Internal Rotation Measurement of the Knee with Polymer-Based Capacitive Strain Gauges versus Mechanical Rotation Measurement Taking Gender Differences into Account: A Comparative Analysis
Abstract
1. Introduction
2. Materials and Methods
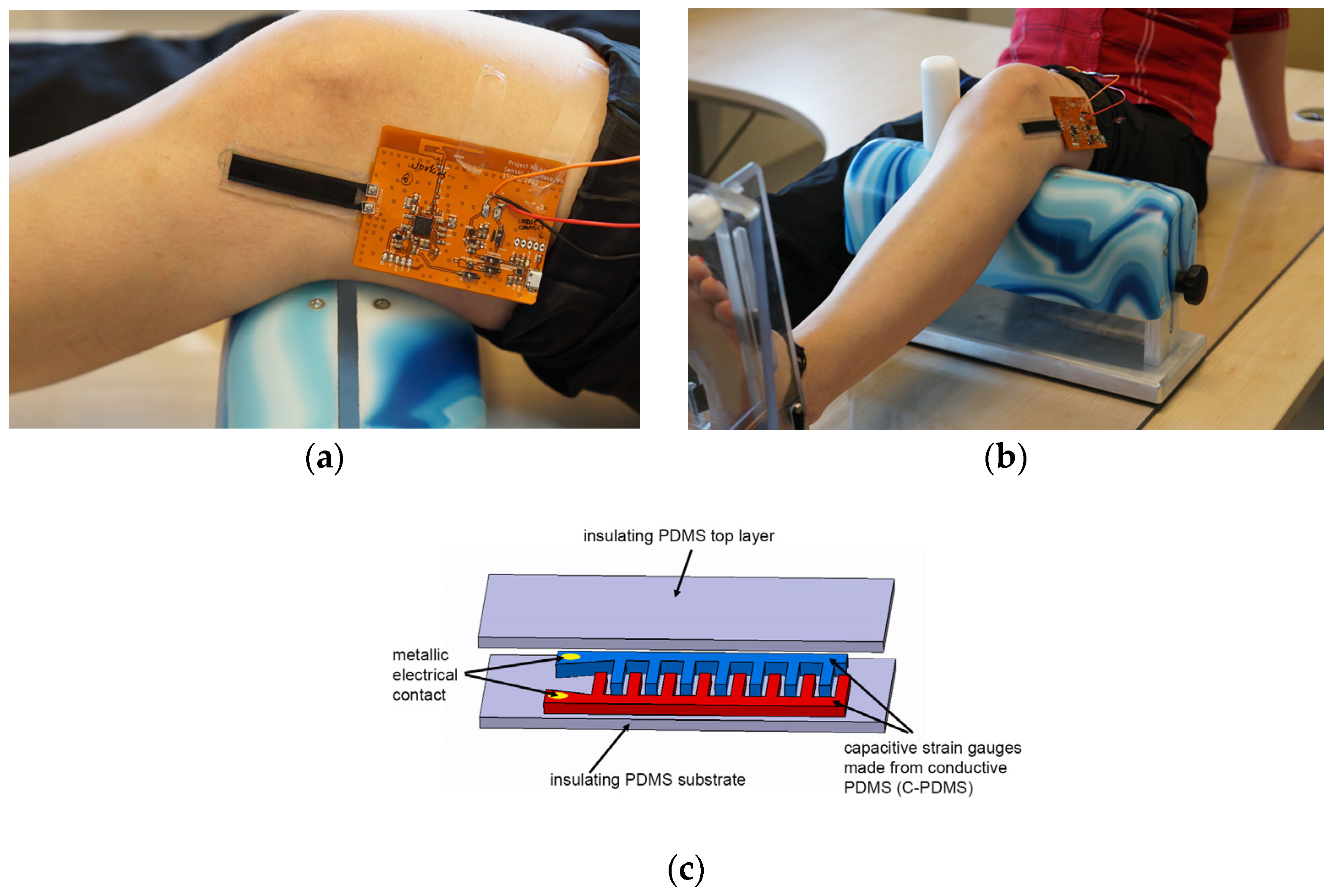
2.1. Materials
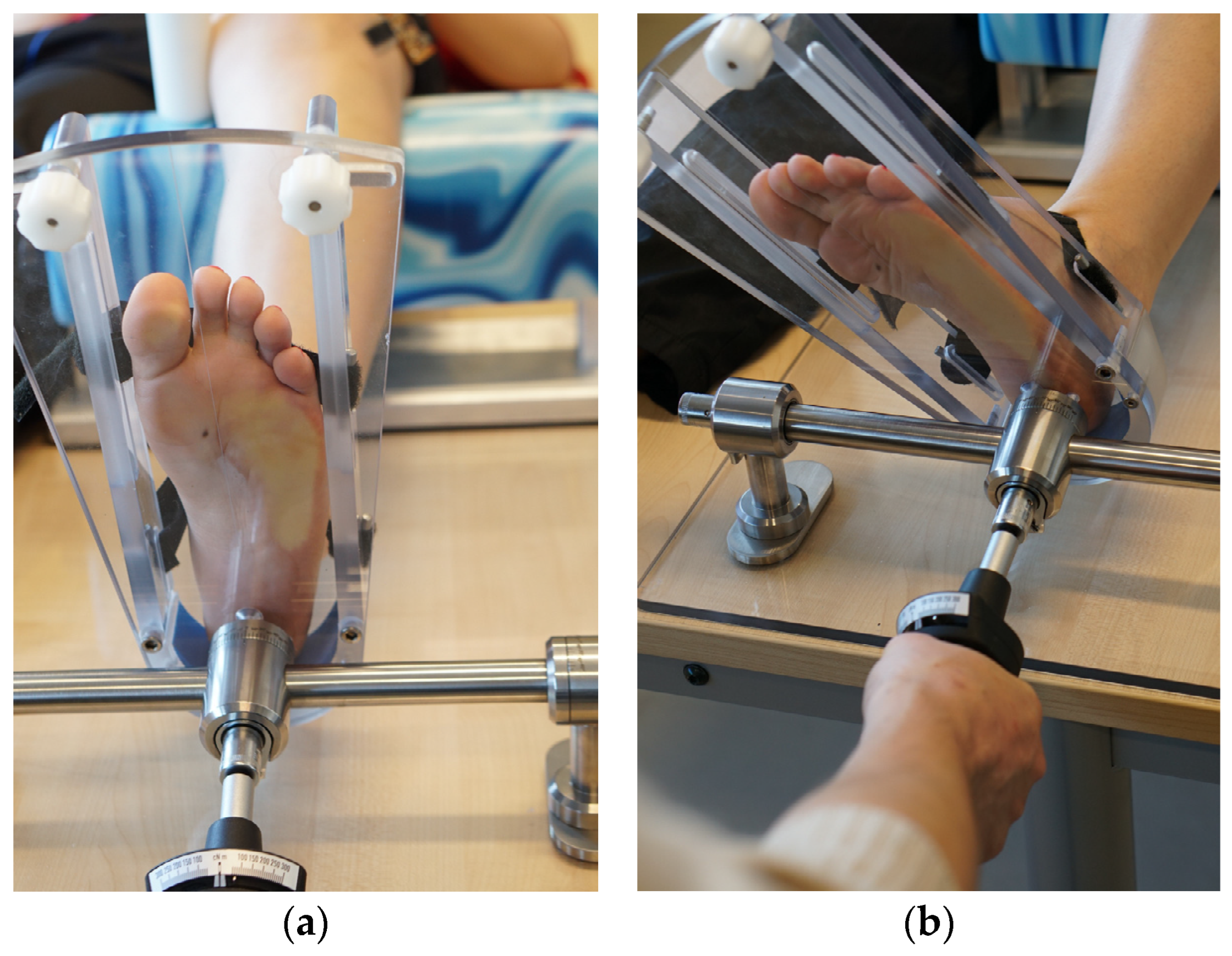
2.2. Methods
2.3. Statistics
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boden, B.P.; Sheehan, F.T. Mechanism of non-contact acl injury: Oref clinical research award 2021. J. Orthop. Res. 2022, 40, 531–540. [Google Scholar] [CrossRef]
- Branch, T.P.; Browne, J.E.; Campbell, J.D.; Siebold, R.; Freedberg, H.I.; Arendt, E.A.; Lavoie, F.; Neyret, P.; Jacobs, C.A. Rotational laxity greater in patients with contralateral anterior cruciate ligament injury than healthy volunteers. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1379–1384. [Google Scholar] [CrossRef] [PubMed]
- Lian, J.; Diermeier, T.; Meghpara, M.; Popchak, A.; Smith, C.N.; Kuroda, R.; Zaffagnini, S.; Samuelsson, K.; Karlsson, J.; Irrgang, J.J.; et al. Rotatory knee laxity exists on a continuum in anterior cruciate ligament injury. JBJS 2020, 102, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Ruhhammer, J.; Zens, M.; Goldschmidtboeing, F.; Seifert, A.; Woias, P. Highly elastic conductive polymeric mems. Sci. Technol. Adv. Mater. 2015, 16, 015003. [Google Scholar] [CrossRef] [PubMed]
- Wiertsema, S.H.; van Hooff, H.J.; Migchelsen, L.A.; Steultjens, M.P. Reliability of the kt1000 arthrometer and the lachman test in patients with an acl rupture. Knee 2008, 15, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Prins, M. The lachman test is the most sensitive and the pivot shift the most specific test for the diagnosis of acl rupture. Aust. J. Physiother. 2006, 52, 66. [Google Scholar] [CrossRef]
- Makhmalbaf, H.; Moradi, A.; Ganji, S.; Omidi-Kashani, F. Accuracy of lachman and anterior drawer tests for anterior cruciate ligament injuries. Arch. Bone Jt. Surg. 2013, 1, 94–97. [Google Scholar]
- Imhoff, A.; Linke, R.; Baumgartner, R. Checkliste Orthopädie; Thieme: Stuttgart, Germany, 2021; Volume 4. [Google Scholar]
- Lange, T.; Freiberg, A.; Dröge, P.; Lützner, J.; Schmitt, J.; Kopkow, C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture—A systematic review. Man. Ther. 2015, 20, 402–411. [Google Scholar] [CrossRef]
- Kuroda, R.; Hoshino, Y.; Kubo, S.; Araki, D.; Oka, S.; Nagamune, K.; Kurosaka, M. Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency:A global survey and kinematics assessment. Am. J. Sports Med. 2012, 40, 91–99. [Google Scholar] [CrossRef]
- Naendrup, J.H.; Zlotnicki, J.P.; Murphy, C.I.; Patel, N.K.; Debski, R.E.; Musahl, V. Influence of knee position and examiner-induced motion on the kinematics of the pivot shift. J. Exp. Orthop. 2019, 6, 11. [Google Scholar] [CrossRef]
- Slichter, M.E.; Wolterbeek, N.; Auw Yang, K.G.; Zijl, J.A.C.; Piscaer, T.M. A novel test for assessment of anterolateral rotatory instability of the knee: The tibial internal rotation test (tir test). J. Exp. Orthop. 2018, 5, 29. [Google Scholar] [CrossRef]
- Slichter, M.E.; Wolterbeek, N.; Auw Yang, K.G.; Zijl, J.A.C.; Piscaer, T.M. Rater agreement reliability of the dial test in the acl-deficient knee. J. Exp. Orthop. 2018, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Daniel, D.M.; Stone, M.L.; Sachs, R.; Malcom, L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am. J. Sports Med. 1985, 13, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Schuster, A.J.; McNicholas, M.J.; Wachtl, S.W.; McGurty, D.W.; Jakob, R.P. A new mechanical testing device for measuring anteroposterior knee laxity. Am. J. Sports Med. 2004, 32, 1731–1735. [Google Scholar] [CrossRef] [PubMed]
- Jardin, C.; Chantelot, C.; Migaud, H.; Gougeon, F.; Debroucker, M.J.; Duquennoy, A. Reliability of the kt-1000 arthrometer in measuring anterior laxity of the knee: Comparative analysis with telos of 48 reconstructions of the anterior cruciate ligament and intra- and interobserver reproducibility. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1999, 85, 698–707. [Google Scholar]
- Hoshino, Y.; Kuroda, R.; Nagamune, K.; Yagi, M.; Mizuno, K.; Yamaguchi, M.; Muratsu, H.; Yoshiya, S.; Kurosaka, M. In vivo measurement of the pivot-shift test in the anterior cruciate ligament—Deficient knee using an electromagnetic device. Am. J. Sports Med. 2007, 35, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Lopomo, N.; Bignozzi, S.; Martelli, S.; Zaffagnini, S.; Iacono, F.; Visani, A.; Marcacci, M. Reliability of a navigation system for intra-operative evaluation of antero-posterior knee joint laxity. Comput. Biol. Med. 2009, 39, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Kümmerlin, J.; Fabro, H.K.; Pedersen, P.H.; Jensen, K.K.; Pedersen, D.; Andersen, M.S. Measuring knee joint laxity in three degrees-of-freedom in vivo using a robotics- and image-based technology. J. Biomech. Eng. 2022, 144, 084502. [Google Scholar] [CrossRef]
- Almquist, P.O.; Arnbjörnsson, A.; Zätterström, R.; Ryd, L.; Ekdahl, C.; Fridén, T. Evaluation of an external device measuring knee joint rotation: An in vivo study with simultaneous roentgen stereometric analysis. J. Orthop. Res. 2002, 20, 427–432. [Google Scholar] [CrossRef]
- Tsai, A.G.; Musahl, V.; Steckel, H.; Bell, K.M.; Zantop, T.; Irrgang, J.J.; Fu, F.H. Rotational knee laxity: Reliability of a simple measurement device in vivo. BMC Musculoskelet. Disord. 2008, 9, 35. [Google Scholar] [CrossRef]
- Quinn, T.P.; Mote, C.D.; Skinner, H.B. The effect of ankle constraint on the torsional laxity of the knee during internal-external rotation of the foot. J. Biomech. 1991, 24, 511–525. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, E.T.; Stentz-Olesen, K.; de Raedt, S.; Jorgensen, P.B.; Sorensen, O.G.; Kaptein, B.; Andersen, M.S.; Stilling, M. Influence of the anterolateral ligament on knee laxity: A biomechanical cadaveric study measuring knee kinematics in 6 degrees of freedom using dynamic radiostereometric analysis. Orthop. J. Sports Med. 2018, 6, 2325967118789699. [Google Scholar] [CrossRef] [PubMed]
- Moewis, P.; Duda, G.N.; Jung, T.; Heller, M.O.; Boeth, H.; Kaptein, B.; Taylor, W.R. The restoration of passive rotational tibio-femoral laxity after anterior cruciate ligament reconstruction. PLoS ONE 2016, 11, e0159600. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Mansilla, I.; Zicaro, J.P.; Martinez, E.F.; Astoul, J.; Yacuzzi, C.; Costa-Paz, M. Overview of the anterolateral complex of the knee. World J. Clin. Cases 2022, 10, 8474–8481. [Google Scholar] [CrossRef] [PubMed]
- Espregueira-Mendes, J.; Andrade, R.; Leal, A.; Pereira, H.; Skaf, A.; Rodrigues-Gomes, S.; Oliveira, J.M.; Reis, R.L.; Pereira, R. Global rotation has high sensitivity in acl lesions within stress mri. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2993–3003. [Google Scholar] [CrossRef]
- Mayr, H.O.; Hoell, A.; Bernstein, A.; Hube, R.; Zeiler, C.; Kalteis, T.; Suedkamp, N.P.; Stoehr, A. Validation of a measurement device for instrumented quantification of anterior translation and rotational assessment of the knee. Arthrosc. J. Arthrosc. Relat. Surg. 2011, 27, 1096–1104. [Google Scholar] [CrossRef] [PubMed]
- Branch, T.P.; Mayr, H.O.; Browne, J.E.; Campbell, J.C.; Stoehr, A.; Jacobs, C.A. Instrumented examination of anterior cruciate ligament injuries: Minimizing flaws of the manual clinical examination. Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, 997–1004. [Google Scholar] [CrossRef] [PubMed]
- Sheeja Prakash, K.; Mayr, H.O.; Agrawal, P.; Agarwal, P.; Seidenstuecker, M.; Rosenstiel, N.; Woias, P.; Comella, L.M. Batch fabrication of a polydimethlysiloxane based stretchable capacitive strain gauge sensor for orthopedics. Polymers 2022, 14, 2326. [Google Scholar] [CrossRef]
- Sheeja Prakash, K.; Andersen, E.; von Einem, V.C.; Muthalagu, S.K.; Agarwal, P.; Mayr, H.O.; Seidenstuecker, M.; Rosenstiel, N.; Roundy, S.; Woias, P.; et al. Design and implementation of a wearable system based on a flexible capacitive sensor, monitoring knee laxity. Adv. Sens. Res. 2023, 2, 2300058. [Google Scholar] [CrossRef]
- Feng, J.; Cao, Y.; Tan, L.; Liang, J.; He, C.; He, J.; Wu, S. Anterior cruciate ligament reconstruction with lateral extra-articular tenodesis reduces knee rotation laxity and graft failure rate: A systematic review and meta-analysis. J. Orthop. Surg. 2022, 30, 10225536221095969. [Google Scholar] [CrossRef]
- Ferretti, A. Extra-articular reconstruction in the anterior cruciate ligament deficient knee: A commentary. Joints 2014, 2, 41–473. [Google Scholar] [PubMed]
- Reider, B. Acl or acl+. Am. J. Sports Med. 2020, 48, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Zens, M.; Niemeyer, P.; Ruhhammer, J.; Bernstein, A.; Woias, P.; Mayr, H.O.; Südkamp, N.P.; Feucht, M.J. Length changes of the anterolateral ligament during passive knee motion: A human cadaveric study. Am. J. Sports Med. 2015, 43, 2545–2552. [Google Scholar] [CrossRef]
- Ellison, T.M.; Flagstaff, I.; Johnson, A.E. Sexual dimorphisms in anterior cruciate ligament injury: A current concepts review. Orthop. J. Sports Med. 2021, 9, 23259671211025304. [Google Scholar] [CrossRef] [PubMed]
- Ahldén, M.; Samuelsson, K.; Fu, F.H.; Musahl, V.; Karlsson, J. Rotatory knee laxity. Clin. Sports Med. 2013, 32, 37–46. [Google Scholar] [CrossRef]
- Kernkamp, W.A.; Van de Velde, S.K.; Hosseini, A.; Tsai, T.-Y.; Li, J.-S.; van Arkel, E.R.A.; Li, G. In vivo anterolateral ligament length change in the healthy knee during functional activities—A combined magnetic resonance and dual fluoroscopic imaging analysis. Arthrosc. J. Arthrosc. Relat. Surg. 2017, 33, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Kosy, J.D.; Mandalia, V.I.; Anaspure, R. Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skelet. Radiol. 2015, 44, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Lording, T.; Corbo, G.; Bryant, D.; Burkhart, T.A.; Getgood, A. Rotational laxity control by the anterolateral ligament and the lateral meniscus is dependent on knee flexion angle: A cadaveric biomechanical study. Clin. Orthop. Relat. Res. 2017, 475, 2401–2408. [Google Scholar] [CrossRef]
- Wang, Y.; Li, S.; Xu, D.; Qian, L.; Jiang, C.; Fu, M.; Sun, P.; Ouyang, J. Strain distribution of the anterolateral ligament during internal rotation at different knee flexion angles: A biomechanical study on human cadavers. Knee 2019, 26, 339–346. [Google Scholar] [CrossRef]
- Kuroda, R.; Hoshino, Y. Electromagnetic tracking of the pivot-shift. Curr. Rev. Musculoskelet. Med. 2016, 9, 164–169. [Google Scholar] [CrossRef]
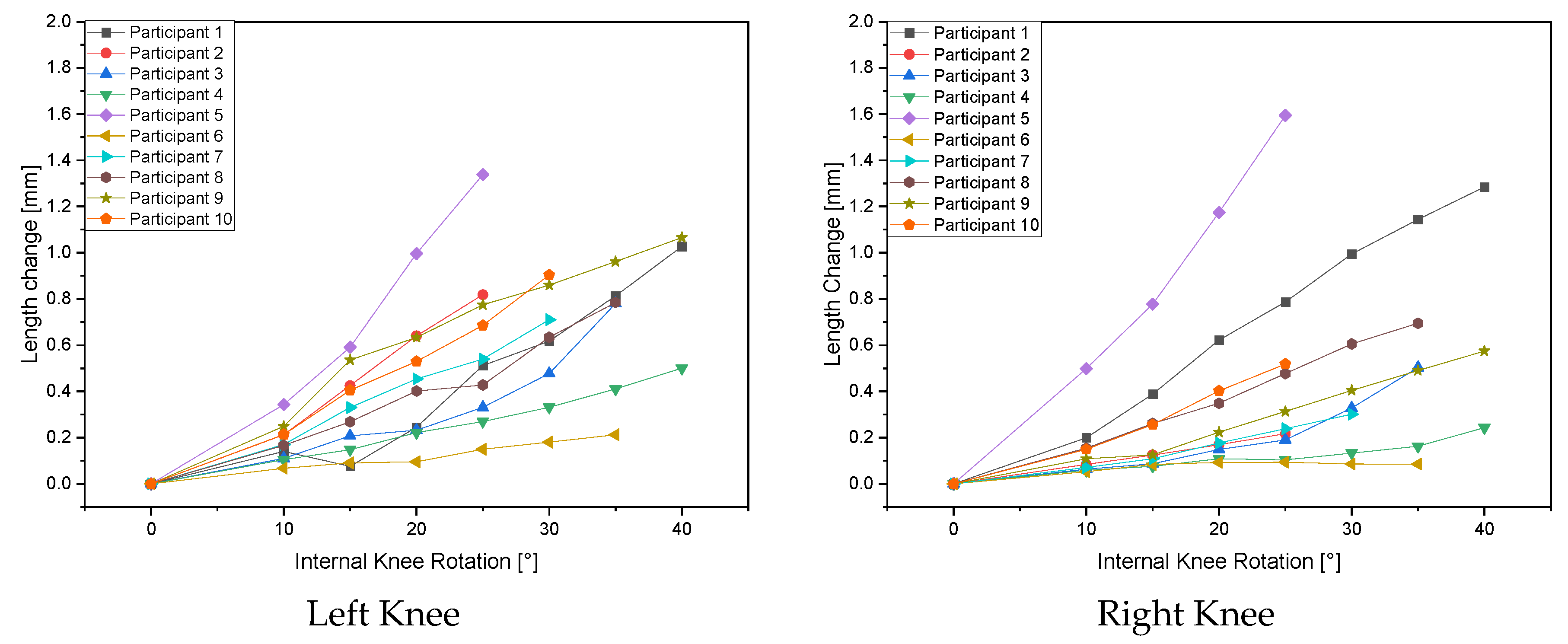
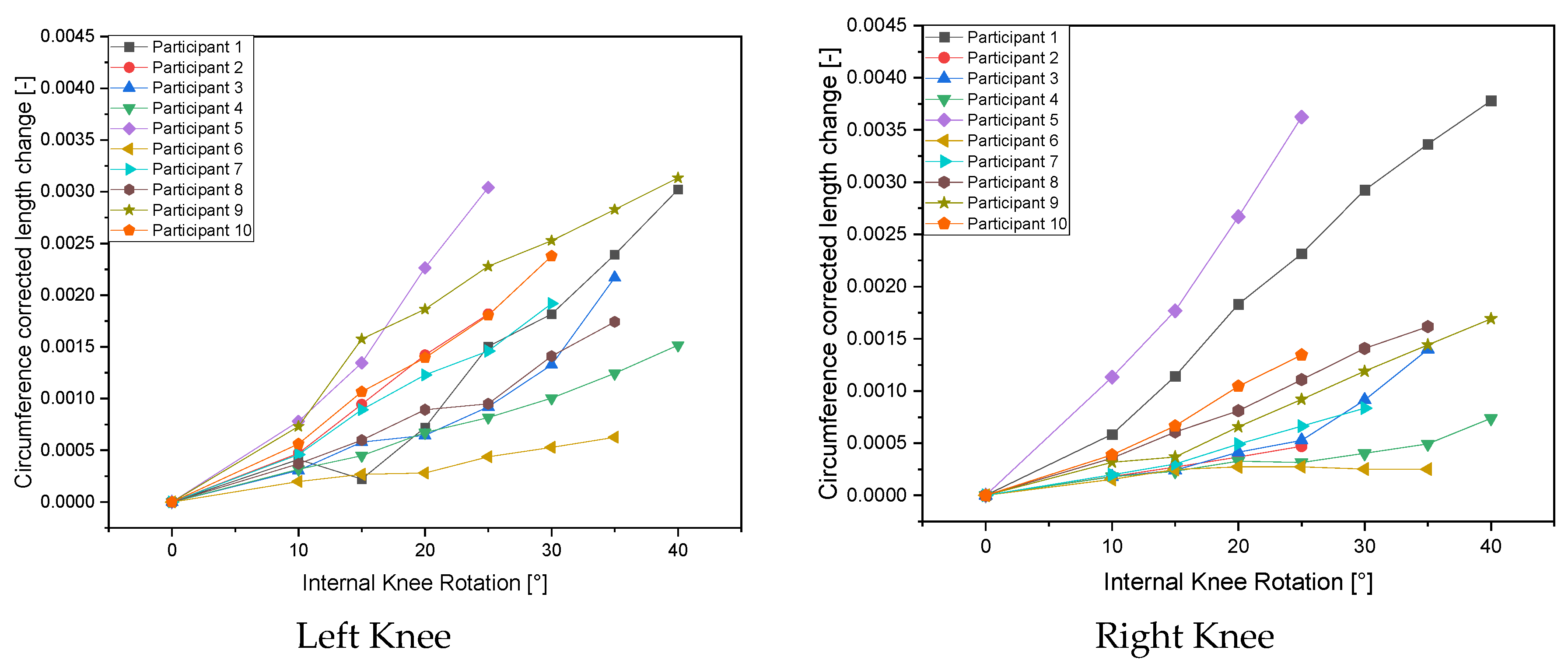
| Length Change in mm [31] | ||||||||
|---|---|---|---|---|---|---|---|---|
| Internal Knee Rotation | 0° | 10° | 15° | 20° | 25° | 30° | 35° | 40° |
| Left Knee Females | ||||||||
| Female 1 | 0 | 0.140 | 0.076 | 0.245 | 0.512 | 0.618 | 0.813 | 1.028 |
| Female 2 | 0 | 0.110 | 0.208 | 0.232 | 0.331 | 0.478 | 0.781 | |
| Female 3 | 0 | 0.104 | 0.148 | 0.222 | 0.270 | 0.332 | 0.410 | 0.500 |
| Female 4 | 0 | 0.166 | 0.269 | 0.402 | 0.428 | 0.635 | 0.784 | |
| Female 5 | 0 | 0.249 | 0.536 | 0.634 | 0.775 | 0.859 | 0.961 | 1.066 |
| Left Knee Males | ||||||||
| Male 1 | 0 | 0.212 | 0.426 | 0.640 | 0.818 | |||
| Male 2 | 0 | 0.344 | 0.592 | 0.996 | 1.338 | |||
| Male 3 | 0 | 0.068 | 0.091 | 0.095 | 0.149 | 0.180 | 0.213 | |
| Male 4 | 0 | 0.170 | 0.330 | 0.454 | 0.540 | 0.710 | ||
| Male 5 | 0 | 0.213 | 0.405 | 0.530 | 0.686 | 0.904 | ||
| Right Knee Females | ||||||||
| Female 1 | 0 | 0.199 | 0.388 | 0.623 | 0.787 | 0.994 | 1.144 | 1.285 |
| Female 2 | 0 | 0.064 | 0.087 | 0.149 | 0.190 | 0.329 | 0.503 | |
| Female 3 | 0 | 0.059 | 0.076 | 0.108 | 0.104 | 0.133 | 0.163 | 0.244 |
| Female 4 | 0 | 0.154 | 0.261 | 0.349 | 0.477 | 0.605 | 0.695 | |
| Female 5 | 0 | 0.108 | 0.126 | 0.223 | 0.313 | 0.404 | 0.490 | 0.575 |
| Right Knee Males | ||||||||
| Male 1 | 0 | 0.084 | 0.124 | 0.169 | 0.217 | |||
| Male 2 | 0 | 0.499 | 0.778 | 1.175 | 1.594 | |||
| Male 3 | 0 | 0.052 | 0.084 | 0.093 | 0.093 | 0.086 | 0.085 | |
| Male 4 | 0 | 0.071 | 0.109 | 0.177 | 0.239 | 0.301 | ||
| Male 5 | 0 | 0.149 | 0.256 | 0.402 | 0.518 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mayr, H.O.; Rosenstiel, N.; Prakash, K.S.; Comella, L.M.; Woias, P.; Schmal, H.; Seidenstuecker, M. Internal Rotation Measurement of the Knee with Polymer-Based Capacitive Strain Gauges versus Mechanical Rotation Measurement Taking Gender Differences into Account: A Comparative Analysis. Life 2024, 14, 142. https://doi.org/10.3390/life14010142
Mayr HO, Rosenstiel N, Prakash KS, Comella LM, Woias P, Schmal H, Seidenstuecker M. Internal Rotation Measurement of the Knee with Polymer-Based Capacitive Strain Gauges versus Mechanical Rotation Measurement Taking Gender Differences into Account: A Comparative Analysis. Life. 2024; 14(1):142. https://doi.org/10.3390/life14010142
Chicago/Turabian StyleMayr, Hermann O., Nikolaus Rosenstiel, Karthika S. Prakash, Laura Maria Comella, Peter Woias, Hagen Schmal, and Michael Seidenstuecker. 2024. "Internal Rotation Measurement of the Knee with Polymer-Based Capacitive Strain Gauges versus Mechanical Rotation Measurement Taking Gender Differences into Account: A Comparative Analysis" Life 14, no. 1: 142. https://doi.org/10.3390/life14010142
APA StyleMayr, H. O., Rosenstiel, N., Prakash, K. S., Comella, L. M., Woias, P., Schmal, H., & Seidenstuecker, M. (2024). Internal Rotation Measurement of the Knee with Polymer-Based Capacitive Strain Gauges versus Mechanical Rotation Measurement Taking Gender Differences into Account: A Comparative Analysis. Life, 14(1), 142. https://doi.org/10.3390/life14010142







