentile, F.; Thomas, J.D.; Weyman, A.E. Prevalence of valvular regurgitation by Doppler echocardiography in patients with structurally normal hearts by two-dimensional echocardiography. Am. Heart J. 1989, 117, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Mills, S.E. (Ed.) Section VI, Thorax and serous membranes. In Histology for Pathologists, 4th ed.; Wolkers Kluwer-Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012; pp. 572–574. [Google Scholar]
- Fishbein, G.A.; Fishbein, M.C. Mitral valve pathology. Curr. Cardiol. Rep. 2019, 21, 61. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.Y. Anatomy of the mitral valve. Heart 2002, 88 (Suppl. S4), iv5–iv10. [Google Scholar] [CrossRef]
- Hagège, A.A.; Carpentier, A.; Levine, R.A. Dynamic changes of the mitral valve annulus: New look at mitral valve diseases. Circ. Cardiovasc. Imaging 2015, 8, 10. [Google Scholar] [CrossRef]
- Harken, D.E.; Ellis, L.B.; Dexter, L.; Farrand, R.E.; Dickson, J.F. The Responsibility of the Physician in the Selection of Patients with Mitral Stenosis for Surgical Treatment. Circulation 1952, 5, 349–362. [Google Scholar] [CrossRef] [PubMed]
- Omran, A.S.; Arifi, A.A.; Mohamed, A.A. Echocardiography of the mitral valve. J. Saudi Heart Assoc. 2010, 22, 165–170. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carpentier, A. Cardiac valve surgery—The French correction. J. Thoracic Cardiovasc. Surg. 2001, 122, 8–15. [Google Scholar] [CrossRef]
- Riggs, T.W.; Lapin, G.D.; Paul, M.H.; Muster, A.J.; Berry, T.E. Measurement of Mitral Valve Orifice Area in Infants and Children by Two-Dimensional Echocardiography. J. Am. Coll. Cardiol. 1983, 3, 873–878. [Google Scholar] [CrossRef]
- Ranganathan, N.; Lam, J.H.; Wigle, E.D.; Silver, M.D. Morphology of the human mitral valve. II. The value leaflets. Circulation 1970, 41, 459–467. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, K.P.; Liam Ring Bushra, S. Rana. Anatomy of the mitral valve: Understanding the mitral valve complex in mitral regurgitation. Eur. J. Echocardiogr. 2010, 11, i3–i9. [Google Scholar] [CrossRef] [PubMed]
- DuPlessis, L.A.; Marchand, P. The anatomy of the mitral valve and its associated structures. Thorax 1964, 19, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Gunnal, S.A.; Wabale, R.N.; Farooqui, M.S. Morphological study of chordae tendinae in human cadaveric hearts. Heart Views 2015, 16, 1–12. [Google Scholar] [CrossRef]
- Chiechi, M.A.; Less, W.M.; Thompson, R. Functional anatomy of the normal mitral valve. J. Thorac. Surg. 1956, 32, 378. [Google Scholar] [CrossRef]
- Kalyanasundaram, A.; Qureshi, A.; Nassef, L.A.; Shirani, J. Functional anatomy of normal mitral valve-left ventricular complex by real-time, three-dimensional echocardiography. J. Heart Valve Dis. 2010, 19, 28–34. [Google Scholar]
- Van der Bel-Kahn, J.; Becker, A.E. The surgical pathology of rheumatic and floppy mitral valves: Distinctive morphologic features upon gross examination. Am. J. Surg. Pathol. 1986, 10, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Roberts, W.C. Morphologic features of the normal and abnormal mitral valve. Am. J. Cardiol. 1983, 51, 1005–1028. [Google Scholar] [CrossRef] [PubMed]
- Harb, S.C.; Griffin, B.P. Mitral valve disease: A comprehensive review. Curr. CArdiol Rep. 2017, 19, 73. [Google Scholar] [CrossRef] [PubMed]
- Saha, A.; Roy, S. Papillary muscles of left ventricle—Morphological variations and it’s clinical relevance. Indian Heart J. 2018, 70, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Kassem, S.; Al-Faraidy, K.; Elkady, Y.; Takriti, A. Face-to-face single patch: A new technique to repair the commissures of the mitral valve. J. Thorac. Cardiovasc. Surg. 2012, 144, 1523–1527. [Google Scholar] [CrossRef]
- Kanzaki, H.; Bazaz, R.; Schwartzman, D.; Dohi, K.; Sade, L.E.; Gorcsan, J. A mechanism for immediate reduction in mitral regurgitation after cardiac resynchronization therapy: Insights from mechanical activation strain mapping. J. Am. Coll. Cardiol. 2004, 44, 1619–1625. [Google Scholar] [CrossRef]
- Sacks, M.S.; He, Z.; Baijens, L.; Wanant, S.; Shah, P.; Sugimoto, H.; Yoganathan, A.P. Surface strains in the anterior leaflet of the functioning mitral valve. Ann. Biomed. Eng. 2002, 30, 1281–1290. [Google Scholar] [CrossRef]
- Parvin Nejad, S.; Blaser, M.C.; Santerre, J.P.; Caldarone, C.A.; Simmons, C.A. Biomechanical conditioning of tissue engineered heart valves: Too much of a good thing? Adv. Drug Deliv. Rev. 2016, 96, 161. [Google Scholar] [CrossRef]
- Gupta, V.; Grande-Allen, K.J. Effects of static and cyclic loading in regulating extracellular matrix synthesis by cardiovascular cells. Cardiovasc. Res. 2006, 72, 375–383. [Google Scholar] [CrossRef]
- Ju, H.; Dixon, I.M. Extracellular matrix and cardiovascular diseases. Can. J. Cardiol. 1996, 12, 1259–1267. [Google Scholar]
- Spadaccio, C.; Mozetic, P.; Nappi, F.; Nenna, A.; Sutherland, F.; Trombetta, M.; Chello, M.; Rainer, A. Cells and extracellular matrix interplay in cardiac valve disease: Because age matters. Basic Res. Cardiol. 2016, 111, 16. [Google Scholar] [CrossRef]
- Rabkin, E.; Aikawa, M.; Stone, J.R.; Fukumoto, Y.; Libby, P.; Schoen, F.J. Activated interstitial myofifibroblasts express catabolic enzymes and mediate matrix remodeling in myxomatous heart valves. Circulation 2001, 104, 2525–2532. [Google Scholar] [CrossRef]
- Fung, Y.C.; Liu, S.Q. Changes of zero-stress state of rat pulmonary arteries in hypoxic hypertension. J. Appl. Physiol. 1991, 70, 2455–2470. [Google Scholar] [CrossRef]
- Tao, G.; Kotick, J.F.; Lincoln, J.; Lincoln, J. Heart valve development, maintenance, and disease: The role of endothelial cells. Curr. Top. Dev. Biol. 2012, 100, 203–232. [Google Scholar] [CrossRef] [PubMed]
- Gumpangseth, T.; Lekawanvijit, S.; Mahakkanukrauh, P. Histological assessment of the human heart valves and its relationship with age. Anat. Cell Biol. 2020, 53, 261–271. [Google Scholar] [CrossRef]
- Kohn, J.C.; Lampi, M.C.; Reinhart-King, C.A. Age-related vascular stiffening: Causes and consequences. Front. Genet. 2015, 6, 112. [Google Scholar] [CrossRef]
- Lin, S.L.; Liu, C.P.; Young, S.T.; Lin, M.; Chiou, C.W. Agerelated changes in aortic valve with emphasis on the relation between pressure loading and thickened leaflflets of the aortic valves. Int. J. Cardiol. 2005, 103, 272–279. [Google Scholar] [CrossRef]
- Yip, C.Y.; Chen, J.H.; Zhao, R.; Simmons, C.A. Calcifification by valve interstitial cells is regulated by the stiffness of the extracellular matrix. Arterioscler. Thromb. Vasc. Biol. 2009, 29, 936–942. [Google Scholar] [CrossRef]
- Balaoing, L.R.; Post, A.D.; Liu, H.; Minn, K.T.; Grande-Allen, K.J. Age-related changes in aortic valve hemostatic protein regulation. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 72–80. [Google Scholar] [CrossRef]
- Pomerance, A. Ageing changes in human heart valves. Br. Heart J. 1967, 29, 222–231. [Google Scholar] [CrossRef] [PubMed]
- Kitzman, D.W.; Scholz, D.G.; Hagen, P.T.; Ilstrup, D.M.; Edwards, W.D. Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): A quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin. Proc. 1988, 63, 137–146. [Google Scholar] [CrossRef]
- Ayoub, S.; Lee, C.H.; Driesbaugh, K.H.; Anselmo, W.; Hughes, C.T.; Ferrari, G.; Gorman, R.C.; Gorman, J.H.; Sacks, M.S. Regulation of valve interstitial cell homeostasis by mechanical deformation: Implications for heart valve disease and surgical repair. J. R. Soc. Interface 2017, 14, 20170580. [Google Scholar] [CrossRef]
- Abramowitz, Y.; Jilaihawi, H.; Chakravarty, T.; Mack, M.J.; Makkar, R.R. Mitral Annulus Calcification. J. Am. Coll Cardiol. 2015, 66, 1934–1941. [Google Scholar] [CrossRef]
- Massera, D.; Trivieri, M.G.; Andrews, J.P.M.; Sartori, S.; Abgral, R.; Chapman, A.R.; Jenkins, W.S.A.; Vesey, A.; Doris, M.; Rawade, T.A.; et al. Disease Activity in Mitral Annular Calcification. Circ. Cardiovasc. Imaging 2019, 12, e008513. [Google Scholar] [CrossRef]
- Aronow, W.S.; Ahn, C.; Kronzon, I. Prevalence of echocardiographic findings in 554 men and in 1,243 women aged > 60 years in a long-term health care facility. Am. J. Cardiol. 1997, 79, 379–380. [Google Scholar] [CrossRef]
- Roberts, W.C.; McIntosh, C.L.; Wallace, R.B. Mechanisms of severe mitral regurgitation in mitral valve prolapse determined from analysis of operatively excised valves. Am. Heart J. 1987, 113, 1316–1323. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Plehn, J.F.; D’Agostino, R.B.; Belanger, A.J.; Comai, K.; Fuller, D.L.; Wolf, P.A.; Levy, D. Mitral annular calcification and the risk of stroke in an elderly cohort. N. Engl. J. Med. 1992, 327, 374–379. [Google Scholar] [CrossRef]
- Hishimura, R.A.; Housmans, P.R.; Hatle, L.K.; Tajik, J. Assessment of Diastolic Function of the Heart: Background and Current Applications of Doppler Echocardiography. Part I. Physiologic and Pathophysiologic Features. Mayo Clin. Proc. 1989, 64, 71–81. [Google Scholar] [CrossRef]
- Silbiger, J.J. Pathophysiology and Echocardiographic Diagnosis of Left Ventricular Diastolic Dysfunction. J. Am. Soc. Echocardiogr. 2019, 32, 216–232.e2. [Google Scholar] [CrossRef]
- Merryman, W.D.; Youn, I.; Lukoff, H.D.; Krueger, P.M.; Guilak, F.; Hopkins, R.A.; Sacks, M.S. Correlation between heart valve interstitial cell stiffness and transvalvular pressure: Implications for collagen biosynthesis. Am. J. Physiol. Heart Circ. Physiol. 2006, 90, H224–H231. [Google Scholar] [CrossRef]
- O’Donnell, A.; Yutzey, K.E. Mechanisms of heart valve development and disease. Development 2020, 147, dev183020. [Google Scholar] [CrossRef] [PubMed]
- de la Torre, J.C. Hemodynamic Instability in Heart Failure Intensifies Age-Dependent Cognitive Decline. J. Alzheimers Dis. 2020, 76, 63–84. [Google Scholar] [CrossRef] [PubMed]
- Mills, W.R.; Barber, J.E.; Ratliff, N.B.; Cosgrove, D.M., 3rd; Vesely, I.; Griffin, B.P. Biomechanical and echocardiographic characterization of flail mitral leaflet due to myxomatous disease: Further evidence for early surgical intervention. Am. Heart J. 2004, 148, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Wight, T.N.; Potter-Perigo, S. The extracellular matrix: An active or passive player in fibrosis? Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 301, G950–G955. [Google Scholar] [CrossRef] [PubMed]
- Van Hemelrijck, M.; Taramasso, M.; Gülmez, G.; Maisano, F.; Mestres, C.A. Mitral annular calcification: Challenges and future perspectives. Indian. J. Thorac. Cardiovasc. Surg. 2020, 36, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.A.; Hagége, A.A.; Judge, D.P.; Padala, M.; Dal-Bianco, J.P.; Aikawa, E.; Beaudoin, J.; Bischoff, J.; Bouatia-Naji, N.; Bruneval, P.; et al. Leducq Mitral Transatlantic Network. Mitral valve disease—Morphology and mechanisms. Nat. Rev. Cardiol. 2015, 12, 689–710. [Google Scholar] [CrossRef] [PubMed]
- Connell, P.S.; Han, R.I.; Grande-Allen, K.J. Differentiating the aging of the mitral valve from human and canine myxomatous degeneration. J. Vet. Cardiol. 2012, 14, 31–45. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.L.; Burstow, D.J.; Tajik, A.J.; Zachariah, P.K.; Taliercio, C.P.; Taylor, C.L.; Bailey, K.R.; Seward, J.B. Age-related prevalence of valvular regurgitation in normal subjects: A comprehensive color flow examination of 118 volunteers. J. Am. Soc. Echocardiogr. 1990, 3, 54–63. [Google Scholar] [CrossRef]
- Enriquez-Sarano, M.; Basmadjian, A.J.; Rossi, A.; Bailey, K.R.; Seward, J.B.; Tajik, A.J. Progression of mitral regurgitation: A prospective Doppler echocardiographic study. J. Am. Coll. Cardiol. 1999, 34, 1137–1144. [Google Scholar] [CrossRef]
- Gerstenblith, G.; Frederiksen, J.; Yin, F.C.; Fortuin, N.J.; Lakatta, E.G.; Weisfeldt, M.L. Echocardiographic assessment of a normal adult aging population. Circulation 1977, 56, 273–278. [Google Scholar] [CrossRef]
- Kitzman, D.W.; Edwards, W.D. Age-related changes in the anatomy of the normal human heart. J. Gerontol. 1990, 45, M33–M39. [Google Scholar] [CrossRef] [PubMed]
- Fares, E.; Howlett, S.E. Effect of age on cardiac excitation-contraction coupling. Clin. Exp. Pharmacol. Physiol. 2010, 37, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Opris, C.E.; Suciu, H.; Flamand, S.; Opris, C.I.; Al Hussein, H.; Gurzu, S. Update on the genetic profile of mitral valve development and prolapse. Pathol. Res. Pract. 2024, in press.
- Forrester, S.J.; Booz, G.W.; Sigmund, C.D.; Coffman, T.M.; Kawai, T.; Rizzo, V.; Scalia, R.; Eguchi, S. Angiotensin II Signal Transduction: An Update on Mechanisms of Physiology and Pathophysiology. Physiol. Rev. 2018, 98, 1627–1738. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, H.; Dhalla, N.S. The Role of pro-inflammatory cytokines in the pathogenesis of cardiovascular disease. Int. J. Mol. Sci. 2024, 25, 1082. [Google Scholar] [CrossRef] [PubMed]
- Ren, L.L.; Miao, H.; Wang, Y.N.; Liu, F.; Li, P.; Zhao, Y.Y. TGF-β as A Master Regulator of Aging-Associated Tissue Fibrosis. Aging Dis. 2023, 14, 1633–1650. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Opris, C.E.; Suciu, H.; Jung, I.; Flamand, S.; Harpa, M.M.; Opris, C.I.; Popa, C.; Kovacs, Z.; Gurzu, S. Significance of Fibrillin-1, Filamin A, MMP2 and SOX9 in mitral valve pathology. Int. J. Mol. Sci. 2024, in press.
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging 2018, 13, 757–772. [Google Scholar] [CrossRef]
- Ambari, A.M.; Setianto, B.; Santoso, A.; Radi, B.; Dwiputra, B.; Susilowati, E.; Tulrahmi, F.; Doevendans, P.A.; Cramer, M.J. Angiotensin Converting Enzyme Inhibitors (ACEIs) Decrease the Progression of Cardiac Fibrosis in Rheumatic Heart Disease Through the Inhibition of IL-33/sST2. Front. Cardiovasc. Med. 2020, 7, 115. [Google Scholar] [CrossRef]
- Antonini-Canterin, F.; Moura, L.M.; Enache, R.; Leiballi, E.; Pavan, D.; Piazza, R.; Popescu, B.A.; Ginghina, C.; Nicolosi, G.L.; Rajamannan, N.M. Effect of hydroxymethylglutaryl coenzyme-a reductase inhibitors on the long-term progression of rheumatic mitral valve disease. Circulation 2010, 121, 2130–2136. [Google Scholar] [CrossRef]
- Boroumand, S.; Haeri, A.; Nazeri, N.; Rabbani, S. Review Insights In Cardiac Tissue Engineering: Cells, Scaffolds, and Pharmacological Agents. Iran. J. Pharm. Res. 2021, 20, 467–496. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Li, T.; Zhu, J. Gene Therapy Strategies Targeting Aging-Related Diseases. Aging Dis. 2023, 14, 398–417. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Opris, C.E.; Suciu, H.; Opris, C.I.; Gurzu, S. An Update on Mitral Valve Aging. Life 2024, 14, 950. https://doi.org/10.3390/life14080950
Opris CE, Suciu H, Opris CI, Gurzu S. An Update on Mitral Valve Aging. Life. 2024; 14(8):950. https://doi.org/10.3390/life14080950
Chicago/Turabian StyleOpris, Carmen Elena, Horatiu Suciu, Cosmin Ioan Opris, and Simona Gurzu. 2024. "An Update on Mitral Valve Aging" Life 14, no. 8: 950. https://doi.org/10.3390/life14080950
APA StyleOpris, C. E., Suciu, H., Opris, C. I., & Gurzu, S. (2024). An Update on Mitral Valve Aging. Life, 14(8), 950. https://doi.org/10.3390/life14080950






