Abstract
Short chain fatty acids (SCFAs), the principle end-products produced by the anaerobic gut microbial fermentation of complex carbohydrates (CHO) in the colon perform beneficial roles in metabolic health. Butyrate, acetate and propionate are the main SCFA metabolites, which maintain gut homeostasis and host immune responses, enhance gut barrier integrity and reduce gut inflammation via a range of epigenetic modifications in DNA/histone methylation underlying these effects. The infant gut microbiota composition is characterized by higher abundances of SCFA-producing bacteria. A large number of in vitro/vivo studies have demonstrated the therapeutic implications of SCFA-producing bacteria in infant inflammatory diseases, such as obesity and asthma, but the application of gut microbiota and its metabolite SCFAs to necrotizing enterocolitis (NEC), an acute inflammatory necrosis of the distal small intestine/colon affecting premature newborns, is scarce. Indeed, the beneficial health effects attributed to SCFAs and SCFA-producing bacteria in neonatal NEC are still to be understood. Thus, this literature review aims to summarize the available evidence on the therapeutic potential of gut microbiota and its metabolite SCFAs in neonatal NEC using the PubMed/MEDLINE database.
1. Introduction
The gut microbiota composition and function undergo drastic changes during the first years of life [1] that are characterized by early microbial colonization with Escherichia and Bifidobacterium, which are gradually decreased following weaning and replaced by species of obligate anaerobic bacteria within the Firmicutes phylum, such as Coprococcus, Enterococcus, Roseburia and Clostridium [2,3,4]. The short-chain fatty acids (SCFAs), butyrate, propionate and acetate, are the main metabolic products of gut microbial Firmicutes phyla fermentation of complex non-digestible dietary substrates, such as fiber and resistant starch [5]. Bifidobacterium and lactic acid bacteria (LAB) produce lactate, which acts as an intermediate fermentation product for butyrate production [6]. In general, Bifidobacterium spp. are considered the primary colonizers of the breastfed infant gut, mainly due to the presence of human milk oligosaccharides (HMOs) [7,8,9,10]. The degradation of HMOs and complex carbohydrates (CHO) could result in high SCFA production (mainly butyrate and acetate), which can be used by other butyrogenic bacteria, such as Faecalibacterium prausnitzi (F. prausnitzi), Bacteroides and Roseburia, for growth by cross-feeding [7,8]. SCFAs produced by the infant-type Bifidobacterium spp. can enhance immunomodulatory responses by reducing inflammatory cytokines through the microbiota-gut-brain axis [10].
Necrotizing enterocolitis (NEC) is a severe inflammatory necrosis of the distal small intestine/colon that primarily affects preterm (less than 32 weeks’ gestation) or very low birth weight (VLBW: <1500 g) infants after the introduction of enteral feeds. NEC is characterized by hyperosmolar injury and intestinal ischemia, which reduce the integrity of the epithelial barrier that is evident by peritonitis, hemodynamic instability, abdominal tenderness/cellulitis, acute feeding intolerance, bacteremia and abdominal distension [11,12]. The aetiology of NEC is not clear, but it is thought to be related to several factors, including pre-eclampsia, aberrant bacterial colonization (e.g., infection), premature rupture of the membranes, placental abruption, intrauterine growth restriction, LBW, patent ductus arteriosus, sepsis and anemia [13]. Early gut microbial dysbiosis is also implicated in disease pathogenesis, in which the gut microbiota composition of preterm infants with NEC is characterized by reduced abundances of Bifidobacterium, Firmicutes and Bacteroidetes and increased abundances of Prevotella, Clostridioides, Staphylococcaceae, Proteobacteria, Enterobacteriaceae, Rothia, Streptococcus and Blautia [14,15,16,17,18,19,20].
Pregnancy and lactation perform a crucial role in shaping the composition of infant gut microbiota, which is influenced by a range of pre-and post-natal factors, such as antibiotic exposure, lactation stage, gestational age, mode of feeding/delivery, diet and body mass index (BMI) [3,17,21]. Maternal diet during pregnancy and lactation has been linked to an increased risk of developing obesity and asthma in the infant’s early years of life [22,23] and the mechanisms underlying such effects are postulated to be the alterations in maternal/infant gut microbiota and/or milk microbiota [21]. A high-fiber diet during pregnancy and lactation increases SCFAs production [21,22,23,24,25,26]. SCFAs are essential for differentiation of helper T cells (Th1, Th2) by their binding to G-protein coupled receptors (GPCRs), including free the fatty acid 2/3 receptor (FFAR2, FFAR3) present in the colon, thereby maintaining gut homeostasis and regulating inflammation by reducing the expression of pro-inflammatory cytokines [24,25]. Higher levels of SCFAs detected in breastmilk may enhance the neonatal anti-inflammatory immune responses by inducing factor fork head box protein 3 (FOXP3+) regulatory T (Treg) cell differentiation in the gut [27]. Breastmilk is a source of secretory IgA immunoglobulin A (SIgA) and IgA-producing antibody-secreting cells (ASCs), which regulate early gut microbiota maturation and immunity by binding to SCFA-producing Bifidobacterium and Lactobacillus, resulting in reduced NEC-related inflammation in preterm infants [28]. It has been suggested that infant feeding with probiotics-supplemented formulas and solid/complementary foods alter gut microbiota composition during the first years of life [9,29,30,31]. Evidence from randomised controlled trials (RCTs) has shown that NEC-specific treatments, such as oral lactoferrin combined with probiotics and parenteral/oral supplementation with arginine, reduce the disease risk [13,32,33,34,35]. Probiotic supplementation with Bifidobacterium and Lactobacillus strains, prebiotics (e.g., HMOs), synbiotics (mixtures of probiotics and prebiotics), long chain polyunsaturated fatty acid (PUFA) and bovine colostrum were also demonstrated by a large number of human RCTs, to be effective preventive strategies for NEC, which are thought to modulate the immune response and increase the abundance of beneficial gut microbes [36,37,38,39]. Breastfeeding has been demonstrated to have a protective role against NEC due to its potential to promote the colonization of commensal bacteria and decrease the susceptibility to gut dysbiosis in premature infants [40,41].
SCFAs contribute as mechanisms linking diet, gut microbiota and human health [5], resulting in induced epigenetic changes in the gene patterns of offspring, thereby being a potential epigenetic target in the treatment of gastrointestinal diseases during the first years of life. SCFAs could alter DNA and histone methylation patterns in several genes, resulting in reduced cytokines and chemokines with pro-inflammatory effects in the infant’s gut [22,23]. Findings from recent reviews in infants/children have demonstrated the potential efficacy of SCFA-producing bacteria in reducing inflammation-related disease risk, including obesity, asthma and inflammatory bowel diseases (IBD) [22,23,42]. However, no reviews yet discuss the role of SCFAs and SCFA-producing bacteria as therapeutic agents against neonatal NEC. Thus, this review aims to explore the therapeutic role of gut microbiota and its metabolite SCFAs in neonatal NEC. It is hypothesized that gut microbial-derived SCFA metabolites can be regarded as having health benefits in neonatal NEC. Preterm infants with NEC who are fed breastmilk/formula and/or supplemented with probiotics/prebiotics are postulated to have higher SCFA levels and abundance of SCFA-producing bacteria, which may perform a significant role in modulating the inflammatory immune responses of immature intestinal cells.
2. Methods
A literature search of PubMed/MEDLINE database was performed up to December 2022 to identify studies exploring the potential role of gut microbiota and its metabolite SCFAs in NEC treatment using the following keywords “NEC”, “preterm/premature infants”, “immature intestinal cells”, “intestinal inflammation”, “inflammatory biomarkers”, “gut microbiota”, “epigenetic”, “SCFAs”, “probiotics/prebiotics” and “feeding types”. The search was limited to retrieve human studies published in English irrespective of design.
3. Epigenetics and Inflammatory Biomarkers in NEC
Epigenetic alternation in the immature intestine, such as changes in DNA methylation and long non-coding RNA (lncRNA) patterns, may contribute to increased risk of NEC. Epigenetic changes are attributed to prenatal and postnatal factors (e.g., microbiome, intrauterine infection and enteral feeding) that may affect intestinal function/structure and cause upregulation of pro-inflammatory cytokines [43,44]. DNA methylation changes in cytosine-phosphate-guanine dinucleotides (CpG) regions of NEC-related genes are related to disease risk. For example, high levels of CpG methylation in the DNMT3A, TNT2/3, TNIP1, GALNT6 and HNF4 genes have been identified in stools and colons of premature infants with NEC [45,46,47]. An association of CpG methylation in the cytokine Oncostatin M (OSM) with NEC has also been observed, which can induce intestinal inflammation [47]. The hypermethylation of four genes (MPL, KDM6A, ZNF335 and RASAL3) has been reported in the intestine of neonatal NEC, which is associated with lymphocyte proliferation and intestinal epithelial permeability [48]. Analyses of CpG methylation positions in the intestinal epithelial cells of neonatal NEC revealed a significant hypermethylation in five genes (toll-like receptor 4; TLR4, ENOS, EPO, DEFA5 and VEGFA) at three sites [49]. Overexpression of micro-431 (miR-431) in the intestinal tissues of neonatal NEC results in significantly inhibited FOXA1 and HNF4A and increased pro-inflammatory (e.g., interleukins IL-6, IL-8, IL-10, LGR5, tumor necrosis factor-α; TNF-α and PRKCZ) gene expression in response to lipopolysaccharide (LPS) stimulation [50]. lncRNA influences the expression of mRNAs in the intestine tissues of neonatal NEC by upregulating expression levels of IL-6, IL-1β and TLR4 after LPS exposure, which induces activation of peroxisome proliferator-activated receptors (PPARs) and phosphatidylinositol-3 kinase/serine-threonine kinase (PI3K-AkT) signaling pathways, suggesting that lncRNA contributes to NEC pathogenesis [51].
NEC is characterized by decreased FOXP3+ Treg cell levels and gut expression of transforming growth factor β (TGF-β). Infants with NEC displayed elevated levels of nitric oxide (NO) and high cytokine expression levels with pro-inflammatory effects (e.g., Nuclear factor-κB; NF-κB, tumor necrosis factor-α; TNF-α, interferon; IFN-γ, IL-6, IL-8, IL-10, IL-1β) induced by LPS and produced by the cells of the adaptive immune system in response to colonization by pathogenic bacteria (e.g., Staphylococcus spp., and Clostridium spp.), thereby disturbing the integrity of epithelial tight junctions [52,53,54,55,56,57,58]. An experimental study has shown overexpression of TLR2 and TLR4 receptor-mediated IL-8 mRNA expression in the immature intestine of neonatal NEC [59]. Data from a human NEC experiment showed that pro-inflammatory cytokine expression of IL-1β, IL-1A, IL-6, TNF-α and IL-36 isoforms IL36A were increased in epithelial cells, whereas cytokines IL-37 and IL-22, which are considered protective, were decreased [60]. Evidence from an experimental study showed that IL-17F expression and its related pro-inflammatory C-X-C motif chemokines ligand 8 and 10 (CXCL8, CXCL10) are upregulated in the intestine of neonatal NEC [61]. A case–control study demonstrated higher levels of TNF-α, IL-8, IL-1β and lower levels of TGF-β, FOXP3+ Treg and IL-10 in the ileum of surgical NEC patients compared with matched controls (patients with spontaneous intestinal perforation/congenital intestinal atresia) [18]. Another case–control study showed that the levels of serum TNF-α, IL-6 and intestinal fatty acid-binding protein (I-FABP) were higher in NEC patients than non-NEC counterparts [62]. In a recent experimental study, preterm newborns displayed increased mRNA expression of fecal cytokines IL-1α/β, IL-7 and IL-12p40 [20]. This suggests that preterm infants with NEC display intestinal inflammation with markedly increased pro-inflammatory cytokines and chemokines, in which DNA methylation and lncRNA as epigenetic mechanisms are involved.
4. Insights into the SCFA-Producing Bacteria in Preterm Infants
SCFAs produced by gut microbiota act as epigenetic mechanisms in reducing intestinal inflammation by inducing DNA/histone methylation changes in the gene patterns of infants [22,23,42]. On this basis, it is important to provide an overview of SCFA-producing bacteria, such as Bifidobacterium, Lactobacillus, Enterococcus and Bacteroides, that may perform a crucial role in protecting from NEC-related inflammation.
The role of SCFAs in neonatal NEC treatment remains controversial. High luminal SCFAs production (e.g., butyric acid) by bacterial colonization in preterm infants is due to poor gastrointestinal motility and carbohydrates malabsorption [63]. Enteric bacterial pathogens, including Clostridium perfringens (C. perfringens), C. difficile, C. paraputrificum, C. butyricum and Klebsiella pneumoniae (K. pneumoniae) have shown to be implicated in NEC via increasing butyric acid production as result of lactose fermentation [64]. A high production of butyric acid by C. butyricum increases inducible nitric oxide synthase (iNOS) gene expression responsible for mucosal injury in NEC [65]. These findings suggest that excessive SCFAs produced by pathogenic bacteria may reduce the intestinal epithelial barrier integrity and increase metabolic inflammation in neonatal NEC. Thus, it is proposed that SCFA-producing commensal microbes (e.g., Bifidobacterium, Lactobacillus) may contribute to the regulation of gut immune homeostasis.
Preterm infants demonstrated a significantly less diverse microbiome, including Bifidobacterium spp. [14,15,16,17,18,19,20]. Bifidobacterium spp. within the Actinobacteria phylum are Gram-positive non-motile/spore forming bacteria [66,67] dominated in the gut of breastfed infants [10]. Several strains belonging to Bifidobacterium spp., including B. breve, B. longum subsp. longum, B. longum subsp. infantis and B. bifidum, are among the prevalent members of breastmilk [68,69,70,71,72,73]. The genomes of Bifidobacterium strains include a large set of enzymes belonging to the glycosyl hydrolase family (β-N-acetylhexosaminidase, α-L-fucosidases) essential for HMO degradation in the breastfed infant gut via the intracellular galacto-N-biose/lacto-N-biose (GNB/LNB) pathway [70,74,75]. HMOs, such as galacto-oligosaccharide (GOS) and fructo-oligosaccharide (FOS), may act as prebiotics, which perform a key role in the development of the infant gut microbiota [76]. FOS promotes the growth of B. breve and B. bifidum in preterm fecal microbiota, which produce high levels of butyric, propionic and acetic acids [77]. Fermentation of resistant starch by Bifidobacterium spp. has been shown to increase production of acetate, propionate and butyrate in pre-weaning and weaning infant feces [78].
Lactobacillus is a genus of Gram-positive facultative LAB that is typically classified in the class Bacilli, phylum Firmicutes [66,79]. Lactobacillus spp. were detected at a relatively high percentage in the meconium of preterm infants [80,81]. Breastmilk and the breast-fed infant gut are dominated by several Lactobacillus spp. mainly L. rhamnosus, L. gasseri, L. reuteri, L. acidophilus, L. fermentum, L. crispatus, L. paracasei and L. salivarius [68,69,82,83,84,85]. Lactobacillus spp. produce high D(−), L(+) and DL-Lactic acid levels [86], which have the ability to generate SCFAs, bacteriocins and FOS [87,88].
Analysis of the fecal and meconium microbiota of preterm infants revealed a high abundance of Enterococcus [80,89,90]. E. faecalis and E. faecium constitute the most dominant Enterococcus of fecal microbiota in preterm infants [80]. The genus Enterococcus belongs to a large group of LAB in the class Bacilli that is typically identified as facultative anaerobic bacteria within the Firmicutes phylum [66,79,91]. Enterococcus spp. produce L(+)-Lactic acid as the main end metabolic product yielded from sugar fermentation [86]. Enterococcus increases the production of acetate, propionate and butyrate in pre-weaned and weaning infants’ feces upon fermentation of resistant starch [78]. The E. faecalis strain ATCC19433 exhibits growth in response to fucosylated HMOs (2′-FL or 3-FL) and produces lactate [92]. The E. faecalis strain AG5 has been found to assimilate cholesterol and produce propionate in vitro [93].
Multiple Streptococcus spp. (S. thermophilus, S. mitis, S. anginosus and S. sanguinis) dominated the meconium microbiome of preterm infants during the first 21 days of early life [80]. The genus Streptococcus is a facultative anaerobe Gram-positive bacteria within the Firmicutes phylum [94]. S. thermophilus has been shown to produce L(+)-Lactic acid as the major fermentative end-product [86]. Such species can use the acetyl-CoA “Wood-Ljungdahl” pathway of carbon dioxide (CO2) fixation as the main mechanism for transforming pyruvate to acetate [95]. Fucosylated HMOs (2-FL or 3-FL) are found to be metabolized into lactate by the S. thermophilus strain ATCC19258 [92].
The genus Bacteroides that belongs to the phylum Bacteroidetes, is the most abundant Gram-negative anaerobic bacteria in the fecal microbiota of preterm infants [96]. B. fragilis was the species that predominated in the fecal microbiota of preterm infants in the first weeks of life [97,98]. Bacteroides spp. have large genomes with extremely high numbers of carbohydrate cleaving enzymes [99,100,101], which degraded complex oligosaccharides, such as mucin glycans [102] and HMOs [103,104,105]. Butyrate, acetate and propionate were the major end-products of resistant starch fermentation generated by Bacteroides spp. in weaned infants’ feces [78]. The acetyl-CoA and succinate pathways are the major routes for the production of acetate and propionate, which exist mainly in Bacteroides spp. [95,106,107,108].
5. Effects of Feeding Types on Gut Microbiota and Its Metabolite SCFAs in Preterm Infants
Evidence from several prospective cohort studies and RCTs suggests that breastmilk and/or formula with probiotics/prebiotics may have the potential to enhance the growth of SCFA-producing bacteria and increase SCFAs levels in preterm infants.
5.1. Prospective Cohort Studies
A cohort study over 1-year period has demonstrated the potential of breastmilk and formula to influence fecal SCFA profiles in LBW preterm infants. The concentrations of fecal acetate and propionate were found to be higher in infants who were fed breastmilk, whereas the concentrations of fecal butyrate were higher in those fed Similac special care formula [109]. It has been has shown that premature infants fed formula have higher concentrations of butyrate and acetate, while those fed breastmilk have higher concentrations of propionate in their feces over 1-year follow-up. This may be due to the colonization of SCFA-producing Bifidobacterium and Lactobacillus influenced by breastmilk and formula [110]. A study evaluated the beneficial effects of probiotics supplementation in preterm infants over 100-day period and found that a combination of B. bifidum with L. acidophilus (Bif/Lacto) increases fecal lactate levels and the abundance of Bifidobacterium spp. consistent with their ability to metablize HMOs into acetate [111].
Over a 10-year longitudinal study, preterm infants who were fed breastmilk or supplemented with two different probiotics (Infloran and Labinic) showed a significant increase in the relative abundance of Bifidobacterium spp. and a significant decrease in the relative abundance of pathogenic bacteria in their feces. The study suggests that long-term colonization of Bifidobacterium depends on the type of probiotics used [112]. In a recent study, with follow-up over 1 year, aimed to identify variation in fecal microbiota from admission to discharge, preterm infants who were fed breastmilk demonstrated a higher abundance of Bifidobacterium spp. and lower abundance of Veillonella. However, infants who were fed probiotic formula demonstrated a lower abundance of Lactobacillus [113]. A cohort study showed that the gut microbiota colonization varied among preterm infants as a result of probiotic formula-feeding. Bifidobacterium and Lactobacillus were found in higher abundance in the fecal microbiota of preterm infants fed with formula supplemented with probiotic B. lactis over 3-month period [114]. Use of the probiotic B. longum subsp. infantis EVC001 in conjunction with breastmilk has been shown to increase the gut microbiome abundance of Bifidobacteriaceae and decrease the abundance of Staphylococcaceae and Enterobacteriaceae associated with gut dysbiosis and antibiotic-resistance in preterm infants in longitudinal 5 months of follow-up [115]. The relative abundances of Bifidobacterium spp. have been found to increase the fecal microbiota of preterm infants fed with breastmilk and human donor milk during the first three months of life [116]. In a study conducted to examine the effect of breastmilk, donor human milk or formula on shaping the fecal microbiota of preterm infants during the first month of life, infants fed with mother’s own milk have higher fecal SCFA-producing bacteria compared with those fed donor human milk or formula [117]. A previous study found that breastmilk influences the microbial colonization of preterm infants over the first 30 days of life. Breastmilk fed infants have higher abundance in Lactobacillus and Granulicatella than non-breast milk fed infants [118].
A study found that oral administration of B. breve M-16V to LBW infants resulted in increased fecal abundance of Bifidobacterium and Enterococcus 10 weeks post-administration. This is attributed to acetic acid, which may inhibit the growth of Proteobacteria, thus providing a suitable environment for SCFA-producing bacteria growth [119]. Evidence from a cohort study supports supplementation with multiple-strain probiotics including bifidobacteria in preterm infants. Three Bifidobacterium strains have been administrated in infants showing lower detection rates of Enterobacteriaceae and higher rates of bifidobacteria in the feces over 6-month follow-up [120]. A longitudinal multi-center study has shown that the fecal microbiota of preterm infants after supplementation with probiotic Infloran have a high relative abundance of Bifidobacterium and Lactobacillus up to 4 months of age [121]. Another multi-center cohort study showed that administering a combination probiotics mixture to preterm infants resulted in influenced the fecal microbiota profile with Lactobacillus and Bifidobacterium predominating over 5-month period [122]. In a cohort study over a 5-month follow-up, suspected bacterial signatures from Bifidobacterium and Lactobacillus were identified in the fecal microbiota of preterm infants after discontinuation of a probiotic mixture containing Bifidobacterium and Lactobacillus spp. [123].
In one cohort study, the administrated strain, B. bifidum ATCC15696 and L. acidophilus NCIMB701748, showed significant alterations in the fecal microbiota of preterm infants as demonstrated by high Lactobacillus and Bifidobacterium abundances over 1-month period [124]. A cohort study on human milk-fed preterm infants has indicated probiotic supplementation with B. longum subsp. infantis influences the fecal colonization by Bifidobacterium [125]. Probiotic supplementation with L. rhamnosus GG and B. animalis ssp. lactis BB-12 increases the relative abundance of Firmicutes and Actinobacteria and decreases the abundance of Weissella, Veillonella and Klebsiella in preterm infants during the first month of life [126]. A recent study showed that supplementation of probiotics rich in L. acidophilus and B. bifidum alters the fecal microbiota of preterm infants during the first 30 days of life by increasing Lactobacillus spp. and E. faecium abundances [127].
5.2. RCTs
A previous study resulted in increased fecal colonization with bifidobacteria and acetic acid levels in premature infants after receiving formula supplemented with prebiotic/probiotic combinations compared to those in the placebo group [128]. In a recent study, multi-strain probiotics are found to be effective in increasing fecal butyric and propionic acid levels, whereas single-strain probiotic increases fecal butyric acid levels only in preterm infants. Infants who were supplemented with probiotics showed higher fecal abundance of Bifidobacterium spp. and lower fecal abundance of Clostridium [129]. An RCT showed that preterm infants receiving probiotic supplementation with the B. breve (BBG-01) strain in conjunction with breastmilk and feeding with maternal colostrum have higher fecal Bifidobacterium abundance compared with those in placebo groups [130]. In one previous study, supplementation of a bovine milk formula with galacto and fructo-oligosaccharide mixtures has been shown to increase the relative abundance of fecal bifidobacteria in preterm infants [131]. Preterm infants supplemented with a probiotic mixture containing S. thermophilus TH-4, B. longum subsp. infantis BB-02 and B. animalis subsp. lactis BB-12 showed a significant increase in the relative abundance of Bifidobacterium spp. in the gut microbiota compared to those in the placebo group [132]. Supplementation of preterm infants with the B. lactis Bb12 probiotic strain compared with placebo modulates the gut microbiota by lowering the cell counts of clostridia and enterobacteria and increasing the cell count of bifidobacteria [133]. Probiotic supplementation with L. reuteri DSM 17938 modulates the gut microbiota composition in preterm infants by increasing the relative abundance of Lactobacillus and decreasing the abundance of Clostridium, Enterobacteriaceae and Staphylococcaceae [134]. A supplementation with a mixture of S. thermophilus TH-4, B. animalis subsp. lactis BB-12 and B. longum subsp. infantis BB-02 increases the bacterial abundance of probiotic species in the preterm infant’s gut [135].
The effects of feeding types on fecal SCFAs and SCFA-producing bacteria in preterm infants are summarized in Table 1.

Table 1.
Effects of feeding types on gut microbiota and its metabolite SCFAs bacteria in preterm infants.
6. Role of Gut Microbiota and Its Metabolite SCFAs as Therapeutic Potential Agents in NEC
Gene expression including cytokines and chemokines result from histone and long non-coding RNA (lncRNA) modifications have been linked to immune cell function and inflammation in NEC [45,46,47,48,49,50,51]. Given that SCFAs have been identified as epigenetic modifier exert anti-inflammatory effects in inflammatory diseases [22,23,42], it is likely that SCFA-producing bacteria and SCFAs could perform an epigenetic role in modulating immune responses in the inflamed gut of neonatal NEC by reducing pro-inflammatory cytokines and chemokines. Thus, this section presents the therapeutic role of gut microbiota and its metabolite SCFAs in regulating NEC-related inflammation in which epigenetic changes are implicated.
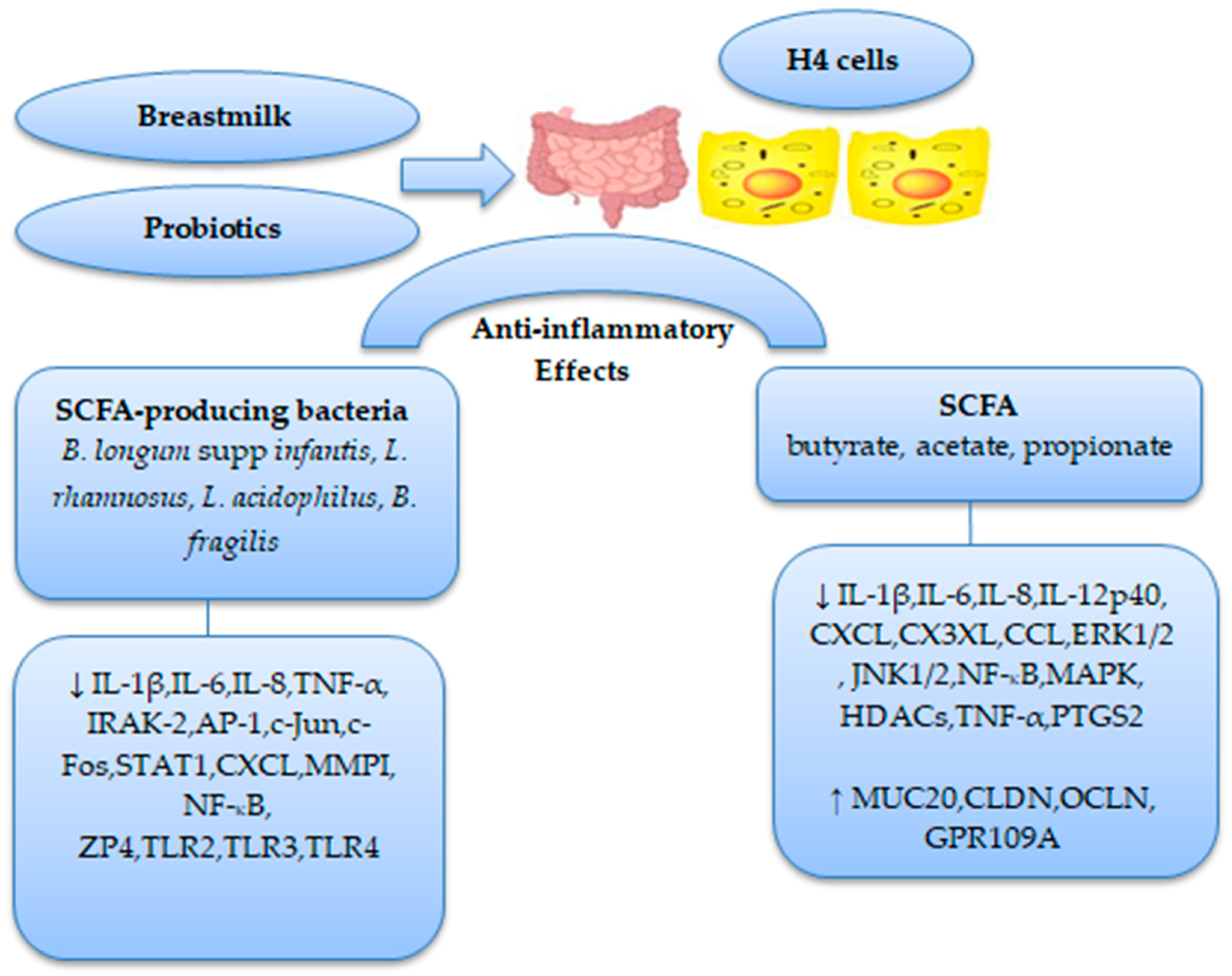
Evidence from a few studies has revealed a significant decrease in the levels of butyric, propionic and acetic acids in NEC patients [18,19]. It has been shown that colonization of fecal microbiota of NEC patients with Firmicutes and Bacteroidetes increases butyric acid synthesis, resulting in increased Treg/Thelper cell ratio [18]. An in vitro study showed that butyrate inhibits IL-1β-induced IL-6, CX3XL1 and CXCL5 gene expression in human immature enterocytes (H4 cells) and regulates tight junction and mucin-related gene expression via increasing the mRNA expression of Mucin (MUC20), Claudins (CLDN4, CLDN11 and CLDN15) and Occludin (OCLN) [136]. In fetal small intestinal epithelial FHs 74 Int cells, butyrate, acetate and propionate were found to decrease IL-1β-induced IL-6 and IL-8 mRNA levels through inhibiting the activation of extracellular signal-regulated kinase 1/2 (ERK1/2), c-JUN NH2-terminal kinase 1/2 (JNK1/2) and NF-κB p65 signaling pathways [137]. Treatment of fetal immature enterocytes (H4 cells) with butyrate, acetate and propionate results in a significant inhibition of IL-1β-induced histone deacetylase 3 and 5 (HDAC3, HDAC5) and IL-8 mRNA expression and activation of G-protein coupled receptor 109A (GPR109A) mRNA expression [24]. Butyrate and propionate have been shown to reduce inflammation in vitro by inhibiting several chemokines (e.g., CCL3, CCL4, CCL5, CCL9) and LPS-induced IL-6 and IL-12p40 mRNA expression in both mature and immature human monocyte-derived dendritic cells (DCs) [138]. In vitro treatment of amnion epithelial and mesenchymal cells in preterm infants with butyrate and propionate inhibit several inflammation-induced cytokines and chemokines (TNF-α, IL-6, IL-1β, CCL2, CCL8, CXCL5, CXCL8 and CXCL10) and prostaglandin (PTGS2) mRNA expression through suppressing activation of NF-κB and mitogen-activated protein kinase (MAPK) signaling pathways [139].
In one experimental study, supplementation with B. infantis EVC001 strain resulted in decreased IL-1β and TNFα production in preterm infants [115]. An in vitro human model showed that probiotic L. rhamnosus GG attenuates fetal intestinal epithelial cell line H4 inflammatory responses by inhibiting TLR3 and TLR4 mRNA expression and Salmonella Typhimurium (S. Typhimurium)-induced TNF-α mRNA expression [140]. Another in vitro study demonstrated a potential inhibitory effect of B. infantis and L. acidophilus on TLR2/TLR4 mRNA expression and IL-1β/LPS-induced IL-6 and IL-8 mRNA expression in fetal immature enterocytes FHs74 [141]. Pretreatment of immature enterocyte H4 cells with B. longum supp infantis resulted in suppression of interleukin-1 receptor-associated kinase 2 (IRAK-2) and IL-1β-induced IL-6 and activator-protein 1 (AP-1) transcription factors c-Jun and c-Fos mRNA expression in a TLR-4-dependent manner [142]. It has also been shown that IL-1β-induced IL-8 mRNA expression is inhibited via downregulating the signal transducer and activator of the transcription 1 (STAT1) signaling pathway in immature enterocyte H4 cells pretreated with indole-3-lactic acid (ILA), a predominant breastmilk tryptophan metabolite, produced by B. longum supp infantis [143]. Treatment with the probiotic strains B. infantis and L. acidophilus modulates the inflammatory response of immature enterocyte H4 cells by inhibiting IL-1β-induced IL-6 and IL-8 mRNA expression and NF-κB p65 levels [144]. Two studies have shown that Polysaccharide (PSA) pretreatment produced by B. fragilis reduces inflammation in immature enterocyte H4 cells by reducing IL-1β-induced IL-8, CXCL5, CXCL10, matrix metalloproteinase-1 (MMPI), P-c-Jun and zona pellucida protein 4 (ZP4) mRNA expression in both TLR2 and TLR4 dependent-manner [145,146].
Taken together, these findings suggest that SCFAs and SCFA-producing bacteria may have a potential anti-inflammatory role in neonatal NEC by protecting fetal intestinal epithelial cells against pro-inflammatory cytokines and chemokines via inhibition of different cellular signaling pathways.
Figure 1 summarizes the therapeutic role of SCFAs and SCFA-producing bacteria in neonatal NEC.
Figure 1.
Role of SCFAs and its producing bacteria in neonatal NEC therapy. (↓) decrease; (↑) increase.
7. Conclusions
SCFAs as epigenetic substrates perform a significant role in mediating microbe-host immune interactions, which could be a potential treatment for NEC-induced inflammation. During the colonization process in preterm infants, the gut is exposed to microbes that are more pathogenic but less commensal, which may contribute to NEC by increasing TLR4 signaling, leading to release of pro-inflammatory cytokines and chemokines. Breastmilk and/or formula with probiotics/prebiotics could modulate preterm infants’ gut microbiota colonization by decreasing the growth of pathogenic microbes, while increasing microbial species belonging to phyla Actinobacteria (Bifidobacterium spp.), Firmicutes (Lactobacillus spp., Enterococcus spp., Streptococcus spp.) and Bacteroidetes (B. fragilis), which produce different amounts of SCFAs.
SCFAs and SCFA-producing bacteria exert anti-inflammatory effects on cytokine and chemokine production in immature enterocyte H4 cells through inhibiting different signaling pathways. Breastmilk and feeding with probiotic/prebiotic formula increase SCFA production and the abundance of SCFA-producing bacteria in preterm infants. However, how these feeding types epigenetically determine NEC phenotype by exerting anti-inflammatory effects are still being unraveled. In conclusion, SCFAs and SCFA-producing bacteria could be potential targets in the treatment of NEC. Further studies are needed to examine whether breastmilk or feeding with probiotic/prebiotic formula could increase SCFA levels and influence the growth of SCFA-producing bacteria and the protective effects thereof on reducing NEC-related inflammatory markers through the epigenetic mechanisms.
Funding
This review received no financial support.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The author declares no conflict of interest.
References
- Bäckhed, F.; Roswall, J.; Peng, Y.; Feng, Q.; Jia, H.; Kovatcheva-Datchary, P.; Li, Y.; Xia, Y.; Xie, H.; Zhong, H.; et al. Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe. 2015, 17, 690–703. [Google Scholar] [CrossRef]
- Mesa, M.D.; Loureiro, B.; Iglesia, I.; Fernandez Gonzalez, S.; Olivé, E.L.; Garcia-Algar, O.; Solana, M.J.; Perez, M.J.C.; Sainz, T.; Martinez, L.; et al. The evolving microbiome from pregnancy to early infancy: A comprehensive review. Nutrients 2020, 12, 133. [Google Scholar] [CrossRef]
- Yao, Y.; Cai, X.; Ye, Y.; Wang, F.; Chen, F.; Zheng, C. The role of microbiota in infant health: From early life to adulthood. Front. Immunol. 2021, 12, 708472. [Google Scholar] [CrossRef]
- Oyedemi, O.T.; Shaw, S.; Martin, J.C.; Ayeni, F.A.; Scott, K.P. Changes in the gut microbiota of Nigerian infants within the first year of life. PLoS ONE 2022, 17, e0265123. [Google Scholar] [CrossRef] [PubMed]
- Ríos-Covián, D.; Ruas-Madiedo, P.; Margolles, A.; Gueimonde, M.; de Los Reyes-Gavilán, C.G.; Salazar, N. Intestinal short chain fatty acids and their link with diet and human health. Front. Microbiol. 2016, 7, 185. [Google Scholar] [CrossRef] [PubMed]
- Den Besten, G.; van Eunen, K.; Groen, A.K.; Venema, K.; Reijngoud, D.; Bakker, B.M. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J. Lipid Res. 2013, 54, 2325–2340. [Google Scholar] [CrossRef] [PubMed]
- Kumar, H.; Collado, M.C.; Wopereis, H.; Salminen, S.; Knol, J.; Roeselers, G. The bifidogenic effect revisited-ecology and health perspectives of bifidobacterial colonization in early life. Microorganisms 2020, 8, 1855. [Google Scholar] [CrossRef]
- Stuivenberg, G.A.; Burton, J.P.; Bron, P.A.; Reid, G. Why are bifidobacteria important for infants? Microorganisms 2022, 10, 278. [Google Scholar] [CrossRef]
- Di Profio, E.; Magenes, V.C.; Fiore, G.; Agostinelli, M.; La Mendola, A.; Acunzo, M.; Francavilla, R.; Indrio, F.; Bosetti, A.; D’Auria, N.; et al. Special diets in infants and children and impact on gut microbioma. Nutrients 2022, 14, 3198. [Google Scholar] [CrossRef]
- Lin, C.; Lin, Y.; Zhang, H.; Wang, G.; Zhao, J.; Zhang, H.; Chen, W. Intestinal ‘infant-type’ bifidobacteria mediate immune system development in the first 1000 days of life. Nutrients 2022, 14, 1498. [Google Scholar] [CrossRef]
- Gregory, K.E.; Deforge, C.E.; Natale, K.M.; Phillips, M.; Van Marter, L.J. Necrotizing enterocolitis in the premature infant: Neonatal nursing assessment, disease pathogenesis, and clinical presentation. Adv. Neonatal Care 2011, 11, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.K.; Shah, J.S. Necrotizing enterocolitis in very low birth weight infants: A systemic review. ISRN Gastroenterol. 2012, 2012, 562594. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.T.; Patel, R.M. A critical analysis of risk factors for NEC. Semin. Fetal Neonatal Med. 2018, 23, 374–379. [Google Scholar] [CrossRef]
- Torrazza, R.M.; Ukhanova, M.; Wang, X.; Sharma, R.; Hudak, M.L.; Neu, J.; Mai, V. Intestinal microbial ecology and environmental factors affecting necrotizing enterocolitis. PLoS ONE 2013, 8, e83304. [Google Scholar] [CrossRef] [PubMed]
- Unger, S.; Stintzi, A.; Shah, P.; Mack, D.; O’Connor, D.L. Gut microbiota of the very-low-birth-weight infant. Pediatr. Res. 2015, 77, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Pammi, M.; Cope, J.; Tarr, P.I.; Warner, B.B.; Morrow, A.L.; Mai, V.; Gregory, K.E.; Kroll, J.S.; McMurtry, V.; Ferris, M.J.; et al. Intestinal dysbiosis in preterm infants preceding necrotizing enterocolitis: A systematic review and meta-analysis. Microbiome 2017, 5, 31. [Google Scholar] [CrossRef]
- Underwood, M.A.; Mukhopadhyay, S.; Lakshminrusimha, S.; Bevins, C.L. Neonatal intestinal dysbiosis. J. Perinatol. 2020, 40, 1597–1608. [Google Scholar] [CrossRef]
- He, Y.; Du, W.; Xiao, S.; Zeng, B.; She, X.; Liu, D.; Du, H.; Li, L.; Li, F.; Ai, Q.; et al. Colonization of fecal microbiota from patients with neonatal necrotizing enterocolitis exacerbates intestinal injury in germfree mice subjected to necrotizing enterocolitis-induction protocol via alterations in butyrate and regulatory T cells. J. Transl. Med. 2021, 19, 510. [Google Scholar] [CrossRef]
- Liu, X.-C.; Du, T.-T.; Gao, X.; Zhao, W.-J.; Wang, Z.-L.; He, Y.; Bao, L.; Li, L.-Q. Gut microbiota and short-chain fatty acids may be new biomarkers for predicting neonatal necrotizing enterocolitis: A pilot study. Front. Microbiol. 2022, 13, 969656. [Google Scholar] [CrossRef]
- Lemme-Dumit, J.M.; Song, Y.; Lwin, H.W.; Hernandez-Chavez, C.; Sundararajan, S.; Viscardi, R.M.; Ravel, J.; Pasetti, M.F.; Ma, B. Altered gut microbiome and fecal immune phenotype in early preterm infants with leaky gut. Front. Immunol. 2022, 13, 815046. [Google Scholar] [CrossRef]
- Alsharairi, N.A. The infant gut microbiota and risk of asthma: The effect of maternal nutrition during pregnancy and lactation. Microorganisms 2020, 8, 1119. [Google Scholar] [CrossRef] [PubMed]
- Alsharairi, N.A. The role of short-chain fatty acids in mediating very low-calorie ketogenic diet-infant gut microbiota relationships and its therapeutic potential in obesity. Nutrients 2021, 13, 3702. [Google Scholar] [CrossRef] [PubMed]
- Alsharairi, N.A. The role of short-chain fatty acids in the interplay between a very low-calorie ketogenic diet and the infant gut microbiota and its therapeutic implications for reducing asthma. Int. J. Mol. Sci. 2020, 21, 9580. [Google Scholar] [CrossRef] [PubMed]
- Zheng, N.; Gao, Y.; Zhu, W.; Meng, D.; Walker, W.A. Short chain fatty acids produced by colonizing intestinal commensal bacterial interaction with expressed breast milk are anti-inflammatory in human immature enterocytes. PLoS ONE 2020, 15, e0229283. [Google Scholar] [CrossRef] [PubMed]
- Ziętek, M.; Celewicz, Z.; Szczuko, M. Short-chain fatty acids, maternal microbiota and metabolism in pregnancy. Nutrients 2021, 13, 1244. [Google Scholar] [CrossRef] [PubMed]
- Łoniewski, I.; Skonieczna-Żydecka, K.; Stachowska, L.; Fraszczyk-Tousty, M.; Tousty, P.; Łoniewska, B. Breastfeeding affects concentration of faecal short chain fatty acids during the first year of life: Results of the systematic review and meta-analysis. Front. Nutr. 2022, 9, 939194. [Google Scholar] [CrossRef] [PubMed]
- Chun, J.; Toldi, G. The impact of short-chain fatty acids on neonatal regulatory T cells. Nutrients 2022, 14, 3670. [Google Scholar] [CrossRef]
- Guo, J.; Ren, C.; Han, X.; Huang, W.; You, Y.; Zhan, J. Role of IgA in the early-life establishment of the gut microbiota and immunity: Implications for constructing a healthy start. Gut Microbes. 2021, 13, 1908101. [Google Scholar] [CrossRef]
- McKeen, S.; Young, W.; Mullaney, J.; Fraser, K.; McNabb, W.C.; Roy, N.C. Infant complementary feeding of prebiotics for the microbiome and immunity. Nutrients 2019, 11, 364. [Google Scholar] [CrossRef]
- Differding, M.K.; Benjamin-Neelon, S.E.; Hoyo, C.; Østbye, T.; Mueller, N.T. Timing of complementary feeding is associated with gut microbiota diversity and composition and short chain fatty acid concentrations over the first year of life. BMC Microbiol. 2020, 20, 56. [Google Scholar] [CrossRef]
- Fabiano, V.; Indrio, F.; Verduci, E.; Calcaterra, V.; Pop, T.L.; Mari, A.; Zuccotti, G.V.; Cokugras, F.C.; Pettoello-Mantovani, M.; Goulet, O. Term infant formulas influencing gut microbiota: An overview. Nutrients 2021, 13, 4200. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, K.; Lyttle, A.; Amin, H.; Shaireen, H.; Robertson, H.L.; Lodha, A.K. Arginine supplementation in prevention of necrotizing enterocolitis in the premature infant: An updated systematic review. BMC Pediatr. 2014, 14, 226. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.S.; Shah, V.S.; Kelly, L.E. Arginine supplementation for prevention of necrotising enterocolitis in preterm infants. Cochrane Database Syst. Rev. 2017, 4, CD004339. [Google Scholar] [CrossRef] [PubMed]
- Pammi, M.; Suresh, G. Enteral lactoferrin supplementation for prevention of sepsis and necrotizing enterocolitis in preterm infants. Cochrane Database Syst. Rev. 2020, 3, CD007137. [Google Scholar] [CrossRef]
- Al-Alaiyan, S.; Abdulaziz, N.; Alkohlani, A.; Almairi, S.O.; Al Hazzani, F.; Binmanee, A.; Alfattani, A. Effects of probiotics and lactoferrin on necrotizing enterocolitis in preterm infants. Cureus 2021, 13, e18256. [Google Scholar] [CrossRef]
- Zhou, P.; Li, Y.; Ma, L.-Y.; Lin, H.-C. The role of immunonutrients in the prevention of necrotizing enterocolitis in preterm very low birth weight infants. Nutrients 2015, 7, 7256–7270. [Google Scholar] [CrossRef]
- Johnson-Henry, K.C.; Abrahamsson, T.R.; Wu, R.Y.; Sherman, P.M. Probiotics, prebiotics, and synbiotics for the prevention of necrotizing enterocolitis. Adv. Nutr. 2016, 7, 928–937. [Google Scholar] [CrossRef]
- Nolan, L.S.; Rimer, J.M.; Good, M. The role of human milk oligosaccharides and probiotics on the neonatal microbiome and risk of necrotizing enterocolitis: A narrative review. Nutrients 2020, 12, 3052. [Google Scholar] [CrossRef]
- Campos-Martinez, A.M.; Expósito-Herrera, J.; Gonzalez-Bolívar, M.; Fernández-Marin, E.; Uberos, J. Evaluation of risk and preventive factors for necrotizing enterocolitis in premature newborns. A systematic review of the literature. Front. Pediatr. 2022, 10, 874976. [Google Scholar] [CrossRef]
- Xu, W.; Judge, M.P.; Maas, K.; Hussain, N.; McGrath, J.M.; Henderson, W.A.; Cong, X. Systematic review of the effect of enteral feeding on gut microbiota in preterm infants. J. Obstet. Gynecol. Neonatal Nurs. 2018, 47, 451–463. [Google Scholar] [CrossRef]
- Davis, J.A.; Baumgartel, K.; Morowitz, M.J.; Giangrasso, V.; Demirci, J.R. The role of human milk in decreasing necrotizing enterocolitis through modulation of the infant gut microbiome: A scoping review. J. Hum. Lact. 2020, 36, 647–656. [Google Scholar] [CrossRef] [PubMed]
- Alsharairi, N.A. The therapeutic role of short-chain fatty acids mediated very low-calorie ketogenic diet-gut microbiota relationships in paediatric inflammatory bowel diseases. Nutrients 2022, 14, 4113. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.; Claud, E.C. Intrauterine inflammation, epigenetics, and microbiome influences on preterm infant health. Curr. Pathobiol. Rep. 2018, 6, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Nair, J.; Maheshwari, A. Epigenetics in necrotizing enterocolitis. Curr. Pediatr. Rev. 2021, 17, 172–184. [Google Scholar] [CrossRef]
- Good, M.; Chu, T.; Shaw, P.; McClain, L.; Chamberlain, A.; Castro, C.; Rimer, J.M.; Mihi, B.; Gong, Q.; Nolan, L.S.; et al. Global hypermethylation of intestinal epithelial cells is a hallmark feature of neonatal surgical necrotizing enterocolitis. Clin. Epigenet. 2020, 12, 190. [Google Scholar] [CrossRef]
- Good, M.; Chu, T.; Shaw, P.; Nolan, L.S.; McClain, L.; Chamberlain, A.; Castro, C.; Gong, Q.; Cooksey, K.; Linneman, L.; et al. Neonatal necrotizing enterocolitis-associated DNA methylation signatures in the colon are evident in stool samples of affected individuals. Epigenomics 2021, 13, 829–844. [Google Scholar] [CrossRef]
- Good, M.; Chu, T.; Shaw, P.; Nolan, L.S.; Wrobleski, J.; Castro, C.; Gong, Q.; DeWitt, O.; Finegold, D.N.; Peters, D. Selective hypermethylation is evident in small intestine samples from infants with necrotizing enterocolitis. Clin. Epigenet. 2022, 14, 49. [Google Scholar] [CrossRef]
- Lu, L.; Fan, J.; Xu, W.; Cui, X.; Hu, S.; Guo, T.; Lv, Z. DNA methylome mapping identifies epigenetic abnormalities in intestinal lymphocyte regulation in human necrotizing enterocolitis. Dig. Dis. Sci. 2022, 67, 4434–4443. [Google Scholar] [CrossRef]
- Klerk, D.H.; Plösch, T.; Verkaik-Schakel, R.N.; Hulscher, J.B.F.; Kooi, E.M.W.; Bos, A.F. DNA methylation of TLR4, VEGFA, and DEFA5 is associated with necrotizing enterocolitis in preterm infants. Front. Pediatr. 2021, 9, 630817. [Google Scholar] [CrossRef]
- Wu, Y.Z.; Chan, K.Y.Y.; Leung, K.T.; Lam, H.S.; Tam, Y.H.; Lee, K.H.; Li, K.; Ng, P.C. Dysregulation of miR-431 and target gene FOXA1 in intestinal tissues of infants with necrotizing enterocolitis. FASEB J. 2019, 33, 5143–5152. [Google Scholar] [CrossRef]
- Chen, W.; Yan, X.; Tian, T.; Yan, R.; Wang, X.; Yu, Z.; Li, Y.; Zhang, L.; Han, S. Integrated analysis of a lncRNA-mRNA network reveals a potential mechanism underlying necrotizing enterocolitis. Mol. Med. Rep. 2020, 22, 423–435. [Google Scholar] [CrossRef] [PubMed]
- Hunter, C.J.; Upperman, J.S.; Ford, H.R.; Camerini, V. Understanding the susceptibility of the premature infant to necrotizing enterocolitis (NEC). Pediatr. Res. 2008, 63, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Frost, B.L.; Jilling, T.; Caplan, M.S. The importance of pro-inflammatory signaling in neonatal NEC. Semin. Perinatol. 2008, 32, 100–106. [Google Scholar] [CrossRef] [PubMed]
- De Plaen, I.G. Inflammatory signaling in Necrotizing enterocolitis. Clin. Perinatol. 2013, 40, 109–124. [Google Scholar] [CrossRef]
- Hunter, C.J.; De Plaen, I.G. Inflammatory signaling in NEC. Role of NFKB and cytokines. Pathophysiology 2014, 21, 55–65. [Google Scholar] [CrossRef]
- Nino, D.F.; Sodhi, C.P.; Hackam, D.J. Necrotizing enterocolitis: New insights into pathogenesis and mechanisms. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 590–600. [Google Scholar] [CrossRef]
- Mohankumar, K.; Namachivayam, K.; Ho, T.T.; Torres, B.A.; Ohls, R.K.; Maheshwari, A. Cytokines and growth factors in the developing intestine and during necrotizing enterocolitis. Semin. Perinatol. 2017, 41, 52–60. [Google Scholar] [CrossRef]
- Niemarkt, H.J.; De Meij, T.G.; van Ganzewinkel, C.-J.; de Boer, N.K.H.; Andriessen, P.; Hütten, M.C.; Kramer, B.W. Necrotizing enterocolitis, gut microbiota, and brain development: Role of the brain-gut axis. Neonatology 2019, 115, 423–431. [Google Scholar] [CrossRef]
- Nanthakumar, N.; Meng, D.; Goldstein, A.M.; Zhu, W.; Lu, L.; Uauy, R.; Llanos, A.; Claud, E.C.; and Walker, W.A. The mechanism of excessive intestinal inflammation in necrotizing enterocolitis: An immature innate immune response. PLoS ONE 2011, 6, e17776. [Google Scholar] [CrossRef]
- Cho, S.X.; Rudloff, I.; Lao, J.C.; Pang, M.A.; Goldberg, R.; Bui, C.B.; McLean, C.A.; Stock, M.; Klassert, T.E.; Slevogt, H.; et al. Characterization of the pathoimmunology of necrotizing enterocolitis reveals novel therapeutic opportunities. Nat. Commun. 2020, 11, 5794. [Google Scholar] [CrossRef]
- Tremblay, E.; Ferretti, E.; Babakissa, C.; Burghardt, K.M.; Levy, E.; Beaulieu, J.-F. IL-17-related signature genes linked to human necrotizing enterocolitis. BMC Res. Notes 2021, 14, 82. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Sheng, L. Significance of dynamic evolution of TNF-α, IL-6 and intestinal fatty acid-binding protein levels in neonatal necrotizing enterocolitis. Exp. Ther. Med. 2018, 15, 1289–1292. [Google Scholar] [CrossRef] [PubMed]
- Lin, J. Too much short chain fatty acids cause neonatal necrotizing enterocolitis. Med. Hypotheses 2004, 62, 291–293. [Google Scholar] [CrossRef] [PubMed]
- Waligora-Dupriet, A.-J.; Dugay, A.; Auzeil, N.; Huerre, M.; Butel, M.J. Evidence for clostridial implication in necrotizing enterocolitis through bacterial fermentation in a gnotobiotic quail model. Pediatr. Res. 2005, 58, 629–635. [Google Scholar] [CrossRef]
- Waligora-Dupriet, A.J.; Dugay, A.; Auzeil, N.; Nicolis, I.; Rabot, S.; Huerre, M.R.; Butel, M.J. Short-chain fatty acids and polyamines in the pathogenesis of necrotizing enterocolitis: Kinetics aspects in gnotobiotic quails. Anaerobe 2009, 15, 138–144. [Google Scholar] [CrossRef]
- Rajili’c-Stojanovi´c, M.; de Vos, W.M. The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol. Rev. 2014, 38, 996–1047. [Google Scholar] [CrossRef]
- Wong, C.B.; Odamaki, T.; Xiao, J. Insights into the reason of Human-Residential Bifidobacteria (HRB) being the natural inhabitants of the human gut and their potential health-promoting benefits. FEMS Microbiol. Rev. 2020, 44, 369–385. [Google Scholar] [CrossRef]
- Kozak, K.; Charbonneau, D.; Sanozky-Dawes, R.; Klaenhammer, T. Characterization of bacterial isolates from the microbiota of mothers breast milk and their infants. Gut Microbes 2015, 6, 341–351. [Google Scholar] [CrossRef]
- Solis, G.; Delosreyes-Gavilan, C.G.; Fernandez, N.; Margolles, A.; Gueimonde, M. Establishment and development of lactic acid bacteria and bifidobacteria microbiota in breast-milk and the infant gut. Anaerobe 2010, 16, 307–310. [Google Scholar] [CrossRef]
- Kitaoka, M. Bifidobacterial enzymes involved in the metabolism of human milk oligosaccharides. Adv. Nutr. 2012, 3, 422S–429S. [Google Scholar] [CrossRef]
- Pokusaeva, K.; Fitzgerald, G.F.; Van Sinderen, D. Carbohydrate metabolism in Bifidobacteria. Genes Nutr. 2011, 6, 285–306. [Google Scholar] [CrossRef] [PubMed]
- OCaliaghan, A.; Van Sinderen, D. Bifidobacteria and their role as members of the human gut microbiota. Front. Microbiol. 2016, 7, 925. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Moyano, S.; Totten, S.M.; Garrido, D.A.; Smilowitz, J.T.; German, J.B.; Lebrilia, C.B.; Mills, D.A. Variation in consumption of human milk oligosaccharides by infant gut-associated srains of bifidobacterium breve. Appl. Envion. Microbiol. 2013, 79, 6040–6049. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, A.; Katoh, T.; Sakanaka, M.; Ling, Y.; Yamada, C.; Asakuma, S.; Urashima, T.; Tomabechi, Y.; Katayama-Ikegami, A.; Kurihara, S.; et al. Sharing of human milk oligosaccharides degrades within bifodobacterial communities in faecal cultures supplemented with bifidobacterium. Sci. Rep. 2018, 8, 13958. [Google Scholar] [CrossRef] [PubMed]
- Zuniga, M.; Monedero, V.; Yebra, M.J. Utilization of host-derived glycans by intestinal lactobacillus and bifidobacterium species. Front. Microbiol. 2018, 9, 1917. [Google Scholar] [CrossRef]
- Barile, D.; Rastall, R.A. Human milk and related oligosaccharides as prebiotics. Curr. Opin. Biotechnol. 2013, 19, 9–16. [Google Scholar] [CrossRef]
- Arboleya, S.; Salazar, N.; Solís, G.; Fernández, N.; Hernández-Barranco, A.M.; Cuesta, I.; Gueimonde, M.; de los Reyes-Gavilán, C.G. Assessment of intestinal microbiota modulation ability of Bifidobacterium strains in in vitro fecal batch cultures from preterm neonates. Anaerobe 2013, 19, 9–16. [Google Scholar] [CrossRef]
- Gopalsamy, G.; Mortimer, E.; Greenfield, P.; Bird, A.R.; Young, G.P.; Christophersen, C.T. Resistant starch is actively fermented by infant faecal microbiota and increases microbial diversity. Nutrients 2019, 11, 1345. [Google Scholar] [CrossRef]
- Bergström, A.; Skov, T.H.; Bahl, M.I.; Roager, H.M.; Christensen, L.B.; Ejlerskov, K.T.; Mølgaard, C.; Michaelsen, K.F.; Licht, T.R. Establishment of intestinal microbiota during early life: A longitudinal, explorative study of a large cohort of Danish infants. Appl. Environ. Microbiol. 2014, 80, 2889–2900. [Google Scholar] [CrossRef]
- Moles, L.; Gómez, M.; Heilig, H.; Bustos, G.; Fuentes, S.; de Vos, W.; Fernández, L.; Rodríguez, J.M.; Jiménez, E. Bacterial diversity in meconium of preterm neonates and evolution of their fecal microbiota during the first month of life. PLoS ONE 2013, 8, e66986. [Google Scholar] [CrossRef]
- Morais, J.; Marques, C.; Teixeira, D.; Durão, C.; Faria, A.; Brito, S.; Cardoso, M.; Macedo, I.; Pereira, E.; Tomé, T.; et al. Extremely preterm neonates have more Lactobacillus in meconium than very preterm neonates—The in utero microbial colonization hypothesis. Gut Microbes 2020, 12, 1785804. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, E.; Fernandez, L.; Maldondado, A.; Martin, R.; Olivares, M.; Xaus, J.; Rodriguez, J.M. Oral administration of lactobacillus strains isolated from breast milk as an alternative for the treatment of infectious mastitis during lactation. Appl. Environ. Microbiol. 2008, 74, 4650–4655. [Google Scholar] [CrossRef] [PubMed]
- Soto, A.; Martin, V.; Jimenez, E.; Mader, I.; Rodtiguez, J.M.; Fernandez, L. Lacobacilli and bifidobacteria in human breast milk: Influence of antibiotherapy and other host clinical factors. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Kirtzalidou, E.; Pramateftaki, P.; Kotsou, M.; Kyriacou, A. Screening for lactobacilli with probiotic properties in the infant gut microbiota. Anaerobe 2011, 17, 440–443. [Google Scholar] [CrossRef]
- Ahrne, S.; Lonnermark, E.; Wold, A.E.; Aberg, N.; Hesselmar, B.; Saalman, R.; Strannegard, I.; Molin, G.; Adlerberth, I. Lcatobacilli in the intestinal microbiota of Swedish infants. Microbes Infect. 2005, 7, 1256–1262. [Google Scholar] [CrossRef] [PubMed]
- Vitetta, L.; Coulson, S.; Thomsen, M.; Nguyen, T.; Hall, S. Probiotics D-lactic acidosis, oxidative stress and strain specificity. Gut Microbes 2017, 8, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Pessione, E. Lactic acid bacteria contribution to gut microbiota complexity: Lights and shadows. Front. Cell. Infect. Microbiol. 2012, 2, 86. [Google Scholar] [CrossRef]
- Markowiak-kopec, P.; Slizewska, K. The effect of probiotics on the production of short-chain fatty acids by human intestinal microbiome. Nutrients 2020, 12, 1107. [Google Scholar] [CrossRef]
- Wandro, S.; Osborne, S.; Enriquez, C.; Bixby, C.; Arrieta, A.; Whiteson, K. The microbiome and metabolome of preterm infant stool are personalized and not driven by health outcomes, including necrotizing enterocolitis and late-onset sepsis. mSphere 2018, 3, e00104-18. [Google Scholar] [CrossRef]
- Jia, Q.; Yu, X.; Chang, Y.; You, Y.; Chen, Z.; Wang, Y.; Liu, B.; Chen, L.; Ma, D.; Xing, Y.; et al. Dynamic changes of the gut microbiota in preterm infants with different gestational age. Front. Microbiol. 2022, 13, 923273. [Google Scholar] [CrossRef]
- Singh, R.K.; Chang, H.; Yan, D.; Lee, K.M.; Ucmak, D.; Wong, K.; Abrouk, M.; Farahnik, B.; Nakamura, M.; Zhu, T.H.; et al. Influence of diet on the gut microbiome and implications for human health. J. Transl. Med. 2017, 15, 73. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Chen, C.; Newburg, D.S. Utilization of major fucosylated and sialylated human milk oligosaccharides isolated human gut microbes. Glycobiology 2013, 23, 1281–1292. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.K.; Kumar, S.S.; Ghosh, A.R. Probiotics enterococcus faecalis effectively assimilates cholesterol and produces fatty acids including propionate. FEMS Microbiol. Lett. 2019, 366, FNZ039. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Zhi, X.; Li, H.; Klenk, H.; Li, W. Comparative genomics of the bacterial genus Streptococcus illuminates evolutionary implications of species groups. PLoS ONE 2014, 9, e101229. [Google Scholar] [CrossRef] [PubMed]
- Koh, A.; De Vadder, F.; Kovatcheva-datchary, P.; Backhed, F. From dietary fiber to host physiology: Short-chain fatty acids as key bacterial metabolites. Cell 2016, 165, 1332–1345. [Google Scholar] [CrossRef]
- Gregory, K.E.; LaPlante, R.D.; Shan, G.; Kumar, D.V.; Gregas, M. Mode of birth influences preterm infant intestinal colonization with bacteroides over the early neonatal period. Adv. Neonatal Care 2015, 15, 386–393. [Google Scholar] [CrossRef]
- Brooks, B.; Firek, B.A.; Miller, C.S.; Sharon, I.; Thomas, B.C.; Baker, R.; Morowitz, M.J.; Banfield, J.F. Microbes in the neonatal intensive care unit resemble those found in the gut of premature infants. Microbiome 2014, 2, 1. [Google Scholar] [CrossRef]
- Yap, P.S.X.; Chong, C.W.; Kamar, A.A.; Yap, I.K.S.; Choo, Y.M.; Lai, N.M.; Teh, C.S.J. Neonatal intensive care unit (NICU) exposures exert a sustained influence on the progression of gut microbiota and metabolome in the first year of life. Sci. Rep. 2021, 11, 1353. [Google Scholar] [CrossRef]
- Lawley, B.; Otal, A.; Moloney-Geany, K.; Diana, A.; Houghton, L.; Hearth, A.M.; Taylor, R.W.; Tannock, G.W. Fecal microbiotas of Indonesian and New Zealand children differ in complexity and bifidobacteria taxa during the first year of life. Appl. Environ. Microbiol. 2019, 85, e01105-19. [Google Scholar] [CrossRef]
- Wang, M.; Li, M.; Wu, S.; Lebrilia, C.B.; Chapkin, R.S.; Ivanov, I.; Donovan, S.M. Fecal microbiota composition breast-fed infants is correlated with human milk oligosaccharides consumed. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 825–833. [Google Scholar] [CrossRef]
- Tannock, G.W.; Lawley, B.; Munro, K.; Pathmanathan, S.G.; Zhou, S.J.; Makrides, M.; Gibson, R.A.; Sullivan, T.; Prosser, C.G.; Lowery, D. Comparison of the compositions of the stool microbiotas of infants fed goat milk formula, cow milk-based formula, or breast milk. Appl. Environ. Microbiol. 2013, 79, 3040–3048. [Google Scholar] [CrossRef]
- Talford, L.E.; Crost, E.H.; Kavanaugh, D.; Juge, N. Mucin glycan foraging in the human gut microbiome. Front. Genet. 2005, 6, 81. [Google Scholar] [CrossRef] [PubMed]
- Marcobal, A.; Barboza, M.; Froehlich, J.W. Consumption of human milk oligosaccharides by gut-related microbes. J. Agric. Food Chem. 2010, 58, 5334–5340. [Google Scholar] [CrossRef] [PubMed]
- Marcobal, A.; Barboza, M.; Sonnenburg, E.D.; Pudlo, N.; Martens, E.C.; Desal, P.; Lebrilia, C.B.; Weimer, B.C.; Mills, D.A.; German, J.B.; et al. Bacteroides in the infant gut consume milk oligosaccharidsvia mucus-utilization pathways. Cell Host Microbe 2011, 10, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Marcobal, A.; Sonnenburg, J.L. Human milk oligosaccharide consumption by intestinal microbiota. Clin. Microbiol. Infect. 2012, 18, 12–15. [Google Scholar] [CrossRef]
- Feichardt, N.; Duncan, S.H.; Young, P.; Belenguer, A.; Mcwilliam, L.C.; Scott, K.P.; Louis, P. Phylogenetic distribution of three pathways for propionate production within the human gut microbiota. ISME J. 2014, 8, 1323–1335. [Google Scholar] [CrossRef]
- Rios-Covian, D.; Salazar, N.; Gueimonde, M.G.; De Los Reyes-Gavilan, C. Shaping the metabolism of intestinal bacteriods population through diet to improve human health. Front. Microbiol. 2017, 8, 376. [Google Scholar] [CrossRef]
- Oliphant, K.; Allen-Vercoe, E. Macronutrient metabolism by the human gut microbioame major fermentation by-products and their impact on host health. Microbiome 2018, 7, 91. [Google Scholar] [CrossRef]
- Pourcyrous, M.; Nolan, V.G.; Goodwin, A.; Davis, S.L.; Buddington, R.K. Fecal short-chain fatty acids of very-low-birth-weight preterm infants fed expressed breast milk or formula. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 725–731. [Google Scholar] [CrossRef]
- Chen, C.; Yin, Q.; Wu, H.; Cheng, L.; Kwon, J.-I.; Jin, J.; Han, T.; Che, H. Different effects of premature infant formula and breast milk on intestinal microecological development in premature infants. Front. Microbiol. 2019, 10, 3020. [Google Scholar] [CrossRef]
- Alcon-Giner, C.; Dalby, M.J.; Caim, S.; Ketskemety, J.; Shaw, A.; Sim, K.; Lawson, M.A.E.; Kiu, R.; Leclaire, C.; Chalklen, L.; et al. Microbiota supplementation with Bifidobacterium and Lactobacillus modifies the preterm infant gut microbiota and metabolome: An observational study. Cell Rep. Med. 2020, 1, 100077. [Google Scholar] [CrossRef] [PubMed]
- Beck, L.C.; Masi, A.C.; Young, G.R.; Vatanen, T.; Lamb, C.A.; Smith, R.; Coxhead, J.; Butler, A.; Marsland, B.J.; Embleton, N.D.; et al. Strain-specific impacts of probiotics are a significant driver of gut microbiome development in very preterm infants. Nat. Microbiol. 2022, 7, 1525–1535. [Google Scholar] [CrossRef] [PubMed]
- Westaway, J.A.F.; Huerlimann, R.; Kandasamy, Y.; Miller, C.M.; Norton, R.; Staunton, K.M.; Watson, D.; Rudd, D. The bacterial gut microbiome of probiotic-treated very-preterm infants: Changes from admission to discharge. Pediatr. Res. 2022, 92, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Chi, C.; Fan, Y.; Li, C.; Li, Y.; Guo, S.; Li, T.; Buys, N.; Clifton, V.L.; Colditz, P.B.; Yin, C.; et al. Early gut microbiota colonisation of premature infants fed with breastmilk or formula with or without probiotics: A cohort study. Nutrients 2021, 13, 4068. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Holdbrooks, H.; Mishra, P.; Abrantes, M.A.; Eskew, S.; Garma, M.; Oca, C.-G.; McGuckin, C.; Hein, C.B.; Mitchell, R.D.; et al. Impact of probiotic B. infantis EVC001 feeding in premature infants on the gut microbiome, nosocomially acquired antibiotic resistance, and enteric inflammation. Front. Pediatr. 2021, 9, 618009. [Google Scholar] [CrossRef] [PubMed]
- Arboleya, S.; Saturio, S.; Suárez, M.; Fernández, N.; Mancabelli, L.; de Los Reyes-Gavilán, C.G.; Ventura, M.; Solís, G.; Gueimonde, M. Donated human milk as a determinant factor for the gut bifidobacterial ecology in premature babies. Microorganisms 2020, 8, 760. [Google Scholar] [CrossRef] [PubMed]
- Morais, J.; Marques, C.; Faria, A.; Teixeira, D.; Barreiros-Mota, I.; Durão, C.; Araújo, J.; Ismael, S.; Brito, S.; Cardoso, M.; et al. Influence of human milk on very preterms’ gut microbiota and alkaline phosphatase activity. Nutrients 2021, 13, 1564. [Google Scholar] [CrossRef]
- Cong, X.; Xu, W.; Janton, S.; Henderson, W.A.; Matson, A.; McGrath, J.M.; Maas, K.; Graf, J. Gut microbiome developmental patterns in early life of preterm infants: Impacts of feeding and gender. PLoS ONE 2016, 11, e0152751. [Google Scholar] [CrossRef]
- Horigome, A.; Hisata, K.; Odamaki, T.; Iwabuchi, N.; Xiao, J.-Z.; Shimizu, T. Colonization of supplemented bifidobacterium breve M-16V in low birth weight infants and its effects on their gut microbiota weeks post-administration. Front. Microbiol. 2021, 12, 610080. [Google Scholar] [CrossRef]
- Ishizeki, S.; Sugita, M.; Takata, M.; Yaeshima, T. Effect of administration of bifidobacteria on intestinal microbiota in low-birth-weight infants and transition of administrated bifidobacteria. A comparison between one-species and three-species administration. Anaerobe 2013, 23, 38–44. [Google Scholar] [CrossRef]
- Esaiassen, E.; Hjerde, E.; Cavanagh, J.P.; Pedersen, T.; Andresen, J.H.; Rettedal, S.I.; Støen, R.; Nakstad, B.; Willassen, N.P.; Klingenberg, C. Effects of probiotic supplementation on the gut microbiota and antibiotic resistance development in preterm infants. Front. Pediatr. 2018, 6, 347. [Google Scholar] [CrossRef] [PubMed]
- Kurath-Koller, S.; Neumann, C.; Moissl-Eichinger, C.; Kraschl, R.; Kanduth, C.; Hopfer, B.; Pausan, M.-R.; Urlesberger, B.; Resch, B. Hospital regimens including probiotics guide the individual development of the gut microbiome of very low birth weight infants in the first two weeks of life. Nutrients 2020, 12, 1256. [Google Scholar] [CrossRef] [PubMed]
- Yousuf, E.I.; Carvalho, M.; Dizzell, S.E.; Kim, S.; Gunn, E.; Twiss, J.; Giglia, L.; Stuart, C.; Hutton, E.K. Persistence of suspected probiotic organisms in preterm infant gut microbiota weeks after probiotic supplementation in the NICU. Front. Microbiol. 2020, 11, 574137. [Google Scholar] [CrossRef] [PubMed]
- Abdulkadir, B.; Nelson, A.; Skeath, T.; Marrs, E.C.L.; Perry, J.D.; Cummings, S.P.; Embleton, N.D.; Berrington, J.E.; Stewart, C.J. Routine use of probiotics in preterm infants: Longitudinal impact on the microbiome and metabolome. Neonatology 2016, 109, 239–247. [Google Scholar] [CrossRef]
- Larke, J.A.; Kuhn-Riordon, K.; Taft, D.H.; Sohn, K.; Iqbal, S.; Underwood, M.A.; Mills, D.A.; Slupsky, C.M. Preterm infant fecal microbiota and metabolite profiles are modulated in a probiotic specific manner. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 535–542. [Google Scholar] [CrossRef]
- Hui, Y.; Smith, B.; Mortensen, M.S.; Krych, L.; Sørensen, S.J.; Greisen, G.; Krogfelt, K.A.; Nielsen, D.S. The effect of early probiotic exposure on the preterm infant gut microbiome development. Gut Microbes 2021, 13, 1951113. [Google Scholar] [CrossRef]
- Chang, C.-M.; Tsai, M.-H.; Liao, W.-C.; Yang, P.-H.; Li, S.-W.; Chu, S.-M.; Huang, H.-R.; Chiang, M.-C.; Hsu, J.-F. Effects of probiotics on gut microbiomes of extremely preterm infants in the neonatal intensive care unit: A prospective cohort study. Nutrients 2022, 14, 3239. [Google Scholar] [CrossRef]
- Underwood, M.A.; Salzman, N.H.; Bennett, S.H.; Barman, M.; Mills, D.A.; Marcobal, A.; Tancredi, D.J.; Bevins, C.L.; Sherman, M.O. A randomized placebo-controlled comparison of 2 prebiotic/probiotic combinations in preterm infants: Impact on weight gain, intestinal microbiota, and fecal short-chain fatty acids. J. Pediatr. Gastroenterol. Nutr. 2009, 48, 216–225. [Google Scholar] [CrossRef]
- Athalye-Jape, G.; Esvaran, M.; Patole, S.; Simmer, K.; Nathan, E.; Doherty, D.; Keil, A.; Rao, S.; Chen, L.; Chandrasekaran, L.; et al. Effect of single versus multistrain probiotic in extremely preterm infants: A randomised trial. BMJ Open Gastroenterol. 2022, 9, e000811. [Google Scholar] [CrossRef]
- Oshiro, T.; Nagata, S.; Wang, C.; Takahashi, T.; Tsuji, H.; Asahara, T.; Nomoto, K.; Takei, H.; Nittono, H.; Yamashiro, Y. Bifidobacterium supplementation of colostrum and breast milk enhances weight gain and metabolic responses associated with microbiota establishment in very-preterm infants. Biomed. Hub 2019, 4, 1–10. [Google Scholar] [CrossRef]
- Boehm, G.; Lidestri, M.; Casetta, P.; Jelinek, J.; Negretti, F.; Stahl, B.; Marini, A. Supplementation of a bovine milk formula with an oligosaccharide mixture increases counts of faecal bifidobacteria in preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 2002, 86, F178–F181. [Google Scholar] [CrossRef] [PubMed]
- Plummer, E.L.; Bulach, D.M.; Murray, G.L.; Jacobs, S.E.; Tabrizi, S.N.; Garland, S.M.; ProPrems Study Group. Gut microbiota of preterm infants supplemented with probiotics: Sub-study of the ProPrems trial. BMC Microbiol. 2018, 18, 184. [Google Scholar] [CrossRef] [PubMed]
- Mohan, R.; Koebnick, C.; Schildt, J.; Schmidt, S.; Mueller, M.; Possner, M.; Radke, M.; Blaut, M. Effects of Bifidobacterium lactis Bb12 supplementation on intestinal microbiota of preterm infants: A double-blind, placebo-controlled, randomized study. J. Clin. Microbiol. 2006, 44, 4025–4031. [Google Scholar] [CrossRef]
- Martí, M.; Spreckels, J.E.; Ranasinghe, P.D.; Wejryd, I.; Marchini, G.; Sverremark-Ekström, E.; Jenmalm, M.C.; Abrahamsson, T. Effects of Lactobacillus reuteri supplementation on the gut microbiota in extremely preterm infants in a randomized placebo-controlled trial. Cell Rep. Med. 2021, 2, 100206. [Google Scholar] [CrossRef] [PubMed]
- Plummer, E.L.; Danielewski, J.A.; Garland, S.M.; Su, J.; Jacobs, S.E.; Murray, J.L. The effect of probiotic supplementation on the gut microbiota of preterm infants. J. Med. Microbiol. 2021, 70, 001403. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Davis, B.; Zhu, W.; Zheng, N.; Meng, D.; Walker, W.A. Short-chain fatty acid butyrate, a breast milk metabolite, enhances immature intestinal barrier function genes in response to inflammation in vitro and in vivo. Am. J. Physiol. Gastrointest. Liver Physiol. 2021, 320, G521–G530. [Google Scholar] [CrossRef]
- Huang, S.; Gao, Y.; Wang, Z.; Yang, X.; Wang, J.; Zheng, N. Anti-inflammatory actions of acetate, propionate, and butyrate in fetal mouse jejunum cultures ex vivo and immature small intestinal cells in vitro. Food Sci. Nutr. 2022, 10, 564–576. [Google Scholar] [CrossRef] [PubMed]
- Nastasi, C.; Candela, M.; Bonefeld, C.M.; Geisler, C.; Hansen, M.; Krejsgaard, T.; Biagi, E.; Andersen, M.H.; Brigidi, P.; Ødum, N.; et al. The effect of short-chain fatty acids on human monocyte-derived dendritic cells. Sci. Rep. 2015, 5, 16148. [Google Scholar] [CrossRef]
- Moylan, H.E.C.; Nguyen-Ngo, C.; Lim, R.; Lappas, M. The short-chain fatty acids butyrate and propionate protect against inflammation-induced activation of mediators involved in active labor: Implications for preterm birth. Mol. Hum. Reprod. 2020, 26, 452–468. [Google Scholar] [CrossRef]
- Ganguli, K.; Collado, M.C.; Rautava, J.; Lu, L.; Satokari, R.; Von Ossowski, I.; Reunaene, J.; De vos, W.M.; Palva, A.; Isolauri, E.; et al. Lactobacillius rhamnosus GG and its spac pilus adhesion modulate inflammatory responsiveness and TLR-related gene expression in the fetal human gut. Pediatr. Res. 2015, 77, 528–535. [Google Scholar] [CrossRef]
- Ganguli, K.; Meng, D.; Rautava, S.; Lu, L.; Walker, W.A.; Nanthakumar, N. Probiotics prevent necrotizing enterocolitis by modulating enterocyte genes that regulate innate immune-mediated inflammation. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 304, G132–G141. [Google Scholar] [CrossRef] [PubMed]
- Meng, D.; Zhu, W.; Ganguli, K.; Shi, H.N.; Walker, W.A. Anti-inflammatory effects of Bifidobacterium longum subsp infantis secretions on fetal human enterocytes are mediated by TLR-4 receptors. Am. J. Physiol. Gastrointest. Liver Physiol. 2016, 311, G744–G753. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Cho, K.Y.; Meng, D.; Walker, W.A. The impact of indole-3-lactic acid on immature intestinal innate immunity and development: A transcriptomic analysis. Sci. Rep. 2021, 11, 8088. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Guo, Y.; Ergun, A.; Lu, L.; Walker, W.A.; Ganguli, K. Secreted metabolites of Bifidobacterium infantis and Lactobacillus acidophilus protect immature human enterocytes from IL-1β-induced inflammation: A transcription profiling analysis. PLoS ONE 2015, 10, e0124549. [Google Scholar] [CrossRef]
- Jiang, F.; Memg, D.; Weng, M.; Zhu, W.; Wu, W.; Kasper, D.; Walker, W.A. The symbiotic bacterial surface factor polysaccharide A on bacteroides fragilis inhibits IL-B-induced inflammation in human fetal enterocytes via toll receptors 2 and 4. PLoS ONE 2017, 12, E0172738. [Google Scholar] [CrossRef]
- Gorreja, F.; Rush, S.T.A.; Kasper, D.L.; Meng, D.; Walker, W.A. The developmentally regulated fetal enterocyte gene, ZP4, mediates anti-inflammation by the symbiotic bacterial surface factor polysaccharide A on Bacteroides fragilis. Am. J. Physiol. Gastrointest. Liver Physiol. 2019, 317, G398–G407. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).