Assessment of Surrogate Markers for Cardiovascular Disease in Familial Mediterranean Fever-Related Amyloidosis Patients Homozygous for M694V Mutation in MEFV Gene
Abstract
:1. Introduction
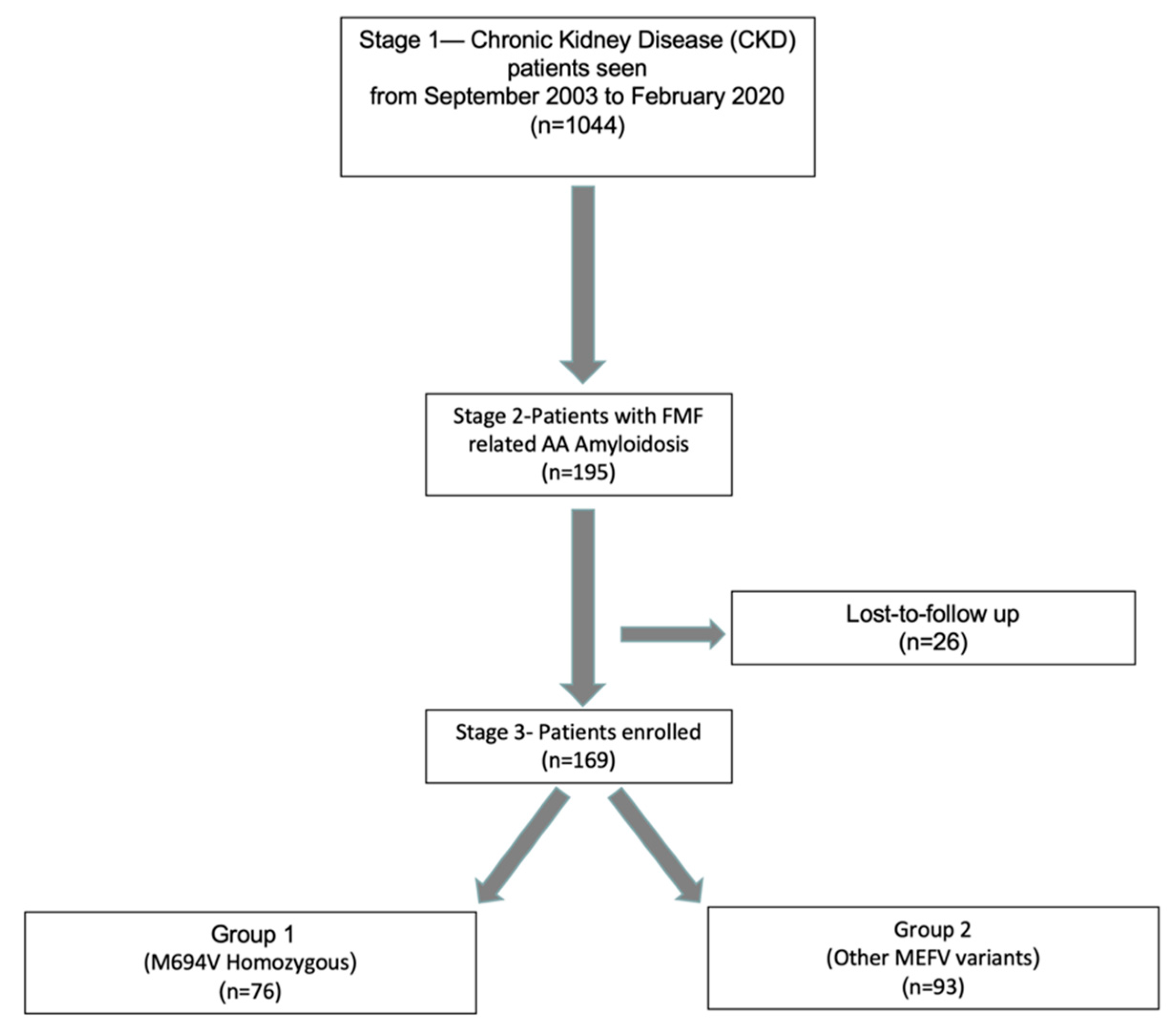
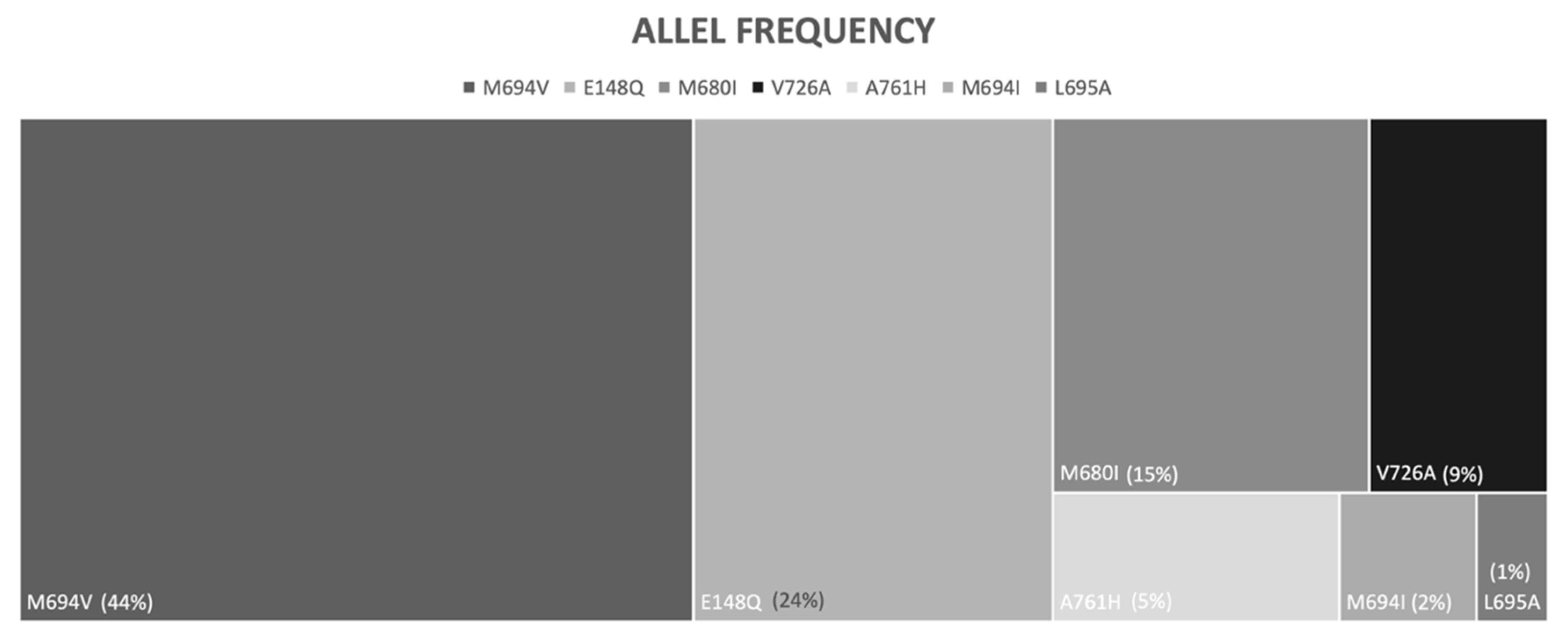
2. Materials and Methods
2.1. Study Design and Patients
2.2. Laboratory Measurements
2.3. Endothelial and Vascular Assessment
2.3.1. Flow-Mediated Dilatation (FMD)
2.3.2. Carotid Artery Intima-Media Thickness (cIMT)
2.3.3. Genetic Screening
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- El-Shanti, H.; Majeed, H.A.; El-Khateeb, M. Familial mediterranean fever in Arabs. Lancet 2006, 367, 1016–1024. [Google Scholar] [CrossRef]
- Papadopoulos, V.P.; Giaglis, S.; Mitroulis, I.; Ritis, K. The population genetics of familial mediterranean fever: A meta-analysis study. Ann. Hum. Genet. 2008, 72, 752–761. [Google Scholar] [CrossRef]
- Tunca, M.; Akar, S.; Onen, F.; Ozdogan, H.; Kasapcopur, O.; Yalcinkaya, F.; Tutar, E.; Ozen, S.; Topaloglu, R.; Yilmaz, E.; et al. Familial Mediterranean fever (FMF) in Turkey: Results of a nationwide multicenter study. Med. Baltim. 2005, 84, 1–11. [Google Scholar]
- Livneh, A.; Langevitz, P.; Zemer, D.; Zaks, N.; Kees, S.; Lidar, T.; Migdal, A.; Padeh, S.; Pras, M. Criteria for the diagnosis of familial mediterranean fever. Arthritis Rheum. 1997, 40, 1879–1885. [Google Scholar] [CrossRef]
- Polat, A.; Acikel, C.; Sozeri, B.; Dursun, I.; Kasapcopur, O.; Gulez, N.; Simsek, D.; Saldir, M.; Dokurel, I.; Poyrazoglu, H.; et al. Comparison of the efficacy of once- and twice-daily colchicine dosage in pediatric patients with familial Mediterranean fever—A randomized controlled noninferiority trial. Arthritis Res. Ther. 2016, 18, 85. [Google Scholar] [CrossRef] [Green Version]
- De Benedetti, F.; Gattorno, M.; Anton, J.; Ben-Chetrit, E.; Frenkel, J.; Hoffman, H.M.; Koné-Paut, I.; Lachmann, H.J.; Ozen, S.; Simon, A.; et al. Canakinumab for the Treatment of Autoinflammatory Recurrent Fever Syndromes. N. Engl. J. Med. 2018, 378, 1908–1919. [Google Scholar] [CrossRef] [Green Version]
- Gül, A.; Ozdogan, H.; Erer, B.; Ugurlu, S.; Kasapcopur, O.; Davis, N.; Sevgi, S. Efficacy and safety of canakinumab in adolescents and adults with colchicine-resistant familial Mediterranean fever. Arthritis Res. Ther. 2015, 17, 243. [Google Scholar] [CrossRef] [Green Version]
- Ozen, S.; Ben-Cherit, E.; Foeldvari, I.; Amarilyo, G.; Ozdogan, H.; Vanderschueren, S.; Marzan, K.; Kahlenberg, J.M.; Dekker, E.; De Benedetti, F.; et al. Long-term efficacy and safety of canakinumab in patients with colchicine-resistant familial Mediterranean fever: Results from the randomised phase III CLUSTER trial. Ann. Rheum. Dis. 2020, 79, 1362–1369. [Google Scholar] [CrossRef]
- Ozen, S.; Bilginer, Y.; Aktay Ayaz, N.; Calguneri, M. Anti-interleukin 1 treatment for patients with familial Mediterranean fever resistant to colchicine. J. Rheumatol. 2011, 38, 516–518. [Google Scholar] [CrossRef]
- Gershoni-Baruch, R.; Brik, R.; Zacks, N.; Shinawi, M.; Lidar, M.; Livneh, A. The contribution of genotypes at the MEFV and SAA1 loci to amyloidosis and disease severity in patients with familial Mediterranean fever. Arthritis Rheum. 2003, 48, 1149–1155. [Google Scholar] [CrossRef]
- Grimaldi, M.P.; Candore, G.; Vasto, S.; Caruso, M.; Caimi, G.; Hoffmann, E.; Colonna-Romano, G.; Lio, D.; Shinar, Y.; Franceschi, C.; et al. Role of the pyrin M694V (A2080G) allele in acute myocardial infarction and longevity: A study in the Sicilian population. J. Leukoc. Biol. 2006, 79, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Mansour, I.; Delague, V.; Cazeneuve, C.; Dodé, C.; Chouery, E.; Pêcheux, C.; Medlej-Hashim, M.; Salem, N.; El Zein, L.; Levan-Petit, I.; et al. Familial Mediterranean fever in Lebanon: Mutation spectrum, evidence for cases in Maronites, Greek orthodoxes, Greek catholics, Syriacs and Chiites and for an association between amyloidosis and M694V and M694I mutations. Eur. J. Hum. Genet. 2001, 9, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Stoler, I.; Freytag, J.; Orak, B.; Unterwalder, N.; Henning, S.; Heim, K.; von Bernuth, H.; Krüger, R.; Winkler, S.; Eschenhagen, P.; et al. Gene-Dose Effect of MEFV Gain-of-Function Mutations Determines ex vivo Neutrophil Activation in Familial Mediterranean Fever. Front. Immunol. 2020, 11, 716. [Google Scholar] [CrossRef]
- Ugurlu, S.; Ergezen, B.; Egeli, B.H.; Selvi, O.; Ozdogan, H. Safety and efficacy of anti-interleukin-1 treatment in 40 patients, followed in a single centre, with AA amyloidosis secondary to familial Mediterranean fever. Rheumatol. Oxf. 2020, 59, 3892–3899. [Google Scholar] [CrossRef] [PubMed]
- Twig, G.; Livneh, A.; Vivante, A.; Afek, A.; Shamiss, A.; Derazne, E.; Tzur, D.; Ben-Zvi, I.; Tirosh, A.; Barchana, M.; et al. Mortality risk factors associated with familial Mediterranean fever among a cohort of 1.25 million adolescents. Ann. Rheum. Dis. 2014, 73, 704–709. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [Green Version]
- Restivo, V.; Candiloro, S.; Daidone, M.; Norrito, R.; Cataldi, M.; Minutolo, G.; Caracci, F.; Fasano, S.; Ciccia, F.; Casuccio, A.; et al. Systematic review and meta-analysis of cardiovascular risk in rheumatological disease: Symptomatic and non-symptomatic events in rheumatoid arthritis and systemic lupus erythematosus. Autoimmun. Rev. 2021, 21, 102925. [Google Scholar] [CrossRef]
- Gendelman, O.; Shapira, R.; Tiosano, S.; Pras, E.; Comaneshter, D.; Cohen, A.; Amital, H. Familial Mediterranean fever is associated with increased risk for ischaemic heart disease and mortality–Perspective derived from a large database. Int. J. Clin. Pract. 2020, 74, e13473. [Google Scholar] [CrossRef]
- Langevitz, P.; Livneh, A.; Neumann, L.; Buskila, D.; Shemer, J.; Amolsky, D.; Pras, M. Prevalence of ischemic heart disease in patients with familial Mediterranean fever. Isr. Med. Assoc. J. 2001, 3, 9–12. [Google Scholar]
- Nidorf, S.M.; Thompson, P.L. Why Colchicine Should Be Considered for Secondary Prevention of Atherosclerosis: An Overview. Clin. Ther. 2019, 41, 41–48. [Google Scholar] [CrossRef] [Green Version]
- Greenland, P.; Alpert, J.S.; Beller, G.A.; Benjamin, E.J.; Budoff, M.J.; Fayad, Z.A.; Foster, E.; Hlatky, M.A.; Hodgson, J.M.; Kushner, F.G.; et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2010, 56, e50–e103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancia, G.; Fagard, R.; Narkiewicz, K.; Redon, J.; Zanchetti, A.; Böhm, M.; Christiaens, T.; Cifkova, R.; De Backer, G.; Dominiczak, A.; et al. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press. 2014, 23, 3–16. [Google Scholar] [CrossRef]
- Celermajer, D.S.; Sorensen, K.E.; Gooch, V.M.; Spiegelhalter, D.J.; Miller, O.I.; Sullivan, I.D.; Lloyd, J.K.; Deanfield, J.E. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992, 340, 1111–1115. [Google Scholar] [CrossRef]
- Atkov, O.Y.; Balahonova, T.V.; Pogorelova, O.A. Non-invasive ultrasound detection of endothelial dysfunction. Eur. J. Ultrasound 1992, 7, 37–45. [Google Scholar] [CrossRef]
- Ristagno, G.; Fumagalli, F.; Bottazzi, B.; Mantovani, A.; Olivari, D.; Novelli, D.; Latini, R. Pentraxin 3 in Cardiovascular Disease. Front. Immunol. 2019, 10, 823. [Google Scholar] [CrossRef] [PubMed]
- Batra, J.; Buttar, R.S.; Kaur, P.; Kreimerman, J.; Melamed, M.L. FGF-23 and cardiovascular disease: Review of literature. Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 423–429. [Google Scholar] [CrossRef]
- Jimbo, R.; Kawakami-Mori, F.; Mu, S.; Hirohama, D.; Majtan, B.; Shimizu, Y.; Yatomi, Y.; Fukumoto, S.; Fujita, T.; Shimosawa, T. Fibroblast growth factor 23 accelerates phosphate-induced vascular calcification in the absence of Klotho deficiency. Kidney Int. 2014, 85, 1103–1111. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, M.I.; Demirkaya, E.; Acikel, C.; Saldir, M.; Akar, S.; Cayci, T.; Saglam, M.; Unal, H.U.; Gok, M.; Polat, A.; et al. Endothelial function in patients with familial Mediterranean fever-related amyloidosis and association with cardiovascular events. Rheumatol. Oxf. 2014, 53, 2002–2008. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, M.I.; Sonmez, A.; Saglam, M.; Qureshi, A.R.; Carrero, J.J.; Caglar, K.; Eyileten, T.; Cakir, E.; Oguz, Y.; Vural, A.; et al. ADMA levels correlate with proteinuria, secondary amyloidosis, and endothelial dysfunction. J. Am. Soc. Nephrol. 2008, 19, 388–395. [Google Scholar] [CrossRef] [Green Version]
- Yilmaz, M.I.; Sonmez, A.; Saglam, M.; Yaman, H.; Kilic, S.; Demirkaya, E.; Eyileten, T.; Caglar, K.; Oguz, Y.; Vural, A.; et al. FGF-23 and vascular dysfunction in patients with stage 3 and 4 chronic kidney disease. Kidney Int. 2010, 78, 679–685. [Google Scholar] [CrossRef] [Green Version]
- Demirkaya, E.; Saglam, C.; Turker, T.; Koné-Paut, I.; Woo, P.; Doglio, M.; Amaryan, G.; Frenkel, J.; Uziel, Y.; Insalaco, A.; et al. Performance of Different Diagnostic Criteria for Familial Mediterranean Fever in Children with Periodic Fevers: Results from a Multicenter International Registry. J. Rheumatol. 2016, 43, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med. 1999, 130, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Corretti, M.C.; Anderson, T.J.; Benjamin, E.J.; Celermajer, D.; Charbonneau, F.; Creager, M.A.; Deanfield, J.; Drexler, H.; Gerhard-Herman, M.; Herrington, D.; et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 2002, 39, 257–265. [Google Scholar] [CrossRef] [Green Version]
- Arici, Z.S.; Romano, M.; Piskin, D.; Guzel, F.; Sahin, S.; Berard, R.A.; Yilmaz, M.I.; Demirkaya, E. Evaluation of E148Q and Concomitant AA Amyloidosis in Patients with Familial Mediterranean Fever. J. Clin. Med. 2021, 10, 3511. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.T.; Khalik, R.N.A.; Hoteit, R.M.; Sarieddine, D.S.; Charafeddine, K.M.; Cortas, N.K.; Mahfouz, R.A.R. The Use of a Reverse Hybridization Strip Assay for the Study of Hemochromatosis-Associated Gene Mutations in Lebanon. Genet. Test. Mol. Biomark. 2011, 15, 909–911. [Google Scholar] [CrossRef]
- Agca, R.; Heslinga, S.C.; van Halm, V.P.; Nurmohamed, M.T. Atherosclerotic cardiovascular disease in patients with chronic inflammatory joint disorders. Heart 2016, 102, 790–795. [Google Scholar] [CrossRef]
- Avina-Zubieta, J.A.; Thomas, J.; Sadatsafavi, M.; Lehman, A.J.; Lacaille, D. Risk of incident cardiovascular events in patients with rheumatoid arthritis: A meta-analysis of observational studies. Ann. Rheum. Dis. 2012, 71, 1524–1529. [Google Scholar] [CrossRef]
- Jamnitski, A.; Visman, I.M.; Peters, M.J.L.; Boers, M.; Dijkmans, B.A.C.; Nurmohamed, M.T. Prevalence of cardiovascular diseases in psoriatic arthritis resembles that of rheumatoid arthritis. Ann. Rheum. Dis. 2011, 70, 875–876. [Google Scholar] [CrossRef] [Green Version]
- Romano, M.; Piskin, D.; Berard, R.A.; Jackson, B.C.; Acikel, C.; Carrero, J.J.; Lachmann, H.J.; Yilmaz, M.I.; Demirkaya, E. Cardiovascular disease risk assessment in patients with familial Mediterranean fever related renal amyloidosis. Sci. Rep. 2020, 10, 18374. [Google Scholar] [CrossRef]
- Lachmann, H.J.; Goodman, H.J.B.; Gilbertson, J.A.; Gallimore, J.R.; Sabin, C.A.; Gillmore, J.D.; Hawkins, P.N. Natural History and Outcome in Systemic AA Amyloidosis. N. Engl. J. Med. 2007, 356, 2361–2371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papa, R.; Lachmann, H.J. Secondary, AA, Amyloidosis. Rheum. Dis. Clin. N. Am. 2018, 44, 585–603. [Google Scholar] [CrossRef] [PubMed]
- Sanai, T.; Nanishi, F.; Nagata, M.; Hirano, T.; Suematsu, E.; Esaki, Y.; Miyahara, H.; Iida, M. Role of amyloidosis in determining the prognosis of dialyzed patients with rheumatoid arthritis. Rheumatol. Int. 2007, 27, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Keles, N.; Caliskan, M.; Aksu, F.U.; Keles, N.N.; Karagoz, V.; Tekin, A.S.; Akcakoyun, M.; Kostek, O.; Elcioglu, O.; Aung, S.M.; et al. Retrobulbar blood flow and carotid intima-media thickness alteration may relate to subclinic atherosclerosis in patients with chronic inflammatory diseases. Ren. Fail. 2015, 37, 1164–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modesto, K.M.; Dispenzieri, A.; Gertz, M.; Cauduro, S.A.; Khandheria, B.K.; Seward, J.B.; Kyle, R.; Wood, C.M.; Bailey, K.R.; Tajik, A.J.; et al. Vascular abnormalities in primary amyloidosis. Eur. Heart J. 2007, 28, 1019–1024. [Google Scholar] [CrossRef] [Green Version]
- Akdogan, A.; Calguneri, M.; Yavuz, B.; Arslan, E.B.; Kalyoncu, U.; Sahiner, L.; Karadag, O.; Ertenli, I.; Kiraz, S.; Aytemir, K.; et al. Are familial Mediterranean fever (FMF) patients at increased risk for atherosclerosis? Impaired endothelial function and increased intima media thickness are found in FMF. J. Am. Coll. Cardiol. 2006, 48, 2351–2353. [Google Scholar] [CrossRef] [Green Version]
- Kosmeri, C.; Milionis, H.; Vlahos, A.P.; Benekos, T.; Bairaktari, E.; Cholevas, V.; Siomou, E. The impact of dyslipidemia on early markers of endothelial and renal dysfunction in children. J. Clin. Lipidol. 2020, 15, 292–300. [Google Scholar] [CrossRef]
- Barut, K.; Sahin, S.; Adrovic, A.; Sinoplu, A.B.; Yucel, G.; Pamuk, G.; Aydın, A.K.; Dasdemir, S.; Turanlı, E.T.; Buyru, N.; et al. Familial Mediterranean fever in childhood: A single-center experience. Rheumatol. Int. 2018, 38, 67–74. [Google Scholar] [CrossRef] [Green Version]
- Shohat, M.; Magal, N.; Shohat, T.; Chen, X.; Dagan, T.; Mimouni, A.; Danon, Y.; Lotan, R.; Ogur, G.; Sirin, A.; et al. Phenotype-genotype correlation in familial Mediterranean fever: Evidence for an association between Met694Val and amyloidosis. Eur. J. Hum. Genet. 1999, 7, 287–292. [Google Scholar] [CrossRef] [Green Version]
- Roitman, A.; Ben-Zvi, I.; Mendel, L.; Livneh, A. Inflammation and cardiovascular disease in familial Mediterranean fever. An analysis of hospital admissions for acute cardiovascular event. Clin. Exp. Rheumatol. 2018, 36, 80–85. [Google Scholar]
| Total (n = 169) | Group 1 (n = 76) | Group 2 (n = 93) | ||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean Difference [95% CI] | ||
| Age (years) | 34.9 ± 5.8 | 35.5 ± 6.3 | 34.5 ± 5.3 | 0.9 [(−0.8)–(2.7)] |
| Age at FMF diagnosis (years) | 15.5 ± 4.8 | 15.2 ± 4.7 | 15.8 ± 4.8 | −0.5 [(−2.1)–(0.8)] |
| Age at amyloidosis diagnosis (years) | 20.2 ± 2.8 | 20 ± 3.2 | 20 ± 2.5 | −0.03 [(−0.9)–(0.8)] |
| Follow-up duration (months) | 90 ± 8 | 88 ± 9 | 91 ± 7 | −3.1 [(−5.6)–(−0.6)] |
| n (%) | n (%) | p | ||
| Sex, male | 104 (61.5) | 50 (65.8) | 54 (58.1) | 0.30 |
| Family history of FMF | 56 (33.1) | 30 (39.5) | 26 (28.0) | 0.11 |
| Family history of amyloidosis | 41 (24.2) | 19 (25.0) | 22 (23.7) | 0.83 |
| Fever | 143 (84.6) | 65 (85.5) | 78 (83.9) | 0.76 |
| Abdominal pain | 121 (71.6) | 55 (72.4) | 66 (71.0) | 0.84 |
| Arthritis | 113 (66.9) | 58 (76.3) | 55 (59.1) | 0.018 |
| Chest pain | 101 (59.8) | 47 (61.8) | 54 (58.1) | 0.61 |
| Arthralgia | 81 (47.9) | 39 (51.3) | 42 (45.2) | 0.42 |
| Vomiting | 52 (30.8) | 26 (34.2) | 26 (28.0) | 0.38 |
| Myalgia/myositis | 46 (27.2) | 20 (26.3) | 26 (28.0) | 0.81 |
| Diarrhea | 32 (18.9) | 17 (22.4) | 15 (16.1) | 0.30 |
| Protracted febrile myalgia | 26 (15.4) | 10 (13.2) | 16 (17.2) | 0.46 |
| Fatigue | 22 (13.0) | 10 (13.2) | 12 (12.9) | 0.96 |
| Headache | 19 (11.2) | 7 (9.2) | 12 (12.9) | 0.45 |
| Erysipelas-like erythema | 10 (5.9) | 7 (9.2) | 3 (3.2) | 0.11 * |
| Treatment | ||||
| Colchicine | 169 (100%) | 76 (100%) | 93 (100%) | |
| Anakinra | 24 (14.2%) | 8 (10.5%) | 16 (17.2%) | 0.22 |
| Canakinumab | 25 (14.7%) | 9 (11.8%) | 16 (17.2%) | 0.33 |
| Group 1 (n = 76) | Group 2 (n = 93) | |||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean Difference [95% CI] | p | |
| SBP (mm/hg) | 130.9 ± 7.2 | 130.1 ± 7.6 | 0.84 [(−1.4)–(3.1)] | 0.46 |
| DBP (mm/hg) | 86.1 ± 3.6 | 86.8 ± 4.7 | −0.7 [(−1.9)–(0.6)] | 0.30 |
| BMI (kg/m2) | 26.6 ± 2.2 | 26.6 ± 2.6 | −0.04 [(−0.7)–(0.7)] | 0.99 |
| Cholesterol (mg/dL) | 269.6 ± 59.1 | 271.2 ± 48.2 | −1.6 [(−18.3)–(15)] | 0.85 |
| Triglyceride (mg/dL) | 186.3 ± 54.9 | 197.9 ± 46.9 | −11.7 [(−27.2)–(3.8)] | 0.14 |
| LDL (mg/dL) | 151.9 ± 31.1 | 152.0 ± 28.1 | −0.04 [(−9.1)–(8.9)] | 0.99 |
| HDL (mg/dL) | 44.9 ± 6.3 | 45.3 ± 6.9 | −0.4 [(−2.4)–(1.6)] | 0.72 |
| Glucose (mg/dL) | 80.1 ± 14.3 | 81.9 ± 15.5 | −1.8 [(−6.4)–(2.8)] | 0.44 |
| Insulin (μUI/mL) | 13.8 ± 6.3 | 13.8 ± 5.9 | −0.03 [(−1.9)–(1.8)] | 0.97 |
| HOMA | 2.7 ± 1.4 | 2.8 ± 1.3 | −0.03 [(−0.4)–(0.4)] | 0.86 |
| Ca (mg/dL) | 9.1 ± 0.8 | 8.7 ± 0.6 | 0.4 [(0.2)–(0.6)] | <0.001 |
| P (mg/dL) | 4.8 ± 1.1 | 4.5 ± 1.0 | 0.3 [(−0.001)–(0.6)] | 0.06 |
| PTH (pg/dL) | 63.4 ± 28.8 | 53.9 ± 21.2 | 9.5 [(1.6)–(17.3)] | 0.02 |
| 25OHVitD (nmol/dL) | 48.9 ± 12.9 | 49.9 ± 11.8 | −1.02 [(−4.8)–(2.7)] | 0.59 |
| Albumin (g/dL) | 3.4 ± 0.7 | 3.4 ± 0.7 | −0.002 [(−0.2)–(0.2)] | 0.98 |
| GFR (mL/min/1.73 m2) | 89.9 ± 7.2 | 90.0 ± 6.8 | −0.1 [(−2.2)–(2.0)] | 0.92 |
| hsCRP (mg/dL) | 21.3 ± 12.0 | 20.0 ± 12.6 | 1.3 [(−2.5)–(5.0)] | 0.51 |
| Group 1 (n = 76) | Group 2 (n = 93) | |||
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean Difference [95% CI] | p | |
| Proteinuria (g/24 h) | 7966.3 ± 3526.4 | 4895.4 ± 1184.8 | 3070.9 [2230.9–3910.9] | <0.001 |
| FMD (%) | 5.85 ± 1.03 | 6.46 ± 0.83 | −0.6 [(−0.89)–(−0.31)] | <0.001 |
| cIMT | 0.79 ± 0.15 | 0.67 ± 0.12 | 0.12 [0.08–0.16] | <0.001 |
| FGF23 (pg/dL) | 55.9 ± 26.2 | 43.2 ± 16.3 | 12.8 [5.9–19.6] | <0.001 |
| PTX3 | 19.4 ± 17.6 | 6.1 ± 7.9 | 13.3 [8.9–17.5] | <0.001 |
| FMD | cIMT | FGF23 | PTX3 | Proteinuria | |||
|---|---|---|---|---|---|---|---|
| Group 1 | cIMT | r | −0.439 | ||||
| p | 0.000 | ||||||
| FGF23 | r | −0.476 | 0.404 | ||||
| p | 0.000 | 0.000 | |||||
| PTX3 | r | −0.482 | 0.614 | 0.455 | |||
| p | 0.000 | 0.000 | 0.000 | ||||
| Proteinuria | r | −0.618 | 0.519 | 0.596 | 0.613 | ||
| p | 0.000 | 0.000 | 0.000 | 0.000 | |||
| hsCRP | r | −0.269 | 0.205 | 0.395 | 0.090 | 0.360 | |
| p | 0.019 | 0.075 | 0.000 | 0.437 | 0.001 | ||
| FMD | cIMT | FGF23 | PTX3 | Proteinuria | |||
| Group 2 | cIMT | r | 0.099 | ||||
| p | 0.346 | ||||||
| FGF23 | r | −0.313 | 0.215 | ||||
| p | 0.002 | 0.039 | |||||
| PTX3 | r | −0.128 | 0.432 | 0.329 | |||
| p | 0.220 | 0.000 | 0.001 | ||||
| Proteinuria | r | −0.460 | −0.046 | 0.192 | −0.070 | ||
| p | 0.000 | 0.663 | 0.066 | 0.504 | |||
| hsCRP | r | −0.124 | 0.185 | 0.379 | 0.248 | −0.002 | |
| p | 0.237 | 0.076 | 0.000 | 0.000 | 0.986 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sahin, S.; Romano, M.; Guzel, F.; Piskin, D.; Poddighe, D.; Sezer, S.; Kasapcopur, O.; Appleton, C.T.; Yilmaz, I.; Demirkaya, E. Assessment of Surrogate Markers for Cardiovascular Disease in Familial Mediterranean Fever-Related Amyloidosis Patients Homozygous for M694V Mutation in MEFV Gene. Life 2022, 12, 631. https://doi.org/10.3390/life12050631
Sahin S, Romano M, Guzel F, Piskin D, Poddighe D, Sezer S, Kasapcopur O, Appleton CT, Yilmaz I, Demirkaya E. Assessment of Surrogate Markers for Cardiovascular Disease in Familial Mediterranean Fever-Related Amyloidosis Patients Homozygous for M694V Mutation in MEFV Gene. Life. 2022; 12(5):631. https://doi.org/10.3390/life12050631
Chicago/Turabian StyleSahin, Sezgin, Micol Romano, Ferhat Guzel, David Piskin, Dimitri Poddighe, Siren Sezer, Ozgur Kasapcopur, C. Thomas Appleton, Ilker Yilmaz, and Erkan Demirkaya. 2022. "Assessment of Surrogate Markers for Cardiovascular Disease in Familial Mediterranean Fever-Related Amyloidosis Patients Homozygous for M694V Mutation in MEFV Gene" Life 12, no. 5: 631. https://doi.org/10.3390/life12050631
APA StyleSahin, S., Romano, M., Guzel, F., Piskin, D., Poddighe, D., Sezer, S., Kasapcopur, O., Appleton, C. T., Yilmaz, I., & Demirkaya, E. (2022). Assessment of Surrogate Markers for Cardiovascular Disease in Familial Mediterranean Fever-Related Amyloidosis Patients Homozygous for M694V Mutation in MEFV Gene. Life, 12(5), 631. https://doi.org/10.3390/life12050631







