Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire® Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Study Groups
2.2.1. Control Group
2.2.2. Intervention Group
2.3. Primary and Secondary Variables
2.4. Statistical Analysis
3. Results
3.1. Patients
3.2. Impact on Quality of Life
3.3. Quality of Life of Patients Compared to the General Spanish Population
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mediano, O.; Mangado, N.G.; Montserrat, J.M.; Alonso-Álvarez, M.L.; Almendros, I.; Alonso-Fernandez, A.; Barbé, F.; Borsini, E.; Caballero-Eraso, C.; Cano-Pumarega, I.; et al. International consensus document on obstructive sleep apnea. Arch. Bronconeumol. 2022, 58, T52–T68. [Google Scholar] [CrossRef]
- Sánchez de la Torre, M.; Campos-Rodriguez, F.; Barbé, F. Obstructive sleep apnoea and cardiovascular disease. Lancet Respir. Med. 2013, 1, 61–72. [Google Scholar] [CrossRef]
- Terán-Santos, J.; Santaolalla, C.E.; Montserrat, J.M.; Jiménez, F.M.; Escribano, M.V.L.; Mirabet, E.; Rodríguez, E.V. Sleep Apnea and Driving. Recommendations for Interpreting Spanish Regulations for Drivers. Arch. Bronconeumol. 2017, 53, 336–341. [Google Scholar] [CrossRef]
- Bjornsdottir, E.; Keenan, B.; Eysteinsdottir, B.; Arnardottir, E.; Janson, C.; Gislason, T.; Sigurdsson, J. Quality of life among untreated sleep apnea patients compared to the general population and changes after treatment with positive airway pressure. J. Sleep Res. 2015, 24, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Durán, J.; Esnaola, S.; Rubio, R. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am. J. Respir. Crit. Care Med. 2001, 163, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.P.; Ayappa, I.A.; Caples, S.M.; Kimoff, R.J.; Patel, S.R.; Harrod, C.G. Treatment of adult obstructive sleep apnea with positive airway pressure: An American Academy of Sleep Medicine clinical practice guideline. J. Clin. Sleep Med. 2019, 15, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Waever, T.; Grunstrin, R. Adherence to continuous positive airway pressure therapy. Proc. Am. Thorac. Soc. 2008, 5, 173–178. [Google Scholar] [CrossRef]
- Salepci, B.; Caglayan, B.; Kiral, N.; Sarac, G.; Fidan, A.; Parmaksiz, E.T.; Comert, S.S.; Gungor, G.A. CPAP adherence of patients with obstructive sleep apnea. Respir. Care 2013, 58, 1467–1473. [Google Scholar] [CrossRef] [PubMed]
- Strollo, P.J., Jr.; Soose, R.J.; Maurer, J.T.; De Vries, N.; Cornelius, J.; Froymovich, O.; Hanson, R.D.; Padhya, T.A.; Steward, D.L.; Gillespie, M.B.; et al. Upper-Airway Stimulation for Obstructive Sleep Apnea. N. Engl. J. Med. 2014, 370, 139–149. [Google Scholar] [CrossRef]
- Orrego, J.P.C.; de Santos, M.M.P.; Gómez, A.I.H.; Matos, S.L. Sistemas de Estimulación del Nervio Hipogloso para el Tratamiento de la Apnea Obstructiva del Sueño; Agencia de Evaluación de Tecnologías Sanitarias (AETS)—Instituto de Salud Carlos III: Madrid, Spain, 2017; Ministerio de Ciencia, Innovación y Universidades (antes Ministerio de Economía, Industria y Competitividad): Madrid, Spain, 2019. [Google Scholar]
- Heiser, C.; Edenharter, G.; Bas, M.; Wirth, M.; Hofauer, B. Palatoglossus coupling in selective upper airway stimulation. Laryngoscope 2017, 127, e378–e383. [Google Scholar] [CrossRef] [PubMed]
- Woodson, B.T.; Gillespie, M.B.; Soose, R.J.; Maurer, J.T.; de Vries, N.; Steward, D.L. Randomized controlled withdrawal study of upper airway stimulation on OSA: Short- and long-term effect. Otolaryngol. Head Neck Surg. 2014, 151, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Woodson, B.T.; Soose, R.J.; Gillespie, M.B.; Strohl, K.P.; Maurer, J.T.; de Vries, N. Three-Year Outcomes of Cranial Nerve Stimulation for Obstructive Sleep Apnea: The STAR Trial. Otolaryngol. Head Neck Surg. 2016, 154, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Heiser, C.; Steffen, A.; Hofauer, B.; Mehra, R.; Strollo, P.; Vanderveken, O.; Maurer, J. Effect of Upper Airway Stimulation in Patients with Obstructive Sleep Apnea (EFFECT): A Randomized Controlled Crossover Trial. J. Clin. Med. 2021, 10, 2880. [Google Scholar] [CrossRef]
- Baptista, P.; Garaycochea, O.; Álvarez-Gómez, L.; Alcalde, J.; Alegre, M.; Urrestarazu, E. Hypoglossal nerve stimulation surgery for obstructive sleep apnoea: Our preliminary experience. Acta Otorrinolaringol. Esp. 2018, 69, 42–47. [Google Scholar] [CrossRef]
- Maresch, K.J. Hypoglossal Nerve Stimulation: Effective Longterm Therapy for Obstructive Sleep Apnea. AANA J. 2018, 86, 412–416. [Google Scholar]
- Costantino, A.; Rinaldi, V.; Moffa, A.; Luccarelli, V.; Bressi, F.; Cassano, M.; Casale, M.; Baptista, P. Hypoglossal nerve stimulation long-term clinical outcomes: A systematic review and meta-analysis. Sleep Breath 2020, 24, 399–411. [Google Scholar] [CrossRef]
- Baptista, P.M.; Costantino, A.; Moffa, A.; Rinaldi, V.; Casale, M. Hypoglossal Nerve Stimulation in the Treatment of Obstructive Sleep Apnea: Patient Selection and New Perspectives. Nat. Sci. Sleep 2020, 12, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Baptista, P.; Prieto-Matos, C.; Alegre-Esteban, M.; Urrestarazu-Bolumbur, E.; Alcalde, J. Hypoglossal nerve stimulation for obstructive sleep apnea in Spain—Implementation strategy and early results in a tertiary care center. Indian J. Otolaryngol. Head Neck Surg. 2021, 74, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Schmidlin, M.; Fritsch, K.; Mateos, F.; Thurnheer, R.; Sen, O.; Bloch, K. Utility indices in patients with the obstructive sleep apnea syndrome. Respiration 2010, 79, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Jurado, J.; Jiménez, A.; Ordóñez, I.; Roldán, B.; Chica, M.; Rueda, M.; Feu, N. Efecto del ejercicio sobre la somnolencia y calidad de vida en pacientes con apneas del sueño sin indicación de tratamiento con CPAP. Rev. Esp. Patol. Torac. 2015, 27, 201–207. [Google Scholar]
- Rollón-Mayordomo, A.; Rollón-Ugalde, V.; López-Jiménez, A.M.; Infante-Cossio, P. Diferencia mínima clínica importante en calidad de vida relacionada con la salud. Rev. Esp. Salud Pública 2021, 95, e1-14X. [Google Scholar]
- Kazis, L.E.; Anderson, J.J.; Meenan, R.F. Effect sizes for interpreting changes in health status. Med. Care 1989, 27 (Suppl. 3), S178–S189. [Google Scholar] [CrossRef] [PubMed]
- Departamento de Economía. Universidad Carlos III de Madrid. Economía Aplicada: Estimador de Diferencias en Diferencias Disponible en. Available online: https://www.eco.uc3m.es/docencia/EconomiaAplicada/materiales/Tema42_DID.pdf (accessed on 14 March 2022).
- Gertler, P.; Martínez, S.; Premand, P.; Rawlings, L.; Vermeersch, C. Diferencias en diferencias. In Impact Evaluation in Practice, 2nd ed.; Banco Internacional para la Reconstrucción y el Desarrollo/Banco Mundial: Washington, DC, USA, 2017; pp. 143–158. [Google Scholar]
- Szende, A.; Janssen, B.; Cabases, J. (Eds.) Self-Reported Population Health: An International Perspective Based on EQ-5D, 1st ed.; Springer: Berlin/Heidelberg, Germany; New York, NY, USA, 2014; pp. 47–152. [Google Scholar]
- Ministerio de Sanidad, Servicios Sociales e Igualdad; Encuesta Nacional de Salud. España 2011/12. Calidad de Vida Relacionada con la Salud en Adultos: EQ-5D-5L; Serie Informes Monográficos nº 3; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2014; pp. 53–82. [Google Scholar]
- Kompelli, A.; Ni, J.; Nguyen, S.; Lentsch, E.; Neskey, D.; Meyer, T. The outcomes of hypoglossal nerve stimulation in the management of OSA: A systematic review and meta-analysis. World J. Otorhinolaryngol. Head Neck Surg. 2018, 5, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Kent, D.; Carden, K.; Wang, L.; Lindsell, C.; Ishman, S. Evaluation of Hypoglossal Nerve Stimulation Treatment in Obstructive Sleep Apnea. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 1044–1052. [Google Scholar] [CrossRef]
- Coman, A.; Borzan, C.; Vesa, C.; Todea, D. Obstructive sleep apnea syndrome and the quality of life. Clujul. Med. 2016, 89, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Lloberes, P.; Martí, S.; Sampol, G.; Roca, A.; Sagales, T.; Muñoz, J. Predictive Factors of Quality of Life Improvement and Continuous Positive Airway Pressure Use in Patients with Sleep Apnea-Hypopnea Syndrome: Study at 1 Year. Chest 2004, 126, 1241–1247. [Google Scholar] [CrossRef] [PubMed]
- Batool-Anwar, S.; Goodwin, J.; Kushida, C.; Walsh, J.; Simon, R.; Nichols, D. Impact of continuous positive airway pressure (CPAP) on quality of life in patients with obstructive sleep apnea (OSA). J. Sleep Res. 2006, 25, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Timkova, V.; Nagyova, I.; Reijneveld, S.A.; Tkacova, R.; van Dijk, J.P.; Bültmann, U. Quality of life of obstructive sleep apnoea patients receiving continuous positive airway pressure treatment: A systematic review and meta-analysis. Heart Lung 2020, 49, 10–24. [Google Scholar] [CrossRef]
- EUnetHTA OTCA21 Authoring Team. Hypoglossal Nerve Stimulation Systems for Treatment of Obstructive Sleep Apnea; Collaborative Assessment, EUnetHTA: Diemen, The Netherlands, 2020; Report No.: OTCA21; Available online: http://www.eunethta.eu (accessed on 24 April 2022).
- National Institute for Health and Care Excellence (NICE). Hypoglossal Nerve Stimulation for Moderate to Severe Obstructive Sleep Apnea. 2017. Available online: https://www.nice.org.uk/guidance/IPG598/chapter/1-Recommendations (accessed on 24 April 2022).
- Haute Autorité de Santé. Inspire IV UAS. Saint-Denis La Plaine: HAS. 2022. Available online: https://www.has-sante.fr/jcms/p_3327279/fr/inspire-iv-uas-avis-de-la-cnedimts-du-29/03/2022 (accessed on 24 April 2022).
- Zorginstituut Nederland. Standpunt Nervus Hypoglossusstimulatie bij Geselecteerde Patiënten met Obstructief Slaapapneusyndroom (OSAS). Available online: https://www.zorginstituutnederland.nl/publicaties/standpunten/2017/04/25/standpunt-nervus-hypoglossus-stimulatie-bij-geselecteerde-patienten-met-obstructief-slaapapneu-syndroom (accessed on 24 October 2022).
- American Academy of Otolaryngology Head and Neck Surgery or Foundation (AAO-HNS/F). Position Statement: Hypoglossal Nerve Stimulation for Treatment of Obstructive Sleep Apnea (OSA). Revised 13 November 2019. Available online: https://www.entnet.org/content/position-statement-hypoglossal-nerve-stimulation-treatment-obstructive-sleep-apnea-osa (accessed on 24 April 2022).
- U.S. Food and Drug Administration (FDA) Center for Devices and Radiological Health. 510(k). Premarket Notification Database. Available online: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm (accessed on 24 April 2022).
| Variable | Total (n = 66) | IGr (n = 22) | CGr (n = 44) | p |
|---|---|---|---|---|
| Sex, male (%) | 84.8 (4.4) | 90.9 (6.1) | 81.8 (5.8) | 0.476 |
| Age (years) | 53.5 (13.0) | 51.7 (11.2) | 54.0 (13,9) | 0.490 |
| BMI (kg/m2) | 28.7 (4,6) | 28.1 (3.7) | 29.05 (5.0) | 0.456 |
| AHI (events/hour) | 39.7 (20.1) | 42.9 (21.1) | 43.7 (24.7) | 0.928 |
| ESS (SD) | 11 (5.3) | 12.1 (5.1) | 10.4 (5.4) | 0.227 |
| HTN, % (SD) | 40.9 (6.1) | 50.0 (10.7) | 36.4 (7.3) | 0.304 |
| DM, % (SD) | 21.2 (5.0) | 18.2 (8.2) | 22.7 (6.3) | 0.759 |
| MI, % (SD) | 9.1 (3.5) | 9.1 (6.1) | 9.1 (4.3) | 1.000 |
| Asthma, % (SD) | 21.2 (5.0) | 27.3 (9.5) | 18.2 (5.8) | 0.524 |
| COPD, % (SD) | 6.1 (2.9) | 9.1 (6.1) | 4.5 (3.1) | 0.596 |
| CRF, % (SD) | 6.1 (2.9) | 4.5 (4.4) | 6.8 (3.8) | 1.000 |
| Dyslipidemia, % (SD) | 47.0 (6.1) | 50.0 (10.7) | 45.5 (7.5) | 0.797 |
| Cognitive failure, % (SD) | 4.5 (2.6) | 4.5 (4.4) | 4.5 (3.1) | 1.000 |
| Chronic pain, % (SD) | 18.2 (4.7) | 31.8 (9.9) | 11.4 (4.8) | 0.086 |
| RLS, % (D SD E) | 21.2 (5.0) | 22.7 (8.9) | 20.5 (6.1) | 1.000 |
| CPAP previous, % (SD) | 78.8 (5.06) | 86.4 (7.3) | 75.0 (6.5) | 0.354 |
| Daily use de CPAP, % (SD) | 21.2 (5.0) | 13.6 (7.3) | 25.0 (6.5) | 0.354 |
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
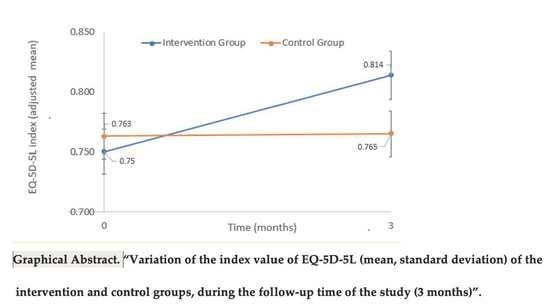
| Group | Mean | SD | Mean | SD |
| IGr-pre | 0.764 | 0.190 | 0.750 | 0.061 |
| CGr-pre | 0.733 | 0.205 | 0.763 | 0.060 |
| IGr-post | 0.935 | 0.101 | 0.814 | 0.056 |
| CGr-post | 0.727 | 0.200 | 0.765 | 0.063 |
| Dimension | Intervention, %; (SD) | Control, % (SD) | Difference, % (SD) | p |
|---|---|---|---|---|
| Mobility | 95.5 (21.3) | 68.2 (47.1) | 27.3 (8.4) | 0.002 * |
| Self-care | 100.0 (0) | 77.3 (42.4) | 22.7 (6.4) | 0.001 * |
| Usual activities | 81.8 (39.5) | 22.7 (42.4) | 59.1 (10.6) | 0.000 * |
| Pain/discomfort | 72.7 (45.6) | 43.2 (50.1) | 29.5 (12.3) | 0.020 * |
| Anxiety/Depression | 77.3 (42.9) | 22.7 (42.9) | 54.5 (11.2) | 0.000 * |
| Utility Index | Difference with Spanish Population: Mean (95% CI) | p |
|---|---|---|
| Intervention | 0.012 (−0.03 to 0.057) | 0.578 ** |
| Control | −0.196 (−0.257 to −0.135) | <0.001 * |
| Variable | Spanish Population (n = 66) % | Difference with IGr (n = 22) % (95% CI) | Difference with CGr (n = 44) % (95% CI) |
|---|---|---|---|
| Mobility | 91.9 | 3.5 (−5.9 to 13.0) ** | −23.7 (−38.1 to −9.4) * |
| Self-care | 97.8 | 2.2 (n.a.) | −20.5 (−33.4 to −7.6) * |
| Usual activities | 94.8 | −13.0 (−30.5 to 4.5) ** | −72.1 (−85.0 to −59.2) * |
| Pain/discomfort | 81.9 | −9.1 (−29.3 to 11.1) ** | −38.7 (−53.9 to −23.4) * |
| Anxiety/Depression | 86.4 | −9.1 (−28.2 to 9.9) ** | −63.7 (−76.6 to −50.8) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baptista, P.; Di Frisco, I.M.; Urrestarazu, E.; Alcalde, J.; Alegre, M.; Sanchez, I.; O’Connor-Reina, C.; Plaza, G. Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire® Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy. Life 2022, 12, 1737. https://doi.org/10.3390/life12111737
Baptista P, Di Frisco IM, Urrestarazu E, Alcalde J, Alegre M, Sanchez I, O’Connor-Reina C, Plaza G. Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire® Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy. Life. 2022; 12(11):1737. https://doi.org/10.3390/life12111737
Chicago/Turabian StyleBaptista, Peter, I. Madeleine Di Frisco, Elena Urrestarazu, Juan Alcalde, Manuel Alegre, Isabel Sanchez, Carlos O’Connor-Reina, and Guillermo Plaza. 2022. "Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire® Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy" Life 12, no. 11: 1737. https://doi.org/10.3390/life12111737
APA StyleBaptista, P., Di Frisco, I. M., Urrestarazu, E., Alcalde, J., Alegre, M., Sanchez, I., O’Connor-Reina, C., & Plaza, G. (2022). Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire® Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy. Life, 12(11), 1737. https://doi.org/10.3390/life12111737