Adequacy of Anaesthesia for Nociception Detection during Vitreoretinal Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
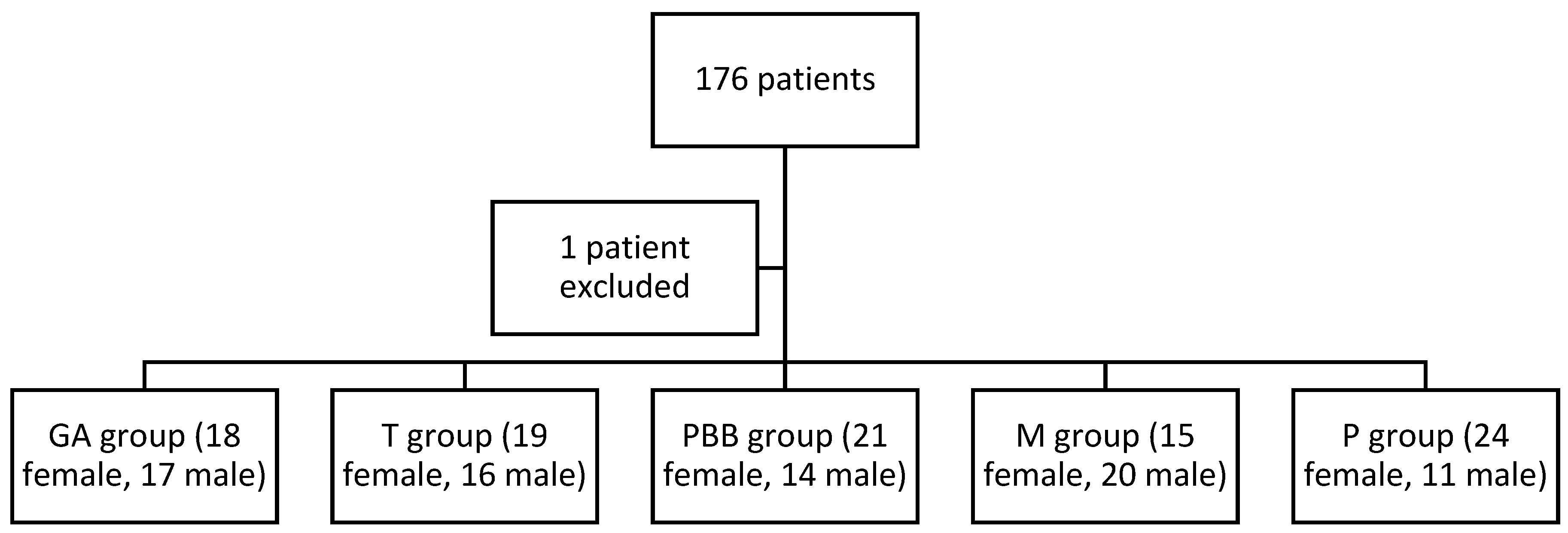
2.2. Subjects
2.3. Procedures
2.4. Statistical Analysis
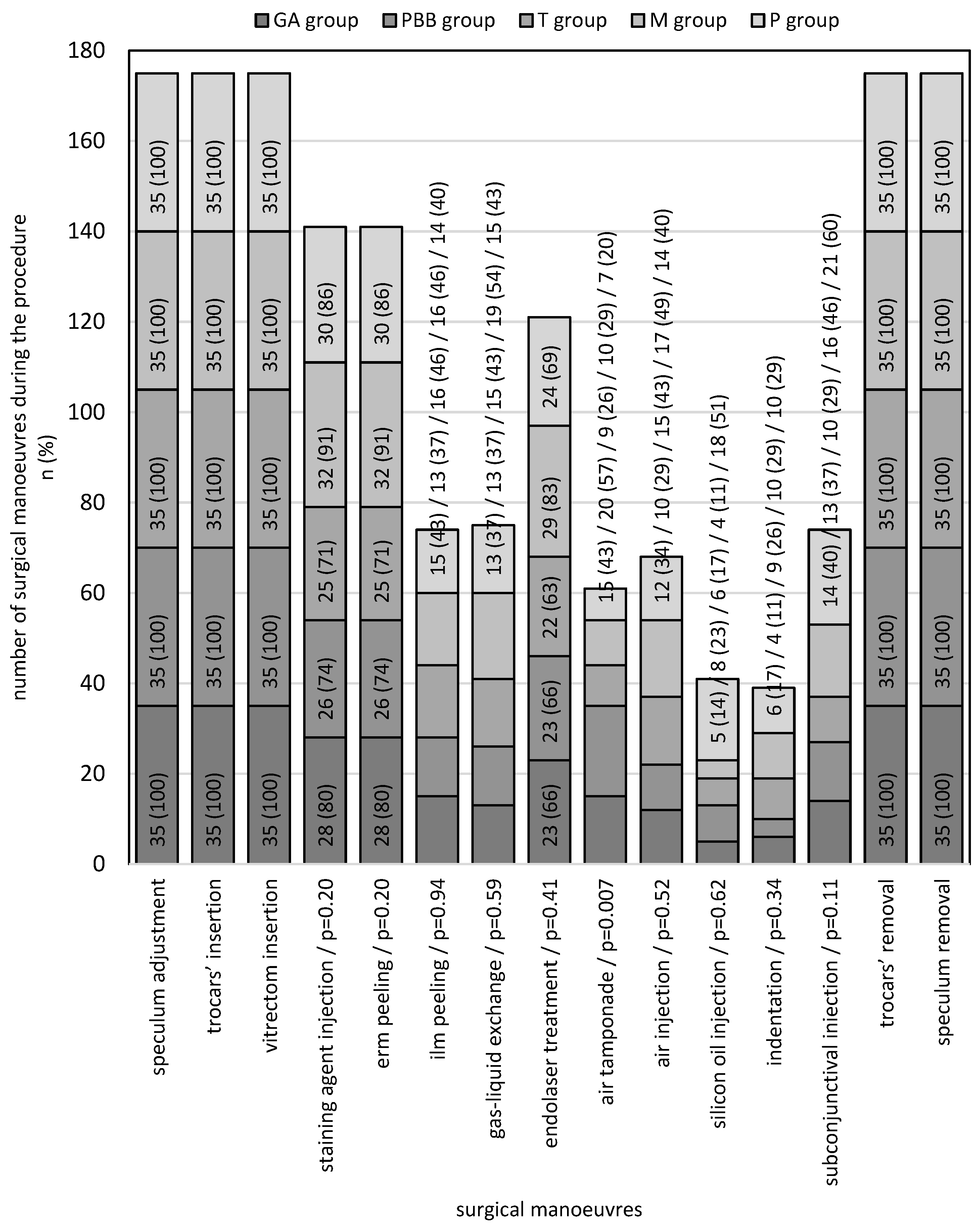
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lavand’homme, P.; Estebe, J.-P. Opioid-Free Anesthesia: A Different Regard to Anesthesia Practice. Curr. Opin. Anaesthesiol. 2018, 31, 556–561. [Google Scholar] [CrossRef]
- Lavand’homme, P.; Steyaert, A. Opioid-Free Anesthesia Opioid Side Effects: Tolerance and Hyperalgesia. Best Pract. Res. Clin. Anaesthesiol. 2017, 31, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Misiołek, H.; Cettler, M.; Woroń, J.; Wordliczek, J.; Dobrogowski, J.; Mayzner-Zawadzka, E. The 2014 Guidelines for Post-Operative Pain Management. Anaesthesiol. Intensive Ther. 2014, 46, 221–244. [Google Scholar] [CrossRef]
- Misiolek, H.; Zajączkowska, R.; Daszkiewicz, A.; Woroń, J.; Dobrogowski, J.; Wordliczek, J.; Owczuk, R. Postoperative Pain Management—2018 Consensus Statement of the Section of Regional Anaesthesia and Pain Therapy of the Polish Society of Anaesthesiology and Intensive Therapy, the Polish Society of Regional Anaesthesia and Pain Therapy, the Polish Association for the Study of Pain and the National Consultant in Anaesthesiology and Intensive Therapy. Anaesthesiol. Intensive Ther. 2018, 50, 173–199. [Google Scholar] [CrossRef] [PubMed]
- Gruenewald, M.; Ilies, C. Monitoring the Nociception–Anti-Nociception Balance. Best Pract. Res. Clin. Anaesthesiol. 2013, 27, 235–247. [Google Scholar] [CrossRef]
- Ilies, C.; Ludwigs, J.; Gruenewald, M.; Thee, C.; Hanf, J.; Hanss, R.; Steinfath, M.; Bein, B. The Effect of Posture and Anaesthetic Technique on the Surgical Pleth Index. Anaesthesia 2012, 67, 508–513. [Google Scholar] [CrossRef]
- Van Gils, M.; Korhonen, I.; Yli-Hankala, A. Procedures for Evaluating the Adequacy of Anesthesia. CRB 2017, 45, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Stasiowski, M.J.; Pluta, A.; Lyssek-Boroń, A.; Kawka, M.; Krawczyk, L.; Niewiadomska, E.; Dobrowolski, D.; Rejdak, R.; Król, S.; Żak, J.; et al. Preventive Analgesia, Hemodynamic Stability, and Pain in Vitreoretinal Surgery. Medicina 2021, 57, 262. [Google Scholar] [CrossRef] [PubMed]
- Stasiowski, M.J.; Pluta, A.; Lyssek-Boroń, A.; Król, S.; Krawczyk, L.; Niewiadomska, E.; Żak, J.; Kawka, M.; Dobrowolski, D.; Grabarek, B.O.; et al. Adverse Events during Vitreoretinal Surgery under Adequacy of Anesthesia Guidance-Risk Factor Analysis. Pharmaceuticals 2022, 15, 237. [Google Scholar] [CrossRef] [PubMed]
- Pluta, A.; Stasiowski, M.J.; Lyssek-Boroń, A.; Król, S.; Krawczyk, L.; Niewiadomska, E.; Żak, J.; Kawka, M.; Dobrowolski, D.; Grabarek, B.O.; et al. Adverse Events during Vitrectomy under Adequacy of Anesthesia—An Additional Report. J. Clin. Med. 2021, 10, 4172. [Google Scholar] [CrossRef] [PubMed]
- Jung, K.; Park, M.H.; Kim, D.K.; Kim, B.J. Prediction of Postoperative Pain and Opioid Consumption Using Intraoperative Surgical Pleth Index after Surgical Incision: An Observational Study. J. Pain. Res. 2020, 13, 2815–2824. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R.; Wall, P.D. Pain Mechanisms: A New Theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef]
- Tomaszek, L.; Fenikowski, D.; Maciejewski, P.; Komotajtys, H.; Gawron, D. Perioperative gabapentin in pediatric thoracic surgery patients—Randomized, placebo-controlled, phase 4 trial. Pain Med. 2020, 21, 1562–1571. [Google Scholar] [CrossRef] [PubMed]
- Bharti, N.; Chari, P.; Kumar, P. Effect of Sevoflurane versus Propofol-Based Anesthesia on the Hemodynamic Response and Recovery Characteristics in Patients Undergoing Microlaryngeal Surgery. Saudi J. Anaesth. 2012, 6, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Struys, M.M.R.F.; Vanpeteghem, C.; Huiku, M.; Uutela, K.; Blyaert, N.B.K.; Mortier, E.P. Changes in a Surgical Stress Index in Response to Standardized Pain Stimuli during Propofol-Remifentanil Infusion. Br. J. Anaesth. 2007, 99, 359–367. [Google Scholar] [CrossRef]
- Bergmann, I.; Göhner, A.; Crozier, T.A.; Hesjedal, B.; Wiese, C.H.; Popov, A.F.; Bauer, M.; Hinz, J.M. Surgical Pleth Index-Guided Remifentanil Administration Reduces Remifentanil and Propofol Consumption and Shortens Recovery Times in Outpatient Anaesthesia. Br. J. Anaesth. 2013, 110, 622–628. [Google Scholar] [CrossRef]
- Gruenewald, M.; Ilies, C.; Herz, J.; Schoenherr, T.; Fudickar, A.; Höcker, J.; Bein, B. Influence of Nociceptive Stimulation on Analgesia Nociception Index (ANI) during Propofol–Remifentanil Anaesthesia. Br. J. Anaesth. 2013, 110, 1024–1030. [Google Scholar] [CrossRef] [PubMed]
- Ahonen, J.; Jokela, R.; Uutela, K.; Huiku, M. Surgical Stress Index Reflects Surgical Stress in Gynaecological Laparoscopic Day-Case Surgery. Br. J. Anaesth. 2007, 98, 456–461. [Google Scholar] [CrossRef]
- Ledowski, T.; Pascoe, E.; Ang, B.; Schmarbeck, T.; Clarke, M.W.; Fuller, C.; Kapoor, V. Monitoring of Intra-Operative Nociception: Skin Conductance and Surgical Stress Index versus Stress Hormone Plasma Levels. Anaesthesia 2010, 65, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Licina, A.; Sidhu, S.; Xie, J.; Wan, C. Local versus General Anaesthesia for Adults Undergoing Pars Plana Vitrectomy Surgery. Cochrane Database Syst. Rev. 2016, 9, CD009936. [Google Scholar] [CrossRef] [PubMed]
- Ghali, A.M.; El Btarny, A.M. The Effect on Outcome of Peribulbar Anaesthesia in Conjunction with General Anesthesia for Vitreoretinal Surgery. Anaesthesia 2010, 65, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, D.; Sain, S.; Azad, S.; Arora, T.; Azad, R. Comparison of Topical Anesthesia and Peribulbar Anesthesia for 23-Gauge Vitrectomy without Sedation. Retina 2013, 33, 1400–1406. [Google Scholar] [CrossRef]
- Bahçecioglu, H.; Unal, M.; Artunay, O.; Rasier, R.; Sarici, A. Posterior Vitrectomy under Topical Anesthesia. Can. J. Ophthalmol. 2007, 42, 272–277. [Google Scholar] [CrossRef]
- Page, M.A.; Fraunfelder, F.W. Safety, Efficacy, and Patient Acceptability of Lidocaine Hydrochloride Ophthalmic Gel as a Topical Ocular Anesthetic for Use in Ophthalmic Procedures. OPTH 2009, 3, 601–609. [Google Scholar] [CrossRef]
- Chaudhary, R.A.; Khaqan, H.A.; Ahmad, A.; Imtiaz, U.; Raza, H.; Shabbir, U. Comparison of Topical Versus Peribulbar Anesthesia for 23G Pars Plana Vitrectomy. J. Coll. Physicians Surg. Pak. 2018, 28, 452–455. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Gu, G.; Fan, G.; Zhu, Y.; Yang, Y.; Gu, X.; Zhang, H.; He, S. The Effect of Preoperative Administration of Morphine in Alleviating Intraoperative Pain of Percutaneous Transforaminal Endoscopic Discectomy under Local Anesthesia. Medicine 2017, 96, e8427. [Google Scholar] [CrossRef]
- Double Masked Randomised Controlled Trial to Assess the Effectiveness of Paracetamol in Reducing Pain in Panretinal Photocoagulation|British Journal of Ophthalmology. Available online: https://bjo.bmj.com/content/90/6/713.long (accessed on 11 October 2022).
- Baldo, B.A.; Rose, M.A. Mechanisms of Opioid-Induced Respiratory Depression. Arch. Toxicol. 2022, 96, 2247–2260. [Google Scholar] [CrossRef]
- Mets, B.; James, M.F. Another Complication of Opiate-Induced Chest Wall Rigidity. S. Afr. Med. J. 1992, 81, 385–386. [Google Scholar] [PubMed]
- Stasiowski, M.J.; Starzewska, M.; Niewiadomska, E.; Król, S.; Marczak, K.; Żak, J.; Pluta, A.; Eszyk, J.; Grabarek, B.O.; Szumera, I.; et al. Adequacy of Anesthesia Guidance for Colonoscopy Procedures. Pharmaceuticals 2021, 14, 464. [Google Scholar] [CrossRef] [PubMed]
- Stasiowski, M.J.; Szumera, I.; Wardas, P.; Król, S.; Żak, J.; Missir, A.; Pluta, A.; Niewiadomska, E.; Krawczyk, L.; Jałowiecki, P.; et al. Adequacy of Anesthesia and Pupillometry for Endoscopic Sinus Surgery. J. Clin. Med. 2021, 10, 4683. [Google Scholar] [CrossRef]
- Stasiowski, M.; Missir, A.; Pluta, A.; Szumera, I.; Stasiak, M.; Szopa, W.; Błaszczyk, B.; Możdżyński, B.; Majchrzak, K.; Tymowski, M.; et al. Influence of infiltration anaesthesia on perioperative outcomes following lumbar discectomy under surgical pleth index-guided general anaesthesia: A preliminary report from a randomised controlled prospective trial. Adv. Med. Sci. 2020, 65, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.-L.; Tong, Y.; Wang, Y.-X.; Zhao, P.-Q.; Wang, Z.-Y. A Prospective, Randomised, Double-Masked Comparison of Local Anaesthetic Agents for Vitrectomy. Br. J. Ophthalmol. 2017, 101, 1016–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Anthropometric Data | Total n = 175 (100) | GA Group n = 35 (20) | PBB Group n = 35 (20) | T Group n = 35 (20) | M Group n = 35 (20) | P Group n = 35 (20) | p-Value |
|---|---|---|---|---|---|---|---|
| Age [years] | 64.5 ± 11.7 66 (13) | 65.1 ± 10.8 67 (9) | 66.8 ± 1.1 69 (13) | 62.7 ± 13.3 65 (14) | 61.9 ± 11.9 63 (14) | 66.1 ± 9.9 67 (8) | 0.25 a |
| Height [cm] | 165.8 ± 8.7 165 (12) | 166.9 ± 8.6 168 (14) | 165.9 ± 8.3 164 (12) | 164.7 ± 10.3 164 (18) | 168 ± 7.4 170 (14) | 163.4 ± 8.7 160 (12) | 0.18 a |
| Weight [kg] | 77.6 ± 15.9 75.5 (17) | 83.4 ± 19.8 82 (20) | 78.8 ± 16 75 (11) | 77.1 ± 13.7 80 (21) | 74.7 ± 14.9 74 (19) | 74.1 ± 13.3 74 (22) | 0.19 a |
| BMI [kg/m2] | 28.3 ± 5.4 27.5 (6.4) | 29.9 ± 6.6 28.4 (5.3) | 28.6 ± 5.1 27.1 (4.4) | 28.5 ± 4.9 28.4 (7.3) | 26.4 ± 4.6 25.3 (5.4) | 27.9 ± 5.3 27.6 (7.7) | 0.06 a |
| Male/ Female | 78 (44.6)/ 97 (55.4) | 17 (48.6)/ 14 (51.4) | 14 (40.0)/ 21 (60.0) | 16 (45.7)/ 19 (54.3) | 20 (57.1)/ 15 (42.9) | 11 (31.4) / 24 (68.6) | 0.26 b |
| Indications for Surgery | Total n = 175 (100) | GA Group n = 35 (100) | PBB Group n = 35 (100) | T Group n = 35 (100) | M Group n = 35 (100) | P group n = 35 (100) | p-Value |
|---|---|---|---|---|---|---|---|
| Vitreal haemorrhage | 36 (20.6) | 9 (25.7) | 5 (14.3) | 6 (17.1) | 10 (28.6) | 6 (17.1) | 0.53 a |
| Retinal detachment | 55 (31.4) | 7 (20.0) | 12 (34.3) | 12 (34.3) | 12 (34.3) | 12 (34.3) | 0.60 a |
| Macular hole | 25 (14.3) | 6 (17.1) | 4 (11.4) | 6 (17.1) | 3 (8.6) | 6 (17.1) | 0.77 a |
| Epiretinal membrane | 146 (83.4) | 33 (94.3) | 26 (74.3) | 26 (74.3) | 31 (88.6) | 30 (85.7) | 0.12 a |
| Macular oedema | 11 (6.3) | 2 (5.7) | 2 (5.7) | 3 (8.6) | 2 (5.7) | 2 (5.7) | 0.97 a |
| Ocular trauma | 3 (1.7) | 0 (0) | 1 (2.9) | 1 (2.9) | 1 (2.9) | 0 (0) | 0.80 a |
| Aphakia | 4 (2.3) | 0 (0) | 1 (2.9) | 0 (0) | 0 (0) | 3 (8.6) | 0.05 a |
| Pseudophakia | 11 (6.3) | 1 (2.9) | 6 (17.1) | 3 (8.6) | 1 (2.9) | 0 (0) | 0.03 a |
| Multiple indications | 99 (56.6) | 25 (71.4) | 18 (51.4) | 20 (57.1) | 13 (37.1) | 23 (65.7) | 0.46 a |
| Cumulative Dose of Rescue FNT in Patients with Intraoperative Pain Perception (∆SPI >15) | Total n = 175 (100) | GA Group n = 35 (20) | PBB Group n = 35 (20) | T Group n = 35 (20) | M Group n = 35 (20) | P Group n = 35 (20) | p-Value |
|---|---|---|---|---|---|---|---|
| FNT—STAGE 3 | |||||||
| Speculum installation | 25.6 ± 27.4 0 (50) | 13.6 ± 23.4 0 (50) | 25 ± 35.4 25 (50) | 50 ± 0 50 (0) | 38.2 ± 28.1 50 (50) | 12.5 ± 22.6 0 (25) | <0.05 a |
| Trocar insertion | 52.6 ± 30.8 50 (0) | 66.7 ± 32.9 50 (50) | 44.4 ± 37.9 50 (50) | 61.5 ± 30 50 (50) | 47.9 ± 27.5 50 (0) | 45.5 ± 21.3 50 (0) | 0.07 a |
| Vitrectomy | 63.9 ± 48 50 (50) | 71.9 + 57.6 50 (50) | 53.6 + 41.4 50 (100) | 90.6 + 41.7 100 (50) | 64.7 + 46 50 (50) | 37.5 + 38.7 50 (50) | <0.05 a T vs. P |
| Laser treatment (endophotocoagulation) | 78.3 ± 50.4 50 (50) | 85 ± 40.1 100 (50) | 73.3 ± 45.8 50 (50) | 85 ± 53 100 (50) | 81.3 ± 68.3 50 (50) | 60 ± 31.6 50 (50) | 0.55 a |
| Liquid–air exchange | - | - | - | - | - | - | - |
| Silicone oil injection | - | - | - | - | - | - | - |
| Subconjunctival injection | - | - | - | - | - | - | - |
| Indentation | 39.6 ± 29.4 50 (50) | 50 ± 0 50 (0) | 70 ± 27.4 50 (50) | 39.6 ± 29.4 50 (50) | 33.3 ± 25.8 50 (50) | 16.7 ± 25.8 0 (50) | 0.21 a |
| Epiretinal membrane peeling | - | - | - | - | - | - | - |
| Diathermy | - | - | - | - | - | - | - |
| OVD removal | - | - | - | - | - | - | - |
| Trypan blue staining | - | - | - | - | - | - | - |
| Trocar removal | - | - | - | - | - | - | - |
| Speculum removal | - | - | - | - | - | - | - |
| Cumulative Dose of Rescue FNT in Patients with Intraoperative Pain Perception (∆SPI >15) | Total n = 175 (100) | GA Group n = 35 (100) | PBB Group n = 35 (100) | T Group n = 35 (100) | M Group n = 35 (100) | P Group n = 35 (100) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| 0 | Speculum installation | 23 (51.1) | 8 (72.7) | 1 (50) | 0 (0) | 5 (29.4) | 9 (75) | 0.09 a |
| 50–100 | 21 (46.7) | 3 (27.3) | 1 (50) | 3 (100) | 11 (64.7) | 3 (25) | ||
| 100–150 | 1 (2.2) | 0 (0) | 0 (0) | 0 (0) | 1 (5.9) | 0 (0) | ||
| 0 | Trocar insertion | 16 (16.3) | 2 (9.5) | 6 (33.3) | 1 (7.7) | 4 (16.7) | 3 (13.6) | <0.05 a |
| 50–100 | 61 (62,2) | 10 (47.6) | 8 (44.4) | 8 (61.5) | 17 (70.8) | 18 (81,8) | ||
| 100–150 | 21 (21.4) | 9 (42.9) | 4 (22.2) | 4 (30.8) | 3 (12.5) | 1 (4.5) | ||
| 0 | Vitrectomy | 17 (21.5) | 2 (12.5) | 4 (28.6) | 1 (6.3) | 3 (17.6) | 7 (43.8) | <0.05 a |
| 50–100 | 32 (40.5) | 9 (56.3) | 5 (35.7) | 4 (25) | 8 (47.1) | 6 (37.5) | ||
| 100–150 | 23 (29.1) | 3 (18.8) | 5 (35.7) | 8 (50) | 4 (23.5) | 3 (18.8) | ||
| 150–200 | 5 (6.3) | 0 (0) | 0 (0) | 3 (18.8) | 2 (11.8) | 0 (0) | ||
| >200 | 2 (2.5) | 2 (12.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| 0 | Laser treatment (endophotocoagulation) | 5 (6.8) | 0 (0) | 1 (6.7) | 1 (10) | 2 (10.5) | 1 (10) | 0.75 a |
| 50–100 | 36 (48.6) | 9 (45) | 8 (53.3) | 3 (30) | 10 (52.6) | 6 (60) | ||
| 100–150 | 25 (33.8) | 9 (45) | 5 (33.3) | 5 (50) | 3 (15.8) | 3 (30) | ||
| 150–200 | 2 (2.7) | 1 (5) | 0 (0) | 0 (0) | 1 (5.3) | 0 (0) | ||
| 200–250 | 5 (6.8) | 1 (5) | 1 (6.7) | 1 (10) | 2 (10.5) | 0 (0) | ||
| >250 | 1 (1.4) | 0 (0) | 0 (0) | 0 (0) | 1 (5.3) | 0 (0) | ||
| 0 | Indentation | 7 (29.2) | 0 (0) | 0 (0) | 1 (33.3) | 2 (33.3) | 4 (66.7) | 0.06 a |
| 50–100 | 15 (62.5) | 4 (100) | 3 (60) | 2 (66.7) | 4 (66.7) | 2 (33.3) | ||
| 100–150 | 2 (8.3) | 0 (0) | 2 (40) | 0 (0) | 0 (0) | 0 (0) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stasiowski, M.J.; Pluta, A.; Lyssek-Boroń, A.; Niewiadomska, E.; Krawczyk, L.; Dobrowolski, D.; Grabarek, B.O.; Kawka, M.; Rejdak, R.; Szumera, I.; et al. Adequacy of Anaesthesia for Nociception Detection during Vitreoretinal Surgery. Life 2023, 13, 505. https://doi.org/10.3390/life13020505
Stasiowski MJ, Pluta A, Lyssek-Boroń A, Niewiadomska E, Krawczyk L, Dobrowolski D, Grabarek BO, Kawka M, Rejdak R, Szumera I, et al. Adequacy of Anaesthesia for Nociception Detection during Vitreoretinal Surgery. Life. 2023; 13(2):505. https://doi.org/10.3390/life13020505
Chicago/Turabian StyleStasiowski, Michał Jan, Aleksandra Pluta, Anita Lyssek-Boroń, Ewa Niewiadomska, Lech Krawczyk, Dariusz Dobrowolski, Beniamin Oskar Grabarek, Magdalena Kawka, Robert Rejdak, Izabela Szumera, and et al. 2023. "Adequacy of Anaesthesia for Nociception Detection during Vitreoretinal Surgery" Life 13, no. 2: 505. https://doi.org/10.3390/life13020505
APA StyleStasiowski, M. J., Pluta, A., Lyssek-Boroń, A., Niewiadomska, E., Krawczyk, L., Dobrowolski, D., Grabarek, B. O., Kawka, M., Rejdak, R., Szumera, I., Missir, A., Hołyś, P., & Jałowiecki, P. (2023). Adequacy of Anaesthesia for Nociception Detection during Vitreoretinal Surgery. Life, 13(2), 505. https://doi.org/10.3390/life13020505






