Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Ethics
2.2. Inclusion and Exclusion Criteria
2.3. Outcome Measures
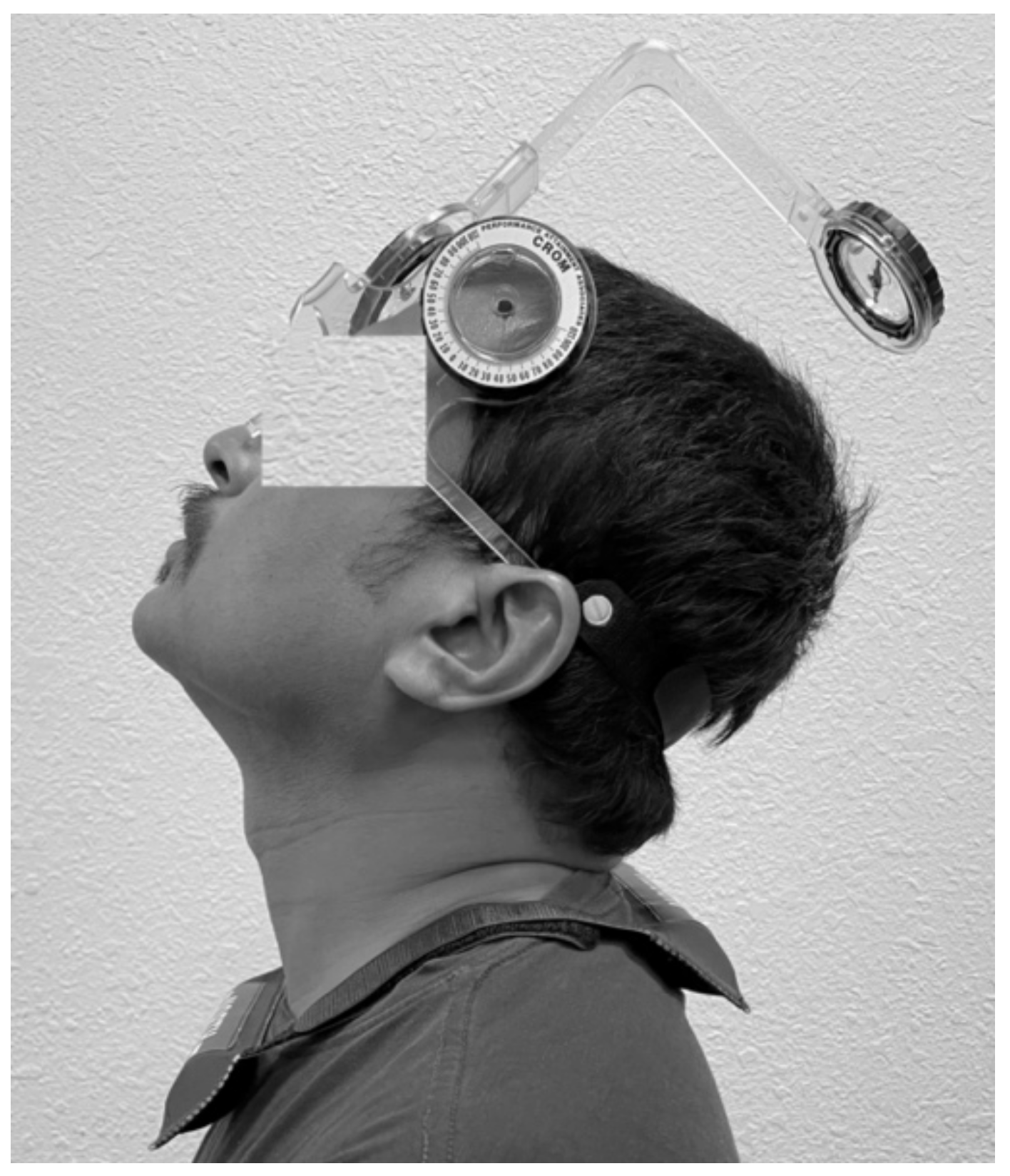
2.3.1. Cervical Joint Position Sense Testing
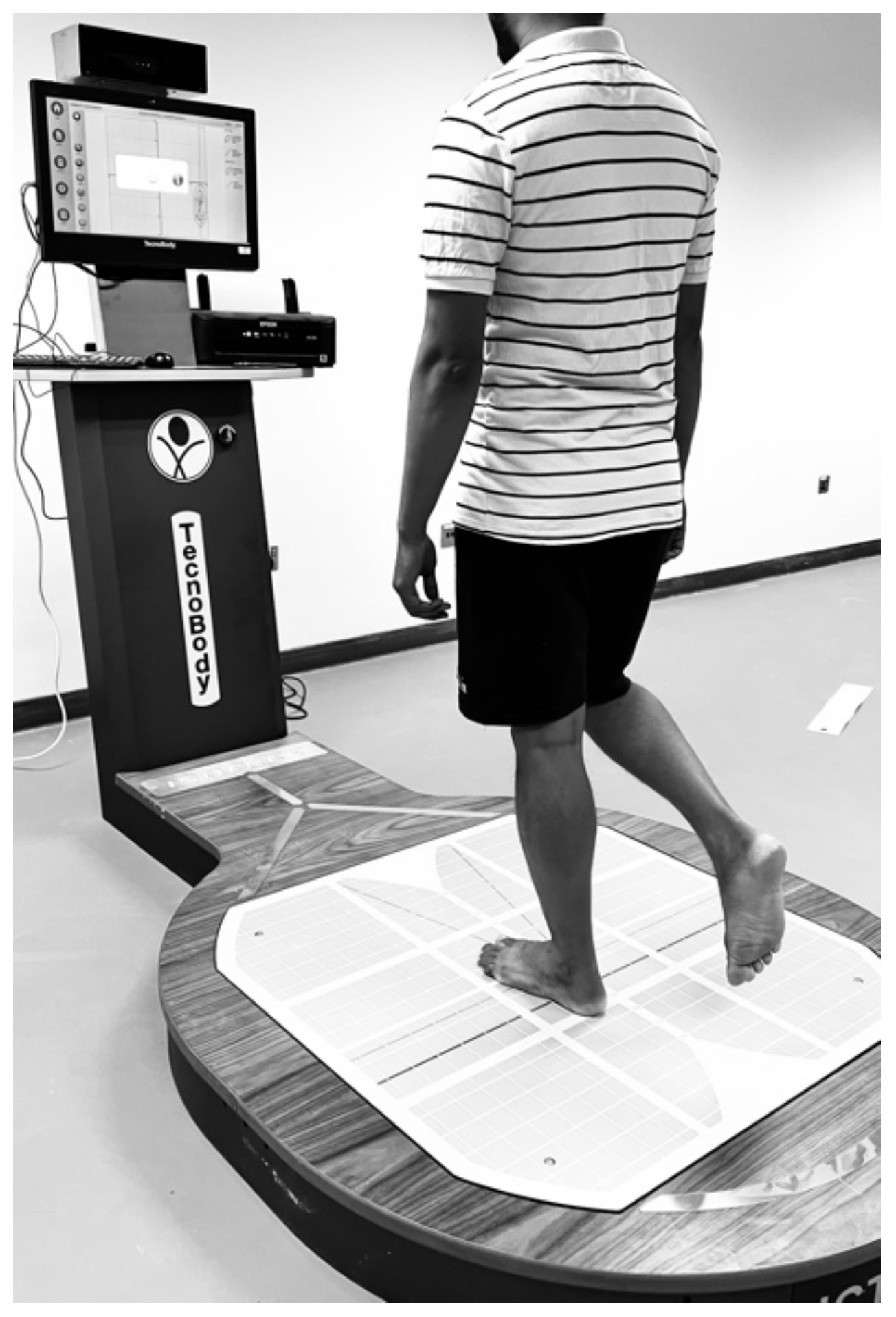
2.3.2. Postural Stability Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Galvez-Sánchez, C.M.; Duschek, S.; Del Paso, G.A.R. Psychological impact of fibromyalgia: Current perspectives. Psychol. Res. Behav. Manag. 2019, 12, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Binkiewicz-Glińska, A.; Bakuła, S.; Tomczak, H.; Landowski, J.; Ruckemann-Dziurdzińska, K.; Zaborowska-Sapeta, K.; Kiebzak, W. Fibromyalgia Syndrome—A multidisciplinary approach. Psychiatr. Pol. 2015, 49, 801–810. [Google Scholar] [PubMed]
- Alshahrani, M.S.; Reddy, R.S.Y.; Tedla, J.S. Effectiveness of Hydro-Galvanic Bath Therapy on Global Health Status, Quality of Life, Depression, and Pain in Individuals with Fibromyalgia—A Quasi-Experimental Study. Phys. Med. Rehabil. Kurortmed. 2020, 30, 370–376. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Tedla, J.S.; Reddy, R.S.; Asiri, F. Effectiveness of Hydrogalvanic Bath on Improving Pain, Disability, and Quality of Life in Individuals with Chronic Nonspecific Neck Pain: A Randomized Controlled Trial. Evid.-Based Complement. Altern. Med. 2020, 2020, 7974816. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.P.; Santo, A.d.S.d.E.; Berssaneti, A.A.; Matsutani, L.A.; Yuan, S.L.K. Prevalence of fibromyalgia: Literature review update. Rev. Bras. Reumatol. 2017, 57, 356–363. [Google Scholar] [CrossRef]
- Grayston, R.; Czanner, G.; Elhadd, K.; Goebel, A.; Frank, B.; Üçeyler, N.; Malik, R.A.; Alam, U. A systematic review and meta-analysis of the prevalence of small fiber pathology in fibromyalgia: Implications for a new paradigm in fibromyalgia etiopathogenesis. In Seminars in Arthritis and Rheumatism; WB Saunders: Philadelphia, PA, USA, 2019; pp. 933–940. [Google Scholar]
- Mukhopadhyay, K. Proprioception and Kinesthesia: The sixth sense organ. Adv. Health Exerc. 2021, 1, 12–17. [Google Scholar]
- Reddy, R.S.; Tedla, J.S.; Alshahrani, M.S.; Asiri, F.; Kakaraparthi, V.N. Comparison and correlation of cervical proprioception and muscle endurance in general joint hypermobility participants with and without non-specific neck pain—A cross-sectional study. PeerJ 2022, 10, e13097. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Dixit, S.; Asiri, F.; Al-Otaibi, M.L.; Kakaraparthi, V.N.; Assiri, S.M.A. Comparison of Cervical Joint Position Sense in Computer Users with Neck Pain, Forward Head Posture, Asymptomatic and Non-Computer Users—A Cross-Sectional Study. Phys. Med. Rehabil. Kurortmed. 2022. [Google Scholar] [CrossRef]
- Peng, B.; Yang, L.; Li, Y.; Liu, T.; Liu, Y. Cervical proprioception Impairment in neck pain-pathophysiology, clinical evaluation, and management: A narrative review. Pain Ther. 2021, 10, 143–164. [Google Scholar] [CrossRef]
- Nyland, J.; Franklin, T.; Short, A.; Calik, M.; Kaya, D. Posture, Kinesthesia, Foot Sensation, Balance, and Proprioception. Proprioception Orthop. Sport. Med. Rehabil. 2018, 12, 13–24. [Google Scholar]
- Mazaheri, M.; Abichandani, D.; Kingma, I.; Treleaven, J.; Falla, D. A meta-analysis and systematic review of changes in joint position sense and static standing balance in patients with whiplash-associated disorder. PLoS ONE 2021, 16, e0249659. [Google Scholar]
- Alahmari, K.A.; Reddy, R.S.; Tedla, J.S.; Samuel, P.S.; Kakaraparthi, V.N.; Rengaramanujam, K.; Ahmed, I. The effect of Kinesio taping on cervical proprioception in athletes with mechanical neck pain—A placebo-controlled trial. BMC Musculoskelet. Disord. 2020, 21, 648. [Google Scholar] [CrossRef]
- Lark, S.D.; McCarthy, P.W. Cervical range of motion and proprioception in rugby players versus non-rugby players. J. Sport. Sci. 2007, 25, 887–894. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alahmari, K.A.; Silvian, P.S. Test-retest reliability of assessing cervical proprioception using cervical range of motion device. Saudi J. Sport. Med. 2016, 16, 118. [Google Scholar] [CrossRef]
- Story, M.R. Equine Cervical Pain and Dysfunction; Colorado State University: Fort Collins, CO, USA, 2021. [Google Scholar]
- Pinsault, N.; Vuillerme, N. Degradation of cervical joint position sense following muscular fatigue in humans. Spine 2010, 35, 294–297. [Google Scholar] [CrossRef]
- de Vries, J.; Ischebeck, B.; Voogt, L.; Van Der Geest, J.; Janssen, M.; Frens, M.; Kleinrensink, G.J. Joint position sense error in people with neck pain: A systematic review. Man. Ther. 2015, 20, 736–744. [Google Scholar] [CrossRef]
- Alahmari, K.; Reddy, R.S.; Silvian, P.; Ahmad, I.; Nagaraj, V.; Mahtab, M. Intra-and inter-rater reliability of neutral head position and target head position tests in patients with and without neck pain. Braz. J. Phys. Ther. 2017, 21, 259–267. [Google Scholar] [CrossRef]
- Paillard, T.; Noé, F. Techniques and methods for testing the postural function in healthy and pathological subjects. BioMed Res. Int. 2015, 2015, 891390. [Google Scholar] [CrossRef] [Green Version]
- Akkaya, N.; Akkaya, S.; Atalay, N.S.; Acar, M.; Catalbas, N.; Sahin, F. Assessment of the relationship between postural stability and sleep quality in patients with fibromyalgia. Clin. Rheumatol. 2013, 32, 325–331. [Google Scholar] [CrossRef]
- Sarıhan, K.; Uzkeser, H.; Erdal, A. Evaluation of balance, fall risk, and related factors in patients with fibromyalgia syndrome. Turk. J. Phys. Med. Rehabil. 2021, 67, 409. [Google Scholar] [CrossRef]
- Qureshi, A.G.; Jha, S.K.; Iskander, J.; Avanthika, C.; Jhaveri, S.; Patel, V.H.; Potini, B.R.; Azam, A.T. Diagnostic challenges and management of fibromyalgia. Cureus 2021, 13, e18692. [Google Scholar] [CrossRef] [PubMed]
- Gucmen, B.; Kocyigit, B.F.; Nacitarhan, V.; Berk, E.; Koca, T.T.; Akyol, A. The relationship between cervical proprioception and balance in patients with fibromyalgia syndrome. Rheumatol. Int. 2022, 42, 311–318. [Google Scholar] [CrossRef] [PubMed]
- Mingorance, J.A.; Montoya, P.; Miranda, J.G.V.; Riquelme, I. An Observational Study Comparing Fibromyalgia and Chronic Low Back Pain in Somatosensory Sensitivity, Motor Function and Balance. Healthcare 2021, 9, 1533. [Google Scholar] [CrossRef] [PubMed]
- Cyma-Wejchenig, M.; Tarnas, J.; Marciniak, K.; Stemplewski, R. The influence of proprioceptive training with the use of virtual reality on postural stability of workers working at height. Sensors 2020, 20, 3731. [Google Scholar] [CrossRef] [PubMed]
- Naderifar, H.; Minoonejad, H.; Barati, A.H.; Lashay, A. Effect of a neck proprioceptive neuromuscular facilitation training program on body postural stability in elite female basketball players. J. Rehabil. Sci. Res. 2018, 5, 41–45. [Google Scholar]
- Galvez-Sánchez, C.M.; Reyes del Paso, G.A. Diagnostic criteria for fibromyalgia: Critical review and future perspectives. J. Clin. Med. 2020, 9, 1219. [Google Scholar] [CrossRef]
- Reddy, R.S.; Alshahrani, M.S.; Tedla, J.S.; Asiri, F.; Nambi, G.; Kakaraparthi, V.N. Cervical Joint Position Sense in Individuals with Type 2 Diabetes and Its Correlations with Glycated Hemoglobin Levels: A Cross-Sectional Study. J. Manip. Physiol. Ther. 2022, 45, 273–281. [Google Scholar] [CrossRef]
- Reddy, R.S.; Tedla, J.S.; Dixit, S.; Abohashrh, M. Cervical proprioception and its relationship with neck pain intensity in subjects with cervical spondylosis. BMC Musculoskelet. Disord. 2019, 20, 447. [Google Scholar] [CrossRef] [Green Version]
- Thoomes-de Graaf, M.; Thoomes, E.; Fernández-de-Las-Peñas, C.; Plaza-Manzano, G.; Cleland, J.A. Normative values of cervical range of motion for both children and adults: A systematic review. Musculoskelet. Sci. Pract. 2020, 49, 102182. [Google Scholar] [CrossRef]
- Vaillant, J.; Coisne, A.; Dumolard, A. Alteration of neck proprioceptive capacity in women with fibromyalgia. Ann. Phys. Rehabil. Med. 2017, 60, e18. [Google Scholar] [CrossRef]
- Toprak Celenay, S.; Mete, O.; Coban, O.; Oskay, D.; Erten, S. Trunk position sense, postural stability, and spine posture in fibromyalgia. Rheumatol. Int. 2019, 39, 2087–2094. [Google Scholar] [CrossRef]
- Ulus, Y.; Akyol, Y.; Tander, B.; Bilgici, A.; KURU, Ö. Knee Proprioception and Balance in Turkish Women with and without Fibromyalgia Syndrome. Turk. J. Phys. Med. Rehabil./Turk. Fiz. Tip Ve Rehabil. Derg. 2013, 59, 128–132. [Google Scholar] [CrossRef]
- Reddy, R.S.; Meziat-Filho, N.; Ferreira, A.S.; Tedla, J.S.; Kandakurti, P.K.; Kakaraparthi, V.N. Comparison of neck extensor muscle endurance and cervical proprioception between asymptomatic individuals and patients with chronic neck pain. J. Bodyw. Mov. Ther. 2021, 26, 180–186. [Google Scholar] [CrossRef]
- Reddy, R.S.; Maiya, A.G.; Rao, S.K. Effect of dorsal neck muscle fatigue on cervicocephalic kinaesthetic sensibility. Hong Kong Physiother. J. 2012, 30, 105–109. [Google Scholar] [CrossRef]
- Kandakurti, P.K.; Reddy, R.S.; Kakarparthy, V.N.; Rengaramanujam, K.; Tedla, J.S.; Dixit, S.; Gautam, A.P.; Silvian, P.; Gular, K.; Eapen, C. Comparison and Association of Neck Extensor Muscles’ Endurance and Postural Function in Subjects with and without Chronic Neck Pain—A Cross-Sectional Study. Phys. Med. Rehabil. Kurortmed. 2021, 31, 295–301. [Google Scholar] [CrossRef]
- Asiri, F.; Reddy, R.S.; Tedla, J.S.; ALMohiza, M.A.; Alshahrani, M.S.; Govindappa, S.C.; Sangadala, D.R. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PLoS ONE 2021, 16, e0254262. [Google Scholar] [CrossRef]
- Alahmari, K.A.; Kakaraparthi, V.N.; Reddy, R.S.; Silvian, P.; Tedla, J.S.; Rengaramanujam, K.; Ahmad, I. Combined effects of strengthening and proprioceptive training on stability, balance, and proprioception among subjects with chronic ankle instability in different age groups: Evaluation of clinical outcome measures. Indian J. Orthop. 2021, 55, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Demir-Göçmen, D.; Altan, L.; Korkmaz, N.; Arabacı, R. Effect of supervised exercise program including balance exercises on the balance status and clinical signs in patients with fibromyalgia. Rheumatol. Int. 2013, 33, 743–750. [Google Scholar] [CrossRef]
- Duruturk, N.; Tuzun, E.H.; Culhaoglu, B. Is balance exercise training as effective as aerobic exercise training in fibromyalgia syndrome? Rheumatol. Int. 2015, 35, 845–854. [Google Scholar] [CrossRef]
- Trevisan, D.C.; Driusso, P.; Avila, M.A.; Gramani-Say, K.; Moreira, F.M.A.; Parizotto, N.A. Static postural sway of women with and without fibromyalgia syndrome: A cross-sectional study. Clin. Biomech. 2017, 44, 83–89. [Google Scholar] [CrossRef]
- Zhang, C.; Zhang, Z.; Li, Y.; Feng, C.; Meng, H.; Gao, Y.; Lo, W.L.A.; Wang, C. Pain catastrophizing is related to static postural control impairment in patients with nonspecific chronic low back pain: A cross-sectional study. Pain Res. Manag. 2020, 2020, 9629526. [Google Scholar] [CrossRef] [PubMed]
- Viseux, F.J.; Martins, D.F.; Villeneuve, P.; Charpentier, P.; de Sant’Anna e Silva, L.; Salgado, A.S.; Lemaire, A. Effect of sensory stimulation applied under the great toe on postural ability in patients with fibromyalgia. Somatosens. Mot. Res. 2020, 37, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Birznieks, I.; Burton, A.R.; Macefield, V.G. The effects of experimental muscle and skin pain on the static stretch sensitivity of human muscle spindles in relaxed leg muscles. J. Physiol. 2008, 586, 2713–2723. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.D.; King, L.A.; Mist, S.D.; Bennett, R.M.; Horak, F.B. Postural control deficits in people with fibromyalgia: A pilot study. Arthritis Res. Ther. 2011, 13, R127. [Google Scholar] [CrossRef] [PubMed]
- Treleaven, J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man. Ther. 2008, 13, 2–11. [Google Scholar] [CrossRef]
- Treleaven, J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control—Part 2: Case studies. Man. Ther. 2008, 13, 266–275. [Google Scholar] [CrossRef]
- Berardi, G.; Senefeld, J.W.; Hunter, S.K.; Bement, M.K.H. Impact of isometric and concentric resistance exercise on pain and fatigue in fibromyalgia. Eur. J. Appl. Physiol. 2021, 121, 1389–1404. [Google Scholar] [CrossRef]
- Meireles, S.A.; Antero, D.C.; Kulczycki, M.M.; Skare, T.L. Prevalence of falls in fibromyalgia patients. Acta Ortop. Bras. 2014, 22, 163–166. [Google Scholar] [CrossRef] [Green Version]
- Peinado-Rubia, A.; Osuna-Pérez, M.C.; Rodríguez-Almagro, D.; Zagalaz-Anula, N.; López-Ruiz, M.C.; Lomas-Vega, R. Impaired balance in patients with fibromyalgia syndrome: Predictors of the impact of this disorder and balance confidence. Int. J. Environ. Res. Public Health 2020, 17, 3160. [Google Scholar] [CrossRef]
- Cooper, R.; Taylor, N.; Feller, J. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Res. Sport. Med. 2005, 13, 163–178. [Google Scholar] [CrossRef] [Green Version]
- Gauchard, G.C.; Jeandel, C.; Tessier, A.; Perrin, P.P. Beneficial effect of proprioceptive physical activities on balance control in elderly human subjects. Neurosci. Lett. 1999, 273, 81–84. [Google Scholar] [CrossRef]
- Wooten, S.V.; Signorile, J.F.; Desai, S.S.; Paine, A.K.; Mooney, K. Yoga meditation (YoMed) and its effect on proprioception and balance function in elders who have fallen: A randomized control study. Complement. Ther. Med. 2018, 36, 129–136. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B.; Yunus, M.B. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010, 62, 600–610. [Google Scholar] [CrossRef] [Green Version]
- Zambolin, F.; Duro-Ocana, P.; Faisal, A.; Bagley, L.; Gregory, W.J.; Jones, A.W.; McPhee, J.S. Fibromyalgia and Chronic Fatigue Syndromes: A systematic review and meta-analysis of cardiorespiratory fitness and neuromuscular function compared with healthy individuals. PLoS ONE 2022, 17, e0276009. [Google Scholar] [CrossRef]
- Saeed Alshahrani, M.; Reddy, R.S.; Asiri, F.; Tedla, J.S.; Alshahrani, A.; Kandakurti, P.K.; Kakaraparthi, V.N. Correlation and comparison of quadriceps endurance and knee joint position sense in individuals with and without unilateral knee osteoarthritis. BMC Musculoskelet. Disord. 2022, 23, 444. [Google Scholar] [CrossRef]
- Alshahrani, M.S.; Reddy, R.S. Relationship between Kinesiophobia and Ankle Joint Position Sense and Postural Control in Individuals with Chronic Ankle Instability—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2792. [Google Scholar] [CrossRef]
| Variables | FMS Individuals (n = 92) | Asymptomatic (n = 92) | p-Value |
|---|---|---|---|
| Age (years) | 51.52 ± 7.7 | 49.36 ± 6.9 | 0.267 |
| Gender (M: F) | 39:53 | 27:65 | 0.010 |
| Height (meters) | 1.68 ± 0.10 | 1.63 ± 0.05 | 0.521 |
| Weight (kg) | 72.20 ± 6.44 | 69.73 ± 5.23 | 0.052 |
| BMI (kg/m2) | 25.72 ± 4.02 | 25.38 ± 2.81 | 0.621 |
| Pain intensity: VAS (0–10 cm) | 5.9 ± 1.3 | - | - |
| Widespread pain index | 13.90 ± 2.50 | - | - |
| Symptom severity score | 9.86 ± 1.70 | - | - |
| Duration of pain in years | 6.82 ± 2.43 | - | - |
| Fibromyalgia impact questionnaire | 61.10 ± 10.0 | - | - |
| Pain catastrophizing | 30.53 ± 4.96 | - | - |
| SF-36 | 37.01 ± 9.02 | - | - |
| Exercise status (n) | - | - | |
| 36 | ||
| 28 | ||
| 16 | ||
| 12 |
| Variables | FMS Group (n = 92) Mean ± SD | Asymptomatic Group (n = 92) Mean ± SD | p-Value |
|---|---|---|---|
| Cervical JPS in flexion (°) | 5.5 ± 1.43 | 2.4 ± 1.30 | <0.001 |
| Cervical JPS in extension (°) | 6.4 ± 1.53 | 3.0 ± 1.25 | <0.001 |
| Cervical JPS in rotation left (°) | 5.4 ± 1.36 | 2.9 ± 0.79 | <0.001 |
| Cervical JPS in rotation right (°) | 5.1 ± 1.29 | 2.8 ± 0.63 | <0.001 |
| Anterior–posterior sway (mm)—non-dominant | 9.92 ± 3.65 | 3.32 ± 1.20 | <0.001 |
| Medial–lateral sway (mm)—non-dominant | 7.34 ± 2.45 | 3.88 ± 1.55 | <0.001 |
| Ellipse Area (mm2)—non-dominant | 986.2 ± 152.63 | 457.88 ± 151.83 | <0.001 |
| Anterior-posterior sway (mm)—dominant | 8.65 ± 3.34 | 3.35 ± 1.27 | <0.001 |
| Medial–lateral sway (mm)—dominant | 6.15 ± 1.83 | 3.49 ± 1.58 | <0.001 |
| Ellipse area (mm2)—dominant | 966.91 ± 136.09 | 432.30 ± 154.40 | <0.001 |
| Variables | Cervical JPS in Flexion (°) | Cervical JPS in Extension (°) | Cervical JPS in Rotation Left (°) | Cervical JPS in Rotation Right (°) | Anterior-Posterior Sway (mm)—Non-Dominant | Medial–Lateral Sway (mm)—Non-Dominant | Ellipse Area (mm2)—Non-Dominant | Anterior-Posterior Sway (mm)—Dominant | Medial–Lateral Sway (mm)—Dominant] | Ellipse area (mm2)—Dominant | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cervical JPS in flexion (°) | r | 1 | |||||||||
| Cervical JPS in extension (°) | r | 0.575 ** | 1 | ||||||||
| Cervical JPS in rotation left (°) | r | 0.591 ** | 0.557 ** | 1 | |||||||
| Cervical JPS in rotation right (°) | r | 0.586 ** | 0.546 ** | 0.801 ** | 1 | ||||||
| Anterior-posterior sway (mm)–non-dominant | r | 0.613 | 0.573 | 0.562 | 0.552 | 1 | |||||
| Medial–lateral sway (mm)—non-dominant | r | 0.574 ** | 0.377 ** | 0.526 ** | 0.545 ** | 0.531 ** | 1 | ||||
| Ellipse area (mm2)—non-dominant | r | 0.650 ** | 0.642 ** | 0.667 ** | 0.651 ** | 0.645 ** | 0.617 ** | 1 | |||
| Anterior–posterior sway (mm)—dominant | r | 0.543 ** | 0.483 ** | 0.524 ** | 0.548 ** | 0.514 ** | 0.583 ** | 0.705 ** | 1 | ||
| Medial–lateral sway (mm)—dominant | r | 0.511 ** | 0.460 ** | 0.438 ** | 0.441 ** | 0.469 ** | 0.531 ** | 0.559 ** | 0.591 ** | 1 | |
| Ellipse area (mm2)—dominant | r | 0.649 ** | 0.662 ** | 0.646 ** | 0.585 ** | 0.713 ** | 0.614 ** | 0.761 ** | 0.683 ** | 0.606 ** | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reddy, R.S.; Tedla, J.S.; Dixit, S.; Raizah, A.; Al-Otaibi, M.L.; Gular, K.; Ahmad, I.; Sirajudeen, M.S. Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life 2022, 12, 1817. https://doi.org/10.3390/life12111817
Reddy RS, Tedla JS, Dixit S, Raizah A, Al-Otaibi ML, Gular K, Ahmad I, Sirajudeen MS. Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life. 2022; 12(11):1817. https://doi.org/10.3390/life12111817
Chicago/Turabian StyleReddy, Ravi Shankar, Jaya Shanker Tedla, Snehil Dixit, Abdullah Raizah, Mohammed Lafi Al-Otaibi, Kumar Gular, Irshad Ahmad, and Mohamed Sherif Sirajudeen. 2022. "Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome" Life 12, no. 11: 1817. https://doi.org/10.3390/life12111817
APA StyleReddy, R. S., Tedla, J. S., Dixit, S., Raizah, A., Al-Otaibi, M. L., Gular, K., Ahmad, I., & Sirajudeen, M. S. (2022). Cervical Joint Position Sense and Its Correlations with Postural Stability in Subjects with Fibromyalgia Syndrome. Life, 12(11), 1817. https://doi.org/10.3390/life12111817










