Post-COVID-19 Condition: Where Are We Now?
Abstract
:1. Introduction
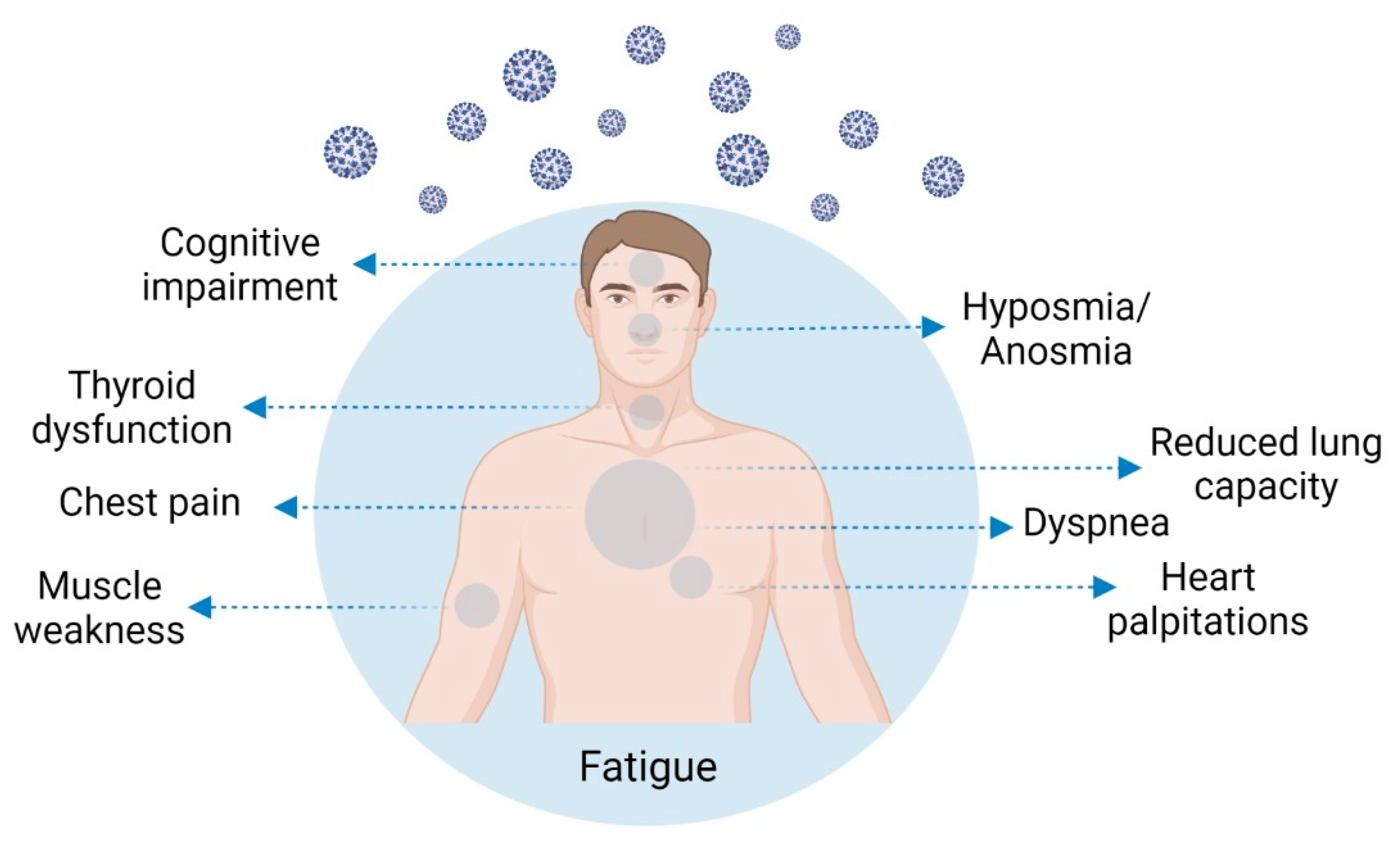
2. Post-COVID-19 Condition Symptomatology and Prevalence
3. Post-COVID-19 Condition Risk Factors
4. Post-COVID-19 Condition Pathophysiology
5. Thyroid Involvement in COVID-19
6. Post-COVID-19 Condition Health Burden and Patient Management
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sancak, B.; Kilic, C. A Psychiatrist’s Own Experience of Long COVID: Looking beyond the Psychosomatic Perspective. Psychiatr. Danub. 2021, 33, 250. [Google Scholar]
- Pan, Y.; Yu, Z.; Yuan, Y.; Han, J.; Wang, Z.; Chen, H.; Wang, S.; Wang, Z.; Hu, H.; Zhou, L. Alteration of Autonomic Nervous System Is Associated with Severity and Outcomes in Patients with COVID-19. Front. Physiol. 2021, 12, 630038. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef] [PubMed]
- Shuwa, H.A.; Shaw, T.N.; Knight, S.B.; Wemyss, K.; McClure, F.A.; Pearmain, L.; Prise, I.; Jagger, C.; Morgan, D.J.; Khan, S.; et al. Alterations in T and B cell function persist in convalescent COVID-19 patients. Med 2021, 2, 720–735.e4. [Google Scholar] [CrossRef]
- Marshall, M. The four most urgent questions about long COVID. Nature 2021, 594, 168–170. [Google Scholar] [CrossRef]
- Sykes, D.L.; Holdsworth, L.; Jawad, N.; Gunasekera, P.; Morice, A.H.; Crooks, M.G. Post-COVID-19 Symptom Burden: What is Long-COVID and How Should We Manage It? Lung 2021, 199, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Q.; Xu, M.; Li, J.; Liu, Y.; Zhang, J.; Xu, Y.; Dong, W. Clinical sequelae of COVID-19 survivors in Wuhan, China: A single-centre longitudinal study. Clin. Microbiol. Infect. 2021, 27, 89–95. [Google Scholar] [CrossRef]
- Dani, M.; Dirksen, A.; Taraborrelli, P.; Torocastro, M.; Panagopoulos, D.; Sutton, R.; Lim, P.B. Autonomic dysfunction in ‘long COVID’: Rationale, physiology and management strategies. Clin. Med. 2021, 21, e63–e67. [Google Scholar] [CrossRef]
- Mehandru, S.; Merad, M. Pathological sequelae of long-haul COVID. Nat. Immunol. 2022, 23, 194–202. [Google Scholar] [CrossRef] [PubMed]
- WHO. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed on 3 March 2022).
- Shouman, K.; Vanichkachorn, G.; Cheshire, W.P.; Suarez, M.D.; Shelly, S.; Lamotte, G.J.; Sandroni, P.; Benarroch, E.E.; Berini, S.E.; Cutsforth-Gregory, J.K.; et al. Autonomic dysfunction following COVID-19 infection: An early experience. Clin. Auton. Res. 2021, 31, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.J. Persistent SARS-2 infections contribute to long COVID-19. Med. Hypotheses 2021, 149, 110538. [Google Scholar] [CrossRef]
- Brodin, P. Immune determinants of COVID-19 disease presentation and severity. Nat. Med. 2021, 27, 28–33. [Google Scholar] [CrossRef]
- Ortona, E.; Buonsenso, D.; Carfi, A.; Malorni, W. Long Covid Kids study g. Long COVID: An estrogen-associated autoimmune disease? Cell Death Discov. 2021, 7, 77. [Google Scholar] [CrossRef]
- Amenta, E.M.; Spallone, A.; Rodriguez-Barradas, M.C.; El Sahly, H.M.; Atmar, R.L.; Kulkarni, P.A. Postacute COVID-19: An Overview and Approach to Classification. Open Forum Infect. Dis. 2020, 7, ofaa509. [Google Scholar] [CrossRef] [PubMed]
- Cabrera Martimbianco, A.L.; Pacheco, R.L.; Bagattini, A.M.; Riera, R. Frequency, signs and symptoms, and criteria adopted for long COVID-19: A systematic review. Int. J. Clin. Pract. 2021, 75, e14357. [Google Scholar] [CrossRef] [PubMed]
- Yong, S.J. Persistent Brainstem Dysfunction in Long-COVID: A Hypothesis. ACS Chem. Neurosci. 2021, 12, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Raveendran, A.V.; Jayadevan, R.; Sashidharan, S. Long COVID: An overview. Diabetes Metab. Syndr. 2021, 15, 869–875. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Logue, J.K.; Franko, N.M.; McCulloch, D.J.; McDonald, D.; Magedson, A.; Wolf, C.R.; Chu, H.Y. Sequelae in Adults at 6 Months After COVID-19 Infection. JAMA Netw. Open 2021, 4, e210830. [Google Scholar] [CrossRef] [PubMed]
- Ramakrishnan, R.K.; Kashour, T.; Hamid, Q.; Halwani, R.; Tleyjeh, I.M. Unraveling the Mystery Surrounding Post-Acute Sequelae of COVID-19. Front. Immunol. 2021, 12, 686029. [Google Scholar] [CrossRef]
- Sette, A.; Crotty, S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell 2021, 184, 861–880. [Google Scholar] [CrossRef]
- Guedj, E.; Campion, J.Y.; Dudouet, P.; Kaphan, E.; Bregeon, F.; Tissot-Dupont, H.; Guis, S.; Barthelemy, F.; Habert, P.; Ceccaldi, M.; et al. 18F-FDG brain PET hypometabolism in patients with long COVID. Eur. J. Pediatr. 2021, 48, 2823–2833. [Google Scholar] [CrossRef]
- Naeije, R.; Caravita, S. Phenotyping long COVID. Eur. Respir. J. 2021, 58, 2101763. [Google Scholar] [CrossRef]
- Moreno-Pérez, O.; Merino, E.; Leon-Ramirez, J.-M.; Andres, M.; Ramos, J.M.; Arenas-Jiménez, J.; Asensio, S.; Sanchez, R.; Ruiz-Torregrosa, P.; Galan, I.; et al. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J. Infect. 2021, 82, 378–383. [Google Scholar] [CrossRef]
- Townsend, L.; Dowds, J.; O’Brien, K.; Sheill, G.; Dyer, A.H.; O’Kelly, B.; Hynes, J.P.; Mooney, A.; Dunne, J.; Ni Cheallaigh, C.; et al. Persistent Poor Health after COVID-19 Is Not Associated with Respiratory Complications or Initial Disease Severity. Ann. Am. Thorac. Soc. 2021, 18, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Gaber, T.A.-Z.K.; Ashish, A.; Unsworth, A. Persistent post-covid symptoms in healthcare workers. Occup. Med. 2021, 71, 144–146. [Google Scholar] [CrossRef]
- Seessle, J.; Waterboer, T.; Hippchen, T.; Simon, J.; Kirchner, M.; Lim, A.; Müller, B.; Merle, U. Persistent symptoms in adult patients one year after COVID-19: A prospective cohort study. Clin. Infect. Dis. 2021, ciab611. [Google Scholar] [CrossRef]
- Mondelli, V.; Pariante, C.M. What can neuroimmunology teach us about the symptoms of long-COVID? Oxf. Open Immunol. 2021, 2, iqab004. [Google Scholar] [CrossRef]
- Stephenson, T.; Pereira, S.M.P.; Shafran, R.; de Stavola, B.L.; Rojas, N.; McOwat, K.; Simmons, R.; Zavala, M.; O’Mahoney, L.; Chalder, T.; et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): A national matched cohort study. Lancet Child Adolesc. Health 2022, 6, 230–239. [Google Scholar] [CrossRef]
- Becker, R.C. Autonomic dysfunction in SARS-CoV-2 infection acute and long-term implications COVID-19 editor’s page series. J. Thromb. Thrombolysis 2021, 52, 692–707. [Google Scholar] [CrossRef] [PubMed]
- Torres-Castro, R.; Vasconcello-Castillo, L.; Alsina-Restoy, X.; Solis-Navarro, L.; Burgos, F.; Puppo, H.; Vilaró, J. Respiratory function in patients post-infection by COVID-19: A systematic review and meta-analysis. Pulmonology 2021, 27, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Bansal, R.; Gubbi, S.; Koch, C.A. COVID-19 and chronic fatigue syndrome: An endocrine perspective. J. Clin. Transl. Endocrinol. 2022, 27, 100284. [Google Scholar] [CrossRef]
- Peghin, M.; Palese, A.; Venturini, M.; De Martino, M.; Gerussi, V.; Graziano, E.; Bontempo, G.; Marrella, F.; Tommasini, A.; Fabris, M.; et al. Post-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin. Microbiol. Infect. 2021, 27, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Kashif, A.; Chaudhry, M.; Fayyaz, T.; Abdullah, M.; Malik, A.; Anwer, J.M.A.; Inam, S.H.A.; Fatima, T.; Iqbal, N.; Shoaib, K. Follow-up of COVID-19 recovered patients with mild disease. Sci. Rep. 2021, 11, 13414. [Google Scholar] [CrossRef]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Mandal, S.; Barnett, J.; Brill, S.E.; Brown, J.S.; Denneny, E.K.; Hare, S.S.; Heightman, M.; Hillman, T.E.; Jacob, J.; Jarvis, H.C.; et al. ‘Long-COVID’: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax 2021, 76, 396–398. [Google Scholar] [CrossRef]
- Kamal, M.; Abo Omirah, M.; Hussein, A.; Saeed, H. Assessment and characterisation of post-COVID-19 manifestations. Int. J. Clin. Pract. 2021, 75, e13746. [Google Scholar] [CrossRef]
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600. [Google Scholar] [CrossRef]
- Taquet, M.; Geddes, J.R.; Husain, M.; Luciano, S.; Harrison, P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. Lancet Psychiatry 2021, 8, 416–427. [Google Scholar] [CrossRef]
- Wildwing, T.; Holt, N. The neurological symptoms of COVID-19: A systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services. Ther. Adv. Chronic Dis. 2021, 12. [Google Scholar] [CrossRef]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’Em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. eClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Alkodaymi, M.S.; Omrani, O.A.; Fawzy, N.A.; Shaar, B.A.; Almamlouk, R.; Riaz, M.; Obeidat, M.; Obeidat, Y.; Gerberi, D.; Taha, R.M.; et al. Prevalence of post-acute COVID-19 syndrome symptoms at different follow-up periods: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022. [Google Scholar] [CrossRef]
- Duggal, P.; Penson, T.; Manley, H.N.; Vergara, C.; Munday, R.M.; Duchen, D.; Linton, E.A.; Zurn, A.; Kerulz, J.C.; Mehta, S.H.; et al. Post-sequelae symptoms and comorbidities after COVID-19. J. Med. Virol. 2022, 94, 2060–2066. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Abellan, J.; Padilla, S.; Fernandez-Gonzalez, M.; Garcia, J.A.; Agullo, V.; Andreo, M.; Ruiz, S.; Galiana, A.; Gutiérrez, F.; Masiá, M. Antibody Response to SARS-CoV-2 is Associated with Long-term Clinical Outcome in Patients with COVID-19: A Longitudinal Study. J. Clin. Immunol. 2021, 41, 1490–1501. [Google Scholar] [CrossRef]
- Iqbal, F.M.; Lam, K.; Sounderajah, V.; Clarke, J.M.; Ashrafian, H.; Darzi, A. Characteristics and predictors of acute and chronic post-COVID syndrome: A systematic review and meta-analysis. eClinicalMedicine 2021, 36, 100899. [Google Scholar] [CrossRef] [PubMed]
- Cortinovis, M.; Perico, N.; Remuzzi, G. Long-term follow-up of recovered patients with COVID-19. Lancet 2021, 397, 173–175. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-Las-Penas, C.; Pellicer-Valero, O.J.; Navarro-Pardo, E.; Palacios-Cena, D.; Florencio, L.L.; Guijarro, C.; Martín-Guerrero, J.D. Symptoms Experienced at the Acute Phase of SARS-CoV-2 Infection as Risk Factor of Long-term Post-COVID Symptoms: The LONG-COVID-EXP-CM Multicenter Study. Int. J. Infect. Dis. 2022, 116, 241–244. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Cuadrado, M.; Florencio, L. Defining Post-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Post-COVID): An Integrative Classification. Int. J. Environ. Res. Public Health 2021, 18, 2621. [Google Scholar] [CrossRef] [PubMed]
- Glynne, P.; Tahmasebi, N.; Gant, V.; Gupta, R. Long COVID following mild SARS-CoV-2 infection: Characteristic T cell alterations and response to antihistamines. J. Investig. Med. 2022, 70, 61–67. [Google Scholar] [CrossRef]
- Iyengar, K.P.; Jain, V.K.; Vaishya, R.; Ish, P. Long COVID-19: An emerging pandemic in itself. Adv. Respir. Med. 2021, 89, 234–236. [Google Scholar] [CrossRef]
- Khunti, K.; Davies, M.J.; Kosiborod, M.N.; Nauck, M.A. Long COVID—metabolic risk factors and novel therapeutic management. Nat. Rev. Endocrinol. 2021, 17, 379–380. [Google Scholar] [CrossRef] [PubMed]
- Fainardi, V.; Meoli, A.; Chiopris, G.; Motta, M.; Skenderaj, K.; Grandinetti, R.; Bergomi, A.; Antodaro, F.; Zona, S.; Esposito, S. Long COVID in Children and Adolescents. Life 2022, 12, 285. [Google Scholar] [CrossRef]
- Borch, L.; Holm, M.; Knudsen, M.; Ellermann-Eriksen, S.; Hagstroem, S. Long COVID symptoms and duration in SARS-CoV-2 positive children—A nationwide cohort study. Eur. J. Pediatr. 2022, 1–11. [Google Scholar] [CrossRef]
- Yelin, D.; Margalit, I.; Yahav, D.; Runold, M.; Bruchfeld, J. Long COVID-19-it’s not over until? Clin. Microbiol. Infect. 2021, 27, 506–508. [Google Scholar] [CrossRef]
- Karlsson, A.C.; Humbert, M.; Buggert, M. The known unknowns of T cell immunity to COVID-19. Sci. Immunol. 2020, 5, eabe8063. [Google Scholar] [CrossRef]
- Doykov, I.; Hallqvist, J.; Gilmour, K.C.; Grandjean, L.; Mills, K.; Heywood, W.E. ‘The long tail of COVID-19’—The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Research 2020, 9, 1349. [Google Scholar] [CrossRef] [PubMed]
- Pasrija, R.; Naime, M. The deregulated immune reaction and cytokines release storm (CRS) in COVID-19 disease. Int. Immunopharmacol. 2021, 90, 107225. [Google Scholar] [CrossRef]
- Kappelmann, N.; Dantzer, R.; Khandaker, G.M. Interleukin-6 as potential mediator of long-term neuropsychiatric symptoms of COVID-19. Psychoneuroendocrinology 2021, 131, 105295. [Google Scholar] [CrossRef] [PubMed]
- Iadecola, C.; Anrather, J.; Kamel, H. Effects of COVID-19 on the Nervous System. Cell 2020, 183, 16–27.e1. [Google Scholar] [CrossRef] [PubMed]
- McFarland, A.J.; Yousuf, M.S.; Shiers, S.; Price, T.J. Neurobiology of SARS-CoV-2 interactions with the peripheral nervous system: Implications for COVID-19 and pain. Pain Rep. 2021, 6, e885. [Google Scholar] [CrossRef]
- Eroğlu, I.; Eroğlu, B.; Güven, G.S. Altered tryptophan absorption and metabolism could underlie long-term symptoms in survivors of coronavirus disease 2019 (COVID-19). Nutrition 2021, 90, 111308. [Google Scholar] [CrossRef] [PubMed]
- Barizien, N.; Le Guen, M.; Russel, S.; Touche, P.; Huang, F.; Vallée, A. Clinical characterization of dysautonomia in long COVID-19 patients. Sci. Rep. 2021, 11, 14042. [Google Scholar] [CrossRef]
- Blitshteyn, S.; Whitelaw, S. Correction to: Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: A case series of 20 patients. Immunol Res. 2021, 69, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Townsend, L.; Moloney, D.; Finucane, C.; McCarthy, K.; Bergin, C.; Bannan, C.; Kenny, R.-A. Fatigue following COVID-19 infection is not associated with autonomic dysfunction. PLoS ONE 2021, 16, e0247280. [Google Scholar] [CrossRef]
- Becker, R.C. Anticipating the long-term cardiovascular effects of COVID-19. J. Thromb. Thrombolysis 2020, 50, 512–524. [Google Scholar] [CrossRef] [PubMed]
- Fan, B.E.; Umapathi, T.; Chua, K.; Chia, Y.W.; Wong, S.W.; Tan, G.W.L.; Chandrasekar, S.; Lum, Y.H.; Vasoo, S.; Dalan, R. Delayed catastrophic thrombotic events in young and asymptomatic post COVID-19 patients. J. Thromb. Thrombolysis 2021, 51, 971–977. [Google Scholar] [CrossRef]
- Campi, I.; Bulgarelli, I.; Dubini, A.; Perego, G.B.; Tortorici, E.; Torlasco, C.; Torresani, E.; Rocco, L.; Persani, L.; Fugazzola, L. The spectrum of thyroid function tests during hospitalization for SARS-CoV-2 infection. Eur. J. Endocrinol. 2021, 184, 699–709. [Google Scholar] [CrossRef]
- Scappaticcio, L.; Pitoia, F.; Esposito, K.; Piccardo, A.; Trimboli, P. Impact of COVID-19 on the thyroid gland: An update. Rev. Endocr. Metab. Disord. 2020, 22, 803–815. [Google Scholar] [CrossRef]
- Coperchini, F.; Ricci, G.; Croce, L.; Denegri, M.; Ruggiero, R.; Villani, L.; Magri, F.; Chiovato, L.; Rotondi, M. Modulation of ACE-2 mRNA by inflammatory cytokines in human thyroid cells: A pilot study. Endocrine 2021, 74, 638–645. [Google Scholar] [CrossRef]
- Ruggeri, R.M.; Campennì, A.; Deandreis, D.; Siracusa, M.; Tozzoli, R.; Ovčariček, P.P.; Giovanella, L. SARS-CoV-2-related immune-inflammatory thyroid disorders: Facts and perspectives. Expert Rev. Clin. Immunol. 2021, 17, 737–759. [Google Scholar] [CrossRef] [PubMed]
- Puig-Domingo, M.; Marazuela, M.; Yildiz, B.O.; Giustina, A. COVID-19 and endocrine and metabolic diseases. An updated statement from the European Society of Endocrinology. Endocrine 2021, 72, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Tian, Y.; Li, Z.; Zhu, J.; Wei, T.; Lei, J. Potential Interaction Between SARS-CoV-2 and Thyroid: A Review. Endocrinology 2021, 162, bqab004. [Google Scholar] [CrossRef]
- Aemaz, U.; Rehman, M.; Farooq, H.; Ali, M.M.; Ebaad, U.; Rehman, M.; Dar, Q.A.; Hussain, A. The Association of Subacute Thyroiditis with COVID-19: A Systematic Review. SN Compr. Clin. Med. 2021, 3, 1515–1527. [Google Scholar] [CrossRef] [PubMed]
- Inaba, H.; Aizawa, T. Coronavirus Disease 2019 and the Thyroid—Progress and Perspectives. Front. Endocrinol. 2021, 12, 708333. [Google Scholar] [CrossRef]
- Gorini, F.; Bianchi, F.; Iervasi, G. COVID-19 and Thyroid: Progress and Prospects. Int. J. Environ. Res. Public Health 2020, 17, 6630. [Google Scholar] [CrossRef]
- Croce, L.; Gangemi, D.; Ancona, G.; Liboà, F.; Bendotti, G.; Minelli, L.; Chiovato, L. The cytokine storm and thyroid hormone changes in COVID-19. J. Endocrinol. Investig. 2021, 44, 891–904. [Google Scholar] [CrossRef] [PubMed]
- Das, L.; Dutta, P.; Walia, R.; Mukherjee, S.; Suri, V.; Puri, G.D.; Mahajan, V.; Malhotra, P.; Chaudhary, S.; Gupta, R.; et al. Spectrum of Endocrine Dysfunction and Association With Disease Severity in Patients With COVID-19: Insights From a Cross-Sectional, Observational Study. Front. Endocrinol. 2021, 12, 645787. [Google Scholar] [CrossRef]
- Lui, D.T.W.; Lee, C.H.; Chow, W.S.; Lee, A.C.H.; Tam, A.R.; Pang, P.; Ho, T.Y.; Fong, C.H.Y.; LAw, C.Y.; Leung, E.K.H.; et al. Long COVID in Patients With Mild to Moderate Disease: Do Thyroid Function and Autoimmunity Play a Role? Endocr. Pract. 2021, 27, 894–902. [Google Scholar] [CrossRef]
- Murugan, A.K.; Alzahrani, A.S. SARS-CoV-2: Emerging Role in the Pathogenesis of Various Thyroid Diseases. J. Inflamm. Res. 2021, 14, 6191–6221. [Google Scholar] [CrossRef]
- Clarke, S.A.; Phylactou, M.; Patel, B.; Mills, E.G.; Muzi, B.; Izzi-Engbeaya, C.; Choudhury, S.; Khoo, B.; Meeran, K.; Comninos, A.N.; et al. Normal Adrenal and Thyroid Function in Patients Who Survive COVID-19 Infection. J. Clin. Endocrinol. Metab. 2021, 106, 2208–2220. [Google Scholar] [CrossRef]
- Lania, A.; Sandri, M.T.; Cellini, M.; Mirani, M.; Lavezzi, E.; Mazziotti, G. Thyrotoxicosis in Patients with COVID-19: The Thyrcov Study. Eur. J. Endocrinol. 2020, 183, 381–387. [Google Scholar] [CrossRef]
- Pizzocaro, A.; Colombo, P.; Vena, W.; Ariano, S.; Magnoni, P.; Reggiani, F.; Favacchio, G.; Mirani, M.; Lavezzi, E.; Voza, A.; et al. Outcome of SARS-CoV-2-related thyrotoxicosis in survivors of COVID-19: A prospective study. Endocrine 2021, 73, 255–260. [Google Scholar] [CrossRef]
- Sandru, F.; Carsote, M.; Petca, R.C.; Gheorghisan-Galateanu, A.A.; Petca, A.; Valea, A.; Dumitrașcu, M.C. COVID-19-related thyroid conditions (Review). Exp. Ther. Med. 2021, 22, 756. [Google Scholar] [CrossRef]
- Dworakowska, D.; Morley, S.; Mulholland, N.; Grossman, A.B. COVID-19-related thyroiditis: A novel disease entity? Clin. Endocrinol. 2021, 95, 369–377. [Google Scholar] [CrossRef] [PubMed]
- Bellastella, G.; Maiorino, M.I.; Esposito, K. Endocrine complications of COVID-19: What happens to the thyroid and adrenal glands? J. Endocrinol. Investig. 2020, 43, 1169–1170. [Google Scholar] [CrossRef]
- Christensen, J.; O’Callaghan, K.; Sinclair, H.; Hawke, K.; Love, A.; Hajkowicz, K.; Stewart, A.G. Risk factors, Treatment and Outcomes of Subacute Thyroiditis Secondary to COVID-19: A Systematic Review. Intern. Med. J. 2021. [Google Scholar] [CrossRef] [PubMed]
- Trimboli, P.; Cappelli, C.; Croce, L.; Scappaticcio, L.; Chiovato, L.; Rotondi, M. COVID-19-Associated Subacute Thyroiditis: Evidence-Based Data From a Systematic Review. Front. Endocrinol. 2021, 12, 707726. [Google Scholar] [CrossRef] [PubMed]
- Lui, D.T.W.; Lee, C.H.; Chow, W.S.; Lee, A.C.H.; Tam, A.R.; Fong, C.H.Y.; Law, C.Y.; Leung, E.K.H.; To, K.K.W.; Tan, K.C.B.; et al. Thyroid Dysfunction in Relation to Immune Profile, Disease Status, and Outcome in 191 Patients with COVID-19. J. Clin. Endocrinol. Metab. 2021, 106, e926–e935. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, Y.; Percik, R.; Oberman, B.; Yaffe, D.; Zimlichman, E.; Tirosh, A. Sick Euthyroid Syndrome on Presentation of Patients With COVID-19: A Potential Marker for Disease Severity. Endocr. Pr. 2021, 27, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Güven, M.; Gültekin, H. The prognostic impact of thyroid disorders on the clinical severity of COVID-19: Results of single-centre pandemic hospital. Int. J. Clin. Pr. 2021, 75, e14129. [Google Scholar] [CrossRef]
- Beltrão, F.E.d.L.; Beltrão, D.C.d.A.; Carvalhal, G.; Beltrão, M.F.E.d.L.; Brito, M.A.d.S.; Capistrano, M.K.H.R.; Bastos, I.H.D.A.; Hecht, F.; Daltro, C.H.D.C.; Bianco, A.C.; et al. Thyroid Hormone Levels During Hospital Admission Inform Disease Severity and Mortality in COVID-19 Patients. Thyroid 2021, 31, 1639–1649. [Google Scholar] [CrossRef]
- Asghar, M.S.; Yasmin, F.; Dapke, K.; Phadke, R.; Shah, S.M.I.; Bin Zafar, M.D. Derangements of biochemical markers and thyroid function analysis among COVID-19-positive patients: A developing country single-center experience. J. Med. Virol. 2021, 93, 5712–5717. [Google Scholar] [CrossRef]
- Gong, J.; Wang, D.-K.; Dong, H.; Xia, Q.-S.; Huang, Z.-Y.; Zhao, Y.; Chen, X.; Yuan, F.; Li, J.-B.; Lu, F.-E. Prognostic significance of low TSH concentration in patients with COVID-19 presenting with non-thyroidal illness syndrome. BMC Endocr. Disord. 2021, 21, 111. [Google Scholar] [CrossRef] [PubMed]
- Zou, R.; Wu, C.; Zhang, S.; Wang, G.; Zhang, Q.; Yu, B.; Wu, Y.; Dong, H.; Wu, G.; Wu, S.; et al. Euthyroid Sick Syndrome in Patients With COVID-Front. Endocrinol. 2020, 11, 566439. [Google Scholar] [CrossRef]
- Giovanella, L.; Ruggeri, R.M.; Ovčariček, P.P.; Campenni, A.; Treglia, G.; Deandreis, D. Prevalence of thyroid dysfunction in patients with COVID-19: A systematic review. Clin. Transl. Imaging 2021, 9, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Duntas, L.H.; Jonklaas, J. COVID-19 and Thyroid Diseases: A Bidirectional Impact. J. Endocr. Soc. 2021, 5, bvab076. [Google Scholar] [CrossRef] [PubMed]
- Anaya, J.-M.; Monsalve, D.M.; Rojas, M.; Rodríguez, Y.; Montoya-García, N.; Mancera-Navarro, L.M.; Villadiego-Santana, A.M.; Rodríguez-Leguizamón, G.; Acosta-Ampudia, Y.; Ramírez-Santana, C. Latent rheumatic, thyroid and phospholipid autoimmunity in hospitalized patients with COVID-19. J. Transl. Autoimmun. 2021, 4, 100091. [Google Scholar] [CrossRef] [PubMed]
- Pal, R.; Banerjee, M. COVID-19 and the endocrine system: Exploring the unexplored. J. Endocrinol. Investig. 2020, 43, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Poma, A.M.; Bonuccelli, D.; Giannini, R.; Macerola, E.; Vignali, P.; Ugolini, C.; Torregrossa, L.; Proietti, A.; Pistello, M.; Basolo, A.; et al. COVID-19 autopsy cases: Detection of virus in endocrine tissues. J. Endocrinol. Investig. 2021, 45, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Jadali, Z. COVID-19 and Thyroid Infection: Learning the Lessons of the Past. Acta Endocrinol. 2020, 16, 375–376. [Google Scholar] [CrossRef] [PubMed]
- Tutal, E.; Ozaras, R.; Leblebicioglu, H. Systematic review of COVID-19 and autoimmune thyroiditis. Travel. Med. Infect. Dis. 2022, 47, 102314. [Google Scholar] [CrossRef]
- Pal, R.; Joshi, A.; Bhadada, S.K.; Banerjee, M.; Vaikkakara, S.; Mukhopadhyay, S. Endocrine Follow-up During Post-Acute COVID-19: Practical Recommendations Based on Available Clinical Evidence. Endocr. Pr. 2022. [Google Scholar] [CrossRef]
- Callard, F.; Perego, E. How and why patients made Long Covid. Soc. Sci. Med. 2021, 268, 113426. [Google Scholar] [CrossRef] [PubMed]
- Roth, P.H.; Gadebusch-Bondio, M. The contested meaning of “long COVID”—Patients, doctors, and the politics of subjective evidence. Soc. Sci. Med. 2022, 292, 114619. [Google Scholar] [CrossRef]
- Sivan, M.; Rayner, C.; Delaney, B. Fresh evidence of the scale and scope of long covid. BMJ 2021, 373, n853. [Google Scholar] [CrossRef]
- Newman, M. Chronic fatigue syndrome and long covid: Moving beyond the controversy. BMJ 2021, 373, n1559. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.D.; Lavelle, M.; Boursiquot, B.C.; Wan, E.Y. Long-term complications of COVID-19. Am. J. Physiol. Physiol. 2022, 322, C1–C11. [Google Scholar] [CrossRef]
- Rebello, C.J.; Axelrod, C.L.; Reynolds, C.F., 3rd; Greenway, F.L.; Kirwan, J.P. Exercise as a Moderator of Persistent Neuroendocrine Symptoms of COVID-19. Exerc. Sport Sci. Rev. 2022, 50, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Chippa, V.; Aleem, A.; Anjum, F. Post Acute Coronavirus (COVID-19) Syndrome; StatPearls: Treasure Island, FL, USA, 2022. [Google Scholar]
- Bushell, W.; Castle, R.; Williams, M.A.; Brouwer, K.C.; Tanzi, R.E.; Chopra, D.; Mills, P.J. Meditation and Yoga Practices as Potential Adjunctive Treatment of SARS-CoV-2 Infection and COVID-19: A Brief Overview of Key Subjects. J. Altern. Complement. Med. 2020, 26, 547–556. [Google Scholar] [CrossRef]
- Mangge, H.; Kneihsl, M.; Schnedl, W.; Sendlhofer, G.; Curcio, F.; Domenis, R. Immune Responses against SARS-CoV-2-Questions and Experiences. Biomedicines 2021, 9, 1342. [Google Scholar] [CrossRef]
- Antonelli, M.; Penfold, R.S.; Merino, J.; Sudre, C.H.; Molteni, E.; Berry, S.; Canas, L.S.; Graham, M.S.; Klaser, K.; Modat, M.; et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: A prospective, community-based, nested, case-control study. Lancet Infect. Dis. 2021, 22, 43–55. [Google Scholar] [CrossRef]
- Moghimi, N.; Di Napoli, M.; Biller, J.; Siegler, J.E.; Shekhar, R.; McCullough, L.D.; Harkins, M.S.; Hong, E.; Alaouieh, D.A.; Mansueto, G.; et al. The Neurological Manifestations of Post-Acute Sequelae of SARS-CoV-2 infection. Curr. Neurol. Neurosci. Rep. 2021, 21, 44. [Google Scholar] [CrossRef]
- Murray, T. Unpacking “long COVID”. CMAJ 2021, 193, E318–E319. [Google Scholar] [CrossRef] [PubMed]
- Drake, T.M.; Riad, A.M.; Fairfield, C.J.; Egan, C.; Knight, S.R.; Pius, R.; Hardwick, H.E.; Norman, L.; Shaw, C.A.; McLean, K.A.; et al. Characterisation of in-hospital complications associated with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol UK: A prospective, multicentre cohort study. Lancet 2021, 398, 223–237. [Google Scholar] [CrossRef]
- Hussain, F.A. Facilitating care: A biopsychosocial perspective on long COVID. Br. J. Gen. Pr. 2021, 72, 30–31. [Google Scholar] [CrossRef] [PubMed]
- Macpherson, K.; Cooper, K.; Harbour, J.; Mahal, D.; Miller, C.; Nairn, M. Experiences of living with long COVID and of accessing healthcare services: A qualitative systematic review. BMJ Open 2022, 12, e050979. [Google Scholar] [CrossRef]
- Inciardi, R.M.; Chandra, A. Editorial commentary: Long COVID-19: A tangled web of lungs, heart, mind, and gender. Trends Cardiovasc. Med. 2022, 32, 18–19. [Google Scholar] [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2021, 58, 297–310. [Google Scholar] [CrossRef]
| Post-COVID-19 Symptoms | Number of Patients Included in the Study | % Patients Suffering from Symptom/References |
|---|---|---|
| Fatigue | 596, 177, 538, 270, 138, 3065, 134, 242, 115, 143, 96, 1733, 5440, 384, 287 | 13.1% [34], 13.6% [20], 28.3% [7], 34.8% [25], 39.0% [27,30], 39.6% [6], 41.7% [35], 47% [26], 53.1% [36], 56.3% [28], 63% [19], up to 65% [16], 69% [37], 72.8% [38] |
| Persistent breathlessness /dyspnea | 596, 3065, 287, 270, 96, 138, 143, 384, 134, 5440, 35 | 6.0% [34], 23.2% [30], 28.2% [38], 34.0% [25], 37.5% [28], 40.0% [27], 43.4% [36], 53.0% [37], 60% [6], up to 61% [16], 80% [23] |
| Myalgia /muscle weakness | 277, 242, 134, 1733 | 19.6% [25], 35,1% [35], 51.5% [6], 63% [19] |
| Anxiety | 287, 402, 134 | 38.0% [38], 42% [39], 47.8% [6] |
| Sleep disturbance | 1733, 96, 134, 35, 138 | 21.1% [35], 26.0% [19], 26.0% [28], 35.1% [6], 40.0% [39], 46% [23], 49% [27] |
| Joint pain | 277, 143, 287 | 19.6% [25], 27.3% [36], 31.4% [38] |
| Headache | 242, 270, 3065, 287 | 19.0% [35], 19.8% [25], 23.4% [30], 28.6% [38] |
| Chest pain | 596, 242, 538, 143, 287, 35, 5440 | 0.8% [34], 10.7% [35], 12.3% [7], 21.7% [36], 28.9% [38], 34.8% [23], up to 89% [16] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boaventura, P.; Macedo, S.; Ribeiro, F.; Jaconiano, S.; Soares, P. Post-COVID-19 Condition: Where Are We Now? Life 2022, 12, 517. https://doi.org/10.3390/life12040517
Boaventura P, Macedo S, Ribeiro F, Jaconiano S, Soares P. Post-COVID-19 Condition: Where Are We Now? Life. 2022; 12(4):517. https://doi.org/10.3390/life12040517
Chicago/Turabian StyleBoaventura, Paula, Sofia Macedo, Filipa Ribeiro, Sónia Jaconiano, and Paula Soares. 2022. "Post-COVID-19 Condition: Where Are We Now?" Life 12, no. 4: 517. https://doi.org/10.3390/life12040517
APA StyleBoaventura, P., Macedo, S., Ribeiro, F., Jaconiano, S., & Soares, P. (2022). Post-COVID-19 Condition: Where Are We Now? Life, 12(4), 517. https://doi.org/10.3390/life12040517








