The Impact of a Nanocellulose-Based Wound Dressing in the Management of Thermal Injuries in Children: Results of a Retrospective Evaluation
Abstract
1. Introduction
2. Results
2.1. Patients
2.2. Duration of Hospital Stay and Dressing Changes
2.3. Infection and Complications
2.4. Reepithelialization and Need for Further Treatments
2.5. Scar Formation, Pain, and Itchiness
3. Discussion
3.1. Infection and Complications
3.2. Cost Effectiveness
3.3. Reepithelialization and Need for Further Treatments
3.4. Limitations
4. Materials and Methods
4.1. Patients
4.2. Data
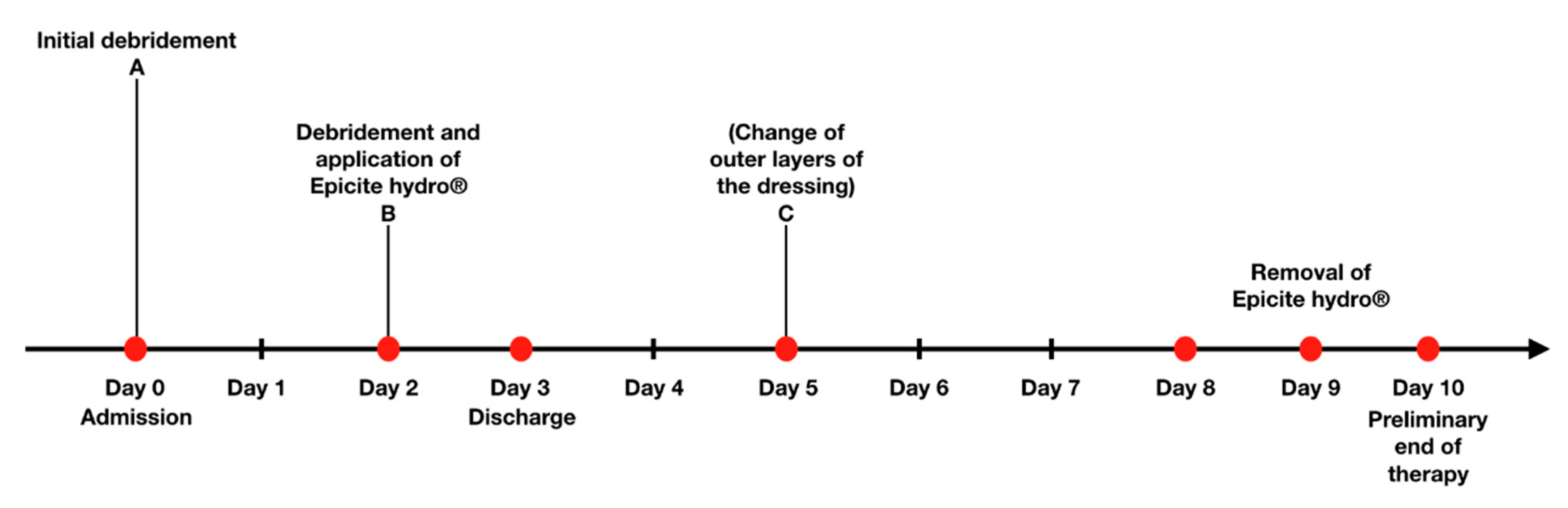
4.3. Treatment Protocol
4.4. Statistical Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AWMF | Arbeitsgemeinschaft der wissenschaftlich medizinischen Fachgesellschaften e.V |
| DTB | Deep, partial- or full-thickness burn |
| SPTB | Superficial, partial-thickness burn |
| TBSA | Total body surface area (%) |
| VSS | Vancouver Scar Scale |
References
- Deutsche Gesellschaft für Verbrennungsmedizin. Available online: https://www.verbrennungsmedizin.de/files/dgv_files/pdf/jahresbericht/Jahresbericht%20VR%202019%20gesamt.pdf (accessed on 18 September 2020).
- Thermische Verletzungen im Kindesalter (Verbrennung, Verbrühung), Behandlung. Available online: https://www.dgpraec.de/wp-content/uploads/2018/03/S2k_Leitlinie_Verbrennung_Kind.pdf (accessed on 18 September 2020).
- Schwarze, H.; Küntscher, M.; Uhlig, C.; Hierlemann, H.; Prantl, L.; Noack, N.; Hartmann, B. Suprathel®, a new skin substitute, in the management of donor sites of split-thickness skin grafts: Results of a clinical study. Burns 2007, 33, 850–854. [Google Scholar] [PubMed]
- Shores, J.T.; Gabriel, A.; Gupta, S. Skin substitutes and alternatives: A review. Adv. Skin Wound Care 2007, 20, 493–508. [Google Scholar] [PubMed]
- Fan, C.; Pek, C.H.; Por, Y.C.; Lim, G.J.S. Biobrane dressing for paediatric burns in Singapore: A retrospective review. Singap. Med. J. 2018, 59, 360. [Google Scholar]
- Cubison, T.C.; Pape, S.A.; Parkhouse, N. Evidence for the link between healing time and the development of hypertrophic scars (HTS) in paediatric burns due to scald injury. Burns 2006, 32, 992–999. [Google Scholar] [PubMed]
- Singer, A.J.; Boyce, S.T. Burn wound healing and tissue engineering. J. Burn Care Res. 2017, 38, e605–e613. [Google Scholar] [PubMed]
- Fu, L.; Zhou, P.; Zhang, S.; Yang, G. Evaluation of bacterial nanocellulose-based uniform wound dressing for large area skin transplantation. Mater. Sci. Eng. 2013, 33, 2995–3000. [Google Scholar]
- Picheth, G.F.; Pirich, C.L.; Sierakowski, M.R.; Woehl, M.A.; Sakakibara, C.N.; De Souza, C.F.; Martin, A.A.; Da Silva, R.; De Freitas, R. Bacterial cellulose in biomedical applications: A review. Int. J. Biol. Macromol. 2017, 104, 97–106. [Google Scholar]
- Anton-Sales, I.; Beekmann, U.; Laromaine, A.; Roig, A.; Kralisch, D. Opportunities of Bacterial Cellulose to Treat Epithelial Tissues. Curr. Drug Targets 2019, 20, 808–822. [Google Scholar]
- Picheth, G.F.; Sierakowski, M.R.; Woehl, M.A.; Ono, L.; Cofré, A.R.; Vanin, L.P.; Pontarolo, A.; De Freitas, R.A. Lysozyme-triggered epidermal growth factor release from bacterial cellulose membranes controlled by smart nanostructured films. J. Pharm. Sci. 2014, 103, 3958–3865. [Google Scholar]
- Klemm, D.; Cranston, E.D.; Fischer, D.; Gama, M.; Kedzior, S.A.; Kralisch, D.; Kramer, F.; Kondo, T.; Lindstrom, T.; Nietzsche, T.; et al. Nanocellulose as a natural source for groundbreaking applications in materials science: Today’s state. Mater. Today 2018, 21, 720–748. [Google Scholar]
- Uhlig, C.; Rapp, M.; Hartmann, B.; Hierlemann, H.; Planck, H.; Dittel, K.-K. Suprathel®—An innovative, resorbable skin substitute for the treatment of burn victims. Burns 2007, 33, 221–229. [Google Scholar] [CrossRef] [PubMed]
- QRSkin. Epicite Hydro 2019. Available online: https://www.qrskin.com/epicite-hydro-for-skin-graft-surgery/properties.html (accessed on 18 September 2020).
- De Mattos, I.B.; Holzer, J.C.; Tuca, A.-C.; Groeber-Becker, F.; Funk, M.; Pop, D.; Mautner, S.; Birngruber, T.; Kamolz, L.-P. Uptake of PHMB in a bacterial nanocellulose-based wound dressing: A feasible clinical procedure. Burns 2019, 45, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Holzer, J.C.; Tiffner, K.; Kainz, S.; Reisenegger, P.; De Mattos, I.B.; Funk, M.; Lemarchand, T.; Laaff, H.; Bal, A.; Birngruber, T.; et al. A novel human ex-vivo burn model and the local cooling effect of a bacterial nanocellulose-based wound dressing. Burns 2020. [Google Scholar] [CrossRef] [PubMed]
- Bernardelli de Mattos, I.; Nischwitz, S.P.; Tuca, A.C.; Groeber-Becker, F.; Funk, M.; Birngruber, T.; Mautner, S.I.; Kamolz, L.-P.; Holzer, J.K.J. Delivery of antiseptic solutions by a bacterial cellulose wound dressing: Uptake, release and antibacterial efficacy of octenidine and povidone-iodine. Burns 2020, 46, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Moritz, S.; Wiegand, C.; Wesarg, F.; Hessler, N.; Müller, F.A.; Kralisch, D. Active wound dressings based on bacterial nanocellulose as drug delivery system for octenidine. Int. J. Phmarm. 2014, 471, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Rashaan, Z.; Krijnen, P.; Allema, J.; Vloemans, A.; Schipper, I.; Breederveld, R. Usability and effectiveness of Suprathel® in partial thickness burns in children. Eur. J. Trauma Emerg. Surg. 2017, 43, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Aboelnaga, A.; Elmasry, M.; Adly, O.A.; Elbadawy, M.A.; Abbas, A.H.; Abdelrahman, I.; Salah, O.; Steinvall, I. Microbial cellulose dressing compared with silver sulphadiazine for the treatment of partial thickness burns: A prospective, randomised, clinical trial. Burns 2018, 44, 1982–1988. [Google Scholar] [CrossRef]
- Cavalcanti, L.; Pinto, F.; Oliveira, G.; Lima, S.; Aguiar, J.; Lins, E. Efficacy of bacterial cellulose membrane for the treatment of lower limbs chronic varicose ulcers: A randomized and controlled trial. Rev. Col. Bras. Cir. 2017, 44, 72–80. [Google Scholar] [CrossRef]
- Czaja, W.; Krystynowicz, A.; Bielecki, S.; Brown, R.M., Jr. Microbial cellulose—The natural power to heal wounds. Biomaterials 2006, 27, 145–151. [Google Scholar] [CrossRef]
- Kee, E.G.; Kimble, R.M.; Cuttle, L.; Stockton, K. Comparison of three different dressings for partial thickness burns in children: Study protocol for a randomised controlled trial. Trials 2013, 14, 403. [Google Scholar] [CrossRef]
- Everett, M.; Massand, S.; Davis, W.; Burkey, B.; Glat, P. Use of a copolymer dressing on superficial and partial-thickness burns in a paediatric population. J. Wound Care 2015, 24, S4–S8. [Google Scholar] [CrossRef] [PubMed]
- Deitch, E.A.; Wheelahan, T.M.; Rose, M.P.; Clothier, J.; Cotter, J. Hypertrophic burn scars: Analysis of variables. J. Trauma 1983, 23, 895–898. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.M.; Sood, R.F.; Honari, S.; Carrougher, G.J.; Gibran, N.S. What score on the Vancouver Scar Scale constitutes a hypertrophic scar? Results from a survey of North American burn-care providers. Burns 2015, 41, 1442–1448. [Google Scholar] [CrossRef] [PubMed]
- Lund, C.C. The estimation of areas of burns. Surg. Gynecol. Obstet. 1944, 79, 352–358. [Google Scholar]
- Sullivan, T.; Smith, J.; Kermode, J.; Mclver, E.; Courtemanche, D. Rating the burn scar. J. Burn Care Rehabil. 1990, 11, 256–260. [Google Scholar] [CrossRef]

| Age (Years), Mean (Std., Range) | 2.4 (2.89, 0–15) |
|---|---|
| Gender, n (%) | |
| Male | 40 (71) |
| Female | 16 (29) |
| Location of the accident, n (%) | |
| Domestic | 53 (94.6) |
| School/Kindergarten | 2 (3.6) |
| Child abuse | 1 (1.8) |
| Etiology of burn, n (%) | |
| Scald | 26 (46.4) |
| Contact | 27 (48.2) |
| Explosion | 2 (3.6) |
| Flame | 1 (1.8) |
| Site of burn, n (%) | |
| Arms | 17 (30.5) |
| Hands | 35 (62.5) |
| Legs | 7 (12) |
| Feet | 9 (16) |
| Head | 7 (12.5) |
| Neck | 3 (5.4) |
| Thorax (ventral) | 9 (16.1) |
| Thorax (dorsal) | 2 (3.6) |
| %TBSA, mean (std., range) | |
| 2a degree of burn (n = 51) | 2.9 (3.15, 1–20) |
| 2b degree of burn (n = 7) | 1.9 (1.86, 1–6) |
| 3 degree of burn (n = 8) | 1 (0.0, 1–1) |
| Depth of burn, n (%) | |
| SPTB | 43 (77) |
| DTB | 13 (23) |
| Parameters | SPTB (n = 43) | DTB (n = 13) | p-Value |
|---|---|---|---|
| Number of surgeries | 2.3 (0.93) | 3.4 (1.39) | 0.002 |
| mean (std.) | |||
| Duration of hospital stay (days) | 5.7 (2.24) | 9.8 (5.0) | 0.001 |
| mean (std.) | |||
| Complications, n (%) | |||
| Pain crisis | 1 (2.3) | 2 (15.4) | 0.13 |
| Pneumonia | 1 (2.3) | 0 (0) | 1.0 |
| Burn-associated infection | 0 (0) | 0 (0) | 1.0 |
| Additional treatments, n (%) | 1 (2.3) | 9 (69) | 0.001 |
| Parameters | SPTB n = 42 | DTB n = 12 | p-Value |
|---|---|---|---|
| Pigmentation, (points), n (%) | 0:42 (0) | 0:11 (91.6) | 0.22 |
| 1:0 (0) | 1:1 (8.3) | ||
| 2:0 (0) | 2:0 (0) | ||
| Vascularity, (points), n (%) | 0:40 (95.2) | 0:9 (75) | 0.03 |
| 1:1 (2.4) | 1:3 (25) | ||
| 2:1 (2.4) | 2:0 (0) | ||
| 3:0 (0) | 3:0 (0) | ||
| Scar height, (points), n (%) | 0:40 (95.2) | 0:10 (83.4) | 0.11 |
| 1:2 (4.8) | 1:1 (8.3) | ||
| 2:0 (0) | 2:1 (8.3) | ||
| 3:0 (0) | 3:0 (0) | ||
| Pliability, (points), n (%) | 0:40 (95.2) | 0:10 (83.4) | 0.14 |
| 1:0 (0) | 1:1 (8.3) | ||
| 2:2 (4.8) | 2:1 (8.3) | ||
| 3:0 (0) | 3:0 (0) | ||
| 4:0 (0) | 4:0 (0) | ||
| 5:0 (0) | 5:0 (0) | ||
| Vancouver Scar scale: cutoff ≥ 1 point, n (%) | 0:38 (91) | 0:8 (67) | 0.14 |
| 1:1 (2) | 1:2 (17) | ||
| 2:1 (2) | 2:1 (8) | ||
| 5:2 (5) | 5:0 (0) | ||
| 8:0 (0) | 8:1 (8) |
| Vancouver Scar Scale | Pigmentation | Vascularity | Scar Height (mm) | Pliability |
|---|---|---|---|---|
| 0 | Normal | Normal | Flat | Normal |
| 1 | Hypopigmentation | Pink | <2 | Soft |
| 2 | Hyperpigmentation | Red | 2–5 | Retreating |
| 3 | - | Purple | >5 | Hard/stiff |
| 4 | - | - | - | Scar-strand |
| 5 | - | - | - | Contracture |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cattelaens, J.; Turco, L.; Berclaz, L.M.; Huelsse, B.; Hitzl, W.; Vollkommer, T.; Bodenschatz, K.J. The Impact of a Nanocellulose-Based Wound Dressing in the Management of Thermal Injuries in Children: Results of a Retrospective Evaluation. Life 2020, 10, 212. https://doi.org/10.3390/life10090212
Cattelaens J, Turco L, Berclaz LM, Huelsse B, Hitzl W, Vollkommer T, Bodenschatz KJ. The Impact of a Nanocellulose-Based Wound Dressing in the Management of Thermal Injuries in Children: Results of a Retrospective Evaluation. Life. 2020; 10(9):212. https://doi.org/10.3390/life10090212
Chicago/Turabian StyleCattelaens, Julia, Laura Turco, Luc M. Berclaz, Birgit Huelsse, Wolfgang Hitzl, Tobias Vollkommer, and Karl J. Bodenschatz. 2020. "The Impact of a Nanocellulose-Based Wound Dressing in the Management of Thermal Injuries in Children: Results of a Retrospective Evaluation" Life 10, no. 9: 212. https://doi.org/10.3390/life10090212
APA StyleCattelaens, J., Turco, L., Berclaz, L. M., Huelsse, B., Hitzl, W., Vollkommer, T., & Bodenschatz, K. J. (2020). The Impact of a Nanocellulose-Based Wound Dressing in the Management of Thermal Injuries in Children: Results of a Retrospective Evaluation. Life, 10(9), 212. https://doi.org/10.3390/life10090212







