Anti-CD20 Antibody and Calcineurin Inhibitor Combination Therapy Effectively Suppresses Antibody-Mediated Rejection in Murine Orthotopic Lung Transplantation
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Model
2.2. Surgical Technique
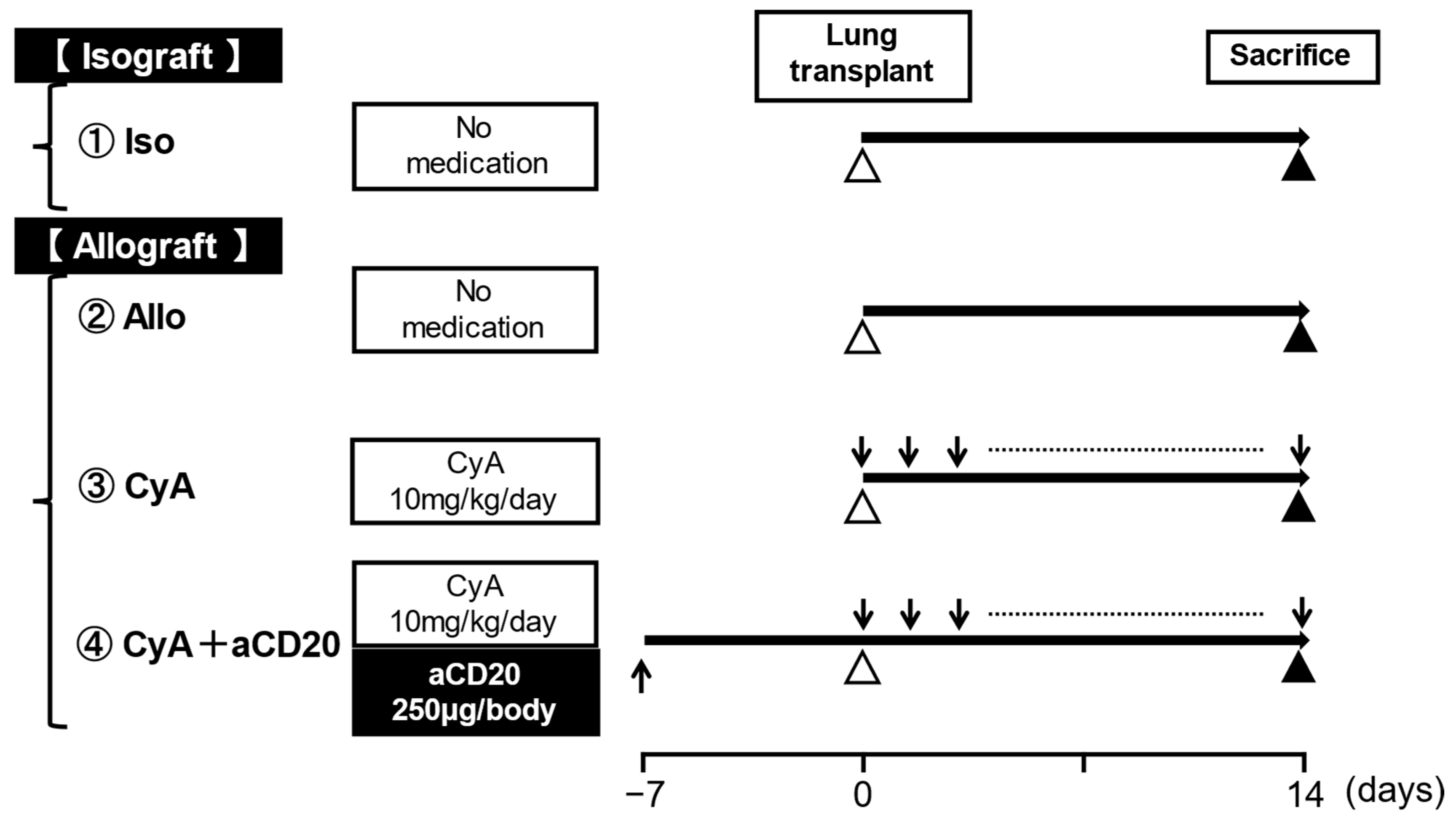
2.3. Medication Protocols
2.4. Histology and Immunohistochemistry
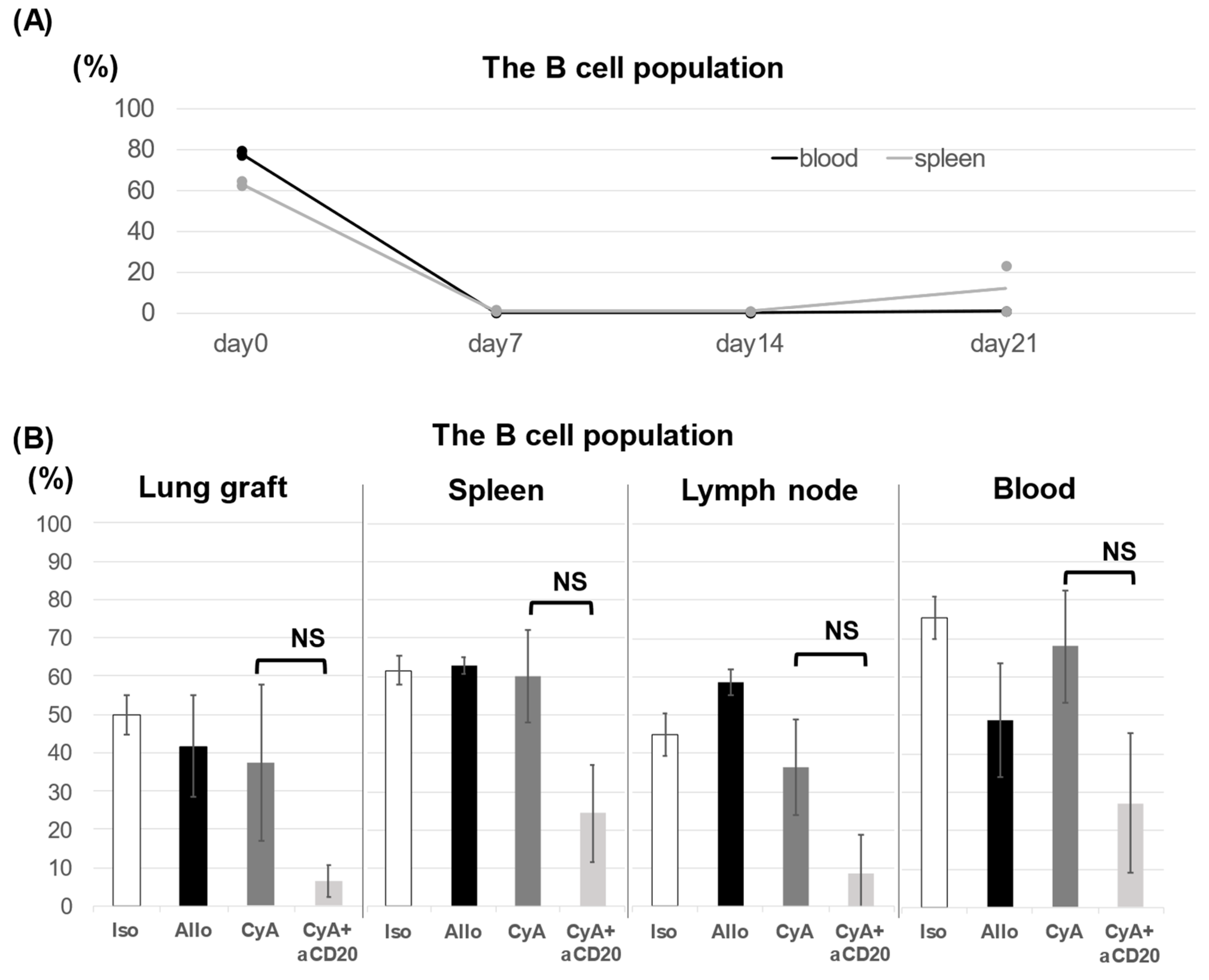
2.5. Flow Cytometry
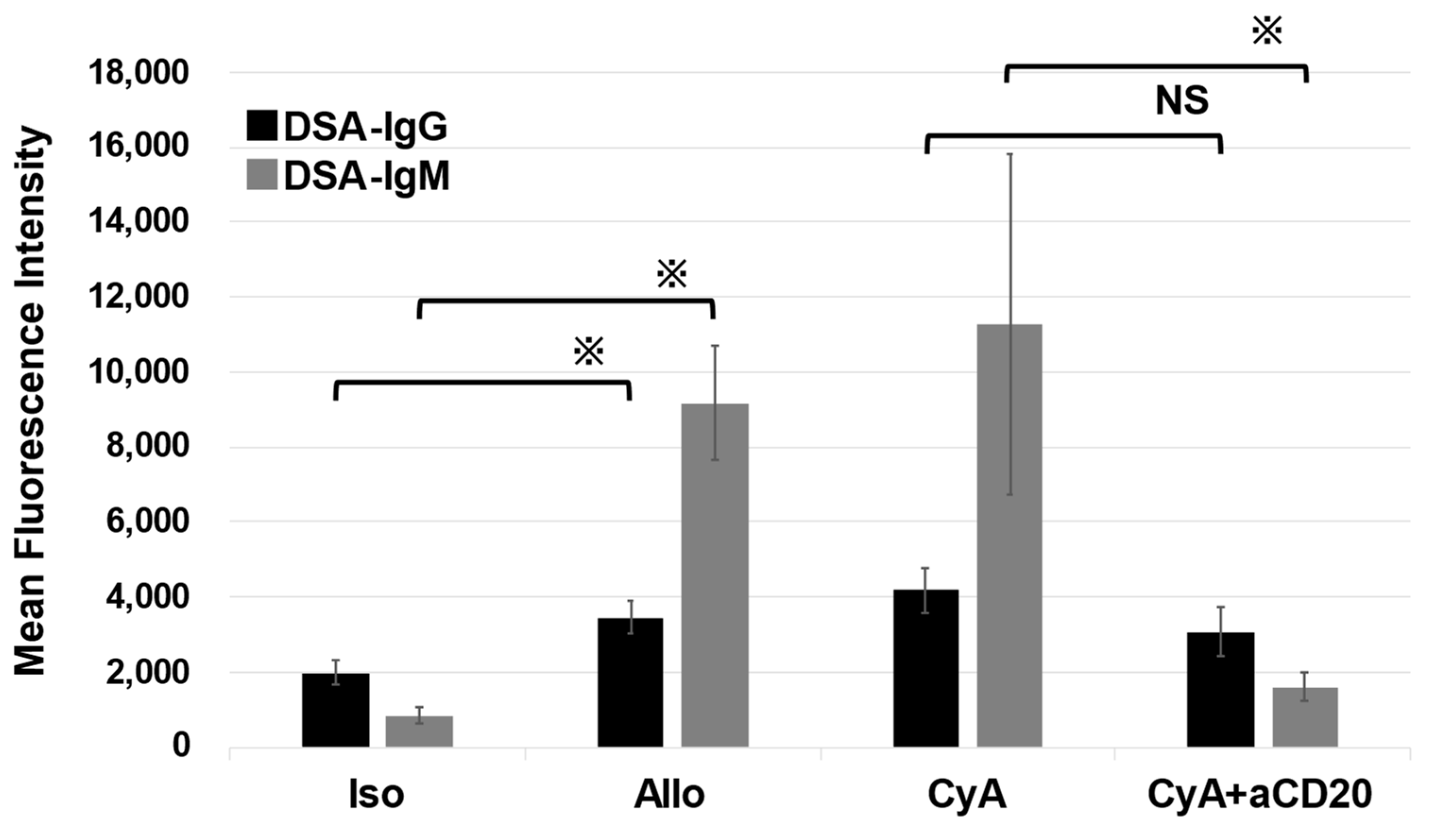
2.6. Measurement of Serum Donor-Specific Antibodies
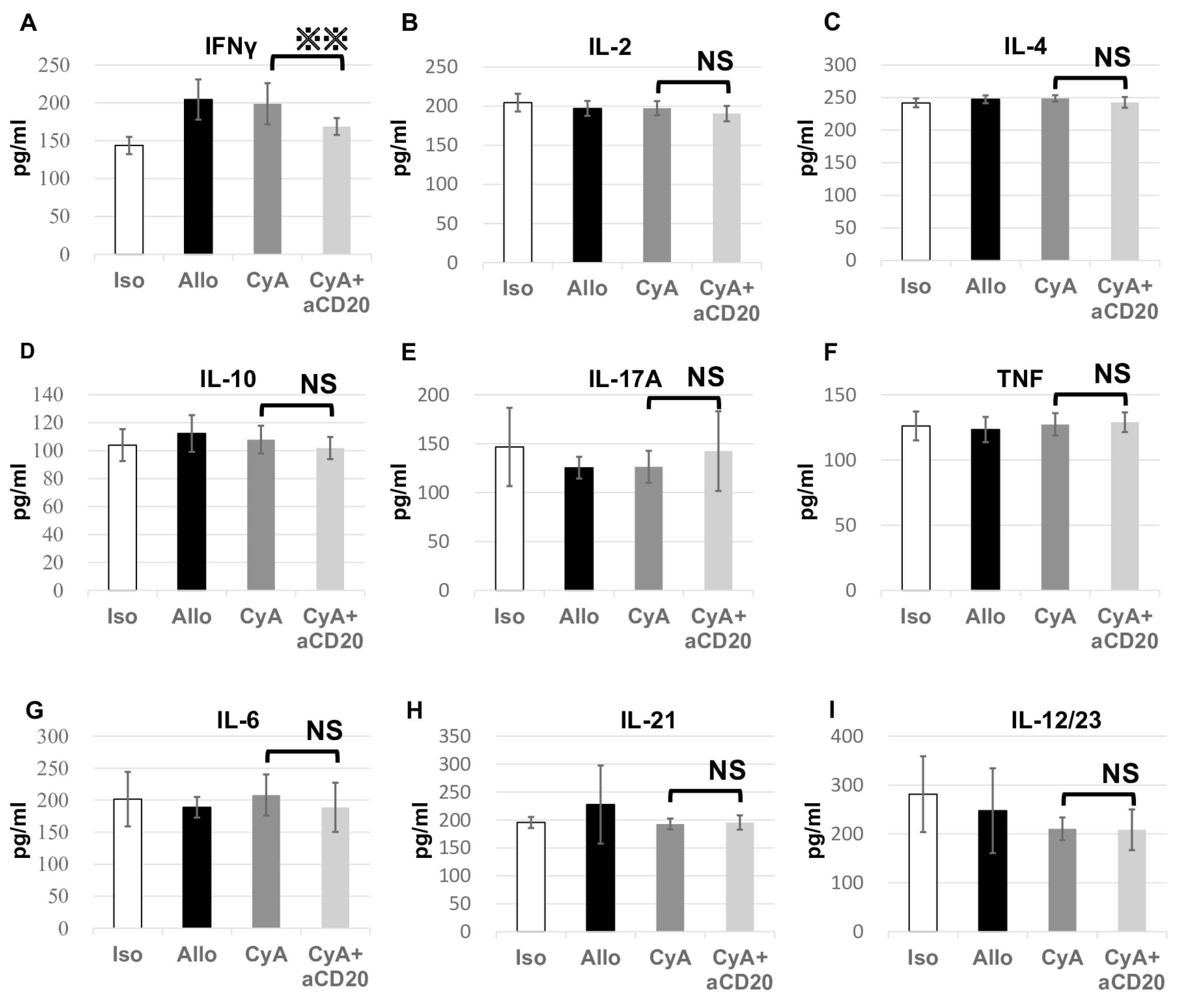
2.7. Cytokine Analysis
2.8. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gracon, A.S.; Wilkes, D.S. Lung transplantation: Chronic allograft dysfunction and establishing immune tolerance. Hum. Immunol. 2014, 75, 887–894. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yusen, R.D.; Christie, J.D.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dipchand, A.I.; Dobbels, F.; Kirk, R.; Lund, L.H.; Rahmel, A.O.; et al. The Registry of the International Society for Heart and Lung Transplantation: Thirtieth Adult Lung and Heart-Lung Transplant Report—2013; focus theme: Age. J. Heart Lung Transplant. 2013, 32, 965–978. [Google Scholar] [CrossRef] [PubMed]
- Yusen, R.D.; Edwards, L.B.; Dipchand, A.I.; Goldfarb, S.B.; Kucheryavaya, A.Y.; Levvey, B.J.; Lund, L.H.; Meiser, B.; Rossano, J.W.; Stehlik, J.; et al. The registry of the International Society for Heart and Lung Transplantation: Thirty-third adult lung and heart-lung transplant Report-2016; focus theme: Primary diagnostic indications for transplant. J. Heart Lung Transplant. 2016, 35, 1170–1184. [Google Scholar] [CrossRef] [PubMed]
- Verleden, G.M.; Vos, R.; Vanaudenaerde, B.; Dupont, L.; Yserbyt, J.; Van Raemdonck, D.; Verleden, S. Current views on chronic rejection after lung transplantation. Transpl. Int. 2015, 28, 1131–1139. [Google Scholar] [CrossRef] [PubMed]
- Christie, J.D.; Edwards, L.B.; Kucheryavaya, A.Y.; Benden, C.; Dobbels, F.; Kirk, R.; Rahmel, A.O.; Stehlik, J.; Hertz, M.I.; International Society for Heart and Lung Transplantation. The registry of the International Society for Heart and Lung Transplantation: Twenty-eighth adult lung and heart-lung transplant report—2011. J. Heart Lung Transplant. 2011, 30, 1104–1122. [Google Scholar] [CrossRef]
- Hachem, R.R.; Yusen, R.D.; Meyers, B.F.; Aloush, A.A.; Mohanakumar, T.; Patterson, G.A.; Trulock, E.P. Anti-human leukocyte antigen antibodies and preemptive antibody-directed therapy after lung transplantation. J. Heart Lung Transplant. 2010, 29, 973–980. [Google Scholar] [CrossRef]
- Hachem, R.R. Acute rejection and antibody-mediated rejection in lung transplantation. Clin. Chest Med. 2017, 38, 667–675. [Google Scholar] [CrossRef]
- Roux, A.; Levine, D.J.; Zeevi, A.; Hachem, R.; Halloran, K.; Halloran, P.F.; Gibault, L.; Taupin, J.L.; Neil, D.A.H.; Loupy, A.; et al. Banff Lung Report: Current knowledge and future research perspectives for diagnosis and treatment of pulmonary antibody-mediated rejection (AMR). Am. J. Transplant. 2019, 19, 21–31. [Google Scholar] [CrossRef]
- Yamanashi, K.; Chen-Yoshikawa, T.F.; Hamaji, M.; Yurugi, K.; Tanaka, S.; Yutaka, Y.; Yamada, Y.; Nakajima, D.; Ohsumi, A.; Date, H. Outcomes of combination therapy including rituximab for antibody-mediated rejection after lung transplantation. Gen. Thorac. Cardiovasc. Surg. 2020, 68, 142–149. [Google Scholar] [CrossRef]
- Levine, D.J.; Glanville, A.R.; Aboyoun, C.; Belperio, J.; Benden, C.; Berry, G.J.; Hachem, R.; Hayes, D.; Neil, D.; Reinsmoen, N.L.; et al. Antibody-mediated rejection of the lung: A consensus report of the International Society for Heart and Lung Transplantation. J. Heart Lung Transplant. 2016, 35, 397–406. [Google Scholar] [CrossRef]
- Bery, A.I.; Hachem, R.R. Antibody-mediated rejection after lung transplantation. Ann. Transl. Med. 2020, 8, 411. [Google Scholar] [CrossRef] [PubMed]
- Dijke, E.I.; Platt, J.L.; Blair, P.; Clatworthy, M.R.; Patel, J.K.; Kfoury, A.G.; Cascalho, M. B cells in transplantation. J. Heart Lung Transplant. 2016, 35, 704–710. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Sekine, Y.; Yoshida, S.; Yasufuku, K.; Petrache, I.; Benson, H.L.; Brand, D.D.; Yoshino, I.; Wilkes, D.S. Type V collagen-induced oral tolerance plus low-dose cyclosporine prevents rejection of MHC class I and II incompatible lung allografts. J. Immunol. 2009, 183, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, H.; Fan, L.; Wilkes, D.S. Development of obliterative bronchiolitis in a murine model of orthotopic lung transplantation. J. Vis. Exp. 2012, 65, e3947. [Google Scholar] [CrossRef]
- Hata, A.; Suzuki, H.; Nakajima, T.; Fujiwara, T.; Shiina, Y.; Kaiho, T.; Toyoda, T.; Inage, T.; Ito, T.; Sakairi, Y.; et al. Differential gene analysis during the development of obliterative bronchiolitis in a murine orthotopic lung transplantation model: A comprehensive transcriptome-based analysis. PLoS ONE 2020, 15, e0232884. [Google Scholar] [CrossRef]
- Suzuki, H.; Lasbury, M.E.; Fan, L.; Vittal, R.; Mickler, E.A.; Benson, H.L.; Shilling, R.; Wu, Q.; Weber, D.J.; Wagner, S.R.; et al. Role of complement activation in obliterative bronchiolitis post-lung transplantation. J. Immunol. 2013, 191, 4431–4439. [Google Scholar] [CrossRef]
- Shiina, Y.; Suzuki, H.; Hata, A.; Kaiho, T.; Matsumoto, H.; Toyoda, T.; Sakairi, Y.; Wada, H.; Motohashi, S.; Yoshino, I. Antibodies against complement component C5 prevent antibody-mediated rejection after lung transplantation in murine orthotopic models with skin-graft-induced pre-sensitization. Gen. Thorac. Cardiovasc. Surg. 2022, 70, 1032–1041. [Google Scholar] [CrossRef]
- Barnett, A.N.R.; Hadjianastassiou, V.G.; Mamode, N. Rituximab in renal transplantation. Transpl. Int. 2013, 26, 563–575. [Google Scholar] [CrossRef]
- Mamode, N.; Bestard, O.; Claas, F.; Furian, L.; Griffin, S.; Legendre, C.; Pengel, L.; Naesens, M. European guideline for the management of kidney transplant patients with HLA antibodies: By the European society for organ transplantation working group. Transpl. Int. 2022, 35, 10511. [Google Scholar] [CrossRef]
- Lee, E.C.; Kim, S.H.; Park, S.J. Outcomes after liver transplantation in accordance with ABO compatibility: A systematic review and meta-analysis. World J. Gastroenterol. 2017, 23, 6516–6533. [Google Scholar] [CrossRef]
- Hwang, S.D.; Lee, J.H.; Kim, K.; Lee, S.W.; Song, J.H. Effect of rituximab used as induction in patients with ABO mismatch kidney transplant: A systematic review and meta-analysis. Transplant. Proc. 2020, 52, 3125–3128. [Google Scholar] [CrossRef] [PubMed]
- Golay, J.; Semenzato, G.; Rambaldi, A.; Foà, R.; Gaidano, G.; Gamba, E.; Pane, F.; Pinto, A.; Specchia, G.; Zaja, F.; et al. Lessons for the clinic from rituximab pharmacokinetics and pharmacodynamics. mAbs. 2013, 5, 826–837. [Google Scholar] [CrossRef] [PubMed]
- Vacha, M.; Chery, G.; Hulbert, A.; Byrns, J.; Benedetti, C.; Finlen Copeland, C.A.; Gray, A.; Onwuemene, O.; Palmer, S.M.; Snyder, L.D. Antibody depletion strategy for the treatment of suspected antibody-mediated rejection in lung transplant recipients: Does it work? Clin. Transplant. 2017, 2017, 886. [Google Scholar] [CrossRef]
- Ius, F.; Verboom, M.; Sommer, W.; Poyanmehr, R.; Knoefel, A.K.; Salman, J.; Kuehn, C.; Avsar, M.; Siemeni, T.; Erdfelder, C.; et al. Preemptive treatment of early donor-specific antibodies with IgA- and IgM-enriched intravenous human immunoglobulins in lung transplantation. Am. J. Transplant. 2018, 18, 2295–2304. [Google Scholar] [CrossRef]
- Moyron-Quiroz, J.E.; Lin, L.; Oida, T.; Garcia-Mojica, S.; Yang, X. Kinetic study of B cell-depletion with a novel mAb anti-mouse CD20, clone SA271G2. J. Immunol. 2016, 196, 923. [Google Scholar] [CrossRef]
- Stewart, S.; Fishbein, M.C.; Snell, G.I.; Berry, G.J.; Boehler, A.; Burke, M.M.; Glanville, A.; Gould, F.K.; Magro, C.; Marboe, C.C.; et al. Revision of the 1996 working formulation for the standardization of nomenclature in the diagnosis of lung rejection. J. Heart Lung Transplant. 2007, 26, 1229–1242. [Google Scholar] [CrossRef]
- Berry, G.; Burke, M.; Andersen, C.; Angelini, A.; Bruneval, P.; Calabrese, F.; Fishbein, M.C.; Goddard, M.; Leone, O.; Maleszewski, J.; et al. Pathology of pulmonary antibody-mediated rejection: 2012 update from the Pathology Council of the ISHLT. J. Heart Lung Transplant. 2013, 32, 14–21. [Google Scholar] [CrossRef]
- Roden, A.C.; Maleszewski, J.J.; Yi, E.S.; Jenkins, S.M.; Gandhi, M.J.; Scott, J.P.; Aubry, M.C. Reproducibility of Complement 4d deposition by immunofluorescence and immunohistochemistry in lung allograft biopsies. J. Heart Lung Transplant. 2014, 33, 1223–1232. [Google Scholar] [CrossRef]
- Miyamoto, E.; Motoyama, H.; Sato, M.; Aoyama, A.; Menju, T.; Shikuma, K.; Sowa, T.; Yoshizawa, A.; Saito, M.; Takahagi, A.; et al. Association of local intrapulmonary production of antibodies specific to donor major histocompatibility complex Class I with the progression of chronic rejection of lung allografts. Transplantation 2017, 101, e156–e165. [Google Scholar] [CrossRef]
- Morgan, E.; Varro, R.; Sepulveda, H.; Ember, J.A.; Apgar, J.; Wilson, J.; Lowe, L.; Chen, R.; Shivraj, L.; Agadir, A.; et al. Cytometric bead array: A multiplexed assay platform with applications in various areas of biology. Clin. Immunol. 2004, 110, 252–266. [Google Scholar] [CrossRef]
- Lobo, L.J.; Aris, R.M.; Schmitz, J.; Neuringer, I.P. Donor-specific antibodies are associated with antibody-mediated rejection, acute cellular rejection, bronchiolitis obliterans syndrome, and cystic fibrosis after lung transplantation. J. Heart Lung Transplant. 2013, 32, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Witt, C.A.; Gaut, J.P.; Yusen, R.D.; Byers, D.E.; Iuppa, J.A.; Bain, K.B.; Patterson, G.A.; Mohanakumar, T.; Trulock, E.P.; Hachem, R.R. Acute antibody-mediated rejection after lung transplantation. J. Heart Lung Transplant. 2013, 32, 1034–1040. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, S.S.; Azimzadeh, A.M.; Zhang, T.; Stoddard, T.; Welty, E.; Avon, C.; Higuchi, M.; Laaris, A.; Cheng, X.F.; McMahon, C.; et al. Preemptive CD20+ B cell depletion attenuates cardiac allograft vasculopathy in cyclosporine-treated monkeys. J. Clin. Invest. 2010, 120, 1275–1284. [Google Scholar] [CrossRef]
- Becker, P.D.; Ratnasothy, K.; Sen, M.; Peng, Q.; Romano, M.; Bazoer, J.; Suvitra, E.; Stout, A.; Hylton, S.G.; Dorling, A.; et al. B lymphocytes contribute to indirect pathway T cell sensitization via acquisition of extracellular vesicles. Am. J. Transplant. 2021, 21, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.; Watanabe, T.; Li, X.K. Approaches for controlling antibody-mediated allograft rejection through targeting B cells. Front. Immunol. 2021, 12, 682334. [Google Scholar] [CrossRef]
- Ohm, B.; Jungraithmayr, W. B cell immunity in lung transplant rejection—Effector mechanisms and therapeutic implications. Front. Immunol. 2022, 13, 845867. [Google Scholar] [CrossRef] [PubMed]
- Smirnova, N.F.; Conlon, T.M.; Morrone, C.; Dorfmuller, P.; Humbert, M.; Stathopoulos, G.T.; Umkehrer, S.; Pfeiffer, F.; Yildirim, A.Ö.; Eickelberg, O. Inhibition of B cell-dependent lymphoid follicle formation prevents lymphocytic bronchiolitis after lung transplantation. JCI Insight 2019, 4, e123971. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, T.; Martinu, T.; Chruscinski, A.; Boonstra, K.; Joe, B.; Horie, M.; Guan, Z.; Bei, K.F.; Hwang, D.M.; Liu, M.; et al. A B cell–dependent pathway drives chronic lung allograft rejection after ischemia–reperfusion injury in mice. Am. J. Transplant. 2019, 19, 3377–3389. [Google Scholar] [CrossRef]
- Ng, Y.H.; Oberbarnscheidt, M.H.; Chandramoorthy, H.C.K.; Hoffman, R.; Chalasani, G. B cells help alloreactive T cells differentiate into memory T cells. Am. J. Transplant. 2010, 10, 1970–1980. [Google Scholar] [CrossRef]
- Zarkhin, V.; Li, L.; Sarwal, M. “To B or not to B?” B-cells and graft rejection. Transplantation 2008, 85, 1705–1714. [Google Scholar] [CrossRef]
- Zhao, D.; Liao, T.; Li, S.; Zhang, Y.; Zheng, H.; Zhou, J.; Han, F.; Dong, Y.; Sun, Q. Mouse model established by early renal transplantation after skin allograft sensitization mimics clinical antibody-mediated rejection. Front. Immunol. 2018, 9, 1356. [Google Scholar] [CrossRef]
- Sweet, S.C.; Armstrong, B.; Blatter, J.; Chin, H.; Conrad, C.; Goldfarb, S.; Hayes, D.; Heeger, P.S.; Lyou, V.; Melicoff-Portillo, E.; et al. CTOTC-08: A multicenter randomized controlled trial of rituximab induction to reduce antibody development and improve outcomes in pediatric lung transplant recipients. Am. J. Transplant. 2022, 22, 230–244. [Google Scholar] [CrossRef] [PubMed]
- Stroopinsky, D.; Katz, T.; Rowe, J.M.; Melamed, D.; Avivi, I. Rituximab-induced direct inhibition of T-cell activation. Cancer Immunol. Immunother. 2012, 61, 1233–1241. [Google Scholar] [CrossRef] [PubMed]
- Ngo, C.; Daniel, C.; Duong-Quy, S.; Brugière, O.; Cazes, A. Utility of C4d by immunohistochemistry for the diagnosis of antibody-mediated rejection in lung transplantation. Eur. Respir. J. 2016, 48, PA4636. [Google Scholar] [CrossRef]
- Aguilar, P.R.; Carpenter, D.; Ritter, J.; Yusen, R.D.; Witt, C.A.; Byers, D.E.; Mohanakumar, T.; Kreisel, D.; Trulock, E.P.; Hachem, R.R. The role of C4d deposition in the diagnosis of antibody-mediated rejection after lung transplantation. Am. J. Transplant. 2018, 18, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Mimura, T.; Walker, N.; Aoki, Y.; Manning, C.M.; Murdock, B.J.; Myers, J.L.; Lagstein, A.; Osterholzer, J.J.; Lama, V.N. Local origin of mesenchymal cells in a murine orthotopic lung transplantation model of bronchiolitis obliterans. Am. J. Pathol. 2015, 185, 1564–1574. [Google Scholar] [CrossRef] [PubMed]

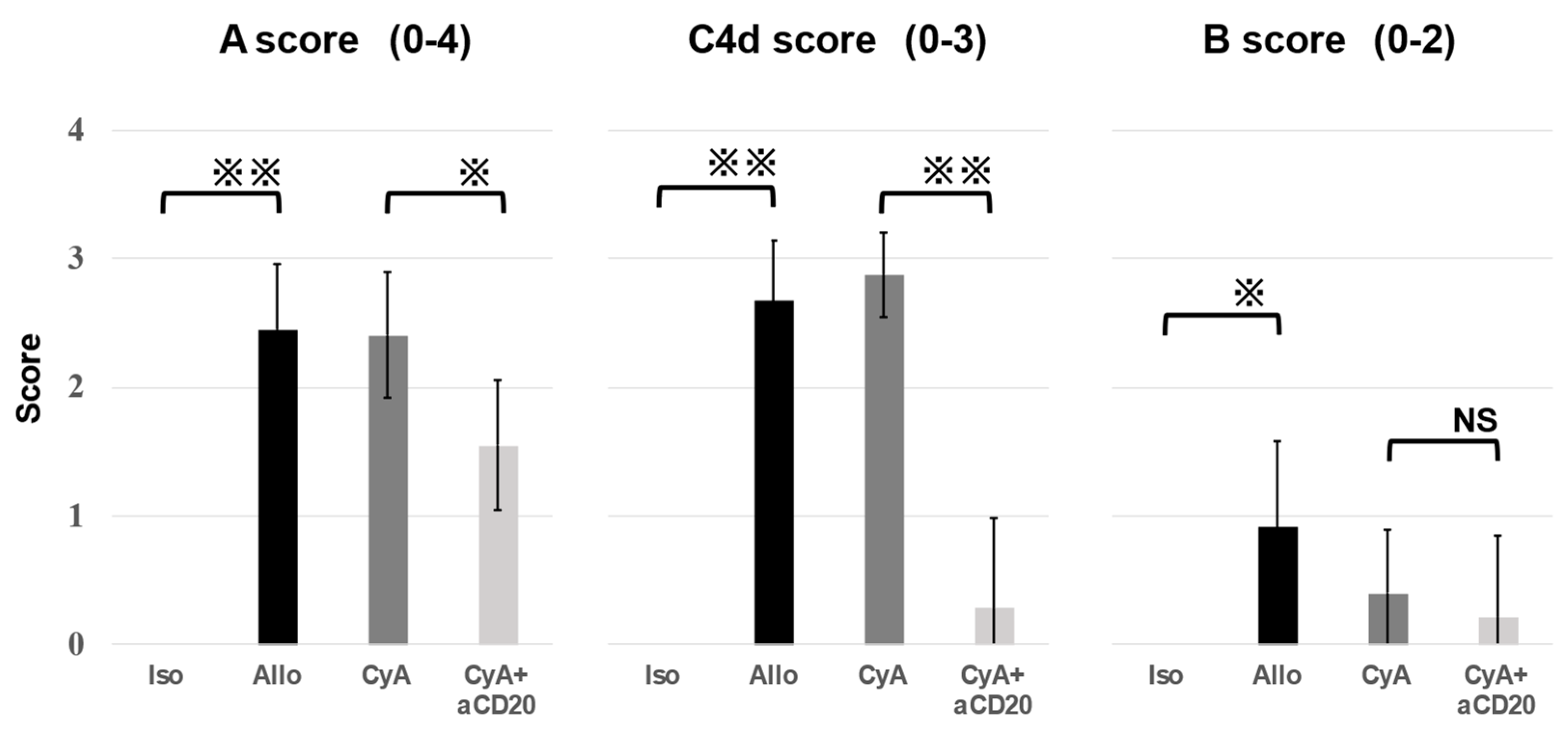
| (a) | |||
|---|---|---|---|
| Allo | CyA | p-Value | |
| A score | 2.45 ± 0.50 | 2.40 ± 0.49 | 0.99 |
| C4d score | 2.67 ± 0.47 | 2.88 ± 0.33 | 0.76 |
| B score | 0.91 ± 0.67 | 0.40 ± 0.49 | 0.31 |
| (b) | |||
| CyA | CyA+aCD20 | p-Value | |
| A score | 2.40 ± 0.49 | 1.55 ± 0.50 | 0.030 |
| C4d score | 2.88 ± 0.33 | 0.29 ± 0.70 | 0.0028 |
| B score | 0.40 ± 0.49 | 0.22 ± 0.63 | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, H.; Suzuki, H.; Yamanaka, T.; Kaiho, T.; Hata, A.; Inage, T.; Ito, T.; Kamata, T.; Tanaka, K.; Sakairi, Y.; et al. Anti-CD20 Antibody and Calcineurin Inhibitor Combination Therapy Effectively Suppresses Antibody-Mediated Rejection in Murine Orthotopic Lung Transplantation. Life 2023, 13, 2042. https://doi.org/10.3390/life13102042
Matsumoto H, Suzuki H, Yamanaka T, Kaiho T, Hata A, Inage T, Ito T, Kamata T, Tanaka K, Sakairi Y, et al. Anti-CD20 Antibody and Calcineurin Inhibitor Combination Therapy Effectively Suppresses Antibody-Mediated Rejection in Murine Orthotopic Lung Transplantation. Life. 2023; 13(10):2042. https://doi.org/10.3390/life13102042
Chicago/Turabian StyleMatsumoto, Hiroki, Hidemi Suzuki, Takahiro Yamanaka, Taisuke Kaiho, Atsushi Hata, Terunaga Inage, Takamasa Ito, Toshiko Kamata, Kazuhisa Tanaka, Yuichi Sakairi, and et al. 2023. "Anti-CD20 Antibody and Calcineurin Inhibitor Combination Therapy Effectively Suppresses Antibody-Mediated Rejection in Murine Orthotopic Lung Transplantation" Life 13, no. 10: 2042. https://doi.org/10.3390/life13102042
APA StyleMatsumoto, H., Suzuki, H., Yamanaka, T., Kaiho, T., Hata, A., Inage, T., Ito, T., Kamata, T., Tanaka, K., Sakairi, Y., Motohashi, S., & Yoshino, I. (2023). Anti-CD20 Antibody and Calcineurin Inhibitor Combination Therapy Effectively Suppresses Antibody-Mediated Rejection in Murine Orthotopic Lung Transplantation. Life, 13(10), 2042. https://doi.org/10.3390/life13102042






