The Moderating Effect of Social Participation on the Relationship between Urban Green Space and the Mental Health of Older Adults: A Case Study in China
Abstract
1. Introduction
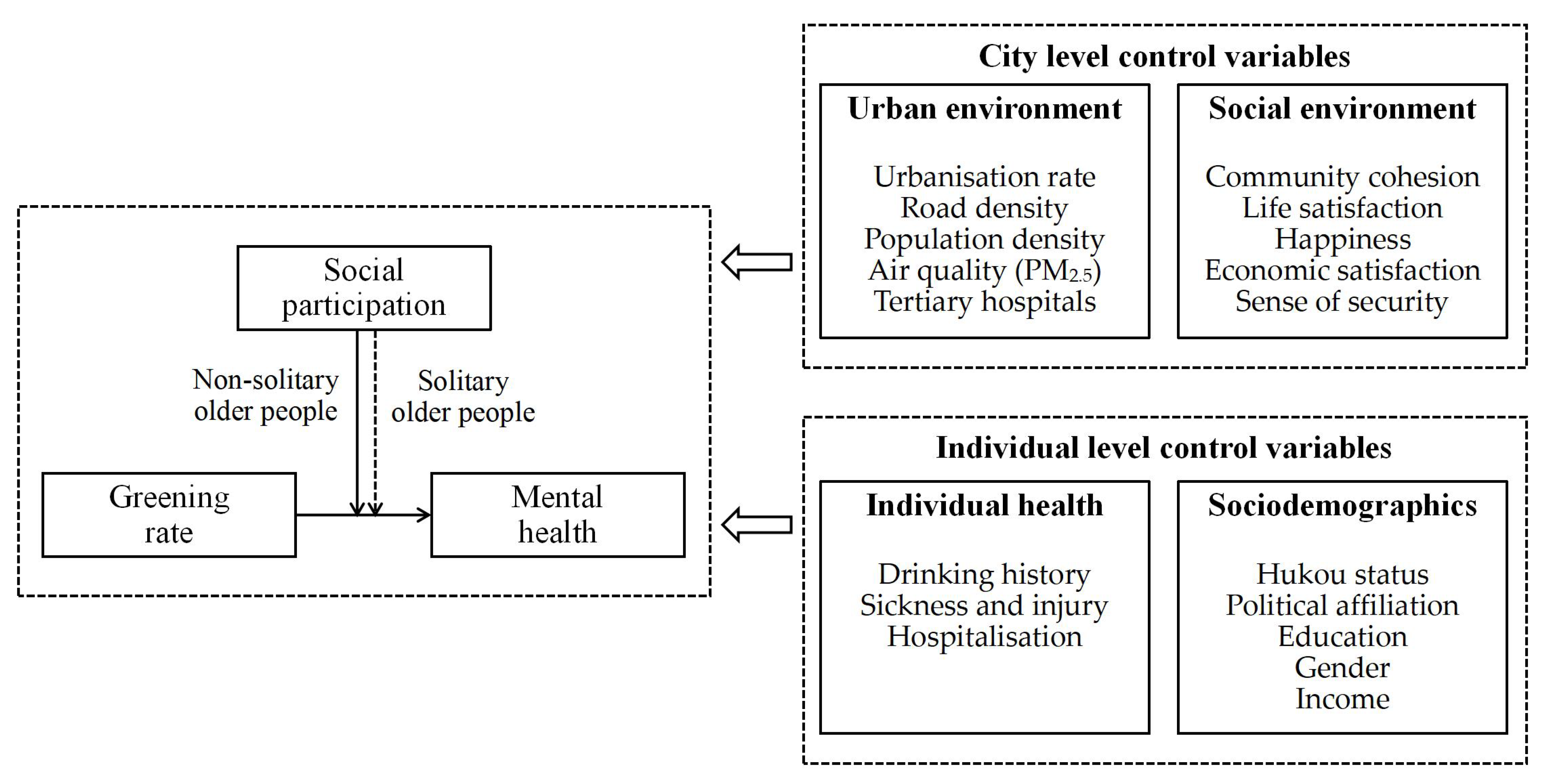
2. Literature Review
2.1. Mental Health and Its Measurements
2.2. Influencing Factors
2.2.1. Urban Environmental Factors
2.2.2. Social Environment Influencing Factors
2.3. Research on Older Adults
3. Materials and Methods
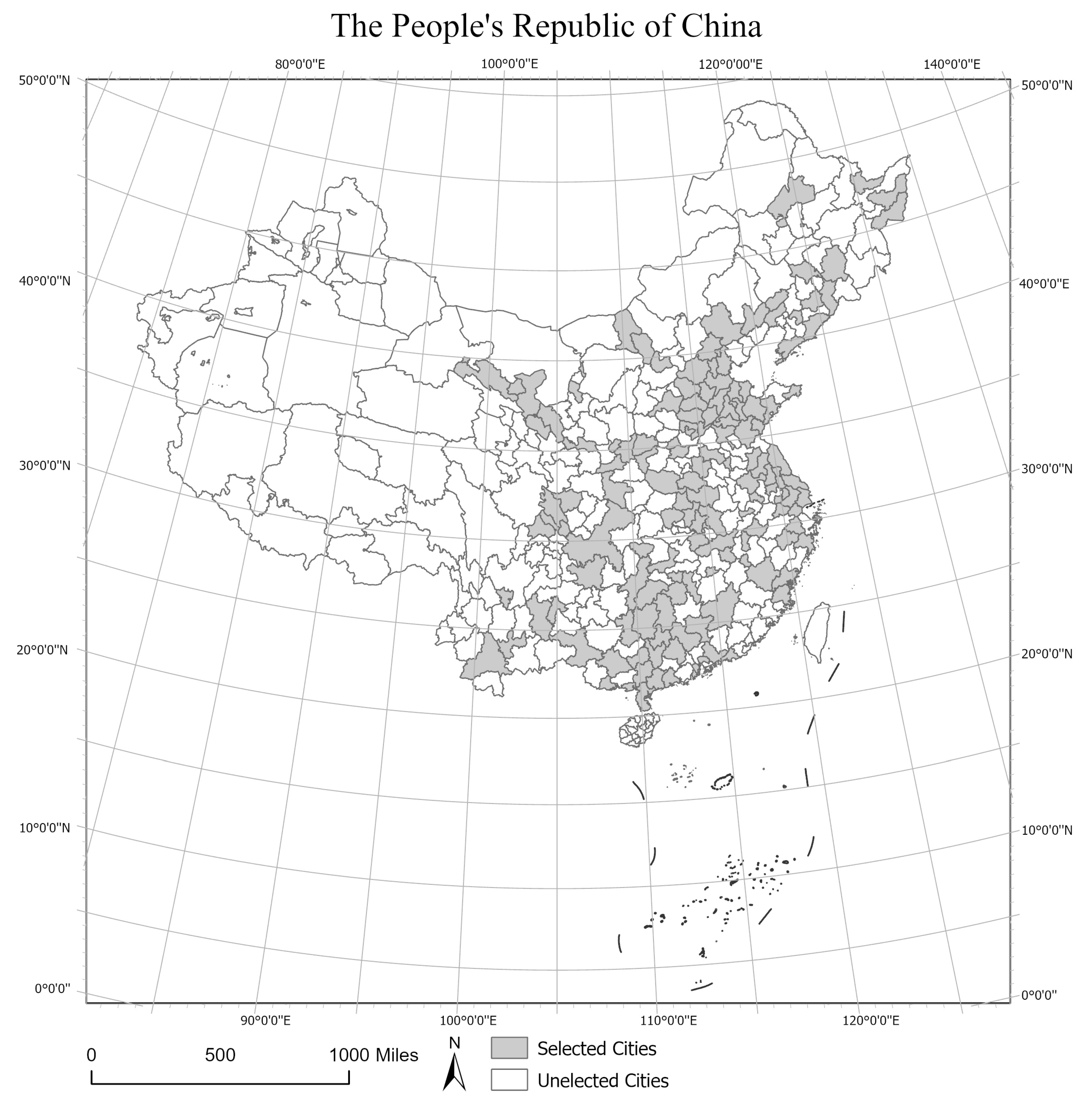
3.1. Data Sources
3.2. Variables and Measurement
3.2.1. Dependent Variables
3.2.2. Independent Variable
3.2.3. Moderating Variable
3.2.4. Control Variables
3.3. Research Methods
3.3.1. Linear Regression Model
3.3.2. Moderating Effect Analysis
4. Results
5. Discussion
5.1. Urban Green Space
5.2. Solitary and Non-Solitary Older Adults
5.3. Limitations and Future Directions
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Bureau of Statistics. Population Age Structure in China. 2019. Available online: https://data.stats.gov.cn/easyquery.htm?cn=C01 (accessed on 21 December 2023).
- Han, H.; Yang, K.; Yang, C.; Yang, G.; Xu, L. Influence and Mechanism of a Multi-Scale Built Environment on the Leisure Activities of the Elderly: Evidence from Hefei City in China. Int. J. Environ. Res. Public Health 2022, 19, 9237. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.-H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.-C. Air Pollution and Symptoms of Depression in Elderly Adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Tong, H.M.; Lai, D.W.L.; Zeng, Q.; Xu, W.Y. Effects of Social Exclusion on Depressive Symptoms: Elderly Chinese Living Alone in Shanghai, China. J. Cross Cult. Gerontol. 2011, 26, 349–364. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Vlahov, D. URBAN HEALTH: Evidence, Challenges, and Directions. Annu. Rev. Public. Health 2005, 26, 341–365. [Google Scholar] [CrossRef] [PubMed]
- Bertram, C.; Rehdanz, K. The Role of Urban Green Space for Human Well-Being. Ecol. Econ. 2015, 120, 139–152. [Google Scholar] [CrossRef]
- Beard, J.R.; Officer, A.M.; Cassels, A.K. The World Report on Ageing and Health. Gerontologist 2016, 56, S163–S166. [Google Scholar] [CrossRef] [PubMed]
- Li, B. (Ed.) Tutorial for Outline of the Healthy China 2030 Plan; Springer: Singapore, 2016; pp. 5–20. [Google Scholar]
- Wang, W.; Lin, Z.; Zhang, L.; Yu, T.; Ciren, P.; Zhu, Y. Building Visual Green Index: A Measure of Visual Green Spaces for Urban Building. Urban For. Urban Green. 2019, 40, 335–343. [Google Scholar] [CrossRef]
- Kutek, S.M.; Turnbull, D.; Fairweather-Schmidt, A.K. Rural Men’s Subjective Well-Being and the Role of Social Support and Sense of Community: Evidence for the Potential Benefit of Enhancing Informal Networks. Aust. J. Rural Health 2011, 19, 20–26. [Google Scholar] [CrossRef]
- Aliyas, Z. Physical, Mental, and Physiological Health Benefits of Green and Blue Outdoor Spaces among Elderly People. Int. J. Environ. Health Res. 2021, 31, 703–714. [Google Scholar] [CrossRef]
- Zijlema, W.L.; Stasinska, A.; Blake, D.; Dirgawati, M.; Flicker, L.; Yeap, B.B.; Golledge, J.; Hankey, G.J.; Nieuwenhuijsen, M.; Heyworth, J. The Longitudinal Association between Natural Outdoor Environments and Mortality in 9218 Older Men from Perth, Western Australia. Environ. Int. 2019, 125, 430–436. [Google Scholar] [CrossRef]
- Balfour, J.L.; Kaplan, G.A. Neighborhood Environment and Loss of Physical Function in Older Adults: Evidence from the Alameda County Study. Am. J. Epidemiol. 2002, 155, 507–515. [Google Scholar] [CrossRef]
- Lu, S.; Oh, W.; Ooka, R.; Wang, L. Effects of Environmental Features in Small Public Urban Green Spaces on Older Adults’ Mental Restoration: Evidence from Tokyo. Int. J. Environ. Res. Public Health 2022, 19, 5477. [Google Scholar] [CrossRef] [PubMed]
- Van Den Berg, M.M.; Van Poppel, M.; Van Kamp, I.; Ruijsbroek, A.; Triguero-Mas, M.; Gidlow, C.; Nieuwenhuijsen, M.J.; Gražulevičiene, R.; Van Mechelen, W.; Kruize, H.; et al. Do Physical Activity, Social Cohesion, and Loneliness Mediate the Association Between Time Spent Visiting Green Space and Mental Health? Environ. Behav. 2019, 51, 144–166. [Google Scholar] [CrossRef]
- Home, R.; Hunziker, M.; Bauer, N. Psychosocial Outcomes as Motivations for Visiting Nearby Urban Green Spaces. Leis. Sci. 2012, 34, 350–365. [Google Scholar] [CrossRef]
- Maas, J.; Van Dillen, S.M.E.; Verheij, R.A.; Groenewegen, P.P. Social Contacts as a Possible Mechanism behind the Relation between Green Space and Health. Health Place 2009, 15, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, T.; Leslie, E.; Giles-Corti, B.; Owen, N. Associations of Neighbourhood Greenness with Physical and Mental Health: Do Walking, Social Coherence and Local Social Interaction Explain the Relationships? J. Epidemiol. Community Health 2008, 62, e9. [Google Scholar] [CrossRef] [PubMed]
- Tomioka, K.; Kurumatani, N.; Hosoi, H. Positive and Negative Influences of Social Participation on Physical and Mental Health among Community-Dwelling Elderly Aged 65–70 Years: A Cross-Sectional Study in Japan. BMC Geriatr. 2017, 17, 111. [Google Scholar] [CrossRef] [PubMed]
- Chiao, C.; Weng, L.-J.; Botticello, A.L. Social Participation Reduces Depressive Symptoms among Older Adults: An 18-Year Longitudinal Analysis in Taiwan. BMC Public Health 2011, 11, 292. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, R.; Lu, Y.; Li, Z.; Chen, H.; Cao, M.; Zhang, Y.; Song, Y. Natural Outdoor Environment, Neighbourhood Social Cohesion and Mental Health: Using Multilevel Structural Equation Modelling, Streetscape and Remote-Sensing Metrics. Urban For. Urban Green. 2020, 48, 126576. [Google Scholar] [CrossRef]
- Piekut, A.; Valentine, G. Spaces of Encounter and Attitudes towards Difference: A Comparative Study of Two European Cities. Soc. Sci. Res. 2017, 62, 175–188. [Google Scholar] [CrossRef]
- Peters, K. Being Together in Urban Parks: Connecting Public Space, Leisure, and Diversity. Leis. Sci. 2010, 32, 418–433. [Google Scholar] [CrossRef]
- Maslow, A.H.; Mittelman, J.H. Principle of Abnormal Psychology. J. Nerv. Ment. Dis. 1937, 3, 335. [Google Scholar]
- Gu, D.; Zhu, H.; Brown, T.; Hoenig, H.; Zeng, Y. Tourism Experiences and Self-Rated Health Among Older Adults in China. J. Aging Health 2016, 28, 675–703. [Google Scholar] [CrossRef]
- Suldo, S.M.; Shaffer, E.J. Looking Beyond Psychopathology: The Dual-Factor Model of Mental Health in Youth. Sch. Psychol. Rev. 2008, 37, 52–68. [Google Scholar] [CrossRef]
- Ewing, R.; Cervero, R. Travel and the Built Environment: A Meta-Analysis. J. Am. Plan. Assoc. 2010, 76, 265–294. [Google Scholar] [CrossRef]
- Cervero, R.; Kockelman, K. Travel Demand and the 3Ds: Density, Diversity, and Design. Transp. Res. Part D Transp. Environ. 1997, 2, 199–219. [Google Scholar] [CrossRef]
- Barnett, D.W.; Barnett, A.; Nathan, A.; Van Cauwenberg, J.; Cerin, E.; on behalf of the Council on Environment and Physical Activity (CEPA)—Older Adults working group. Built Environmental Correlates of Older Adults’ Total Physical Activity and Walking: A Systematic Review and Meta-Analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 103. [Google Scholar] [CrossRef]
- Morenoff, J.D. Neighborhood Mechanisms and the Spatial Dynamics of Birth Weight. Am. J. Sociol. 2003, 108, 976–1017. [Google Scholar] [CrossRef]
- Pun, V.C.; Manjourides, J.; Suh, H. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environ. Health Perspect. 2017, 125, 342–348. [Google Scholar] [CrossRef]
- Liu, Y.; Dijst, M.; Faber, J.; Geertman, S.; Cui, C. Healthy Urban Living: Residential Environment and Health of Older Adults in Shanghai. Health Place 2017, 47, 80–89. [Google Scholar] [CrossRef]
- Chiou, S.-T.; Chen, L.-K. Towards Age-Friendly Hospitals and Health Services. Arch. Gerontol. Geriatr. 2009, 49, S3–S6. [Google Scholar] [CrossRef] [PubMed]
- Bilgel, F.; Karahasan, B.C. Self-Rated Health and Endogenous Selection into Primary Care. Soc. Sci. Med. 2018, 197, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Chang, P.-J. Effects of the Built and Social Features of Urban Greenways on the Outdoor Activity of Older Adults. Landsc. Urban Plan. 2020, 204, 103929. [Google Scholar] [CrossRef]
- Cleland, C.; Reis, R.S.; Ferreira Hino, A.A.; Hunter, R.; Fermino, R.C.; Koller De Paiva, H.; Czestschuk, B.; Ellis, G. Built Environment Correlates of Physical Activity and Sedentary Behaviour in Older Adults: A Comparative Review between High and Low-Middle Income Countries. Health Place 2019, 57, 277–304. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, R.; Grekousis, G.; Liu, Y.; Yuan, Y.; Li, Z. Neighbourhood Greenness and Mental Wellbeing in Guangzhou, China: What Are the Pathways? Landsc. Urban Plan. 2019, 190, 103602. [Google Scholar] [CrossRef]
- Korpela, K.M.; Ylen, M.; Tyrvainen, L.; Silvennoinen, H. Favorite Green, Waterside and Urban Environments, Restorative Experiences and Perceived Health in Finland. Health Promot. Int. 2010, 25, 200–209. [Google Scholar] [CrossRef]
- Van Den Berg, A.E.; Hartig, T.; Staats, H. Preference for Nature in Urbanized Societies: Stress, Restoration, and the Pursuit of Sustainability. J. Soc. Issues 2007, 63, 79–96. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X.; Kolt, G.S. Mental Health Benefits of Neighbourhood Green Space Are Stronger among Physically Active Adults in Middle-to-Older Age: Evidence from 260,061 Australians. Prev. Med. 2013, 57, 601–606. [Google Scholar] [CrossRef]
- Fjaestad, S.L.; Mackelprang, J.L.; Sugiyama, T.; Chandrabose, M.; Owen, N.; Turrell, G.; Kingsley, J. Associations of Time Spent Gardening with Mental Wellbeing and Life Satisfaction in Mid-to-Late Adulthood. J. Environ. Psychol. 2023, 87, 101993. [Google Scholar] [CrossRef]
- Zhang, J.; Cui, J.; Astell-Burt, T.; Shi, W.; Peng, J.; Lei, L.; Xin, X.; Zhang, J.; Feng, X.; Jiang, Y.; et al. Weekly Green Space Visit Duration Is Positively Associated with Favorable Health Outcomes in People with Hypertension: Evidence from Shenzhen, China. Environ. Res. 2022, 212, 113228. [Google Scholar] [CrossRef]
- Putra, I.G.N.E.; Astell-Burt, T.; Feng, X. Perceived Green Space Quality, Child Biomarkers and Health-Related Outcomes: A Longitudinal Study. Environ. Pollut. 2022, 303, 119075. [Google Scholar] [CrossRef] [PubMed]
- John, E.E.; Astell-Burt, T.; Yu, P.; Brennan-Horley, C.; Feng, X. Green Space Type and Healthy Ageing in Place: An Australian Longitudinal Study. Urban For. Urban Green. 2023, 84, 127903. [Google Scholar] [CrossRef]
- Feldman, R.S. Development across the Life Span, 6th ed.; Pearson Education Asia Ltd.: Beijing, China; World Publishing Corporation: Beijing, China, 2013; pp. 675–676. [Google Scholar]
- Takagi, D.; Kondo, K.; Kawachi, I. Social Participation and Mental Health: Moderating Effects of Gender, Social Role and Rurality. BMC Public Health 2013, 13, 701. [Google Scholar] [CrossRef]
- Tomioka, K.; Kurumatani, N.; Hosoi, H. Association Between Social Participation and 3-Year Change in Instrumental Activities of Daily Living in Community-Dwelling Elderly Adults. J. Am. Geriatr. Soc. 2017, 65, 107–113. [Google Scholar] [CrossRef]
- Cohen, S. Social Relationships and Health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef]
- Kawachi, I.; Berkman, L.F. Social Ties and Mental Health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Umberson, D.; Karas Montez, J. Social Relationships and Health: A Flashpoint for Health Policy. J. Health Soc. Behav. 2010, 51, S54–S66. [Google Scholar] [CrossRef]
- Shiba, K.; Torres, J.M.; Daoud, A.; Inoue, K.; Kanamori, S.; Tsuji, T.; Kamada, M.; Kondo, K.; Kawachi, I. Estimating the Impact of Sustained Social Participation on Depressive Symptoms in Older Adults. Epidemiology 2021, 32, 886–895. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a Specific Risk Factor for Depressive Symptoms: Cross-Sectional and Longitudinal Analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef]
- Feldman, R.S. Development across the Life Span, 4th ed.; Pearson Education New Zealand: Auckland, New Zealand, 2006; pp. xxvii, 773. ISBN 978-0-13-192538-0. [Google Scholar]
- Takeuchi, K.; Aida, J.; Kondo, K.; Osaka, K. Social Participation and Dental Health Status among Older Japanese Adults: A Population-Based Cross-Sectional Study. PLoS ONE 2013, 8, e61741. [Google Scholar] [CrossRef]
- Min, J.; Ailshire, J.; Crimmins, E.M. Social Engagement and Depressive Symptoms: Do Baseline Depression Status and Type of Social Activities Make a Difference? Age Ageing 2016, 45, 838–843. [Google Scholar] [CrossRef]
- Roberts, B.L.; Dunkle, R.; Haug, M. Physical, Psychological, and Social Resources as Moderators of the Relationship of Stress to Mental Health of the Very Old. J. Gerontol. 1994, 49, S35–S43. [Google Scholar] [CrossRef]
- Chou, K.-L.; Ho, A.H.Y.; Chi, I. Living Alone and Depression in Chinese Older Adults. Aging Ment. Health 2006, 10, 583–591. [Google Scholar] [CrossRef]
- Baune, B.T.; Suslow, T.; Arolt, V.; Berger, K. The Relationship between Psychological Dimensions of Depressive Symptoms and Cognitive Functioning in the Elderly—The MEMO-Study. J. Psychiatr. Res. 2007, 41, 247–254. [Google Scholar] [CrossRef]
- Bennetto, L.; Pennington, B.F.; Rogers, S.J. Intact and Impaired Memory Functions in Autism. Child Dev. 1996, 67, 1816–1835. [Google Scholar] [CrossRef]
- Adams, J.H. Perspectives of the Oldest-Old Concerning Resilience across the Life Span. Ph.D. Thesis, New Mexico State University, Las Cruces, NM, USA, 1998. [Google Scholar]
- Chou, K.-L.; Chi, I. Comparison Between Elderly Chinese Living Alone and Those Living with Others. J. Gerontol. Soc. Work. 2000, 33, 51–66. [Google Scholar] [CrossRef]
- Williams, L.; Zhang, R.; Packard, K.C. Factors Affecting the Physical and Mental Health of Older Adults in China: The Importance of Marital Status, Child Proximity, and Gender. SSM-Popul. Health 2017, 3, 20–36. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.-M.; Lee, T.M.; Chi, I. Relationship between Living Arrangements and the Psychological Well-Being of Older People in Hong Kong. Australas. J. Ageing 2004, 23, 167–171. [Google Scholar] [CrossRef]
- Wang, Q.; Zhou, Q. China’s Divorce and Remarriage Rates: Trends and Regional Disparities. J. Divorce Remarriage 2010, 51, 257–267. [Google Scholar] [CrossRef]
- Chen, X.; Silverstein, M. Intergenerational Social Support and the Psychological Well-Being of Older Parents in China. Res. Aging 2000, 22, 43–65. [Google Scholar] [CrossRef]
- Xia, H. China Population Association. Trend in the Nuclear Family Development and the Old-Age Support to the Elderly in the Market-Oriented Economic; Xin Hua Press: Beijing, China, 1997; pp. 333–340. [Google Scholar]
- Older Persons. Available online: https://emergency.unhcr.org/protection/persons-risk/older-persons (accessed on 24 December 2023).
- Indicator Definitions—Older Adults|CDI|DPH|CDC. Available online: https://www.cdc.gov/cdi/definitions/older-adults.html (accessed on 24 December 2023).
- National Bureau of Statistics of China. China Statistical Yearbook 2018; China Statistics Press: Beijing, China, 2018; ISBN 978-7-5037-8587-0.
- Van Donkelaar, A.; Hammer, M.S.; Bindle, L.; Brauer, M.; Brook, J.R.; Garay, M.J.; Hsu, N.C.; Kalashnikova, O.V.; Kahn, R.A.; Lee, C.; et al. Monthly Global Estimates of Fine Particulate Matter and Their Uncertainty. Environ. Sci. Technol. 2021, 55, 15287–15300. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Edmonston, B. Living Alone Among Older Adults in Canada and the U.S. Healthcare 2019, 7, 68. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Chen, H.; Li, Z.; Wang, R.; Liu, Y.; Qin, X. Exploring Neighborhood Environmental Effects on Mental Health: A Case Study in Guangzhou. Prog. Geogr. 2019, 38, 283–295. [Google Scholar] [CrossRef]
- Helbich, M.; Klein, N.; Roberts, H.; Hagedoorn, P.; Groenewegen, P.P. More Green Space Is Related to Less Antidepressant Prescription Rates in the Netherlands: A Bayesian Geoadditive Quantile Regression Approach. Environ. Res. 2018, 166, 290–297. [Google Scholar] [CrossRef]
- Knapp, M.R. The Activity Theory of Aging an Examination in the English Context. Gerontologist 1977, 17, 553–559. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Abdulrazaq, S. Social Engagement Mediates the Relationship between Participation in Social Activities and Psychological Distress among Older Adults. Aging Ment. Health 2021, 25, 299–305. [Google Scholar] [CrossRef]
- Sarkar, C.; Webster, C.; Gallacher, J. Healthy Cities: Public Health through Urban Planning; Edward Elgar Publishing: Cheltenham, UK, 2014; ISBN 978-1-78195-572-7. [Google Scholar]
- Zhang, L.; Zhou, S.; Kwan, M.-P. A Comparative Analysis of the Impacts of Objective versus Subjective Neighborhood Environment on Physical, Mental, and Social Health. Health Place 2019, 59, 102170. [Google Scholar] [CrossRef]
- Diener, E.; Oishi, S.; Lucas, R.E. Personality, Culture, and Subjective Well-Being: Emotional and Cognitive Evaluations of Life. Annu. Rev. Psychol. 2003, 54, 403–425. [Google Scholar] [CrossRef]
- Chen, W.; Okumiya, K.; Wada, T.; Sakamoto, R.; Imai, H.; Ishimoto, Y.; Kimura, Y.; Fukutomi, E.; Fujisawa, M.; Shih, H.-I.; et al. Social Cohesion and Health in Old Age: A Study in Southern Taiwan. Int. Psychogeriatr. 2015, 27, 1903–1911. [Google Scholar] [CrossRef]
- White, M.; Kasl, S.V.; Zahner, G.E.P.; Will, J.C. Perceived Crime in the Neighborhood and Mental Health of Women and Children. Environ. Behav. 1987, 19, 588–613. [Google Scholar] [CrossRef]
- Foster, S.; Wood, L.; Christian, H.; Knuiman, M.; Giles-Corti, B. Planning Safer Suburbs: Do Changes in the Built Environment Influence Residents’ Perceptions of Crime Risk? Soc. Sci. Med. 2013, 97, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Foster, S.; Wood, L.; Francis, J.; Knuiman, M.; Villanueva, K.; Giles-Corti, B. Suspicious Minds: Can Features of the Local Neighbourhood Ease Parents’ Fears about Stranger Danger? J. Environ. Psychol. 2015, 42, 48–56. [Google Scholar] [CrossRef]
- Guo, Y.; Liu, Y.; Lu, S.; Chan, O.F.; Chui, C.H.K.; Lum, T.Y.S. Objective and Perceived Built Environment, Sense of Community, and Mental Wellbeing in Older Adults in Hong Kong: A Multilevel Structural Equation Study. Landsc. Urban Plan. 2021, 209, 104058. [Google Scholar] [CrossRef]
- James, L.R.; Brett, J.M. Mediators, Moderators, and Tests for Mediation. J. Appl. Psychol. 1984, 69, 307–321. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, R.; Xiao, Y.; Huang, B.; Chen, H.; Li, Z. Exploring the Linkage between Greenness Exposure and Depression among Chinese People: Mediating Roles of Physical Activity, Stress and Social Cohesion and Moderating Role of Urbanicity. Health Place 2019, 58, 102168. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhou, Y.; Wang, F.; Ding, L.; Love, P.E.D.; Li, S. The Influence of the Built Environment on People’s Mental Health: An Empirical Classification of Causal Factors. Sustain. Cities Soc. 2021, 74, 103185. [Google Scholar] [CrossRef]
- Ohrnberger, J.; Fichera, E.; Sutton, M. The Dynamics of Physical and Mental Health in the Older Population. J. Econ. Ageing 2017, 9, 52–62. [Google Scholar] [CrossRef]
- Cutler, D.M.; Lleras-Muney, A. Education and Health: Evaluating Theories and Evidence; National Bureau of Economic Research: Cambridge, MA, USA, 2006. [Google Scholar]
- Wang, L.; Liu, W.; Liang, Y.; Wei, Y. Mental Health and Depressive Feeling of Empty-Nest Elderly People in China. Am. J. Health Behav. 2019, 43, 1171–1185. [Google Scholar] [CrossRef]
- Zhang, Y.; Yao, E. Exploring Elderly People’s Daily Time-Use Patterns in the Living Environment of Beijing, China. Cities 2022, 129, 103838. [Google Scholar] [CrossRef]
- Tan, T.H. Perceived Environmental Attributes: Their Impact on Older Adults’ Mental Health in Malaysia. Int. J. Environ. Res. Public Health 2022, 19, 3595. [Google Scholar] [CrossRef]
- Li, H.; Browning, M.H.E.M.; Dzhambov, A.M.; Zhang, G.; Cao, Y. Green Space for Mental Health in the COVID-19 Era: A Pathway Analysis in Residential Green Space Users. Land 2022, 11, 1128. [Google Scholar] [CrossRef]
- Clarke, P.; Ailshire, J.A.; Lantz, P. Urban Built Environments and Trajectories of Mobility Disability: Findings from a National Sample of Community-Dwelling American Adults (1986–2001). Soc. Sci. Med. 2009, 69, 964–970. [Google Scholar] [CrossRef]
- Francis, J.; Giles-Corti, B.; Wood, L.; Knuiman, M. Creating Sense of Community: The Role of Public Space. J. Environ. Psychol. 2012, 32, 401–409. [Google Scholar] [CrossRef]
- Bedimo-Rung, A.L.; Mowen, A.J.; Cohen, D.A. The Significance of Parks to Physical Activity and Public Health: A Conceptual Model. Am. J. Prev. Med. 2005, 28, 159–168. [Google Scholar] [CrossRef]
- Kroeger, T.; Escobedo, F.J.; Hernandez, J.L.; Varela, S.; Delphin, S.; Fisher, J.R.B.; Waldron, J. Reforestation as a Novel Abatement and Compliance Measure for Ground-Level Ozone. Proc. Natl. Acad. Sci. USA 2014, 111, E4204–E4213. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; Clougherty, J.E.; Shmool, J.L.C.; Kubzansky, L.D. Is All Urban Green Space the Same? A Comparison of the Health Benefits of Trees and Grass in New York City. Int. J. Environ. Res. Public Health 2017, 14, 1411. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Astell-Burt, T. Perceived Qualities, Visitation and Felt Benefits of Preferred Nature Spaces during the COVID-19 Pandemic in Australia: A Nationally-Representative Cross-Sectional Study of 2940 Adults. Land 2022, 11, 904. [Google Scholar] [CrossRef]
- Hickman, P. “Third Places” and Social Interaction in Deprived Neighbourhoods in Great Britain. J. Hous. Built Environ. 2013, 28, 221–236. [Google Scholar] [CrossRef]
- Alidoust, S.; Bosman, C. Planning for an Ageing Population: Links between Social Health, Neighbourhood Environment and the Elderly. Aust. Plan. 2015, 52, 177–186. [Google Scholar] [CrossRef]
- Neal, S.; Bennett, K.; Jones, H.; Cochrane, A.; Mohan, G. Multiculture and Public Parks: Researching Super-Diversity and Attachment in Public Green Space. Popul. Space Place 2015, 21, 463–475. [Google Scholar] [CrossRef]
- Almedom, A.M. Social Capital and Mental Health: An Interdisciplinary Review of Primary Evidence. Soc. Sci. Med. 2005, 61, 943–964. [Google Scholar] [CrossRef]
- Ertel, K.A.; Glymour, M.M.; Berkman, L.F. Effects of Social Integration on Preserving Memory Function in a Nationally Representative US Elderly Population. Am. J. Public Health 2008, 98, 1215–1220. [Google Scholar] [CrossRef] [PubMed]
- Pasanen, T.P.; White, M.P.; Elliott, L.R.; van den Bosch, M.; Bratman, G.N.; Ojala, A.; Korpela, K.; Fleming, L.E. Urban Green Space and Mental Health among People Living Alone: The Mediating Roles of Relational and Collective Restoration in an 18-Country Sample. Environ. Res. 2023, 232, 116324. [Google Scholar] [CrossRef] [PubMed]
- Kaźmierczak, A. The Contribution of Local Parks to Neighbourhood Social Ties. Landsc. Urban Plan. 2013, 109, 31–44. [Google Scholar] [CrossRef]
- Weinstein, N.; Balmford, A.; DeHaan, C.R.; Gladwell, V.; Bradbury, R.B.; Amano, T. Seeing Community for the Trees: The Links among Contact with Natural Environments, Community Cohesion, and Crime. BioScience 2015, 65, 1141–1153. [Google Scholar] [CrossRef]
- Scannell, L.; Gifford, R. The Experienced Psychological Benefits of Place Attachment. J. Environ. Psychol. 2017, 51, 256–269. [Google Scholar] [CrossRef]
- Merz, E.-M.; Consedine, N.S. The Association of Family Support and Wellbeing in Later Life Depends on Adult Attachment Style. Attach. Hum. Dev. 2009, 11, 203–221. [Google Scholar] [CrossRef] [PubMed]
- Thomas, P.A.; Liu, H.; Umberson, D. Family Relationships and Well-Being. Innov. Aging 2017, 1, igx025. [Google Scholar] [CrossRef]
- Boyd, F.; White, M.P.; Bell, S.L.; Burt, J. Who Doesn’t Visit Natural Environments for Recreation and Why: A Population Representative Analysis of Spatial, Individual and Temporal Factors among Adults in England. Landsc. Urban Plan. 2018, 175, 102–113. [Google Scholar] [CrossRef]
- Enssle, F.; Kabisch, N. Urban Green Spaces for the Social Interaction, Health and Well-Being of Older People—An Integrated View of Urban Ecosystem Services and Socio-Environmental Justice. Environ. Sci. Policy 2020, 109, 36–44. [Google Scholar] [CrossRef]
- Knight, A.; Black, R.; Whitsed, R.; Harvey, R. Enhancing the Usability and Benefits of Open Space for Older People in Regional Australia. Aust. Plan. 2018, 55, 73–83. [Google Scholar] [CrossRef]
| Characteristic | Total | Non-Solitary | Solitary |
|---|---|---|---|
| Total number | 3501 | 3199 | 302 |
| Mean age (years) | 67.72 | 67.55 | 69.5 |
| Sex (%) | |||
| Male | 40.7 | 40.7 | 40.7 |
| Female | 59.3 | 59.3 | 59.3 |
| CPC membership (%) | |||
| Member | 6.8 | 6.8 | 6.6 |
| Non-member | 93.2 | 93.2 | 93.4 |
| Hukou (%) | |||
| Local | 94.9 | 94.8 | 95.7 |
| Non-local | 5.1 | 5.2 | 4.3 |
| Education (%) | |||
| Primary school or below | 61.2 | 60.9 | 64.6 |
| Junior high school | 23.5 | 23.9 | 18.5 |
| High school | 13.2 | 13 | 14.9 |
| College or above | 2.1 | 2.1 | 2 |
| Income (%) | |||
| 0–50,000 | 56 | 55 | 56.8 |
| 50,000–100,000 | 4.4 | 3 | 4.5 |
| 100,000–200,000 | 0.2 | 0.7 | 0.2 |
| 200,000 or above | 38.7 | 41.3 | 38.5 |
| Category | Mean Value | T-Value | p-Value | |
|---|---|---|---|---|
| Sex | Male | 72.88 | 4.805 | 0.000 |
| Female | 71.39 | |||
| CPC membership | Member | 75.04 | 6.718 | 0.000 |
| Non-member | 71.77 | |||
| Hukou | Local | 74.59 | 6.431 | 0.000 |
| Non-local | 71.74 | |||
| Marital status | Non-solitary | 72.12 | 2.187 | 0.029 |
| Solitary | 70.71 | |||
| Sickness and injury status | No sickness or injury in the last two weeks | 72.69 | 9.812 | 0.000 |
| Sickness and injury within the last two weeks | 68.03 | |||
| Hospitalization history | No hospitalizations since July 2017 | 72.54 | 7.911 | 0.000 |
| Hospitalization since July 2017 | 68.7 | |||
| History of alcohol consumption | No history of alcohol consumption | 71.81 | −2.481 | 0.013 |
| History of alcohol consumption | 72.79 | |||
| Variable | Model 1 | Model 2 | ||
|---|---|---|---|---|
| Coefficient (95% CI) | Standard Error | Coefficient (95% CI) | Standard Error | |
| Urban environment | ||||
| Greening rate | 0.192 *** (0.10, 0.27) | 0.044 | 0.19 *** (0.10, 0.27) | 0.044 |
| Urbanization rate | −0.079 *** (−0.11, −0.04) | 0.017 | −0.08 *** (−0.11, −0.04) | 0.017 |
| Road density | 2.714 *** (1.90, 3.52) | 0.411 | 2.716 *** (1.91, 3.52) | 0.411 |
| Air quality (PM2.5) | 0.023 (−0.00, 0.05) | 0.015 | 0.023 (−0.00, 0.05) | 0.015 |
| Tertiary hospitals | 0.057 *** (0.02, 0.08) | 0.015 | 0.06 *** (0.03, 0.09) | 0.016 |
| Population density | −0.002 *** (−0.00, −0.00) | 0.000 | −0.002 *** (−0.00, −0.00) | 0.000 |
| Social environment | ||||
| Community cohesion | 0.128 * (−0.00, 0.26) | 0.07 | 0.126 * (−0.07, 1.00) | 0.07 |
| Life satisfaction | 0.48 * (−0.06, 1.02) | 0.276 | 0.463 * (0.59, 1.62) | 0.276 |
| Happiness | 1.101 *** (0.58, 1.62) | 0.265 | 1.109 *** (0.59, 1.62) | 0.265 |
| Economic satisfaction | 1.268 *** (0.90, 1.62) | 0.184 | 1.296 *** (0.93, 1.65) | 0.185 |
| Sense of security | 0.324 *** (0.24, 0.40) | 0.042 | 0.321 *** (0.23, 0.40) | 0.042 |
| Individual health | ||||
| History of alcohol consumption | −0.184 (−0.99, 0.62) | 0.412 | 2.797 (−0.97, 0.64) | 0.412 |
| Sickness and injury | 2.789 *** (1.95, 3.62) | 0.424 | 2.797 *** (1.96, 3.62) | 0.423 |
| Hospitalization history | 2.239 *** (1.39, 3.08) | 0.429 | 2.261 *** (1.41, 3.10) | 0.429 |
| Sociodemographic characteristics | ||||
| Hukou | 0.264 (−1.03, 1.56) | 0.661 | 0.234 (−1.06, 1.53) | 0.661 |
| CPC membership | 0.611 (−0.57, 1.81) | 0.607 | 0.654 (−0.53, 1.84) | 0.607 |
| Sex | 0.915 *** (0.24, 1.58) | 0.343 | 0.905 *** (0.23, 1.57) | 0.343 |
| Marital status | 0.817 (−0.19, 1.83) | 0.517 | 0.815 (−0.19, 1.82) | 0.517 |
| Education | 0.795 *** (0.39, 1.2) | 0.207 | 0.814 *** (0.40, 1.22) | 0.209 |
| Income | 0.324 *** (0.15, 0.48) | 0.084 | 0.336 *** (0.17, 0.50) | 0.085 |
| Moderating variable | ||||
| Social participation | 0.022 (−0.07, 0.12) | 0.051 | ||
| Interaction term | ||||
| Greening rate × social participation | 0.034 ** (0.00, 0.06) | 0.015 | ||
| Constant | 39.986 *** (35.24, 44.72) | 2.419 | 39.354 *** (33.40, 45.30) | 3.033 |
| R2 | 0.176 | 0.178 | ||
| Variable | Model 3 | Model 4 | ||
|---|---|---|---|---|
| Coefficient (95% CI) | Standard Error | Coefficient (95% CI) | Standard Error | |
| Urban environment | ||||
| Greening rate | 0.279 * (−0.05, 0.61) | 0.168 | 0.343 ** (0.01, 0.67) | 0.169 |
| Urbanization rate | −0.22 *** (−0.34, −0.09) | 0.063 | −0.212 *** (−0.33, −0.08) | 0.063 |
| Road density | 4.447 *** (1.33, 7.55) | 1.579 | 4.504 *** (1.41, 7.59) | 1.568 |
| Air quality (PM2.5) | 0.037 (−0.07, 0.15) | 0.057 | 0.038 (−0.07, 0.15) | 0.057 |
| Tertiary hospitals | 0.189 *** (0.08, 0.29) | 0.055 | 0.168 *** (0.05, 0.27) | 0.055 |
| Population density | −0.003 * (−0.00, 0.00) | 0.002 | −0.003 * (−0.00, 0.00) | 0.002 |
| Social environment | ||||
| Community cohesion | 0.332 (−0.19, 0.86) | 0.268 | 0.356 (−0.16, 0.88) | 0.267 |
| Life satisfaction | 1.437 (−0.38, 3.26) | 0.928 | 1.368 (−0.44, 3.18) | 0.922 |
| Happiness | −0.752 (−2.64, 1.14) | 0.961 | −0.667 (−2.54, 1.21) | 0.954 |
| Economic satisfaction | 3.136 *** (1.82, 4.44) | 0.667 | 3.167 *** (1.85, 4.47) | 0.665 |
| Sense of security | 0.039 (−0.28, 0.36) | 0.163 | 0.027 (−0.29, 0.34) | 0.163 |
| Individual health | ||||
| History of alcohol consumption | 4.952 *** (2.20, 7.70) | 1.396 | 5.139 *** (2.39, 7.88) | 1.393 |
| Sickness and injury | 3.639 ** (0.80, 6.47) | 1.441 | 3.861 *** (1.03, 6.68) | 1.434 |
| Hospitalization history | 2.048 (−1.28, 5.38) | 1.693 | 2.096 (−1.21, 5.40) | 1.68 |
| Sociodemographic characteristics | ||||
| Hukou | −0.47 (−5.70, 4.76) | 2.657 | −0.393 (−5.59, 4.80) | 2.64 |
| CPC membership | 3.068 (−1.38, 7.51) | 2.26 | 3.311 (−1.12, 7.74) | 2.251 |
| Sex | 1.962 (−0.52, 4.44) | 1.262 | 1.992 (−0.47, 4.46) | 1.254 |
| Education | 0.068 (−1.45, 1.59) | 0.773 | 0.206 (−1.34, 1.75) | 0.786 |
| Income | 0.135 (−0.47, 0.74) | 0.31 | 0.161 (−0.44, 0.76) | 0.309 |
| Moderating variable | ||||
| Social participation | 0.425 ** (0.00, 0.84) | 0.214 | ||
| Interaction term | ||||
| Greening rate × social participation | −0.137 ** (−0.27, −0.00) | 0.069 | ||
| Constant | 41.431 *** (24.73, 58.13) | 8.481 | 22.829 * (−0.78, 46.44) | 11.994 |
| R2 | 0.352 | 0.367 | ||
| Variable | Model 5 | Model 6 | ||
|---|---|---|---|---|
| Coefficient (95% CI) | Standard Error | Coefficient (95% CI) | Standard Error | |
| Urban environment | ||||
| Greening rate | 0.178 *** (0.08, 0.26) | 0.045 | 0.176 *** (0.08, 0.26) | 0.045 |
| Urbanization rate | −0.063 *** (−0.09, −0.02) | 0.018 | −0.064 *** (−0.09, −0.02) | 0.018 |
| Road density | 2.468 *** (1.63, 3.30) | 0.425 | 2.472 *** (1.64, 3.30) | 0.424 |
| Air quality (PM2.5) | 0.02 (−0.01, 0.05) | 0.015 | 0.019 (−0.01, 0.04) | 0.015 |
| Tertiary hospitals | 0.041 ** (0.00, 0.07) | 0.016 | 0.045 *** (0.01, 0.07) | 0.016 |
| Population density | −0.001 *** (−0.00, 0.00) | 0.000 | −0.001 *** (−0.00, −0.00) | 0.000 |
| Social environment | ||||
| Community cohesion | 0.102 (−0.03, 0.24) | 0.072 | 0.099 (−0.04, 0.24) | 0.072 |
| Life satisfaction | 0.333 (−0.23, 0.89) | 0.288 | 0.309 (−0.25, 0.87) | 0.288 |
| Happiness | 1.279 *** (0.74, 1.81) | 0.274 | 1.292 *** (0.75, 1.82) | 0.274 |
| Economic satisfaction | 1.076 *** (0.70, 1.45) | 0.191 | 1.102 *** (0.72, 1.47) | 0.191 |
| Sense of security | 0.345 *** (0.25, 0.43) | 0.044 | 0.344 *** (0.25, 0.42) | 0.044 |
| Individual health | ||||
| History of alcohol consumption | −0.716 * (−1.56, 0.12) | 0.43 | −0.675 (−1.51, 0.16) | 0.43 |
| Sickness and injury | 2.76 *** (1.89, 3.62) | 0.443 | 2.769 *** (1.90, 3.63) | 0.442 |
| Hospitalization history | 2.224 *** (1.35, 3.08) | 0.441 | 2.246 *** (1.38, 3.11) | 0.441 |
| Sociodemographic characteristics | ||||
| Hukou | 0.285 (−1.04, 1.61) | 0.679 | 0.258 (−1.07, 1.59) | 0.679 |
| CPC membership | 0.263 (−0.96, 1.49) | 0.627 | 0.32 (−0.90, 1.55) | 0.627 |
| Sex | 0.847 *** (0.15, 1.54) | 0.355 | 0.852 ** (0.15, 1.54) | 0.355 |
| Education | 0.887 *** (0.46, 1.30) | 0.214 | 0.886 *** (0.46, 1.30) | 0.216 |
| Income | 0.318 *** (0.14, 0.48) | 0.087 | 0.33 *** (0.15, 0.50) | 0.088 |
| Moderating variable | ||||
| Social participation | −0.005 (−0.10, 0.09) | 0.052 | ||
| Interaction term | ||||
| Greening rate × social participation | 0.041 *** (0.01, 0.07) | 0.015 | ||
| Constant | 41.461 *** (36.58, 46.34) | 2.488 | 41.745 *** (35.66, 47.82) | 3.099 |
| R2 | 0.166 | 0.169 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, Y.; Cheng, B.; Dong, L.; Zheng, T.; Wu, R. The Moderating Effect of Social Participation on the Relationship between Urban Green Space and the Mental Health of Older Adults: A Case Study in China. Land 2024, 13, 317. https://doi.org/10.3390/land13030317
Zheng Y, Cheng B, Dong L, Zheng T, Wu R. The Moderating Effect of Social Participation on the Relationship between Urban Green Space and the Mental Health of Older Adults: A Case Study in China. Land. 2024; 13(3):317. https://doi.org/10.3390/land13030317
Chicago/Turabian StyleZheng, Yuan, Bin Cheng, Letian Dong, Tianxiang Zheng, and Rong Wu. 2024. "The Moderating Effect of Social Participation on the Relationship between Urban Green Space and the Mental Health of Older Adults: A Case Study in China" Land 13, no. 3: 317. https://doi.org/10.3390/land13030317
APA StyleZheng, Y., Cheng, B., Dong, L., Zheng, T., & Wu, R. (2024). The Moderating Effect of Social Participation on the Relationship between Urban Green Space and the Mental Health of Older Adults: A Case Study in China. Land, 13(3), 317. https://doi.org/10.3390/land13030317






