Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study
Abstract
1. Introduction
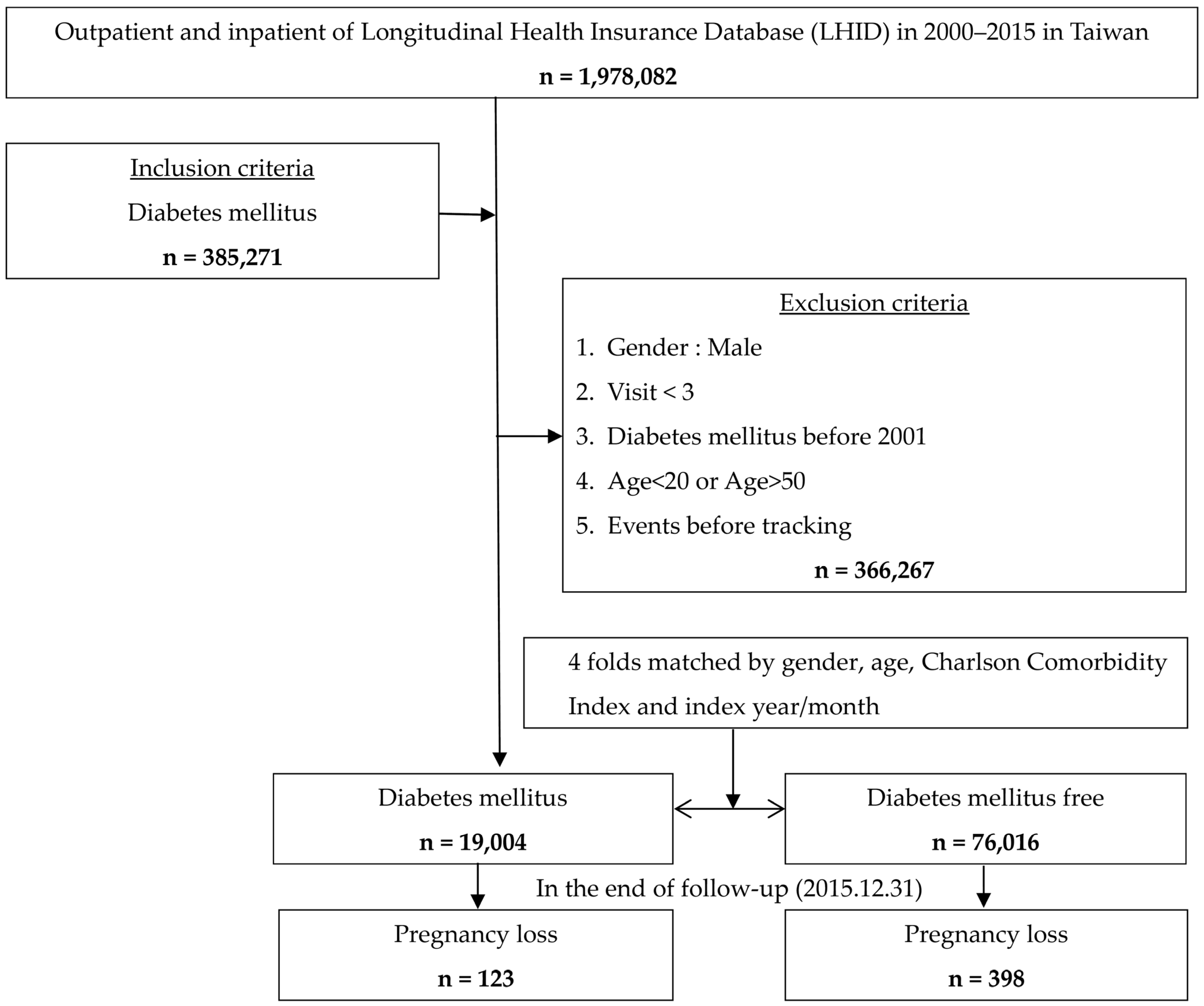
2. Materials and Methods
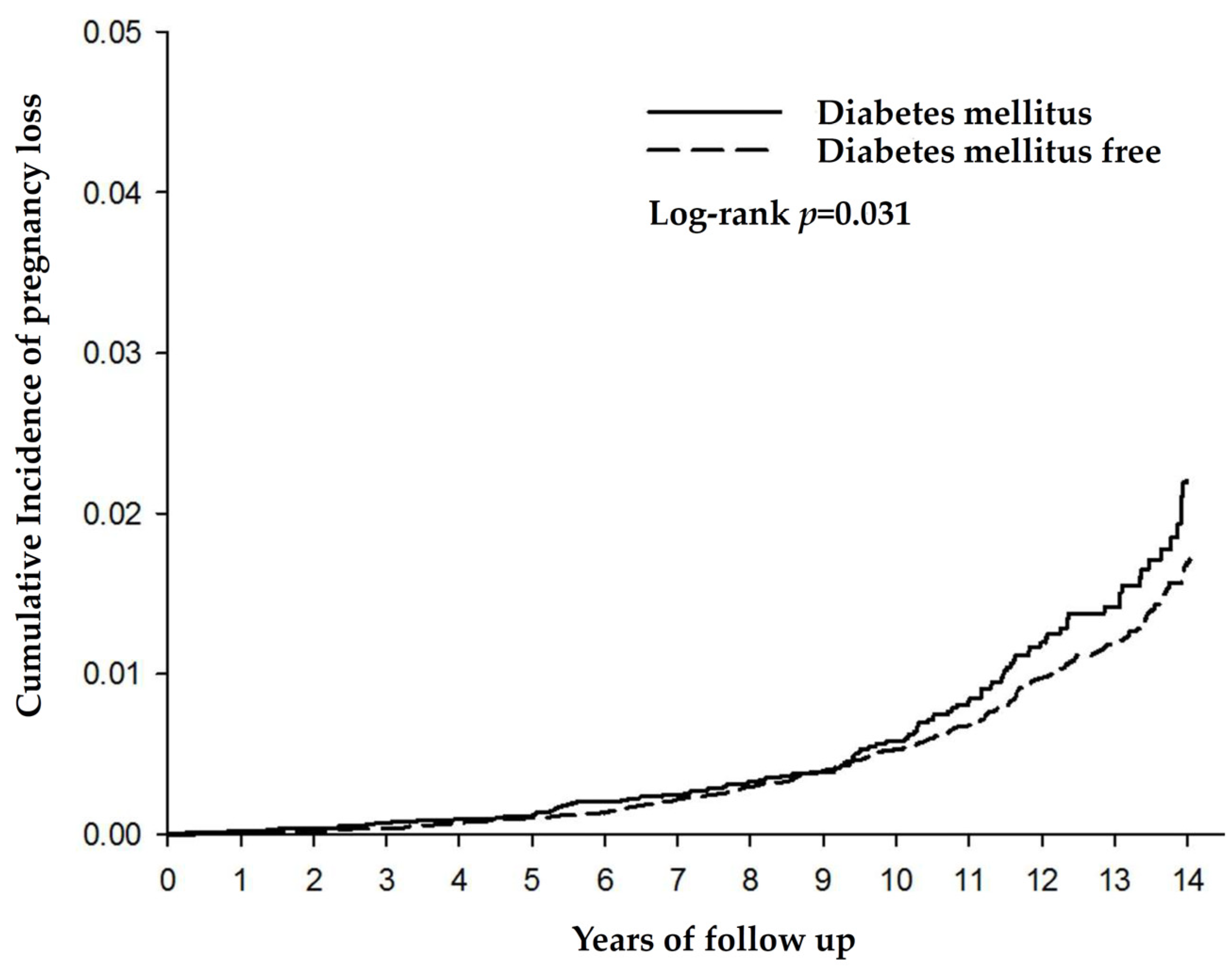
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quenby, S.; Gallos, I.D.; Dhillon-Smith, R.K.; Podesek, M.; Stephenson, M.D.; Fisher, J.; Brosens, J.J.; Brewin, J.; Ramhorst, R.; Lucas, E.S.; et al. Miscarriage matters: The epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet 2021, 397, 1658–1667. [Google Scholar] [CrossRef] [PubMed]
- Lek, S.M.; Ku, C.W.; Allen, J.C., Jr.; Malhotra, R.; Tan, N.S.; Østbye, T.; Tan, T.C. Validation of serum progesterone < 35 nmol/L as a predictor of miscarriage among women with threatened miscarriage. BMC Pregnancy Childbirth 2017, 17, 78. [Google Scholar] [CrossRef]
- Verheijen, E.C.; Critchley, J.A.; Whitelaw, D.C.; Tuffnell, D.J. Outcomes of pregnancies in women with pre-existing type 1 or type 2 diabetes, in an ethnically mixed population. BJOG 2005, 112, 1500–1533. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Xu, Q.; Yang, H.; Yang, Y.; Wang, L.; Chen, H.; Anderson, C.; Liu, X.; Song, G.; Li, Q.; et al. Preconception diabetes mellitus and adverse pregnancy outcomes in over 6.4 million women: A population-based cohort study in China. PLoS Med. 2019, 16, e1002926. [Google Scholar] [CrossRef] [PubMed]
- Cortés, Y.I.; Zhang, S.; Hussey, J.M. Pregnancy loss is related to body mass index and prediabetes in early adulthood: Findings from Add Health. PLoS ONE 2022, 17, e0277320. [Google Scholar] [CrossRef] [PubMed]
- Creţu, D.; Cernea, S.; Onea, C.R.; Pop, R.M. Reproductive health in women with type 2 diabetes mellitus. Hormones 2020, 19, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Colamatteo, A.; Fusco, C.; Micillo, T.; D’Hooghe, T.; de Candia, P.; Alviggi, C.; Longobardi, S.; Matarese, G. Immunobiology of pregnancy: From basic science to translational medicine. Trends Mol. Med. 2023, 29, 711–725. [Google Scholar] [CrossRef] [PubMed]
- Massimiani, M.; Lacconi, V.; La Civita, F.; Ticconi, C.; Rago, R.; Campagnolo, L. Molecular Signaling Regulating Endometrium-Blastocyst Crosstalk. Int. J. Mol. Sci. 2019, 21, 23. [Google Scholar] [CrossRef]
- Singh, A.; Kukreti, R.; Saso, L.; Kukreti, S. Mechanistic Insight into Oxidative Stress-Triggered Signaling Pathways and Type 2 Diabetes. Molecules 2022, 27, 950. [Google Scholar] [CrossRef]
- Gäreskog, M.; Cederberg, J.; Eriksson, U.J.; Wentzel, P. Maternal diabetes in vivo and high glucose concentration in vitro increases apoptosis in rat embryos. Reprod. Toxicol. 2007, 23, 63–74. [Google Scholar] [CrossRef]
- Wang, M.; Zhang, J.; Yuan, L.; Hu, H.; Li, T.; Feng, Y.; Zhao, Y.; Wu, Y.; Fu, X.; Ke, Y.; et al. Miscarriage and stillbirth in relation to risk of cardiovascular diseases: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 297, 1–7. [Google Scholar] [CrossRef]
- Huang, S.; Hee, J.Y.; Zhang, Y.O.; Gongye, R.; Zou, S.; Tang, K. Association between pregnancy and pregnancy loss with COPD in Chinese women: The China Kadoorie Biobank study. Front. Public Health 2022, 10, 990057. [Google Scholar] [CrossRef]
- Hee, J.Y.; Huang, S.; Leong, K.P.; Chun, L.; Zhang, Y.O.; Gongye, R.; Tang, K. Pregnancy loss and the risk of rheumatoid arthritis in Chinese women: Findings from the China Kadoorie biobank. BMC Public Health 2022, 22, 1768. [Google Scholar] [CrossRef]
- Taiwanese National Health Insurance Dataset. Available online: https://nhird.nhri.edu.tw (accessed on 1 February 2024).
- Das, M.; Patidar, H.; Singh, M. Understanding trimester-specific miscarriage risk in Indian women: Insights from the calendar data of National Family Health Survey (NFHS-5) 2019-21. BMC Womens Health 2024, 24, 63. [Google Scholar] [CrossRef] [PubMed]
- Cundy, T.; Gamble, G.; Neale, L.; Elder, R.; McPherson, P.; Henley, P.; Rowan, J. Differing causes of pregnancy loss in type 1 and type 2 diabetes. Diabetes Care 2007, 30, 2603–2607. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, Y.; Chen, H.; Dou, Y.; Wang, Y.; He, W.; Ma, X.; Sheng, W.; Yan, W.; Huang, G. Association Between Serum Glycated Hemoglobin Levels at Early Gestation and the Risk of Subsequent Pregnancy Loss in Pregnant Women Without Diabetes Mellitus: Prospective Cohort Study. JMIR Public Health Surveill. 2023, 9, e46986. [Google Scholar] [CrossRef] [PubMed]
- Munné, S.; Alikani, M.; Tomkin, G.; Grifo, J.; Cohen, J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil. Steril. 1995, 64, 382–391, Corrected and republished in: Fertil. Steril. 2019, 112 (Suppl. S1), e71–e80. [Google Scholar] [CrossRef]
- Ayana, G.M.; Raru, T.B.; Deressa, A.; Regassa, L.D.; Gamachu, M.; Negash, B.; Birhanu, A.; Merga, B.T. Association of alcohol consumption with abortion among ever-married reproductive age women in Ethiopia: A multilevel analysis. Front. Glob. Women’s Health 2022, 3, 1028166. [Google Scholar] [CrossRef]
- Khadra, M.M.; Suradi, H.H.; Amarin, J.Z.; El-Bassel, N.; Kaushal, N.; Jaber, R.M.; Al-Qutob, R.; Dasgupta, A. Risk factors for miscarriage in Syrian refugee women living in non-camp settings in Jordan: Results from the Women ASPIRE cross-sectional study. Confl. Health 2022, 16, 32. [Google Scholar] [CrossRef]
- Moradinazar, M.; Najafi, F.; Nazar, Z.M.; Hamzeh, B.; Pasdar, Y.; Shakiba, E. Lifetime Prevalence of Abortion and Risk Factors in Women: Evidence from a Cohort Study. J. Pregnancy 2020, 2020, 4871494. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, W.; Xu, H.; Hu, M.; Guo, X.; Jia, W.; Liu, G.; Li, J.; Cui, P.; Lager, S.; et al. Hyperandrogenism and insulin resistance-induced fetal loss: Evidence for placental mitochondrial abnormalities and elevated reactive oxygen species production in pregnant rats that mimic the clinical features of polycystic ovary syndrome. J. Physiol. 2019, 597, 3927–3950. [Google Scholar] [CrossRef]
- Vidali, A.; Riccio, L.G.C.; Abrao, M.S. Endometriosis and recurrent pregnancy loss: Two manifestations of the same underlying dysfunction? Fertil. Steril. 2023, 119, 836–837. [Google Scholar] [CrossRef] [PubMed]
- Salmeri, N.; Li Piani, L.; Cavoretto, P.I.; Somigliana, E.; Viganò, P.; Candiani, M. Endometriosis increases the risk of gestational diabetes: A meta-analysis stratified by mode of conception, disease localization and severity. Sci. Rep. 2023, 13, 8099. [Google Scholar] [CrossRef] [PubMed]
- Nakhai-Pour, H.R.; Broy, P.; Sheehy, O.; Bérard, A. Use of nonaspirin nonsteroidal anti-inflammatory drugs during pregnancy and the risk of spontaneous abortion. CMAJ 2011, 183, 1713–1720. [Google Scholar] [CrossRef] [PubMed]
- Boje, A.D.; Egerup, P.; Westergaard, D.; Bertelsen, M.M.F.; Nyegaard, M.; Hartwell, D.; Lidegaard, Ø.; Nielsen, H.S. Endometriosis is associated with pregnancy loss: A nationwide historical cohort study. Fertil. Steril. 2023, 119, 826–835. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.M.; Chien, W.C.; Cheng, C.G.; Chang, Y.H.; Chung, C.H.; Cheng, C.A. Females with Diabetes Mellitus Increased the Incidence of Premenstrual Syndrome. Life 2022, 12, 777. [Google Scholar] [CrossRef] [PubMed]
- Beddig, T.; Reinhard, I.; Kuehner, C. Stress, mood, and cortisol during daily life in women with Premenstrual Dysphoric Disorder (PMDD). Psychoneuroendocrinology 2019, 109, 104372. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.H.; Wong, T.H.; Suen, J.L.; Lin, P.C.; Long, C.Y.; Yen, J.Y. Estrogen, progesterone, cortisol, brain-derived neurotrophic factor, and vascular endothelial growth factor during the luteal phase of the menstrual cycle in women with premenstrual dysphoric disorder. J. Psychiatr. Res. 2024, 169, 307–317. [Google Scholar] [CrossRef]
- Seo, J.; Lee, J.; Kim, S.; Lee, M.; Yang, H. Lipid Polysaccharides have a Detrimental Effect on the Function of the Ovaries and Uterus in Mice through Increased Pro-Inflammatory Cytokines. Dev. Reprod. 2022, 26, 135–144. [Google Scholar] [CrossRef]
- MacKenzie, S.; Montserrat, N.; Mas, M.; Acerete, L.; Tort, L.; Krasnov, A.; Goetz, F.W.; Planas, J.V. Bacterial lipopolysaccharide induces apoptosis in the trout ovary. Reprod. Biol. Endocrinol. 2006, 4, 46. [Google Scholar] [CrossRef]
- Grewal, K.; Lee, Y.S.; Smith, A.; Brosens, J.J.; Bourne, T.; Al-Memar, M.; Kundu, S.; MacIntyre, D.A.; Bennett, P.R. Chromosomally normal miscarriage is associated with vaginal dysbiosis and local inflammation. BMC Med. 2022, 20, 38. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Wambua, S.; Lee, S.I.; Okoth, K.; Wang, Z.; Fayaz, F.F.A.; Eastwood, K.A.; Nelson-Piercy, C.; Reynolds, J.A.; Nirantharakumar, K.; et al. Autoimmune diseases and adverse pregnancy outcomes: An umbrella review. BMC Med. 2024, 22, 94. [Google Scholar] [CrossRef] [PubMed]
- Li, P.F.; Li, S.; Zheng, P.S. Reproductive Effect by Rheumatoid Arthritis and Related Autoantibodies. Rheumatol. Ther. 2024, 11, 239–256. [Google Scholar] [CrossRef] [PubMed]
- Nathan, N.O.; Mørch, L.S.; Wu, C.S.; Olsen, J.; Hetland, M.L.; Li, J.; Rom, A.L. Rheumatoid arthritis and risk of spontaneous abortion: A Danish nationwide cohort study. Rheumatology 2020, 59, 1984–1991. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Li, Q.; Wang, Q.; Ma, X. Thyroid antibodies and gestational diabetes mellitus: A meta-analysis. Fertil. Steril. 2015, 104, 665–671.e3. [Google Scholar] [CrossRef] [PubMed]
- Napolitano, G.; Fasciolo, G.; Di Meo, S.; Venditti, P. Vitamin E Supplementation and Mitochondria in Experimental and Functional Hyperthyroidism: A Mini-Review. Nutrients 2019, 11, 2900. [Google Scholar] [CrossRef] [PubMed]
- Andersen, S.L.; Olsen, J.; Wu, C.S.; Laurberg, P. Spontaneous abortion, stillbirth and hyperthyroidism: A danish population-based study. Eur. Thyroid J. 2014, 3, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Corrales-Gutierrez, I.; Mendoza, R.; Gomez-Baya, D.; Leon-Larios, F. Understanding the Relationship between Predictors of Alcohol Consumption in Pregnancy: Towards Effective Prevention of FASD. Int. J. Environ. Res. Public Health 2020, 17, 1388. [Google Scholar] [CrossRef] [PubMed]
- Magnus, M.C.; Havdahl, A.; Morken, N.H.; Wensaas, K.A.; Wilcox, A.J.; Håberg, S.E. Risk of miscarriage in women with psychiatric disorders. Br. J. Psychiatry 2021, 219, 501–506. [Google Scholar] [CrossRef]
- Andersen, J.T.; Andersen, N.L.; Horwitz, H.; Poulsen, H.E.; Jimenez-Solem, E. Exposure to selective serotonin reuptake inhibitors in early pregnancy and the risk of miscarriage. Obstet. Gynecol. 2014, 124, 655–661. [Google Scholar] [CrossRef]
- Polli, A.; Hendrix, J.; Ickmans, K.; Bakusic, J.; Ghosh, M.; Monteyne, D.; Velkeniers, B.; Bekaert, B.; Nijs, J.; Godderis, L. Genetic and epigenetic regulation of Catechol-O-methyltransferase in relation to inflammation in chronic fatigue syndrome and Fi-bromyalgia. J. Transl. Med. 2022, 20, 487. [Google Scholar] [CrossRef] [PubMed]
- Venturini, L.; Bacchi, S.; Capelli, E.; Lorusso, L.; Ricevuti, G.; Cusa, C. Modification of Immunological Parameters, Oxidative Stress Markers, Mood Symptoms, and Well-Being Status in CFS Patients after Probiotic Intake: Observations from a Pilot Study. Oxidative Med. Cell. Longev. 2019, 2019, 1684198. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Kubera, M.; Kotańska, M. Aberrations in the Cross-Talks Among Redox, Nuclear Factor-κB, and Wnt/β-Catenin Pathway Signaling Underpin Myalgic Encephalomyelitis and Chronic Fatigue Syndrome. Front. Psychiatry 2022, 13, 822382. [Google Scholar] [CrossRef] [PubMed]
- Jöud, A.; Nilsson-Condori, E.; Schmidt, L.; Ziebe, S.; Vassard, D.; Mattsson, K. Infertility, pregnancy loss and assisted reproduction in women with asthma: A population-based cohort study. Hum. Reprod. 2022, 37, 2932–2941. [Google Scholar] [CrossRef] [PubMed]
- Khashan, A.S.; Quigley, E.M.; McNamee, R.; McCarthy, F.P.; Shanahan, F.; Kenny, L.C. Increased risk of miscarriage and ectopic pregnancy among women with irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 2012, 10, 902–909. [Google Scholar] [CrossRef]
- Davidson, A.J.F.; Park, A.L.; Berger, H.; Aoyama, K.; Harel, Z.; Cohen, E.; Cook, J.L.; Ray, J.G. Association of Improved Periconception Hemoglobin A1c With Pregnancy Outcomes in Women with Diabetes. JAMA Netw. Open 2020, 3, e2030207. [Google Scholar] [CrossRef] [PubMed]
- Coton, S.J.; Nazareth, I.; Petersen, I. A cohort study of trends in the prevalence of pregestational diabetes in pregnancy recorded in UK general practice between 1995 and 2012. BMJ Open 2016, 6, e009494. [Google Scholar] [CrossRef] [PubMed]
- Lashen, H.; Fear, K.; Sturdee, D.W. Obesity is associated with increased risk of first trimester and recurrent miscarriage: Matched case-control study. Hum. Reprod. 2004, 19, 1644–1646. [Google Scholar] [CrossRef]
- Nutrition Health Survey in Taiwan, 2017–2020. Available online: https://www.hpa.gov.tw/File/Attach/15562/File_18775.pdf. (accessed on 1 February 2024).
- Teodoro, J.S.; Nunes, S.; Rolo, A.P.; Reis, F.; Palmeira, C.M. Therapeutic Options Targeting Oxidative Stress, Mitochondrial Dys-function and Inflammation to Hinder the Progression of Vascular Complications of Diabetes. Front. Physiol. 2019, 9, 1857. [Google Scholar] [CrossRef]
- Yang, H.L.; Zhou, W.J.; Gu, C.J.; Meng, Y.H.; Shao, J.; Li, D.J.; Li, M.Q. Pleiotropic roles of melatonin in endometriosis, recurrent spon-taneous abortion, and polycystic ovary syndrome. Am. J. Reprod. Immunol. 2018, 80, e12839. [Google Scholar] [CrossRef]
- Picard, M.; Tauveron, I.; Magdasy, S.; Benichou, T.; Bagheri, R.; Ugbolue, U.C.; Navel, V.; Dutheil, F. Effect of exercise training on heart rate variability in type 2 diabetes mellitus patients: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251863. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Song, Y.; Gaskins, A.J.; Li, L.J.; Huang, Z.; Eriksson, J.G.; Hu, F.B.; Chong, Y.S.; Zhang, C. Mediterranean diet and female repro-ductive health over lifespan: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2023, 229, 617–631. [Google Scholar] [CrossRef] [PubMed]
- Devall, A.J.; Papadopoulou, A.; Podesek, M.; Haas, D.M.; Price, M.J.; Coomarasamy, A.; Gallos, I.D. Progestogens for preventing mis-carriage: A network meta-analysis. Cochrane Database Syst. Rev. 2021, 4, CD013792. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.C.; Hill, J.W.; Anderson, G.M. Role of insulin in the neuroendocrine control of reproduction. J. Neuroendocrinol. 2021, 33, e12930. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Zhang, W. Application of Gestational Blood Glucose Control During Perinatal Period in Parturients with Diabetes Mellitus: Meta-Analysis of Controlled Clinical Studies. Front. Surg. 2022, 9, 893148. [Google Scholar] [CrossRef]
- Mehdi, S.F.; Pusapati, S.; Anwar, M.S.; Lohana, D.; Kumar, P.; Nandula, S.A.; Nawaz, F.K.; Tracey, K.; Yang, H.; LeRoith, D.; et al. Glucagon-like peptide-1: A multi-faceted anti-inflammatory agent. Front. Immunol. 2023, 14, 1148209. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Liu, J.; Larsson, S.C. Smoking, alcohol and coffee consumption and pregnancy loss: A Mendelian randomization inves-tigation. Fertil. Steril. 2021, 116, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Murphy, H.R.; Howgate, C.; O’Keefe, J.; Myers, J.; Morgan, M.; Coleman, M.A.; Jolly, M.; Valabhji, J.; Scott, E.M.; Knighton, P.; et al. Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: A 5-year national population-based cohort study. Lancet Diabetes Endocrinol. 2021, 9, 153–164. [Google Scholar] [CrossRef]
| Variables | Total | Diabetes Mellitus | Without Diabetes Mellitus | p |
|---|---|---|---|---|
| Number | 95,020 | 19,004 | 76,016 | 1 |
| Low-income | 1294 (1.4%) | 383 (2%) | 911 (1.2%) | <0.001 * |
| Polycystic ovary syndrome | 2968 (3.1%) | 1081 (5.7%) | 1887 (2.5%) | <0.001 * |
| Pelvis inflammation disorder | 63,262 (66.6%) | 12,238 (64.4%) | 51,024 (67.1%) | <0.001 * |
| Urinary tract infection | 31,863 (33.5%) | 6460 (34%) | 25,403 (33.4%) | 0.144 |
| Premenstrual syndrome | 2786 (2.9%) | 410 (2.2%) | 2376 (3.1%) | <0.001 * |
| Endometriosis | 10,925 (11.5%) | 2007 (10.6%) | 8918 (11.7%) | <0.001 * |
| Autoimmune disease | 9531 (10%) | 1163 (6.1%) | 8368 (11%) | <0.001 * |
| Obesity | 3321 (3.5%) | 1727 (9.1%) | 1594 (2.1%) | <0.001 * |
| Hypertension | 17,705 (18.6%) | 7565 (39.8%) | 10,140 (13.3%) | <0.001 * |
| Hyperlipidemia | 21,161 (22.3%) | 9319 (49%) | 11,842 (15.6%) | <0.001 * |
| Chronic kidney disease | 7815 (8.2%) | 1407 (7.4%) | 6408 (8.4%) | <0.001 * |
| Hyperthyroidism | 7583 (8%) | 1797 (9.5%) | 5786 (7.6%) | <0.001 * |
| Fibromyalgia | 39,543 (41.6%) | 7505 (39.5%) | 32,038 (42.1%) | <0.001 * |
| Chronic fatigue syndrome | 1345 (1.4%) | 277 (1.5%) | 1068 (1.4%) | 0.5907 |
| Chronic obstructive pulmonary disease | 15,567 (16.4%) | 2085 (11%) | 13,482 (17.7%) | <0.001 * |
| Asthma | 17,032 (17.9%) | 2406 (12.7%) | 14,626 (19.2%) | <0.001 * |
| Alcoholic disorder | 1658 (1.7%) | 431 (2.3%) | 1227 (1.6%) | <0.001 * |
| Depression | 10,722 (11.3%) | 2006 (10.6%) | 8716 (11.5%) | 0. 003 * |
| Anxiety | 10,141 (10.7%) | 1804 (9.5%) | 8337 (11%) | <0.001 * |
| Irritable bowel disorder | 13,057 (13.7%) | 2063 (10.9%) | 10,994 (14.5%) | <0.001 * |
| Bladder disorder | 2517 (2.6%) | 455 (2.4%) | 2062 (2.7%) | 0.01 * |
| Polyneuropathies | 471 (0.5%) | 430 (2.3%) | 41 (0.1%) | <0.001 * |
| Urbanization levels | 0.773 | |||
| 1 (The highest) | 29,386 (30.9%) | 5564 (29.3%) | 23,822 (31.3%) | |
| 2 | 31,769 (33.4%) | 6235 (32.8%) | 25,534 (33.6%) | |
| 3 | 26,916 (28.3%) | 5600 (29.5%) | 21,316 (28%) | |
| 4 (The lowest) | 6593 (6.9%) | 1546 (8.1%) | 5047 (6.6%) | |
| Missing | 356 (0.4%) | 59 (0.3%) | 297 (0.4%) | |
| Hospital levels | <0.001 * | |||
| Medical center | 15,775 (16.6%) | 3479 (18.3%) | 12,296 (16.2%) | |
| Regional hospital | 18,644 (19.6%) | 4851 (25.5%) | 13,793 (18.1%) | |
| Local hospital | 14,649 (15.4%) | 3901 (20.5%) | 10,748 (14.1%) | |
| Clinic | 45,952 (48.4%) | 6773 (35.6%) | 39,179 (51.5%) |
| Crude Hazard Ratio | p | Adjusted Hazard Ratio | p | |
|---|---|---|---|---|
| Diabetes mellitus | 1.682 (95% C.I.: 1.423–1.971) | <0.001 * | 1.407 (95% C.I.: 1.099–1.801) | 0.007 * |
| Age | 1.034 (95% C.I.: 1.025–1.073) | <0.01 * | 1.020 (95% C.I.: 1.004–1.063) | 0.002 * |
| Post CCI | 1.311 (95% C.I.: 1.164–1.571) | <0.001 * | 1.221 (95% C.I.: 1.133–1.468) | <0.001 * |
| Low-income | 1.567 (95% C.I.: 0.795–1.798) | 0.246 | 1.268 (95% C.I.: 0.575–1.483) | 0.387 |
| Polycystic ovary syndrome | 6.765 (95% C.I.: 4.282–8.835) | <0.01 * | 1.792 (95% C.I.:1.403–2.121) | <0.001 * |
| Pelvis inflammation disorder | 2.245 (95% C.I.: 2.013–2.498) | <0.001 * | 2.145 (95% C.I.: 1.911–2.220) | <0.001 * |
| Urinary tract infection | 1.894 (95% C.I.: 1.625–1.972) | <0.001 * | 1.803 (95% C.I.: 1.529–1.880) | <0.001 * |
| Premenstrual syndrome | 2.701 (95% C.I.: 1.941–3.177) | <0.001 * | 2.067 (95% C.I.: 1.486–2.763) | <0.001 * |
| Endometriosis | 1.443 (95% C.I.: 1.202–1.694) | <0.001 * | 1.420 (95% C.I.: 1.197–1.683) | <0.001 * |
| Autoimmune disease | 1.382 (95% C.I.: 1.125–1.553) | <0.001 * | 1.290 (95% C.I.: 1.111–1.543) | <0.001 * |
| Obesity | 1.843 (95% C.I.: 1.354–2.241) | <0.001 * | 1.068 (95% C.I.: 0.867–1.798) | 0.465 |
| Hypertension | 1.006 (95% C.I.: 0.435–1.972) | 0.904 | 0.986 (95% C.I.: 0.421–1.933) | 0.804 |
| Hyperlipidemia | 1.343 (95% C.I.:0.791–1.597) | 0.803 | 1.146 (95% C.I.:0.682–1.371) | 0.201 |
| Chronic kidney disease | 1.262 (95% C.I.: 0.679–1.486) | 0.797 | 1.135 (95% C.I.: 0.597–1.337) | 0.663 |
| Hyperthyroidism | 1.680 (95% C.I.: 1.423–1.986) | <0.001 * | 1.234 (95% C.I.: 1.056–1.503) | 0.001 * |
| Fibromyalgia | 1.403 (95% C.I.: 1.276–1.688) | <0.001 * | 1.353 (95% C.I.: 1.204–1.579) | <0.001 * |
| Chronic fatigue syndrome | 2.561 (95% C.I.: 1.897–3.808) | <0.001 * | 1.835 (95% C.I.: 1.106–2.978) | <0.001 * |
| Chronic obstructive pulmonary disease | 1.264 (95% C.I.: 0.925–1.440) | 0.703 | 1.116 (95% C.I.: 0.875–1.438) | 0.069 |
| Asthma | 1.467 (95% C.I.: 1.303–1.765) | <0.001 * | 1.382 (95% C.I.: 1.204–1.595) | <0.001 * |
| Alcoholic disorder | 2.016 (95% C.I.: 1.513–2.897) | <0.001 * | 1.562 (95% C.I.: 1.303–2.701) | <0.001 * |
| Depression | 1.680 (95% C.I.: 1.27–1.864) | <0.001 * | 1.528 (95% C.I.: 1.131–1.735) | <0.001 * |
| Anxiety | 1.065 (95% C.I.: 0.755–1.279) | 0.301 | 0.972 (95% C.I.: 0.734–1.186) | 0.702 |
| Irritable bowel disorder | 1.513 (95% C.I.: 1.331–1.792) | <0.001 * | 1.340 (95% C.I.: 1.104–1.532) | <0.001 * |
| Bladder disorder | 1.030 (95% C.I.: 0.681–1.156) | 0.333 | 0.972 (95% C.I.: 0.513–1.097) | 0.498 |
| Polyneuropathies | 0.998 (95% C.I.: 0.425–1.201) | 0.505 | 0.706 (95% C.I.: 0.342–1.084) | 0.488 |
| Urbanization level | ||||
| 1 (The highest) | Reference | Reference | ||
| 2 | 1.098 (95% CI:0.511–1.584) | 0.465 | 1.003 (95% C.I.: 0.408–1.438) | 0.565 |
| 3 | 1.145 (95% C.I.: 0.562–1.601) | 0.43 | 1.072 (95% C.I.: 0.492–1.483) | 0.551 |
| 4 (The lowest) | 1.246 (95% C.I.: 0.678–1.65) | 0.301 | 1.125 (95% C.I.: 0.533–1.572) | 0.48 |
| Hospital levels | ||||
| Medical Center | 0.655 (95% C.I.: 0.512–0.834) | <0.001 * | 0.687 (95% C.I.: 0.586–0.917) | 0.001 * |
| Regional hospital | 0.724 (95% C.I.: 0.409–0.978) | 0.014 * | 0.782 (95% C.I.: 0.432–1.034) | 0.132 |
| Local hospital | 0.832 (95% C.I.: 0.335–1.106) | 0.505 | 0.89 (95%C.I.: 0.356–1.297) | 0.202 |
| Clinic | Reference | Reference | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, C.-G.; Su, S.-H.; Chien, W.-C.; Chen, R.; Chung, C.-H.; Cheng, C.-A. Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study. Life 2024, 14, 903. https://doi.org/10.3390/life14070903
Cheng C-G, Su S-H, Chien W-C, Chen R, Chung C-H, Cheng C-A. Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study. Life. 2024; 14(7):903. https://doi.org/10.3390/life14070903
Chicago/Turabian StyleCheng, Chun-Gu, Sheng-Hua Su, Wu-Chien Chien, Ryan Chen, Chi-Hsiang Chung, and Chun-An Cheng. 2024. "Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study" Life 14, no. 7: 903. https://doi.org/10.3390/life14070903
APA StyleCheng, C.-G., Su, S.-H., Chien, W.-C., Chen, R., Chung, C.-H., & Cheng, C.-A. (2024). Diabetes Mellitus and Gynecological and Inflammation Disorders Increased the Risk of Pregnancy Loss in a Population Study. Life, 14(7), 903. https://doi.org/10.3390/life14070903







