Effect of Combined Balance Exercises and Kinesio Taping on Balance, Postural Stability, and Severity of Ankle Instability in Female Athletes with Functional Ankle Instability
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Sample Size
2.3. The Pre-Test Assessment
2.4. The CAIT
2.5. Biodex Balance System, Single-Leg Test
2.6. WB Balance Exercises Protocol
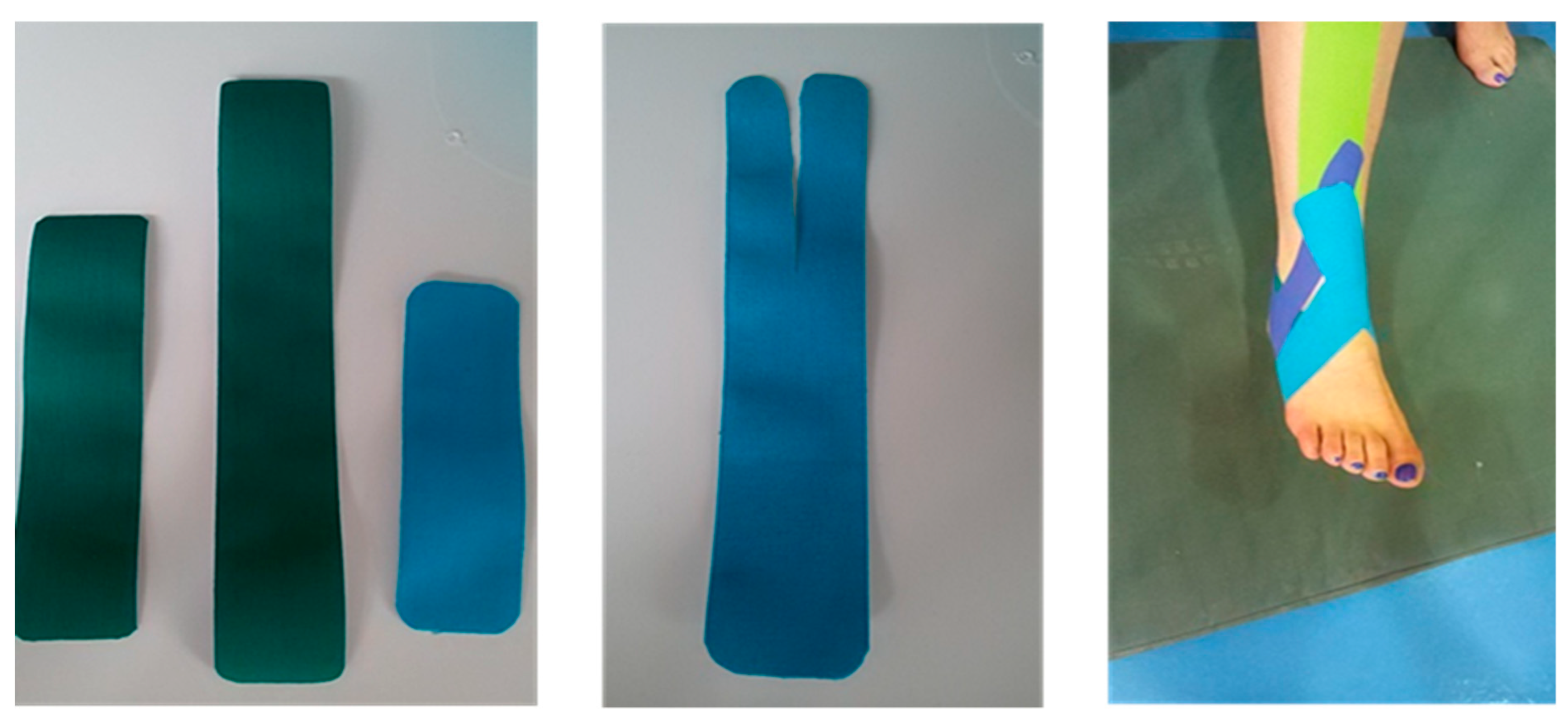
2.7. KT Technique1
2.8. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gribble, P.A.; Robinson, R.H. Alterations in knee kinematics and dynamic stability associated with chronic ankle instability. J. Athl. Train. 2009, 44, 350–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef] [PubMed]
- Fu, S.N.; Hui-Chan, C. Modulation of prelanding lower-limb muscle responses in athletes with multiple ankle sprains. Med. Sci. Sports Exerc. 2007, 39, 1774–1783. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.-P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O. 2016 consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef] [Green Version]
- Konradsen, L.; Bech, L.; Ehrenbjerg, M.; Nickelsen, T. Seven years follow-up after ankle inversion trauma. Scand. J. Med. Sci. Sports 2002, 12, 129–135. [Google Scholar] [CrossRef]
- Freeman, M.; Dean, M.; Hanham, I. The etiology and prevention of functional instability of the foot. Bone Jt. J. 1965, 47, 678–685. [Google Scholar] [CrossRef]
- Caldemeyer, L.E.; Brown, S.M.; Mulcahey, M.K. Neuromuscular training for the prevention of ankle sprains in female athletes: A systematic review. Physician Sportsmed. 2020, 48, 363–369. [Google Scholar] [CrossRef]
- Hertel, J. Functional instability following lateral ankle sprain. Sports Med. 2000, 29, 361–371. [Google Scholar] [CrossRef]
- Hals, T.-M.V.; Sitler, M.R.; Mattacola, C.G. Effect of a semi-rigid ankle stabilizer on performance in persons with functional ankle instability. J. Orthop. Sports Phys. Ther. 2000, 30, 552–556. [Google Scholar] [CrossRef] [Green Version]
- Ho, Y.-H.; Lin, C.-F.; Chang, C.-H.; Wu, H.-W. Effect of ankle kinesio taping on vertical jump with run-up and countermovement jump in athletes with ankle functional instability. J. Phys. Ther. Sci. 2015, 27, 2087–2090. [Google Scholar] [CrossRef] [Green Version]
- Kunugi, S.; Masunari, A.; Noh, B.; Mori, T.; Yoshida, N.; Miyakawa, S. Cross-cultural adaptation, reliability, and validity of the Japanese version of the Cumberland ankle instability tool. Disabil. Rehabil. 2017, 39, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caulfield, B.; Garrett, M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin. Biomech. 2004, 19, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.; Robinson, R. Differences in spatiotemporal landing variables during a dynamic stability task in subjects with CAI. Scand. J. Med. Sci. Sports 2010, 20, e63–e71. [Google Scholar] [CrossRef] [PubMed]
- Nobari, H.; Mainer-Pardos, E.; Denche Zamorano, A.; Bowman, T.G.; Clemente, F.M.; Pérez-Gómez, J. Sprint Variables Are Associated with the Odds Ratios of Non-Contact Injuries in Professional Soccer Players. Int. J. Environ. Res. Public Health 2021, 18, 10417. [Google Scholar] [CrossRef]
- Cho, B.-K.; Park, J.-K. Correlation between joint-position sense, peroneal strength, postural control, and functional performance ability in patients with chronic lateral ankle instability. Foot Ankle Int. 2019, 40, 961–968. [Google Scholar] [CrossRef]
- Hertel, J. Sensorimotor deficits with ankle sprains and chronic ankle instability. Clin. Sports Med. 2008, 27, 353–370. [Google Scholar] [CrossRef]
- Holmes, A.; Delahunt, E. Treatment of common deficits associated with chronic ankle instability. Sports Med. 2009, 39, 207–224. [Google Scholar] [CrossRef]
- Seyedi, M.; Nobari, H.; Abbasi, H.; Khezri, D.; Oliveira, R.; Pérez-Gómez, J.; Badicu, G.; Afonso, J. Effect of Four Weeks of Home-Based Balance Training on the Performance in Individuals with Functional Ankle Instability: A Remote Online Study. Healthcare 2021, 9, 1428. [Google Scholar] [CrossRef]
- Cruz-Diaz, D.; Lomas-Vega, R.; Osuna-Pérez, M.; Contreras, F.; Martínez-Amat, A. Effects of 6 weeks of balance training on chronic ankle instability in athletes: A randomized controlled trial. Int. J. Sports Med. 2015, 36, 754–760. [Google Scholar] [CrossRef] [Green Version]
- Pintsaar, A.; Brynhildsen, J.; Tropp, H. Postural corrections after standardised perturbations of single limb stance: Effect of training and orthotic devices in patients with ankle instability. Br. J. Sports Med. 1996, 30, 151–155. [Google Scholar] [CrossRef] [Green Version]
- Hopkins, J.T.; Ingersoll, C.D. Arthrogenic muscle inhibition: A limiting factor in joint rehabilitation. J. Sport Rehabil. 2000, 9, 135–159. [Google Scholar] [CrossRef]
- Cordova, M.L.; Ingersoll, C.D.; Palmieri, R.M. Efficacy of prophylactic ankle support: An experimental perspective. J. Athl. Train. 2002, 37, 446. [Google Scholar] [PubMed]
- Kemler, E.; van de Port, I.; Backx, F.; van Dijk, C.N. A systematic review on the treatment of acute ankle sprain. Sports Med. 2011, 41, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Fu, T.-C.; Wong, A.M.; Pei, Y.-C.; Wu, K.P.; Chou, S.-W.; Lin, Y.-C. Effect of Kinesio taping on muscle strength in athletes—A pilot study. J. Sci. Med. Sport 2008, 11, 198–201. [Google Scholar] [CrossRef] [PubMed]
- Shields, C.A.; Needle, A.R.; Rose, W.C.; Swanik, C.B.; Kaminski, T.W. Effect of elastic taping on postural control deficits in subjects with healthy ankles, copers, and individuals with functional ankle instability. Foot Ankle Int. 2013, 34, 1427–1435. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Wang, L. Acute effect of kinesiology taping on postural stability in individuals with unilateral chronic ankle instability. Front. Physiol. 2020, 11, 192. [Google Scholar] [CrossRef] [PubMed]
- Docherty, C.L.; McLeod, T.C.V.; Shultz, S.J. Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system. Clin. J. Sport Med. 2006, 16, 203–208. [Google Scholar] [CrossRef]
- Ross, S.E.; Guskiewicz, K.M.; Gross, M.T.; Yu, B. Assessment tools for identifying functional limitations associated with functional ankle instability. J. Athl. Train. 2008, 43, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Ross, S.E.; Guskiewicz, K.M.; Yu, B. Single-leg jump-landing stabilization times in subjects with functionally unstable ankles. J. Athl. Train. 2005, 40, 298. [Google Scholar]
- Ross, S.E.; Guskiewicz, K.M. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin. J. Sport Med. 2006, 16, 323–328. [Google Scholar] [CrossRef]
- Delahunt, E.; Coughlan, G.F.; Caulfield, B.; Nightingale, E.J.; Lin, C.-W.C.; Hiller, C.E. Inclusion criteria when investigating insufficiencies in chronic ankle instability. Med. Sci. Sports Exerc. 2010, 42, 2106–2121. [Google Scholar] [CrossRef] [PubMed]
- Mallaee, F.; Naseri, N.; Ghotbi, N. The effect of trapezius muscles kinesio taping on pain, functional movement of shouhder joint and lateral scapular slide in athletes with impingement syndrome. Mod. Rehabil. 2016, 9, 30–37. [Google Scholar]
- Suda, E.Y.; Amorim, C.F.; Sacco, I.d.C.N. Influence of ankle functional instability on the ankle electromyography during landing after volleyball blocking. J. Electromyogr. Kinesiol. 2009, 19, e84–e93. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Bailey, D.; Firth, P. Does kinesiology taping of the ankles affect proprioceptive control in professional football (soccer) players? Phys. Ther. Sport 2017, 25, 94–98. [Google Scholar] [CrossRef]
- Choi, I.-R.; Lee, J.-H. Effect of kinesiology tape application direction on quadriceps strength. Medicine 2018, 97, e11038. [Google Scholar] [CrossRef]
- Hadadi, M.; Ebrahimi Takamjani, I.; Ebrahim Mosavi, M.; Aminian, G.; Fardipour, S.; Abbasi, F. Cross-cultural adaptation, reliability, and validity of the Persian version of the Cumberland Ankle Instability Tool. Disabil. Rehabil. 2017, 39, 1644–1649. [Google Scholar] [CrossRef]
- Haji-Maghsoudi, M.; Naseri, N.; Nouri-Zadeh, S.; Jalayi, S. Evidence of reliability for persian version of the “Cumberland Ankle Instability Tool (CAIT)” in Iranian athletes with lateral ankle sprain. Arch. Rehabil. 2016, 16, 304–311. [Google Scholar]
- Hiller, C.E.; Refshauge, K.M.; Bundy, A.C.; Herbert, R.D.; Kilbreath, S.L. The Cumberland ankle instability tool: A report of validity and reliability testing. Arch. Phys. Med. Rehabil. 2006, 87, 1235–1241. [Google Scholar] [CrossRef]
- Rozzi, S.L.; Lephart, S.M.; Sterner, R.; Kuligowski, L. Balance training for persons with functionally unstable ankles. J. Orthop. Sports Phys. Ther. 1999, 29, 478–486. [Google Scholar] [CrossRef] [Green Version]
- Martin, R.L.; Davenport, T.E.; Paulseth, S.; Wukich, D.K.; Godges, J.J.; Altman, R.D.; Delitto, A.; DeWitt, J.; Ferland, A.; Fearon, H. Ankle stability and movement coordination impairments: Ankle ligament sprains: Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2013, 43, A1–A40. [Google Scholar] [PubMed] [Green Version]
- Hinman, M.R. Factors affecting reliability of the Biodex Balance System: A summary of four studies. J. Sport Rehabil. 2000, 9, 240–252. [Google Scholar] [CrossRef]
- Arifin, N.; Osman, N.A.A.; Abas, W.A.B.W. Intrarater test-retest reliability of static and dynamic stability indexes measurement using the Biodex Stability System during unilateral stance. J. Appl. Biomech. 2014, 30, 300–304. [Google Scholar] [CrossRef]
- Taş, S.; Ünlüer, N.Ö.; Çetin, A. Thickness, cross-sectional area, and stiffness of intrinsic foot muscles affect performance in single-leg stance balance tests in healthy sedentary young females. J. Biomech. 2020, 99, 109530. [Google Scholar] [CrossRef] [PubMed]
- Testerman, C.; Griend, R.V. Evaluation of ankle instability using the Biodex Stability System. Foot Ankle Int. 1999, 20, 317–321. [Google Scholar] [CrossRef]
- Baumgartner, T.A.; Chung, H. Confidence limits for intraclass reliability coefficients. Meas. Phys. Educ. Exerc. Sci. 2001, 5, 179–188. [Google Scholar] [CrossRef]
- Clark, V.M.; Burden, A.M. A 4-week wobble board exercise programme improved muscle onset latency and perceived stability in individuals with a functionally unstable ankle. Phys. Ther. Sport 2005, 6, 181–187. [Google Scholar] [CrossRef]
- Hopkins, W.; Marshall, S.; Batterham, A.; Hanin, J. Progressive statistics for studies in sports medicine and exercise science. Med. Sci. Sports Exerc. 2009, 41, 3. [Google Scholar] [CrossRef] [Green Version]
- Park, D.-J.; Kim, B.-J.; Kim, Y.-H.; Park, S.-Y. A three-week intervention emphasized diagonal eccentric contraction on balance and joint position sense and ankle strength in subjects with ankle instability: A randomized controlled trial. J. Back Musculoskelet. Rehabil. 2021, 34, 95–101. [Google Scholar] [CrossRef]
- Lazarou, L.; Kofotolis, N.; Malliou, P.; Kellis, E. Effects of two proprioceptive training programs on joint position sense, strength, activation and recurrent injuries after ankle sprains. Isokinet. Exerc. Sci. 2017, 25, 289–300. [Google Scholar] [CrossRef]
- Winter, D.A.; Patla, A.E.; Rietdyk, S.; Ishac, M.G. Ankle muscle stiffness in the control of balance during quiet standing. J. Neurophysiol. 2001, 85, 2630–2633. [Google Scholar] [CrossRef] [PubMed]
- Linens, S.W.; Ross, S.E.; Arnold, B.L. Wobble board rehabilitation for improving balance in ankles with chronic instability. Clin. J. Sport Med. 2016, 26, 76–82. [Google Scholar] [CrossRef] [PubMed]
- McKeon, P.O.; Hertel, J. Systematic review of postural control and lateral ankle instability, part I: Can deficits be detected with instrumented testing? J. Athl. Train. 2008, 43, 293–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ly, K.; Michaud, L.; Lajoie, Y. The effects of Kinesiology Tape on static postural control in individuals with functional ankle instability. Phys. Ther. Sport 2021, 48, 146–153. [Google Scholar] [CrossRef]
- Hubbard, T.J.; Hertel, J.; Olmsted-Kramer, L.; Denegar, C.R. Contributing Factors to Chronic Ankle Instability: 9478: 45 AM–9: 00 AM. Med. Sci. Sports Exerc. 2006, 38, S86–S87. [Google Scholar] [CrossRef]
- Sarvestan, J.; Kovacikova, Z.; Svoboda, Z.; Needle, A. Ankle Kinesio taping impacts on lower limbs biomechanics during countermovement jump among collegiate athletes with chronic ankle instability. Gait Posture 2020, 81, 327–328. [Google Scholar] [CrossRef]
- de Almeida Lins, C.A.; Neto, F.L.; de Amorim, A.B.C.; de Brito Macedo, L.; Brasileiro, J.S. Kinesio Taping® does not alter neuromuscular performance of femoral quadriceps or lower limb function in healthy subjects: Randomized, blind, controlled, clinical trial. Man. Ther. 2013, 18, 41–45. [Google Scholar] [CrossRef]
- Oliveira, A.K.; Borges, D.T.; Lins, C.A.; Cavalcanti, R.L.; Macedo, L.B.; Brasileiro, J.S. Immediate effects of Kinesio Taping® on neuromuscular performance of quadriceps and balance in individuals submitted to anterior cruciate ligament reconstruction: A randomized clinical trial. J. Sci. Med. Sport 2016, 19, 2–6. [Google Scholar] [CrossRef]
- Inglés, M.; Serra-Añó, P.; Méndez, À.G.; Zarzoso, M.; Aguilar-Rodríguez, M.; Suso-Martí, L.; Cuenca-Martínez, F.; Espí-López, G.V. Effect of Kinesio Taping and balance exercises on postural control in amateur soccer players: A randomised control trial. J. Sports Sci. 2019, 37, 2853–2862. [Google Scholar] [CrossRef]
- Momeni-lari, H.; Ghasemi, M.; Khademi-kalantari, K.; Akbarzadeh-baghban, A. The Short-Term Effects of Kinesio Tape on Joint Position Sense, Sense of Force and Postural Control in Patients with Functional Ankle Instability. J. Babol Univ. Med. Sci. 2018, 20, 51–55. [Google Scholar]
- Lee, B.-G.; Lee, J.-H. Immediate effects of ankle balance taping with kinesiology tape on the dynamic balance of young players with functional ankle instability. Technol. Health Care 2015, 23, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Dowell, H.; Ross, S. The Effects of Leg Spiral Kinesiology Tape Technique on Postural Sway in Clients with Multiple Sclerosis: A Quantitative Preliminary Study. J. Phys. Ther. 2017. Available online: https://research.edgehill.ac.uk/en/publications/the-effects-of-leg-spiral-kinesiology-tape-technique-on-postural--2 (accessed on 20 January 2022).
- Wilson, V.; Douris, P.C. The Immediate and Long-term Effects of Kinesio Tape on Balance And Functional Performance: Spo150. J. Orthop. Sports Phys. 2017, 47, A225. [Google Scholar]

| Eyes Status—Surface | Sets and Reps—Rest (between Sets) | Exercise | Session |
|---|---|---|---|
| Eyes open—Hard Surface | 3 sets, 10 s-10 s rest | Maintain balance on wobble board | 1 |
| Eyes open—Hard Surface | 1 × 30 s + 3 × 30 s-10 s rest | Maintain balance + forward and backward motion of the wobble board on both legs | 2 |
| Repeat the exercises of the second session | 3 | ||
| Eyes open—Hard Surface | 1 × 30 s + 3 × 30 s + 3 × 30 s + 1 × 30 s-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides + circular movement of wobble board from front to side | 4 |
| Repeat the exercises of the fourth session | 5 | ||
| Eyes open—Hard Surface | Each exercise (3 × 30 s)-10 s rest | Repeat the exercises of the fourth session in a semi-squat position | 6 |
| Eyes open—Hard Surface- | First 4 exercises (1 ×30 s) + last exercise (6 × 10 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides + circular movement of wobble board from front to side + standing with FAI leg on the wobble board and maintaining balance | 7 |
| Repeat the exercises of the seventh session | 8 | ||
| Eyes open—Hard Surface | 1 × 30 s+ Next 3 exercises (2 × 30 s) + last exercise (6 × 10 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides + circular movement of wobble board from front to side + standing with FAI leg on the wobble board and maintaining balance | 9 |
| Closed eyes—Hard surface | 2 × 30 s-10 s rest | Maintain balance | 10 |
| Closed eyes—Hard surface | 1 × 30 s + 3 × 30 s-10 s rest | Maintain balance + forward and backward motion of the wobble board on both legs | 11 |
| Closed eyes—Hard surface | 1 × 30 s + next 2 exercises (3 × 30 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides | 12 |
| Closed eyes—Hard surface | 1 × 30 s + next 2 exercises (3 × 30 s) + last exercise (1 × 30 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides + circular movement of wobble board from front to side | 13 |
| Closed eyes—Hard surfaceIn semi-sitting position | 1 × 30 s + next 2 exercises (3 × 30 s) + last exercise (2 × 30 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides + circular movement of wobble board from front to side | 14 |
| Closed eyes—Hard surface | 6 × 10 s-10 s rest | Standing with FAI leg on the wobble board and maintaining balance | 15 |
| Eyes open—Soft Surface | Each exercise (1 × 30 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides | 16 |
| Closed eyes—Soft surface | Each exercise (1 × 30 s)-10 s rest | Maintain balance + forward and backward motion + move the wobble board to the sides + circular movement of wobble board from front to side | 17 |
| Closed eyes—Soft surface | 6 × 10 s-10 s rest | Standing with FAI leg on the wobble board and maintaining balance | 18 |
| Groups | BMI (Kg/m2) | Age (yrs) |
|---|---|---|
| SG | 22.61 ± 2.91 | 24.8 ± 2.6 |
| CG | 21.88 ± 2.18 | 25.6 ± 2.5 |
| Assessments | Groups | Pre- Intervention | Post- Intervention | Within Groups | Between Groups | CI95% for Difference | Hedge’s g (95% CI) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| t | p | t | p | t | p | Values [Lower-Upper] | Values [Lower-Upper] | ||||
| Balance and postural stability | BTG | 1.38 ± 0.51 | 0.89 ± 0.21 | 3.95 | 0.002 a | −2.07 | 0.051 | 2.79 | 0.011 b | −0.49[−0.82 to −0.16] | −1.21[−2.08 to −0.34] L |
| BT + KTG | 1.88 ± 0.62 | 0.86 ± 0.22 | 7.22 | 0.001 a | −1.01[−1.42 to −0.6] | −1.99[−2.96 to −1.01] L | |||||
| Severity of instability | BTG | 20.67 ± 2.39 | 23.42 ± 2.71 | −5.4 | 0.001 a | 0.44 | 0.667 | 2.082 | 0.049 b | 2.74[0.58 to 4.9] | 1.03[0.18 to 1.89] M |
| BT + KTG | 20.08 ± 3.97 | 24.58 ± 3.8 | 6.73 | 0.001 a | 5.5[2.21 to 8.79] | 1.36[0.48 to 2.25] L | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khalili, S.M.; Barati, A.H.; Oliveira, R.; Nobari, H. Effect of Combined Balance Exercises and Kinesio Taping on Balance, Postural Stability, and Severity of Ankle Instability in Female Athletes with Functional Ankle Instability. Life 2022, 12, 178. https://doi.org/10.3390/life12020178
Khalili SM, Barati AH, Oliveira R, Nobari H. Effect of Combined Balance Exercises and Kinesio Taping on Balance, Postural Stability, and Severity of Ankle Instability in Female Athletes with Functional Ankle Instability. Life. 2022; 12(2):178. https://doi.org/10.3390/life12020178
Chicago/Turabian StyleKhalili, Sara Mahmoudzadeh, Amir Hossein Barati, Rafael Oliveira, and Hadi Nobari. 2022. "Effect of Combined Balance Exercises and Kinesio Taping on Balance, Postural Stability, and Severity of Ankle Instability in Female Athletes with Functional Ankle Instability" Life 12, no. 2: 178. https://doi.org/10.3390/life12020178
APA StyleKhalili, S. M., Barati, A. H., Oliveira, R., & Nobari, H. (2022). Effect of Combined Balance Exercises and Kinesio Taping on Balance, Postural Stability, and Severity of Ankle Instability in Female Athletes with Functional Ankle Instability. Life, 12(2), 178. https://doi.org/10.3390/life12020178







