Abstract
Cardiovascular diseases (CVD) are one of the leading causes of death globally, and a major contributor to CVD mortality is ambient air pollution (AAP). This study aimed to evaluate associations between AAP and mortality from CVD, including ischemic heart diseases (IHD) and strokes. Data on daily mortality records, six criteria AAP and meteorology in the capital city of Mongolia were collected between 1 January 2016 and 31 December 2022. A time-stratified case-crossover design was analysed with distributed lag conditional Poisson regression to estimate the relative risk of CVD mortality. We found that for each interquartile range increase in PM2.5, PM10, SO2 and NO2 pollutants, the risk of CVD mortality increased by 1.5% (RR = 1.015; 95% CI: 1.005, 1.025), 4.4% (RR = 1.044; 95% CI: 1.029, 1.059), 3.1% (RR = 1.033; 95% CI: 1.015, 1.047) and 4.8% (RR = 1.048; 95% CI: 1.013, 1.085) at lag01, respectively. The association between all pollutants, except O3, and CVD mortality was higher in subgroups ≥ 65 years and male, during the cold season and after using a new type of coal briquettes. Despite using the new type of coal briquettes, Ulaanbaatar’s ambient air pollution remained higher than the WHO’s guidelines. Based on our findings, we recommend that efforts should be focused on adopting more efficient strategies to reduce the current pollution level.
1. Introduction
Ambient air pollution is the fourth leading cause of mortality and is a major contributor to the global burden of diseases, with over 89% occurring in low- and middle-income countries (LMICs) [1,2]. On the other hand, cardiovascular diseases (CVD), including ischemic heart diseases (IHD) and stroke, are the leading causes of mortality globally, and 20.5 million people died from CVD in 2021, of which 4.8 million deaths were attributable to air pollution [3]. Among CVD, stroke is the second-leading cause of death and the third major cause of disability among adults worldwide [4]. A growing number of systematic reviews and observational epidemiological studies on the acute effects of air pollution on CVD mortality have been primarily conducted in developed countries; however, a few studies have been carried out in LMICs, where air pollution levels are remarkably high [5,6,7]. Previous studies were predominantly focused on exposure to particulate matter with an aerodynamic diameter of less than 2.5 µm and 10 µm (PM2.5 and PM10) [8,9,10,11,12], with comparatively fewer studies examining the impacts of gaseous pollutants, and also the findings have been inconsistent [13,14,15]. Considering the substantial differences in air pollution levels, weather conditions, population vulnerability and sociodemographic characteristics across various geographic regions and countries, scientific evidence specific to LMICs, like Mongolia, is required.
Mongolia is suffering from significantly high levels of outdoor air pollution due to coal consumption during the harsh and long winter season. Meanwhile, CVD is the first major cause of mortality and the third leading cause of morbidity among the general population of Mongolia [16]. The majority of deaths in the nation were caused by CVD, with IHD accounting for 44% and stroke for 22.8% in 2022 [16]. To reduce outdoor air pollution in the capital city (Ulaanbaatar), the Mongolian government has implemented a series of step-by-step actions, such as providing households with low-emission stoves, expanding heating networks and introducing new types of coal briquettes. In response, the Mongolian government banned raw coal consumption in Ulaanbaatar on 15 May 2019, and any raw coal transport has been restricted from entering the city [17]. In this regard, Tavan Tolgoi Fuel LLC, a state-owned fuel company, was established to produce up to 600,000 tons of refined coal briquettes annually and distribute them to traditional households in the 6 central districts of the city [18].
To date, no study has been conducted to evaluate the difference between air pollution levels before and after the raw coal ban and the association between short-term exposure to air pollution and the risk of CVD death. The main purpose of this study was (a) to compare outdoor air pollution levels before and after consuming the new type of coal briquettes, and (b) to assess the acute effects of ambient air pollution on mortality from CVD, IHD and stroke in the capital city of Mongolia.
2. Materials and Methods
2.1. Study Area
Mongolia is an independent country with 3.4 million people located between Russia and China; it is classified as a lower-middle-income country based on the World Bank’s Country Classification by income level [19]. The country has four seasons: winter, spring, summer and autumn, and its temperature ranges from −40 °C to 30 °C. The capital city of Mongolia is Ulaanbaatar, spanning a total land area of 4704 square km (1816 square miles); it is situated in the Tuul River Valley at an elevation of approximately 1300 m (4300 ft.) from the sea level and surrounded by four big mountains. The capital city accommodates nearly 50% of the total population; the majority of the residents live in traditional round-shaped dwellings called “ger” [20]. These ger households consume 600,000 tons of coal per year without any pollution control devices, and each ger household uses around 5 tons of coal annually for cooking and heating purposes [20]. The ger households use either traditional or improved stoves connected with chimneys that disperse significant amounts of particulate matter and gaseous pollutants into the outside air. As previous studies have reported, coal combustion in traditional household areas and the three major coal-fired power plants are the primary sources of outdoor air pollution in Ulaanbaatar [21,22]. Furthermore, another study reported that these ger household suburbs face myriad challenges due to poor development of essential infrastructures, such as central heating, sewage systems and paved roads [23].
2.2. Environmental Data
We collected daily mean concentrations of six criteria air pollutants and meteorological data (temperature and relative humidity) between 1 January 2016 and 31 December 2022 from the National Centre for Environmental Monitoring in Ulaanbaatar, Mongolia. The six criteria air pollutants included particulate matter ≤ 2.5 µm (PM2.5) and ≤ 10 µm in diameter (PM10), sulphur dioxide (SO2), nitrogen dioxide (NO2), ozone (O3) in micrograms per cubic meter (µg/m3) and carbon monoxide (CO) in milligram per cubic meter (mg/m3) as the indicators of air quality recommended by the World Health Organization (WHO) [24]. Daily mean levels of PM2.5, PM10, SO2 and NO2 and 8-h mean concentrations of O3 and CO averaged across seven monitoring stations were used. We also collected the daily mean atmospheric temperature and relative humidity as meteorological data from the stations. The capital city of Mongolia has nine districts; however, six central districts (Bayangol, Bayanzurkh, Khan-Uul, Sukhbaatar, Chingeltei and Songinokhairkhan) that provided sufficient datasets were included in this study. There are 15 air monitoring stations in Ulaanbaatar city, but we included only 7 monitoring stations with less than 25% of missing data.
2.3. Mortality Data
The data on all-cause and cause-specific mortality between 1 January 2016 and 31 December 2022 were collected from the National Centre for Health Development at the Ministry of Health in Ulaanbaatar, Mongolia. Health data from nine public hospitals (six secondary and three tertiary levels) were included in this study. Each mortality record includes a national identity card number, age, gender, date of birth, date of death, the main cause of death, home address and name of the hospital. These mortality data were classified based on the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) coding [25]. The primary outcomes included CVDs (ICD10: I00–I99), IHDs (ICD10: I20–I25) and cerebrovascular diseases, defined as total stroke (ICD10: I60–I69). These nine public hospitals use accurate diagnoses based on medical examinations and computed tomography or magnetic resonance imaging. This study was approved by the Human Research Ethics Committee of Curtin University (Approval No: HRE2021-0062) and classified as a low-risk study.
2.4. Statistical Analyses
In this study, a time-stratified case-crossover design was conducted to assess the relationship between outdoor air pollution and mortality for CVD, IHD and stroke. A conditional Poisson model was used for the main analysis since it provided smaller or more precise confidence intervals than the quasi-Poisson regression. The quasi-Poisson regression analysis was reported as a secondary analysis. The conditional Poisson regression with distributed lag model (DLM) was used to estimate the exposure-lag response relationship between air pollution exposure and cause-specific mortality. Adding a flexible “cross-basis” function to specify exposure–lag–response allowed the DLM model to simultaneously account for both linear exposure–response relationships and non-linear delayed (lagged) effects [26]. Daily mean concentrations of air pollutants and aggregated daily mortality cases were merged by date. The aggregated daily mortality cases were time stratified on the event (case) day and compared with those on the control days by matching case and control days on the same day of the week (DOW) in the same month of the same year. The modelling framework was specified as follows:
where α is the intercept; [E()] is the observed number of daily mortality counts on day t; cb (AP) is the cross-basis function specified using R package “dlnm” for daily air pollution exposure concentration; ns () is the natural cubic splines for nonlinear variable adjustment, including average temperature (Temp) and relative humidity (RH); and dfs represent the degrees of freedom of the exposure and lag scales, respectively. The optimal dfs were selected based on minimum Akaike Information Criterion (AIC) after varying 2–7 dfs. Finally, 3 dfs for the lag scale for all air pollutants were selected based on the lowest AIC [26], using a maximum lag of 7 days. Similarly, the 3 dfs for the non-linear adjustment of Temp and RH were also selected based on the minimum AIC. The conditional factor variable stratum specified the same DOW in the same month of the same year (defined as interaction terms among the variables DOW, month and year of the cases) to control the influence of the DOW and long-term and seasonal trends [27,28]. Single-pollutant conditional Poisson regressions were performed using the R package “gnm” [29], and the eliminate function was used to include the stratum factor variable [27]. To minimize inaccurate results caused by collinearity in single-lag estimates in distributed lag models, we used cumulative effect estimates rather than individual lag days [30].
The relative risk (RR) and 95% confidence intervals (CI) of mortality for CVD, IHD and stroke were estimated as per interquartile range (IQR) increase in all air pollutants (53.5 µg/m3 for PM2.5, 78.0 µg/m3 for PM10, 47.7 µg/m3 for SO2, 28.9 µg/m3 for NO2, 1.3 mg/m3 for CO and 19.5 µg/m3 for O3). Subgroup analyses were conducted based on age (<65 vs. ≥65), gender (male vs. female), two seasons (cold vs. warm) and before/after the raw coal prohibition. Seasons were classified as warm (April–September) and cold (October–March) based on weather conditions and coal consumption for heating and cooking purposes. All analyses were performed with the R statistical software program (version 4.1.1) [31]. Following the new recommendations of the American Statistical Association, we reported and interpreted the RR (95% CI) without considering the “statistical significance” or arbitrary p-value threshold [32].
3. Results
During the study period, a total of 30,319 people died, with 11,557 deaths from CVD at a daily mortality rate of 4.5 (standard deviation (SD) 2.2), and the average age of CVD mortality was 69.7 (SD 15.5) years. Among those with CVD mortality, 4804 people died due to stroke, accounting for 41.6% of the total CVD deaths at a daily mortality rate of 1.8 (SD 1.3), and the average age was 63.9 (SD 14.0) years. IHD caused 4905 deaths, accounting for 42.4% of the total CVD mortality, with a daily mortality rate of 1.9 (SD 1.4) and an average age of 75.2 (SD 14.3) years. Among the cause-specific mortality, males and the 65 and older age group (≥65 years) had a higher death rate, except for stroke. More people died in the cold season than in the warm season, and after the raw coal ban period (Table 1 and Table S1). The mortality rates from CVD, IHD and stroke fluctuated throughout the study period; however, the maximum fatality rate was recorded in 2021, while the lowest was in 2017 (Figure S1).

Table 1.
Demographic characteristics of cause-specific mortality in Ulaanbaatar, Mongolia (2016–2022).
The annual mean concentrations (SD) of PM2.5, PM10, SO2, NO2, O3 and CO were 52.2 (57.8) µg/m3, 118.1 (71.8) µg/m3, 41.0 (51.7) µg/m3, 51.4 (22.5) µg/m3, 29.4 (14.8) µg/m3 and 1.3 (1.1) mg/m3, respectively. During the study period, Ulaanbaatar’s daily mean temperature and relative humidity were 0.9 °C (ranging from −30.4 °C to 26.6 °C) and 53.2% (11.4% to 85.0%), respectively (Table 2). On average, the cold season (October–March) had higher air pollution levels, lower temperatures and higher relative humidity. After the Mongolian government banned raw coal burning in the capital city, the people living in traditional households started consuming the new types of refined coal briquettes for cooking and heating during the cold months between October and March. Since using the new type of coal, the annual mean concentrations of PM2.5, PM10 and O3 decreased; however, SO2 concentrations rose by two- to three-fold between 2020 and 2022 compared to the previous years. The annual mean concentrations of CO increased slightly between 2019 and 2022, whereas NO2 levels fluctuated during the study period (Figure 1).

Table 2.
Summary statistics * of air pollutant concentrations and meteorological factors in Ulaanbaatar, Mongolia (2016–2022).
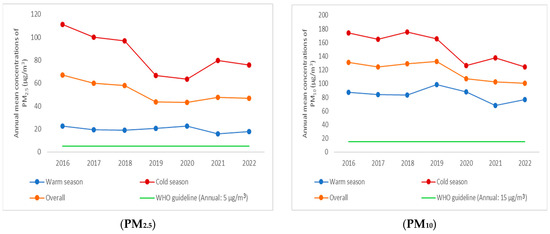
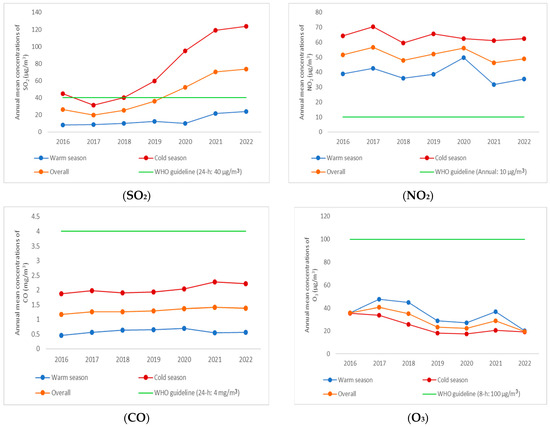
Figure 1.
Annual mean concentrations of air pollutants overall and by the two seasons compared with the WHO guidelines.
The levels of PM2.5, PM10, SO2, NO2 and CO were positively correlated with each other (correlation coefficient: 0.21–0.77, p-value < 0.05), while O3 was negatively correlated with other pollutants. The correlation between PM2.5 and PM10 was the strongest, with a Spearman correlation coefficient of 0.77. Following that, the correlations between PM2.5 and NO2, as well as PM10 and NO2, were the next strongest, whereas the correlations between CO and other pollutants were the weakest. Most pollutants showed negative correlations with daily average temperature; however, the correlations were negligible between air pollutants and relative humidity (Table S2).
The RRs of air pollution on mortality for CVD, IHD and stroke at lag0 to lag02 days are shown in Table 3 and Figure 2. Overall, after controlling for DOW, seasonal and long-term trends and meteorological factors, all air pollutants, except O3, were positively associated with CVD, IHD and stroke mortality. The highest RRs of air pollution on the cause-specific mortality occurred on the two-day or three-day average (lag01 and lag02). For each IQR increase in PM2.5, PM10, SO2 and NO2 pollutants, the risk of CVD mortality increased by 1.5% (RR = 1.015; 95% CI: 1.005, 1.025 ), 4.4% (RR = 1.044; 95% CI: 1.029, 1.059), 3.1% (RR = 1.033; 95% CI: 1.015, 1.047) and 4.8% (RR = 1.048; 95% CI: 1.013, 1.085) at lag01, respectively (Table 3 and Figure 1). The RRs of stroke mortality increased by 1.4% (RR = 1.014; 95% CI: 1.000, 1.028), 4.7% (RR = 1.047; 95% CI: 1.014, 1.078), 5.3% (RR = 1.053; 95% CI: 1.021, 1.085) and 6.7% (RR = 1.067; 95% CI: 1.032, 1.102) per IQR increase in PM2.5, PM10, SO2 and NO2 at lag01, respectively. Each IQR increase in PM2.5, PM10, SO2 and NO2 at lag01 and CO at lag0 was associated with a 0.8% (RR = 1.008; 95% CI: 0.994, 1.022), 1.0% (RR = 1.010; 95% CI: 0.980, 1.041), 3.0% (RR = 1.030; 95% CI: 1.000, 1.060), 1.7% (RR = 1.017; 95% CI: 0.968, 1.069) and 0.2% (RR = 1.002; 95% CI: 0.985, 1.019) increase in IHD mortality, respectively (Table 3 and Table S3).

Table 3.
Relative risks of CVD, stroke and IHD mortality risk associated with air pollutants per IQR at Lag0–lag02 days for single pollutant models.
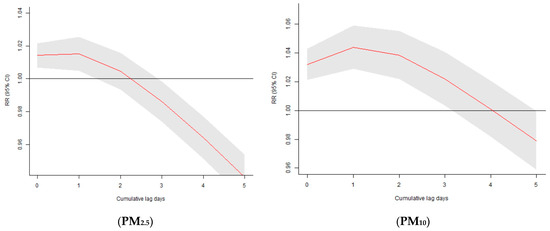
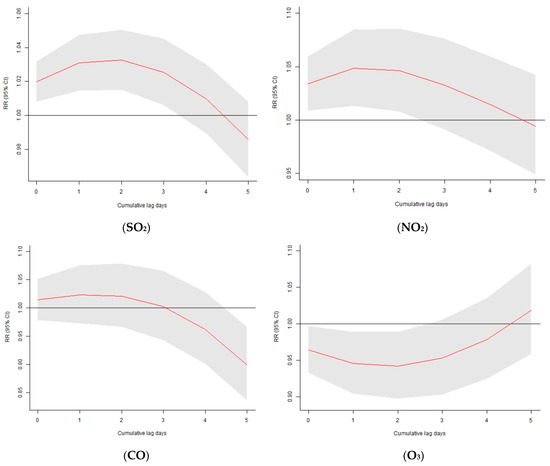
Figure 2.
Relative risks of CVD mortality associated with air pollutants per IQR increase at Lag0–Lag05 days.
According to the subgroup analyses, the association varied by age, sex, the two seasons and before and after the new types of coal consumption. The association between all pollutants, except O3, and CVD mortality was higher in those aged 65 and older and in the male group. The short-term effects of air pollution on CVD mortality were greater in the cold season than in the warm season, with higher levels of air pollutants (except O3) and lower temperatures. When comparing the two different types of coal consumption, the risk of total CVD mortality associated with NO2 and SO2 pollutants was higher after using the new coal briquettes (Table 4).

Table 4.
Relative risks of CVD mortality risk associated with air pollutants per IQR increase at lag01 days by subgroups.
Although with lower precision, the results of the conditional quasi-Poisson DLM models were consistent with those of the main results from the conditional Poisson DLM models (Figure S2).
4. Discussion
This study investigated the association between short-term exposure to ambient air pollution and cause-specific mortality in the capital city of Mongolia from 2016 to 2022. To the best of our knowledge, this is the first study to evaluate the effects of six criteria air pollutants on mortality from CVD, IHD and stroke and compare the levels of air pollutants before and after the raw coal ban in the capital city of Mongolia.
Overall, we found that short-term exposure to PM2.5, PM10, SO2, NO2 and CO were positively associated with increased risk of CVD, IHD and stroke mortality in single-pollutant models. The strongest associations were found between PM2.5, PM10, SO2 and NO2 exposure and mortality for CVD and stroke at lag01. Our research results were consistent with previous findings that showed positive associations between outdoor air pollution and CVD mortality in China [33], Thailand [34] and Korea [35]. For instance, Zhou and colleagues assessed the acute effects of particulate matter pollution on CVD mortality in China. This study results showed that each 10 µg/m3 increase in PM2.5 and PM10 was associated with an increase of 1.33% (95% CI: 0.08%, 2.60%) and 1.12% (95% CI: 0.43%, 1.82%) in CVD mortality at lag0 [33]. Crouse and colleagues conducted a 16-year follow-up cohort study in Canada to investigate the impact of PM2.5 and NO2 pollutants on CVD mortality [36]. This cohort study found that for each 5 µg/m3 increase in PM2.5 and 15.2 µg/m3 increase in NO2, the risk of CVD mortality increased by 3.0% (Hazard Ratio (HR) = 1.030; 95% CI: 1.021, 1.040) and 4.1% (HR = 1.041; 95% CI: 1.028, 1.053), respectively [36]. A systematic review and meta-analysis study results revealed that the RRs of CVD mortality associated with per 10 µg/m3 increments of PM2.5 and PM10 were increased by 0.9% (RR = 1.009; 95% CI: 1.006, 1.012) and 0.6% (RR = 1.006; 95% CI: 1.004, 1.007), respectively [7]. According to findings from another systematic review and meta-analysis study, each 10 µg/m3 increase in PM2.5 and PM10 was linked to increases in CVD mortality by 11.0% (RR = 1.11; 95% CI: 1.09, 1.14) and 4.0% (RR = 1.04; 95% CI: 0.99, 1.10); stroke by 11.0% (RR = 1.11; 95% CI: 1.04, 1.18) and 1.0% (RR = 1.01; 95% CI: 0.83, 1.21) and IHD mortality by 16.0% (RR = 1.16; 95% CI: 1.10, 1.21) and 1.0% (RR = 1.01; 95% CI: 0.83, 1.21), respectively [37]. These discrepancies might be due to differences in air pollution levels, source of air pollution emissions, weather conditions, housing types, population susceptibility, classification of diseases and sociodemographic characteristics across studies and countries. Most of these studies reported that industrial processes and vehicular emissions were the main causes of outdoor air pollution. Conversely, burning raw or processed coal during the cold winter season is the main source of outdoor air pollution in the capital city of Mongolia, such as particles, SO2 and CO pollutants [21,38], whereas vehicle emissions are the main sources of NO2 due to high traffic congestion in the city [22]. Furthermore, instead of 10 µg/m3, we used an IQR increment for all pollutants in the single-pollutant models, which may result in larger effect estimates compared to other studies.
In the subgroup analyses, the risk of CVD mortality was larger in men than women and higher in people aged ≥ 65 years than those aged < 65 years. The cold season (October–March) was more positively associated with CVD mortality than the warm season (April–September). After introducing the new types of coal briquettes, the annual mean concentrations of PM2.5, PM10 and O3 decreased gradually. However, throughout the cold season, the annual mean concentrations of PM2.5 and PM10 remained higher than the Mongolian Air Quality Standard and the WHO Air Quality Guidelines [24,39]. In contrast, the annual mean concentration of SO2 between 2020 and 2022 rose by two- to three-fold compared to previous years and exceeded the WHO Air Quality Guidelines of 40 µg/m3. On the other hand, the annual mean concentrations of NO2 fluctuated during the study period and remained higher than the WHO Air Quality Guidelines of 10 µg/m3. The seasonal influence of air pollution was consistent with previous studies conducted in the nation [20,21,40,41,42].
In Mongolia, very few studies have been conducted to evaluate the acute effects of outdoor air pollution on cardiovascular health outcomes. To give an example, Enkhjargal and colleagues estimated RRs of outdoor air pollution on hospital admissions for CVD between 2008 and 2017 in Ulaanbaatar, Mongolia [40]. The study results showed that daily mean concentrations of PM2.5, PM10, SO2, NO2, O3 and CO were 85.7 µg/m3, 182.7 µg/m3, 24.6 µg/m3, 45.4 µg/m3, 29.4 µg/m3 and 1.0 mg/m3, respectively; these pollutant concentrations were slightly higher than our study findings. Therefore, Enkhjargal and colleagues found positive associations between PM2.5, PM10, SO2, CO and O3 and CVD admissions in the cold season, which are similar to our findings regarding the seasonal effects, except O3 pollutant. Another research estimated that the RR of outdoor air pollution on cardiopulmonary mortality was 29% (RR = 1.29; 95% CI: 1.12, 1.43) in Mongolia [21], which was much higher than our study effect estimates. As a result of differences in the research methodology, exposure assessment, data analysis and health outcomes, we were unable to directly compare our findings to their study results.
Regarding the biological mechanisms, several studies have investigated the associations between ambient air pollution and CVD mortality [1,3,43]. Air pollutants may adversely affect the cardiovascular system directly and indirectly. Direct effects can be caused by substances that pass through the pulmonary epithelium and enter the blood circulation. The indirect effects can occur when endothelial dysfunction and systematic inflammation are induced, which involve altering the heart rate, elevating oxidative stress and enhancing blood coagulation and thrombosis formation [44,45]. Animal study results showed that exposure to particulate and gaseous pollutants elevated the level of cyclooxygenase-2, interleukin-1b and intercellular adhesion molecule-1 and protein, which might play a significant role in CVD, predominantly the development of stroke [46,47]. However, the biological pathways related to adverse health effects of air pollution need further investigation.
There are several strengths in this research study. To our knowledge, this study is the first and currently the only study conducted in Mongolia after the Mongolian government banned raw coal consumption on 15 May 2019, making possible comparisons before and after the new types of coal consumption and the effects of air pollution on CVD mortality. In this study, we applied a robust study design that controlled potential confounding factors, including long-term trends, seasonal trends, DOW, atmospheric temperature and relative humidity. Thus, our study would suggest more valid and reliable estimates of the effects of air pollution on CVD mortality in Ulaanbaatar, Mongolia.
There are several limitations in this study. Firstly, we utilized secondary data from air monitoring stations in Ulaanbaatar, Mongolia, which might result in exposure misclassification. Secondly, most of Ulaanbaatar’s ambient air quality monitoring stations were located in less polluted areas, so they may not represent the real air pollution levels in the traditional household suburbs and industrial areas. Thirdly, we did not have data to account for or examine other important variables, such as socioeconomic status, housing type, type of workplaces and the main sources of air pollution exposure. Furthermore, during the COVID-19 pandemic, total mortality rates increased globally, and this outbreak duration overlapped the period of the new coal briquette consumption in Ulaanbaatar, which might have affected our study results. Future studies could enhance its accuracy and representativeness by integrating primary data related to socioeconomic status, housing types, employment status and sources of individual exposure to outdoor air pollution and collecting air quality data from the most polluted areas in the city. In addition, it would be advantageous for future research to consider a longer period of the new coal briquette consumption and COVID-19 mortality and morbidity cases in the analysis.
5. Conclusions
To the best of our knowledge, this is the first study to evaluate the differences in ambient air pollution concentrations and the short-term effects of the six criteria air pollutants on the risk of CVD mortality before and after raw coal was banned by introducing a new type of coal briquettes in Ulaanbaatar, Mongolia. The results indicated that despite the new type of coal briquettes intervention, Ulaanbaatar’s ambient air pollution remained higher than the WHO’s guidelines and Mongolian national standard limits, especially during the cold winter season. Applying a robust methodological approach, we found that short-term exposures particularly to PM2.5, PM10, SO2 and NO2 pollutants were associated with higher risks of CVD mortality, including IHD and strokes. The effects of the pollutants on CVD mortality were slightly higher in subgroups ≥65 years and male and during the cold season. While reduced slightly for other pollutants, the risk of total CVD mortality associated with NO2 and SO2 pollutants was higher after using the new coal briquettes. The findings suggest an urgent need for evidence-based decision-making, and efforts should be focused on switching to cleaner fuels or adopting more efficient strategies to reduce the current air pollution level and associated adverse health effects in the capital city of Mongolia.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/atmos15091110/s1, Table S1: Summary statistics of all-cause and cause-specific mortality in Ulaanbaatar city, Mongolia (2016–2022); Figure S1: Cause-specific mortality rates in Ulaanbaatar, Mongolia by year (2016–2022); Table S2: Spearman correlation coefficients among exposure variables in Ulaanbaatar, Mongolia; Table S3: RRs of CVD, stroke and IHD mortality risk associated with air pollutants per IQR at Lag0–lag05 days for single pollutant models; Figure S2: Relative risks of CVD mortality associated with air pollutants at Lag0–Lag05 days per IQR increment in exposure using the conditional quasi-Poisson DLM model.
Author Contributions
N.-E.B. collected, cleaned and prepared the research data. N.-E.B. conducted the preliminary and final analysis and wrote the first draft of this manuscript. S.D.N. participated in the final analyses and interpretation of the findings and critically reviewed the manuscript. G.P., K.R. and C.M.R. participated in the study design and critically reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Ethics Committee at the Institutional Review Board of Curtin University (Approval No: HRE2021-0062) and was classified as a low-risk study.
Informed Consent Statement
Not applicable.
Data Availability Statement
Secondary data can be shared on request from any qualified investigator following approval of a protocol and signed data access agreement via the Research Office at Curtin University in Western Australia.
Acknowledgments
The authors would like to thank the Centre for Health Development and the National Centre for Environmental Monitoring in Ulaanbaatar, Mongolia, for providing data for this research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organisation (WHO). Ambient (Outdoor) Air Pollution. Available online: https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health (accessed on 17 April 2024).
- Kim, H.; Byun, G.; Choi, Y.; Kim, S.; Kim, S.-Y.; Lee, J.-T. Effects of long-term exposure to air pollution on all-cause mortality and cause-specific mortality in seven major cities of South Korea: Korean national health and nutritional examination surveys with mortality follow-up. Environ. Res. 2021, 192, 110290. [Google Scholar] [CrossRef] [PubMed]
- World Heart Federation. World Heart Report 2023: Confronting the World’s Number One Killer. Available online: https://world-heart-federation.org/resource/world-heart-report-2023/ (accessed on 16 February 2024).
- Murray, C.J.L.; Barber, R.M.; Foreman, K.J.; Ozgoren, A.A.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Abraham, J.P.; Abubakar, I.; Abu-Raddad, L.J.; et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.K.; Bing, R.; Kiang, J.; Bashir, S.; Spath, N.; Stelzle, D.; Mortimer, K.; Bularga, A.; Doudesis, D.; Joshi, S.S.; et al. Adverse health effects associated with household air pollution: A systematic review, meta-analysis, and burden estimation study. Lancet Glob. Health 2020, 8, e1427–e1434. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Geng, H.; Dong, C.; Bai, T. The short-term harvesting effects of ambient particulate matter on mortality in Taiyuan elderly residents: A time-series analysis with a generalized additive distributed lag model. Ecotoxicol. Environ. Saf. 2021, 207, 111235. [Google Scholar] [CrossRef]
- Orellano, P.; Reynoso, J.; Quaranta, N.; Bardach, A.; Ciapponi, A. Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta-analysis. Environ. Int. 2020, 142, 105876. [Google Scholar] [CrossRef]
- Ma, Y.; Chen, R.; Pan, G.; Xu, X.; Song, W.; Chen, B.; Kan, H. Fine particulate air pollution and daily mortality in Shenyang, China. Sci. Total. Environ. 2011, 409, 2473–2477. [Google Scholar] [CrossRef]
- Pope, C.A.; Muhlestein, J.B.; May, H.T.; Renlund, D.G.; Anderson, J.L.; Horne, B.D. Ischemic heart disease events triggered by short-term exposure to fine particulate air pollution. Circulation 2006, 114, 2443–2448. [Google Scholar] [CrossRef]
- Xu, R.; Wang, Q.; Wei, J.; Lu, W.; Wang, R.; Liu, T.; Wang, Y.; Fan, Z.; Li, Y.; Xu, L.; et al. Association of short-term exposure to ambient air pollution with mortality from ischemic and hemorrhagic stroke. Eur. J. Neurol. 2022, 29, 1994–2005. [Google Scholar] [CrossRef]
- Zhang, C.; Quan, Z.; Wu, Q.; Jin, Z.; Lee, J.H.; Li, C.; Zheng, Y.; Cui, L. Association between atmospheric particulate pollutants and mortality for cardio-cerebrovascular diseases in Chinese Korean population: A Case-crossover study. Int. J. Environ. Res. Public. Health 2018, 15, 2835. [Google Scholar] [CrossRef]
- Lin, H.; Liu, T.; Xiao, J.; Zeng, W.; Guo, L.; Li, X.; Xu, Y.; Zhang, Y.; Chang, J.J.; Vaughn, M.G.; et al. Hourly peak PM2.5 concentration associated with increased cardiovascular mortality in Guangzhou, China. J. Expo. Sci. Environ. Epidemiol. 2017, 27, 333–338. [Google Scholar] [CrossRef]
- Lin, C.; Ma, Y.; Liu, R.; Shao, Y.; Ma, Z.; Zhou, L.; Jing, Y.; Bell, M.L.; Chen, K. Associations between short-term ambient ozone exposure and cause-specific mortality in rural and urban areas of Jiangsu, China. Environ. Res. 2022, 211, 113098. [Google Scholar] [CrossRef] [PubMed]
- Qian, Z.; He, Q.; Lin, H.-M.; Kong, L.; Liao, D.; Yang, N.; Bentley, C.M.; Xu, S. Short-Term Effects of Gaseous Pollutants on Cause-Specific Mortality in Wuhan, China. J. Air Waste Manag. Assoc. 2007, 57, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Yin, P.; Meng, X.; Wang, L.; Liu, C.; Niu, Y.; Lin, Z.; Liu, Y.; Liu, J.; Qi, J.; et al. Associations Between Ambient Nitrogen Dioxide and Daily Cause-specific Mortality. Epidemiology 2018, 29, 482–489. [Google Scholar] [CrossRef] [PubMed]
- MDoH. Mongolian Department of Health: Annual Report on Health Indicators. Available online: http://hdc.gov.mn/media/files/2022.pdf (accessed on 10 December 2023).
- ADB. Asian Development Bank Briefs: Improving Air Quality in Ulaanbaatar. Available online: www.adb.org/publications/series/adb-briefs (accessed on 22 September 2023).
- Jun, S. Is the Raw Coal Ban a Silver Bullet to Solving Air Pollution in Mongolia?: A Study of the Mongolian Government’s Air Pollution Reduction Policies and Recommendations in the Context of COVID-19. J. Public Int. Affairs. 2021, 1. [Google Scholar]
- World Bank. New World Bank Country Classifications by Income Level. Available online: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2022-2023 (accessed on 23 September 2023).
- Warburton, D.; Warburton, N.; Wigfall, C.; Chimedsuren, O.; Lodoisamba, D.; Lodoysamba, S.; Jargalsaikhan, B. Impact of Seasonal Winter Air Pollution on Health across the Lifespan in Mongolia and Some Putative Solutions. Conf. Paper. Ann. Am. Thorac. Soc. 2018, 15, S86–S90. [Google Scholar] [CrossRef]
- Allen, R.W.; Gombojav, E.; Barkhasragchaa, B.; Byambaa, T.; Lkhasuren, O.; Amram, O.; Takaro, T.K.; Janes, C.R. An assessment of air pollution and its attributable mortality in Ulaanbaatar, Mongolia. Air Qual. Atmos. Health 2011, 6, 137–150. [Google Scholar] [CrossRef]
- Huang, Y.-K.; Luvsan, M.-E.; Gombojav, E.; Ochir, C.; Bulgan, J.; Chan, C.-C. Land use patterns and SO2 and NO2 pollution in Ulaanbaatar, Mongolia. Environ. Res. 2013, 124, 1–6. [Google Scholar] [CrossRef]
- Enkhbat, U.; Rule, A.M.; Resnick, C.; Ochir, C.; Olkhanud, P.; Williams, D.L. Exposure to PM2.5 and Blood Lead Level in Two Populations in Ulaanbaatar, Mongolia. Int. J. Environ. Res. Public. Health 2016, 13, 214. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. Available online: https://www.who.int/publications/i/item/9789240034228 (accessed on 17 May 2023).
- WHO. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-WHO Version for 2016. Available online: https://icd.who.int/browse10/2016/en#/IX (accessed on 22 March 2023).
- Gasparrini, A. Distributed Lag Linear and Non-Linear Models in R: The Packagedlnm. J. Stat. Softw. 2011, 43, 2–20. [Google Scholar] [CrossRef]
- Armstrong, B.G.; Gasparrini, A.; Tobias, A. Conditional Poisson models: A flexible alternative to conditional logistic case cross-over analysis. BMC Med. Res. Methodol. 2014, 14, 122. [Google Scholar] [CrossRef]
- Mostofsky, E.; Coull, B.A.; Mittleman, M.A. Analysis of Observational Self-matched Data to Examine Acute Triggers of Outcome Events with Abrupt Onset. Epidemiology 2018, 29, 804–816. [Google Scholar] [CrossRef] [PubMed]
- Turner, H.; Firth, D. Generalized Nonlinear Models in R: An Overview of the Gnm Package. Version 1.1-5. Available online: https://cran.r-project.org/web/packages/gnm/vignettes/gnmOverview.pdf (accessed on 21 April 2024).
- Basagaña, X.; Barrera-Gómez, J. Reflection on modern methods: Visualizing the effects of collinearity in distributed lag models. Int. J. Epidemiol. 2022, 51, 334–344. [Google Scholar] [CrossRef] [PubMed]
- R. Core Team. R (Version 4.1.1): A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.r-project.org/ (accessed on 16 February 2024).
- Wasserstein, R.L.; Schirm, A.L.; Lazar, N.A. Moving to a World Beyond “p < 0.05”. Am. Stat. 2019, 73 (Suppl. 1), 1–19. [Google Scholar] [CrossRef]
- Zhou, X.; Wang, C.; Chen, P.; Chen, Y.; Yin, L.; Du, W.; Pu, Y. Time series analysis of short-term effects of particulate matter pollution on the circulatory system disease mortality risk in Lishui District, China. Environ. Sci. Pollut. Res. Int. 2022, 29, 17520–17529. [Google Scholar] [CrossRef] [PubMed]
- Taneepanichskul, N.; Gelaye, B.; Grigsby-Toussaint, D.S.; Lohsoonthorn, V.; Jimba, M.; Williams, M.A. Short-term effects of particulate matter exposure on daily mortality in Thailand: A case-crossover study. Air Qual. Atmos. Health 2018, 11, 639–647. [Google Scholar] [CrossRef]
- Kim, H.; Bell, M.L.; Lee, J.-T. Multi-dimensional community characteristics in linking particulate matter pollution and cause-specific mortality: 72 communities of South Korea. Environ. Res. 2021, 196, 110989. [Google Scholar] [CrossRef]
- Crouse, D.L.; Peters, P.A.; Hystad, P.; Brook, J.R.; Van Donkelaar, A.; Martin, R.V.; Villeneuve, P.J.; Jerrett, M.; Goldberg, M.S.; Pope, C.A., III; et al. Ambient PM2.5, O3, and NO2 Exposures and Associations with Mortality over 16 Years of Follow-Up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ. Health Perspect. 2015, 123, 1180–1186. [Google Scholar] [CrossRef]
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef]
- Lim, M.; Myagmarchuluun, S.; Ban, H.; Hwang, Y.; Ochir, C.; Lodoisamba, D.; Lee, K. Characteristics of Indoor PM2.5 Concentration in Gers Using Coal Stoves in Ulaanbaatar, Mongolia. Int. J. Environ. Res. Public. Health 2018, 15, 2524. [Google Scholar] [CrossRef]
- MASM. National Air Quality Standards in Mongolia (MNS 4585:2016). 2021. Available online: http://www.agaar.mn/article-view/546 (accessed on 11 September 2024).
- Enkhjargal, A.; Burmaajav, B.; Tsegmed, S.; Suvd, B.; Norolkhoosuren, B.; Unurbat, D.; Batbayar, J. Impact of Ambient Air Pollution and Meteorological Factors on Hospital Admission to the Cardiovascular System Disease on Ulaanbaatar City of Mongolia. Open J. Epidemiol. 2020, 10, 100–114. [Google Scholar] [CrossRef][Green Version]
- Tileubai, A.; Tsend, J.; Oyunbileg, B.-E.; Luvsantseren, P.; Luvsan-Ish, A.; Chilhaasuren, B.; Puntsagdash, J.; Chuluunbaatar, G.; Tsagaan, B. Study of decision tree algorithms: Effects of air pollution on under five mortality in Ulaanbaatar. BMJ Health Care Inform. 2023, 30, e100678. [Google Scholar] [CrossRef]
- Barn, P.; Gombojav, E.; Ochir, C.; Laagan, B.; Beejin, B.; Naidan, G.; Boldbaatar, B.; Galsuren, J.; Byambaa, T.; Janes, C.; et al. The effect of portable HEPA filter air cleaners on indoor PM2.5 concentrations and second hand tobacco smoke exposure among pregnant women in Ulaanbaatar, Mongolia: The UGAAR randomized controlled trial. Sci. Total. Environ. 2018, 615, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- EPA. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, Dec 2019). Available online: https://assessments.epa.gov/isa/document/&deid=347534 (accessed on 25 March 2024).
- Bhatnagar, A. Environmental Cardiology: Studying Mechanistic Links Between Pollution and Heart Disease. Circ. Res. 2006, 99, 692–705. [Google Scholar] [CrossRef] [PubMed]
- Routledge, H.C.; Manney, S.; Harrison, R.M.; Ayres, J.G.; Townend, J.N. Effect of inhaled sulphur dioxide and carbon particles on heart rate variability and markers of inflammation and coagulation in human subjects. Heart 2006, 92, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Tao, J.; Du, Y.; Liu, T.; Qian, Z.; Tian, L.; Di, Q.; Zeng, W.; Xiao, J.; Guo, L.; et al. Differentiating the effects of characteristics of PM pollution on mortality from ischemic and hemorrhagic strokes. Int. J. Hyg. Environ. Health 2016, 219, 204–211. [Google Scholar] [CrossRef]
- Sang, N.; Yun, Y.; Li, H.; Hou, L.; Han, M.; Li, G. SO2 Inhalation Contributes to the Development and Progression of Ischemic Stroke in the Brain. Toxicol. Sci. 2010, 114, 226–236. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).