Allergen-Specific IgE and IgG4 as Biomarkers for Immunologic Changes during Subcutaneous Allergen Immunotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Allergy Diagnosis In Vivo
2.3. Allergen-Specific Immunotherapy
2.4. Allergen-Specific IgE and IgG4 Determination
2.5. Statistical Analysis
3. Results
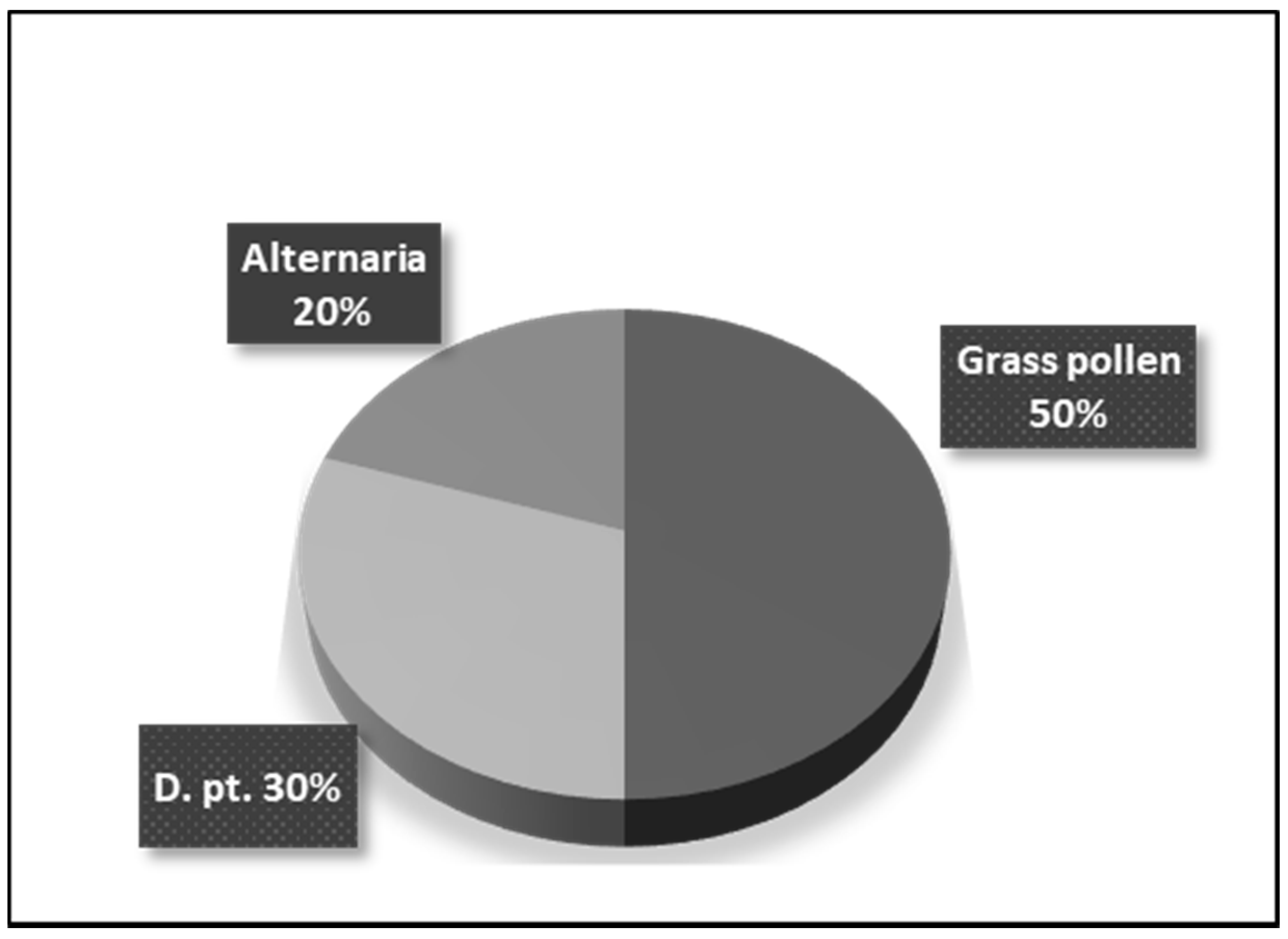
3.1. Determination of Specific Sensitization of Patients with Respiratory Allergy
3.2. Changes of sIgE Levels after SCIT Using ImmunoCAP
3.3. Changes of sIgG4 Levels after SCIT Using ImmunoCAP
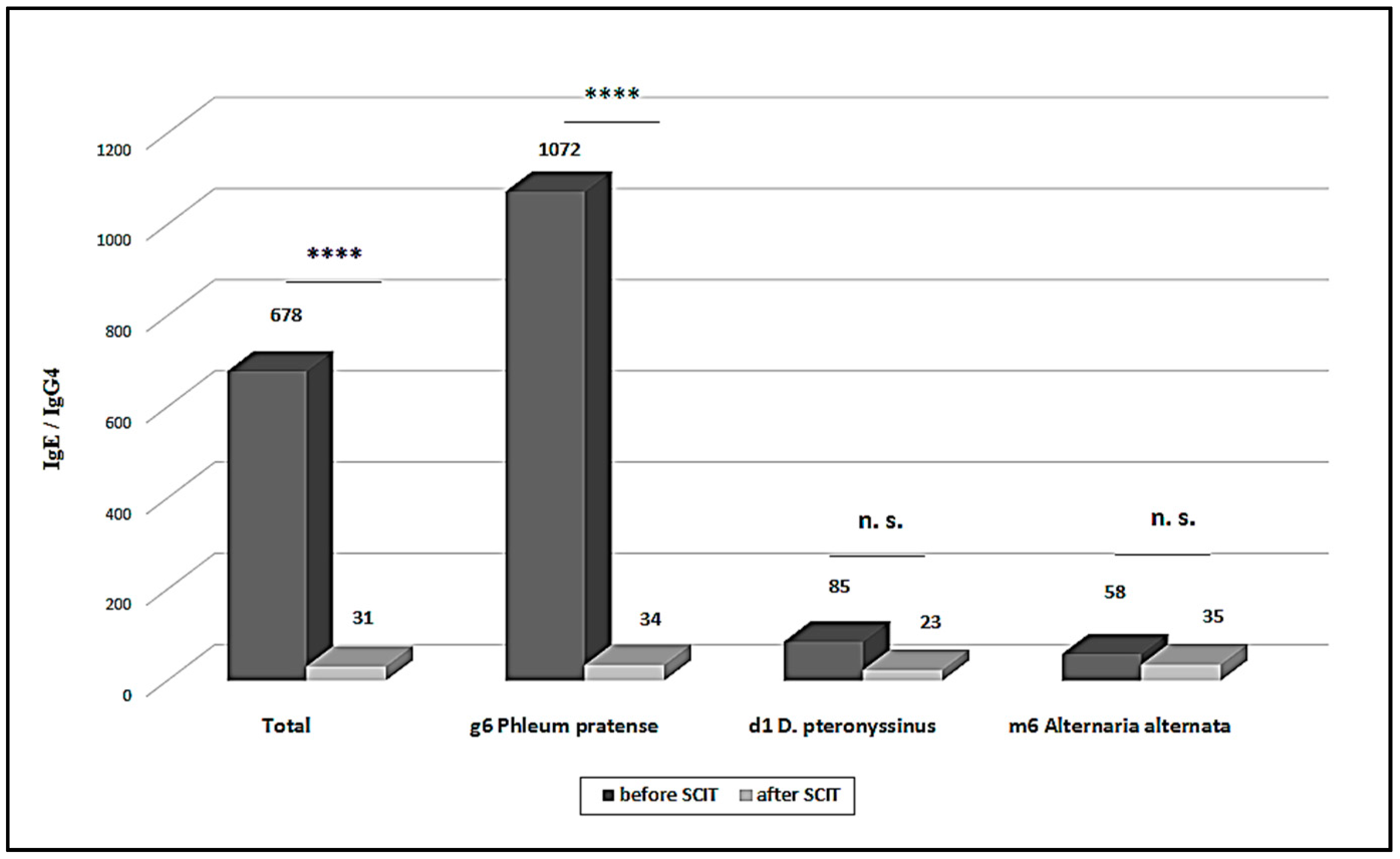
3.4. sIgE/sIgG4 Ratio
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, S.H.; Shin, S.Y.; Lee, K.H.; Kim, S.W.; Cho, J.S. Long-term effects of specific allergen immunotherapy against house dust mites in polysensitized patients with allergic rhinitis. Allergy Asthma Immunol. Res. 2014, 6, 535–540. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jutel, M.; Kosowska, A.; Smolinska, S. Allergen immunotherapy: Past, present, and future. Allergy Asthma Immunol. Res. 2016, 8, 191–197. [Google Scholar] [CrossRef]
- Akdis, C.A.; Akdis, M. Mechanisms of allergen-specific immunother apy and immune tolerance to allergens. World Allergy Organ. J. 2015, 8, 17. [Google Scholar] [CrossRef]
- Shamji, M.H.; Ljørring, C.; Francis, J.N.; Calderon, M.A.; Larché, M.; Kimber, I.; Frew, A.J.; Ipsen, H.; Lund, K.; Würtzen, P.A.; et al. Functional rather than immunoreactive levels of IgG4 correlate closely with clinical response to grass pollen immunotherapy. Allergy 2012, 67, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Głobińska, A.; Boonpiyathad, T.; Satitsuksanoa, P.; Kleuskens, M.; van de Veen, W.; Sokolowska, M.; Akdis, M. Mechanisms of allergen-specific immunotherapy: Diverse mechanisms of immune tolerance to allergens. Ann. Allergy Asthma Immunol. 2018, 121, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Jutel, M.; Akdis, C.A. Immunological mechanisms of allergen-specific immunotherapy. Allergy 2011, 66, 725–732. [Google Scholar] [CrossRef]
- Burks, A.W.; Calderon, M.A.; Casale, T.; Cox, L.; Demoly, P.; Jutel, M.; Nelson, H.; Akdis, C.A. Update on allergy immunotherapy: American Academy of Allergy, Asthma & Immunology/European Academy of Allergy and Clinical Immunology/PRACTALL consensus report. J. Allergy Clin. Immunol. 2013, 131, 1288–1296. [Google Scholar]
- Wachholz, P.A.; Soni, N.K.; Till, S.J.; Durham, S.R. Inhibition of allergen-IgE binding to B cells by IgG antibodies after grass pollen immunotherapy. J. Allergy Clin. Immunol. 2003, 112, 915–922. [Google Scholar] [CrossRef]
- Chen, J.; Zhou, Y.; Wang, Y.; Zheng, Y.; Lai, X.; Westermann-Clark, E.; Cho, S.H.; Kong, W. Specific immunoglobulin E and immunoglobulin G4 toward major allergens of house-dust mite during allergen-specific immunotherapy. Am. J. Rhinol. Allergy 2017, 31, 156–160. [Google Scholar] [CrossRef]
- Gomez, E.; Fernandez, T.D.; Dona, I.; Rondon, C.; Campo, P.; Gomez, F.; Salas, M.; Gonzalez, M.; Perkins, J.R.; Palomares, F.; et al. Initial immunological changes as predictors for House Dust Mite immunotherapy response. Clin. Exp. Allergy 2015, 45, 1542–1553. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.S.; Nolte, H.; Creticos, P.; Maloney, J.; Wu, J.M.; Bernstein, D.I. Efficacy and safety of timothy grass allergy immunotherapy tablet treatment in North American adults. J. Allergy Clin. Immunol. 2011, 127, 72–80. [Google Scholar] [CrossRef]
- Satoguina, J.; Weyand, E.; Larbi, J.; Hoerauf, A. T regulatory-1 cells induce IgG4 production by B cells: Role of IL-10. J. Immunol. 2005, 174, 4718–4726. [Google Scholar] [CrossRef] [PubMed]
- Nikolov, G.; Michova, A.; Hristova, M.; Kandova, Y.; Hristova, R.; Konstantinova, D.; Petrunov, B. Allergen specific immunotherapy of respiratory allergy: The clinical outcome. Int. J. Immunorehabil. 2010, 12, 13–15. [Google Scholar]
- Wurtzen, P.A.; Lund, G.; Lund, K.; Arvidsson, M.; Rak, S.; Ipsen, H. A double-blind placebo-controlled birch allergy vaccination study II: Correlation between inhibition of IgE binding, histamine release and facilitated allergen presentation. Clin. Exp. Allergy 2008, 38, 1290–1301. [Google Scholar] [CrossRef]
- Burton, O.T.; Tamayo, J.M.; Stranks, A.J.; Koleoglou, K.J.; Oettgen, H.C. Allergen-specific IgG antibody signaling through FcgRIIb promotes food tolerance. J. Allergy Clin. Immunol. 2018, 141, 189–201. [Google Scholar] [CrossRef] [PubMed]
- Aalberse, R.C.; Schuurman, J. IgG4 breaking the rules. Immunology 2002, 105, 9–19. [Google Scholar] [CrossRef]
- Shamji, M.H.; Kappen, J.H.; Akdis, M.; Jensen-Jarolim, E.; Knol, E.F.; Kleine-Tebbe, J.; Schmidt-Weber, C.B.; Bohle, B.; Chaker, A.M.; Till, S.J.; et al. Biomarkers for monitoring clinical efficacy of allergen immunotherapy for allergic rhinoconjunctivitis and allergic asthma: An EAACI position paper. Allergy 2017, 72, 1156–1173. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Caraballo, J.M.; Cardona Villa, R. Clinical and immunological changes of immunotherapy in patients with atopic dermatitis: Randomized controlled trial. ISRN Allergy 2012, 2012, 183983. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Novak, N.; Bieber, T.; Hoffmann, M.; Fölster-Holst, R.; Homey, B.; Werfel, T.; Zuberbier, T.; Sager, A. Eficacy and safety of subcutaneous allergenspecific immunotherapy with depigmented polymerized mite extract in atopic dermatitis. J. Allergy Clin. Immunol. 2012, 130, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Blumberga, G.; Groes, L.; Dahl, R. SQ-standardized house dust mite immunotherapy as an immunomodulatory treatment in patients with asthma. Allergy 2011, 66, 178–185. [Google Scholar] [CrossRef] [PubMed]
- Vickery, B.P.; Scurlock, A.M.; Kulis, M.; Steele, P.H.; Kamilaris, J.; Berglund, J.P.; Burk, C.; Hiegel, A.; Carlisle, S.; Christie, L.; et al. Sustained unresponsiveness to peanut in subjects who have completed peanut oral immunotherapy. J. Allergy Clin. Immunol. 2014, 133, 468–475. [Google Scholar] [CrossRef] [PubMed]
| Allergen | SCIT | p | |
|---|---|---|---|
| Before SCIT | After SCIT | ||
| g6 Phleum pratense | 61.38 ± 23.36 | 43.75 ± 33.71 | 0.2394 |
| d1 D. pteronyssinus | 21.18 ± 21.61 | 5.32 ± 4.21 | 0.0260 * |
| m6 Alternaria alternata | 6.96 ± 5.06 | 10.07 ± 7.02 | 0.4571 |
| TOTAL | 38.44 ± 31.07 | 25.48 ± 30.00 | 0.1190 |
| Allergen | SCIT | p | |
|---|---|---|---|
| Before SCIT | After SCIT | ||
| g6 Phleum pratense | 0.09 ± 0.05 | 1.31 ± 0.63 | <0.0001 * |
| d1 D. pteronyssinus | 0.44 ± 0.43 | 0.71 ± 1.31 | 0.4567 |
| m6 Alternaria alternata | 0.2 ± 0.14 | 0.30 ± 0.04 | 0.342 |
| TOTAL | 0.21 ± 0.28 | 0.93 ± 0.90 | <0.0001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nikolov, G.; Todordova, Y.; Emilova, R.; Hristova, D.; Nikolova, M.; Petrunov, B. Allergen-Specific IgE and IgG4 as Biomarkers for Immunologic Changes during Subcutaneous Allergen Immunotherapy. Antibodies 2021, 10, 49. https://doi.org/10.3390/antib10040049
Nikolov G, Todordova Y, Emilova R, Hristova D, Nikolova M, Petrunov B. Allergen-Specific IgE and IgG4 as Biomarkers for Immunologic Changes during Subcutaneous Allergen Immunotherapy. Antibodies. 2021; 10(4):49. https://doi.org/10.3390/antib10040049
Chicago/Turabian StyleNikolov, Georgi, Yana Todordova, Radoslava Emilova, Diana Hristova, Maria Nikolova, and Bogdan Petrunov. 2021. "Allergen-Specific IgE and IgG4 as Biomarkers for Immunologic Changes during Subcutaneous Allergen Immunotherapy" Antibodies 10, no. 4: 49. https://doi.org/10.3390/antib10040049
APA StyleNikolov, G., Todordova, Y., Emilova, R., Hristova, D., Nikolova, M., & Petrunov, B. (2021). Allergen-Specific IgE and IgG4 as Biomarkers for Immunologic Changes during Subcutaneous Allergen Immunotherapy. Antibodies, 10(4), 49. https://doi.org/10.3390/antib10040049







