Orf Infection on the Scalp of a Taiwanese Woman: A Case Report and Literature Review
Abstract
1. Introduction
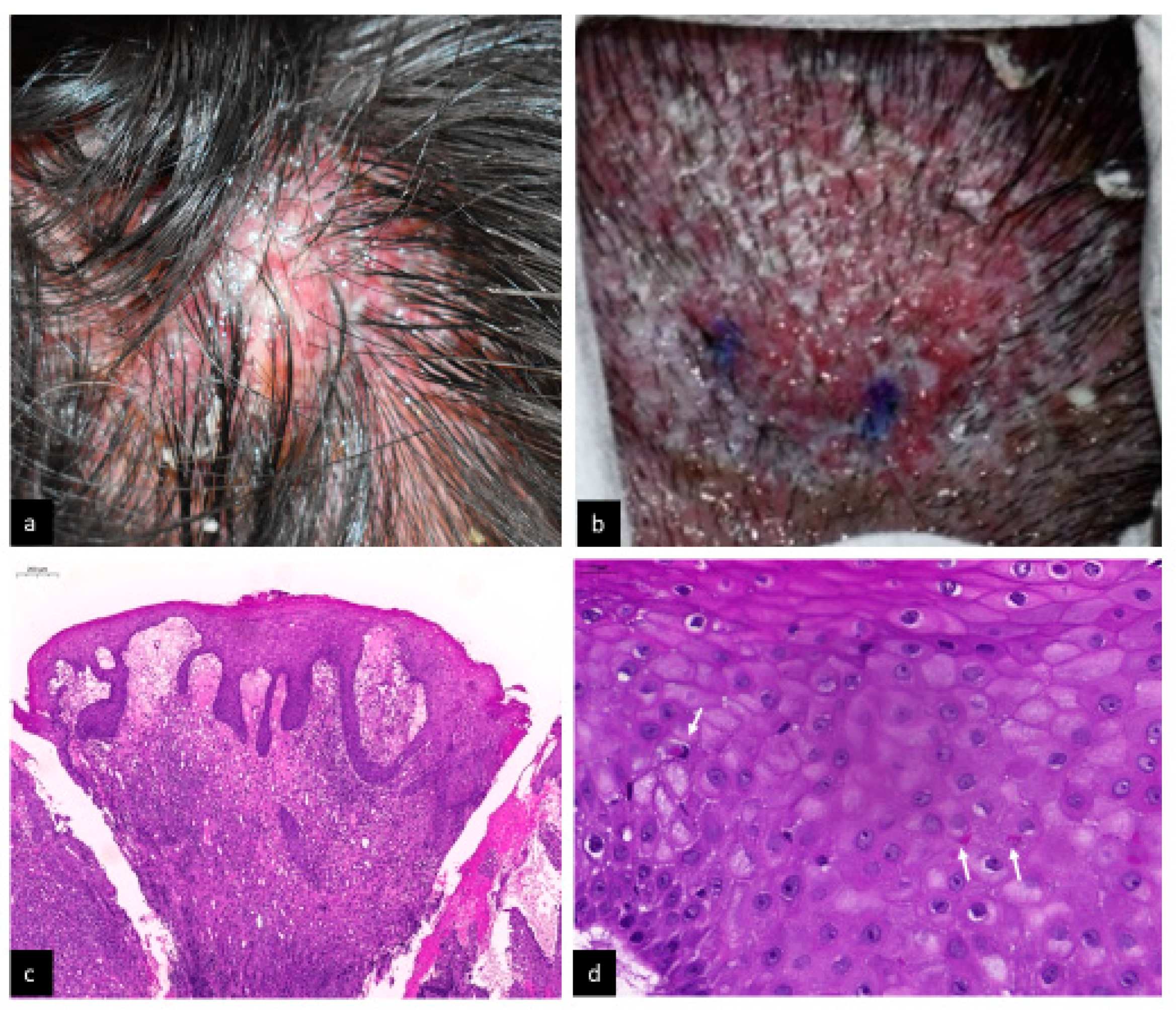
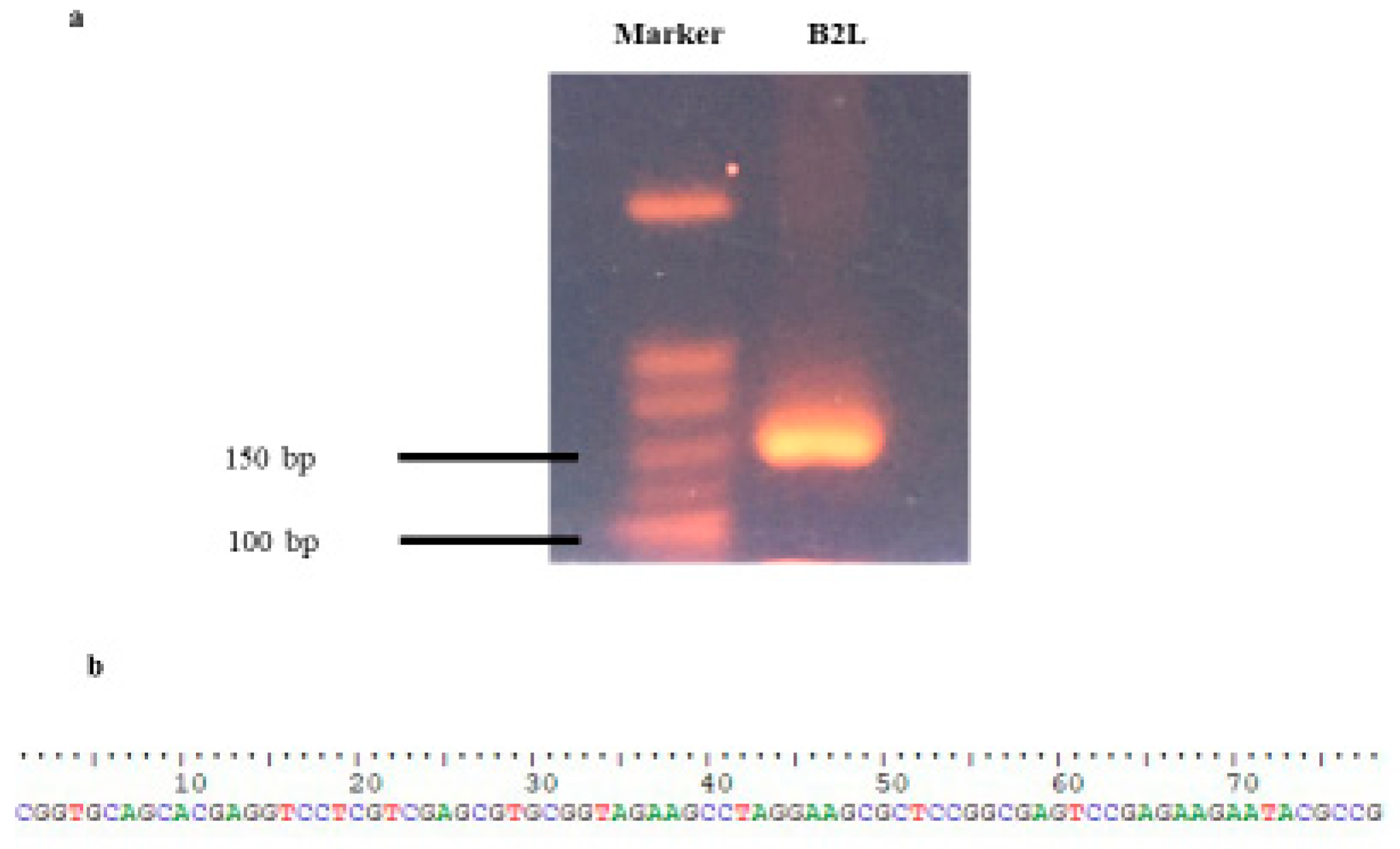
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kassa, T. A Review on Human Orf: A Neglected Viral Zoonosis. Res. Rep. Trop. Med. 2021, 12, 153–172. [Google Scholar] [CrossRef] [PubMed]
- Glass, J.; Ghali, F.E.; Sinkre, P.; Ricotti, C.A.; Cockerell, C.J. Acute Onset of Erythematous Scalp Nodules in a Child—Quiz Case. Arch. Dermatol. 2009, 145, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Rees, J.; Marks, J.M. Two unusual cases of orf following trauma to the scalp. Br. J. Dermatol. 1988, 118, 445–447. [Google Scholar] [CrossRef] [PubMed]
- Andreani, J.; Fongue, J.; Khalil, J.Y.B.; David, L.; Mougari, S.; Le Bideau, M.; Abrahão, J.; Berbis, P.; La Scola, B. Human Infection with Orf Virus and Description of Its Whole Genome, France, 2017. Emerg. Infect. Dis. 2019, 25, 2197–2204. [Google Scholar] [CrossRef] [PubMed]
- Mayet, A.; Sommer, B.; Heenan, P. Rapidly growing cutaneous tumour of the right temple: Orf. Australas. J. Dermatol. 1997, 38, 217–219. [Google Scholar] [CrossRef] [PubMed]
- Revenga, F.; Paricio, J.F.; del Agua, C.; Merino, F.J. Facial orf. J. Eur. Acad. Dermatol. Venereol. 2001, 15, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Gündüz, K.; Inanır, I.; Sacar, T. Orf and Religious Practices. J. Dermatol. 2005, 32, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Key, S.J.; Catania, J.; Mustafa, S.F.; Logan, R.; Kalavala, M.; Hodder, S.C.; Patton, D. Unusual Presentation of Human Giant Orf (Ecthyma Contagiosum). J. Craniofacial Surg. 2007, 18, 1076–1078. [Google Scholar] [CrossRef] [PubMed]
- Bayindir, Y.; Bayraktar, M.; Karadag, N.; Ozcan, H.; Kayabas, U.; Otlu, B.; Durmaz, R.; Doganay, M. Investigation and analysis of a human orf outbreak among people living on the same farm. New Microbiol. 2011, 34, 37–43. [Google Scholar] [PubMed]
- Duchateau, N.C.; Aerts, O.; Lambert, J. Autoinoculation with Orf virus (ecthyma contagiosum). Int. J. Dermatol. 2013, 53, e60–e62. [Google Scholar] [CrossRef] [PubMed]
- Turk, B.G.; Senturk, B.; Dereli, T.; Yaman, B. A rare human-to-human transmission of orf. Int. J. Dermatol. 2013, 53, e63–e65. [Google Scholar] [CrossRef] [PubMed]
- Ata, N.; Göğüş, H.E.; Kiliç, S. Giant Orf on the Nose. J. Craniofac. Surg. 2017, 28, e234–e235. [Google Scholar] [CrossRef] [PubMed]
- Gore Karaali, M.; Esra Koku Aksu, A.; Kara Polat, A.; Salih Gurel, M. Solitary facial lesion of orf: An unusual presentation. North Clin. Istanb. 2021, 8, 626–628. [Google Scholar] [CrossRef] [PubMed]
- Rezende, A.L.R.A.; Filho, F.B.; De Paula, N.A.; Towersey, L.; Hay, R.; Frade, M.A.C. Clinical Manifestation, Dermoscopy, and Scanning Electron Microscopy in Two Cases of Contagious Ecthyma (Orf Nodule). Case Rep. Dermatol. Med. 2018, 2018, 2094086. [Google Scholar] [CrossRef] [PubMed]
- Flores, C.; González, E.; Verna, A.; Peralta, A.; Madariaga, C.; Odeón, A.C.; Cantón, G. Orf virus in human, confirmation in case report from Chile. Rev. Chilena Infectol. 2017, 34, 607–609. [Google Scholar] [CrossRef] [PubMed]
- Sunderkötter, C.; Becker, K.; Kutzner, H.; Meyer, T.; Blödorn-Schlicht, N.; Reischl, U.; Nenoff, P.; Geißdörfer, W.; Gräser, Y.; Herrmann, M.; et al. Molecular diagnosis of skin infections using paraffin-embedded tissue-review and interdisciplinary consensus. JDDG J. Dtsch. Dermatol. Ges. 2018, 16, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Santiago, L.; Oliveira, D.; Cardoso, J.C.; Figueired, A. Human Orf: An Under-recognized Entity. Acta Dermatovenerol. Croat. 2019, 27, 280–281. [Google Scholar] [PubMed]
- Haddock, E.S.; Cheng, C.E.; Bradley, J.S.; Hsu, C.H.; Zhao, H.; Davidson, W.B.; Barrio, V.R. Extensive orf infection in a toddler with associated id reaction. Pediatr. Dermatol. 2017, 34, e337–e340. [Google Scholar] [CrossRef] [PubMed]
| Author, Year | Age/Sex | Occupation | Contact History | Location | Clinical Features | Further Confirming Diagnostic Tools Except Skin Biopsy | Time to Resolution |
|---|---|---|---|---|---|---|---|
| Glass et al., 2009 [2] | 10/M | Not mentioned | Not mentioned | Bilateral occipital scalp | A 0.9 cm bleeding nodule and another 2.5 cm ulcerated crusted nodule and the biopsied lesion recurred with an adjacent new lesion | No | Not mentioned |
| Rees et al., 1988 [3] | 59/M | Mechanic of a farm | With trauma history | Right parietal scalp | A 2 × 3 cm pustular nodule. Lymphadenopathy in the posterior triangle of the neck | Electron microscopy | 4 weeks |
| 61/M | Shepherd | With trauma history | Left parietal scalp | A 3 cm diameter haemorrhagic pustule Lymphadenopathy in the posterior triangle of the neck Fever (+) | Electron microscopy | 4 weeks | |
| Revenga et al., 2001 [6] | 40/F | Shepherd | With trauma history | Right eyelid | A 2 cm crusted nodule | Electron microscopy | Weeks |
| Turk et al., 2014 [11] | 16/F | Not mentioned | With trauma history | Frontotemporal region (face) | 0.7–2.0 cm targetoid nodules | No | 2 weeks |
| Gore Karaali et al., 2021 [13] | 54/M | Not mentioned | With trauma history | Left eyebrow | A 3 cm edematous, ulcerated, hemorrhagic nodule | No | 6 weeks |
| Mayet et al., 1997 [5] | 61/M | Visitor of a farm | No trauma (contact with contaminated material in a shearing shed or the barbed wire of a fence) | Right temple | A 2 cm ulcerated nodule | Electron microscopy | Not mentioned |
| Gündüz et al., 2005 [7] | Not mentioned/M | Farmer | No trauma (fed animals) | Left mandible | Erythematous weeping nodule | No | 8 weeks |
| Key et al. 2007 [8] | 41/M | Farmer | No trauma (fed newborn lambs) | Right cheek | 1. A 5 cm exophytic oozing crusted tumor, Cervical lymphadenopathy (+) Fever (+) 2. Lesions progressed after therapy (curettage and pulsed dye lase) | Electron microscopy | Weeks |
| Bayindir et al., 2011 [9] | 19/M | Not mentioned | No trauma (contact with the animals or eating meat of sick animals) | Upper lip | Targetoid/weeping nodule | PCR | 36 days |
| Duchateau et al., 2014 [10] | 38/M | Not mentioned | No trauma (contact with a lamb) | Right hand and right lower jaw | A tender, erosive lesion and multiple papulonodules | No | 8 weeks |
| Ata et al., 2017 [12] | 52/M | Not mentioned | No trauma (contact with sheep with hands) | Nose | A painless 2 × 1.7 cm nodule | PCR | 8 weeks |
| Our case | 55/F | Farmer | No trauma (contact with a lamb) | Vertex and occipital scalp | Four 2 × 2 cm to 4 × 4 cm weeping and infiltrated noduloplaques | PCR | 2 weeks |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juang, S.-J.; Win, K.-T.; Chen, Y.-L.; Chen, H.-W.; Cheng, P.-S. Orf Infection on the Scalp of a Taiwanese Woman: A Case Report and Literature Review. Life 2023, 13, 358. https://doi.org/10.3390/life13020358
Juang S-J, Win K-T, Chen Y-L, Chen H-W, Cheng P-S. Orf Infection on the Scalp of a Taiwanese Woman: A Case Report and Literature Review. Life. 2023; 13(2):358. https://doi.org/10.3390/life13020358
Chicago/Turabian StyleJuang, Shiow-Jen, Khin-Than Win, Yen-Lin Chen, Hung-Wen Chen, and Pai-Shan Cheng. 2023. "Orf Infection on the Scalp of a Taiwanese Woman: A Case Report and Literature Review" Life 13, no. 2: 358. https://doi.org/10.3390/life13020358
APA StyleJuang, S.-J., Win, K.-T., Chen, Y.-L., Chen, H.-W., & Cheng, P.-S. (2023). Orf Infection on the Scalp of a Taiwanese Woman: A Case Report and Literature Review. Life, 13(2), 358. https://doi.org/10.3390/life13020358





