1. Introduction
The level of stress in the workplace environment, which includes variables like poor lighting, extreme cold or heat, inadequate ventilation, and high humidity, can have a significant impact on employees’ health and productivity [
1]. Inadequate management of environmental stress can hinder job performance in several ways, such as heightened fatigue and distractibility, as well as diminished motivation, focus, and overall well-being of workers. The effects of environmental stresses on workers can be cumulative and additive [
2]. Furthermore, unsuitable working conditions in a work environment are often associated with the onset of cardiovascular, skeletal, and psychological diseases [
3].
The volume of surgical procedures is increasing worldwide, with an average daily count of 240 million surgeries [
4]. Consequently, the analysis of operating room (OR) data is crucial for hospital executives to minimize risks, considering that the number of studies in the field of risk management, particularly within hospital operating rooms worldwide, remains notably limited to date [
5,
6].
Specifically, an assessment of performance in terms of efficiency, effectiveness, and safety forms the foundation of surgical risk management. Ensuring precise environmental control is paramount within an OR. It serves as a distinctive workspace where the stakes are exceptionally high. Even slight distractions or decreases in staff attention and productivity due to work-related stress can result in catastrophic outcomes.
As a result, maintaining optimal environmental conditions in ORs is essential to safeguard the well-being and comfort of healthcare professionals and patients, as well as to enhance team productivity [
7]. Research on indoor air quality (IAQ) in hospitals and other healthcare facilities is limited compared to studies conducted on IAQ in residential buildings, schools, or commercial properties [
8]. Additionally, to date, there have been few studies that have evaluated the microclimatic parameters in operating rooms over an extended period. In Italy, Ferrante et al. monitored health and safety compliance in 38 ORs in Sicily from 2011 to 2020. Their results revealed that most microclimatic and microbiological parameters exceeded recommended limits, with 5.6% of sevoflurane measurements above permissible levels [
9]. Deiana et al. conducted a comparable study at the University Hospital of Sassari (Italy). Their research analyzed ten years (2010–2019) of periodic monitoring of microclimatic conditions in operating rooms (ORs) to assess thermal comfort, employing Fanger indices and regulatory standards. Nearly all assessments (98.8%) indicated non-compliant conditions. Furthermore, thermal discomfort was reported by 3.6% of healthcare professionals and 98.3% of patients [
10].
Therefore, it is crucial to identify and sustain appropriate environmental conditions to ensure a healthy, safe, and comfortable atmosphere. Microclimatic parameters such as temperature, humidity, and ventilation, along with factors like anesthetic gas concentrations, airborne particulate matter, and differential pressure, can significantly influence the comfort levels of both healthcare professionals and patients [
11,
12].
A study of Brazilian hospitals during summer found inadequate positive pressure in operating rooms, indicating contamination risks. However, the study’s limited sample size and cross-sectional design limit the generalizability of its findings, suggesting further research is needed to improve hospital heating, ventilation, and air-conditioning (HVAC) systems to prevent transmission of contaminated air and diseases through HVAC systems [
13].
Monitoring the levels of anesthetic gases in ORs is crucial, both for its implications on healthcare professionals and its environmental consequences, necessitating proper disposal systems and continuous monitoring [
14]. Prolonged exposure to these anesthetic gases can result in adverse health effects for individuals exposed, as demonstrated by neurotoxic, immunosuppressive, hepatotoxic, and reproductive effects [
15]. Therefore, diligent attention to monitoring and implementing appropriate disposal measures is essential to safeguard the comfort of individuals and minimize environmental impact [
16].
A proper ventilation system is essential to isolate and reduce airborne particles in a hospital OR [
17]. Ventilation systems serve as the primary means to eliminate infectious agents while simultaneously ensuring a thermally comfortable environment for the surgical staff and preventing the patient from experiencing extreme hypothermia [
17,
18]. The systematic review of operating room ventilation by Sadrizadeh et al. emphasizes their crucial role in controlling airborne infections, yet reveals significant disagreements among experts, indicating challenges in optimizing these systems across diverse surgical settings. Limitations include inconsistent methodologies, varied OR environments, and the controlled nature of many studies, which hinder generalization and practical application [
17]. Additionally, Mičko et al. recently studied air flow rate design from distribution elements to operating rooms, focusing on thermal comfort assessed by PMV and PPD indices. They found that an optimal discharge speed of 0.15–0.175 m/s correlates with a PPD index up to 22%, beyond which user dissatisfaction sharply increases to 70%. However, they noted potential limitations such as the absence of medical personnel, inaccuracies in measurement devices, and the controlled laboratory setting not fully representing real operating room conditions [
18]. The majority of healthcare facilities employ a unidirectional (laminar) downward airflow in the surgical field to establish a sterile environment for the patient. Indeed, elevated concentrations of airborne particulate matter can lead to surgical site infections (SSIs) [
19]. Recent studies indicate that a significant percentage of infections is circulated through the air, and during surgical procedures, airborne particles laden with bacteria, including textile fibers, dust particles, skin fragments, and respiratory aerosols, can settle on surgical instruments or directly enter the surgical site, resulting in SSI [
20,
21]. Hansen et al. observed that bacterial counts were lower in environments with fewer suspended airborne particles, and the number of particles larger than 5 μm was closely correlated with bacterial concentration [
22]. Other studies have demonstrated that 80–90% of detected pathogenic bacteria in surgical wounds were correlated with airborne particles in the OR [
23]. Tan et al. evaluated the relationships between PM and microbial contamination in operating rooms through on-site measurements and sampling. They found that PM 5 and PM 10 positively correlated (7% and 15%, respectively) with microbial levels under
at rest conditions. However, the study had limitations such as a small sample size and measurements conducted only under
at rest conditions. Therefore, the authors emphasized the need for future studies during surgical operations to capture real-time contamination [
24].
The current national regulations consist of various guidelines on environmental monitoring for ORs to prevent diseases and enhance working conditions. However, these documents should be consistently reviewed and updated to ensure their ongoing relevance. Furthermore, the health hazard level in surgical suites is intricately connected to the safety standards provided by healthcare institutions; hence, adherence to the national regulatory framework on occupational health and safety is obligatory, with meticulous consideration given to the healthcare domain. Specifically, the risk within operating theaters is intimately tied to safety protocols, ventilation setups, operator well-being, surgical apparatus, personal protective gear, and the training of medical personnel.
The main purpose of this study is to investigate the environmental conditions in healthcare settings, particularly focusing on air quality and its impact on healthcare professionals and patients. The study aims to assess various parameters such as microclimatic conditions, thermal comfort indices, air pressure differentials, and concentrations of anesthetic gases using standardized methods and advanced instruments. By identifying potential deviations from acceptable limits in these parameters, the study underscores the need for strict adherence to environmental standards and continuous monitoring practices to ensure optimal conditions in healthcare facilities. Furthermore, the research emphasizes the importance of educating healthcare staff on preventive practices and calls for ongoing updates to national guidelines and safety protocols. Ultimately, this work seeks to contribute to improving occupational health, enhancing patient safety, and optimizing clinical outcomes across healthcare settings globally.
2. Materials and Methods
The samples were taken at healthcare facilities in the Campania Region, which regularly require environmental monitoring to verify the maintenance of OR performance as mandated by the Italian regulatory system. This is also necessary for the management and maintenance of air treatment systems to prevent health hazards. The sampling was carried out by technicians from the Department of Public Health, who are authorized to perform environmental monitoring. The sampling was conducted in 141 monitored ORs, distributed among 33 public hospitals in the provinces of Naples, Caserta, Salerno, Avellino, and Benevento, across the entire Campania Region, and were analyzed from January 2015 to December 2022. In particular, the chemical and physical surveys planned every six months were carried out during the winter and the summer seasons, while the analyses planned every four months were conducted during the spring/summer and winter season. The samples used for this study were collected in hospital buildings that required regular environmental monitoring of air in ORs as part of their air quality and safety plans, in compliance with Italian operational guidelines for the management and the maintenance of air handling systems to avoid health and safety risks during work. The layout of a typical OR includes the following (
Figure S1):
- (1)
Main entrance: entrance with automatic doors for medical staff access.
- (2)
Preparation area: space where medical staff can prepare and dress in sterile attire.
- (3)
Sterile zone: includes the actual operating room, with sterile flooring, walls, and ceil-ing.
- (4)
Operating table: positioned at the center of the room, adjustable in height and tilt.
- (5)
Surgical lights: surgical lights mounted on the ceiling to illuminate the surgical field.
- (6)
Carts and surgical instruments: mobile carts containing the necessary instruments for the procedure.
- (7)
Anesthesia machines: equipment for administering anesthesia to the patient.
- (8)
Monitors and life support equipment: screens to monitor the patient’s vital signs.
- (9)
Staff stations: designated areas for surgeons, anesthesiologists, and nurses.
- (10)
Emergency exit: for rapid exit in case of emergencies.
- (11)
Ventilation system: systems to maintain sterile air and control temperature.
The ORs for minor procedures must have a surface area of no less than 25 m
2; for medium-assistance surgical procedures, a surface area of no less than 30 m
2; and for high-specialty surgical disciplines, a surface area of no less than 36 m
2. All surfaces must be fire-resistant, washable, disinfectable, smooth, and ungrooved with a rounded junction to the floor. The floor must be resistant to chemical and physical agents, polished, and non-slip. In most ORs, the HVAC system was equipped with high-efficiency particulate air filters, which could remove particles of ≥0.3 µm with an efficiency of 99.97% and provided at least 15 air changes per hour. Every operating room was equipped with an operating table and a lighting system consisting of three joined arms, each one holding three light lamps. A sliding door connected the ORs to the corridor.
Figure S2 shows the flowchart with the methodology steps followed in this research, and
Figure S3 displayed the 2D and 3D graphical representations of sensor locations in operating rooms. The surveillance comprised the microclimatic parameters (air temperature, relative humidity, and air velocity), air changes/hour, thermal comfort indices (or Fanger indices) PMV (predicted mean vote) and PPD (predicted percentage of dissatisfied), air pressure difference, number concentration of particles size ≥ 0.5 μm (p/m
3), and the anesthetic gases (nitrous oxide and the halogenated gases such as sevoflurane and desflurane). The parameters chosen for this study fall within the primary environmental controls regulated by the Public Health Department at healthcare facilities in the Campania Region. These controls were selected because they are representative of the air quality in ORs and form the basis of the chemical-physical controls required by Italian technical standards. Additionally, a significant amount of data was available. The evaluation of microclimatic conditions within the ORs was conducted using a data acquisition instrument (model: LSI Lastem microclimate control unit) and a data logger (M-Log) (
Figure S4), in accordance with regulations [
25] in “at rest” (t
0, operating room not in operation) and “in operation” (t
1, during the surgical procedure) conditions [
10,
25]. This instrument comprises a multi-acquisition device affixed to a mobile and adjustable stand, connected to a set of sensors. These sensors include a psychrometer with forced ventilation and a distilled water tank to monitor dry-bulb temperature and relative humidity. Additionally, a globe thermometer was used to ascertain the mean radiant temperature, and a hot-wire anemometer was employed to measure airspeed. The sampling time for these kinds of monitoring was at least 30 min.
Depending on the requirements, the measurement of air changes per hour was conducted using either an ESV202 vane anemometer probe (measurement range 0.2 ÷ 20 m/s; uncertainty: 5%) or an ESV307 hot-wire anemometer probe (measurement range 0.01 ÷ 20 m/s; accuracy: ±10 cm/s for 0.5 ÷ 1.5 m/s, 4% for air velocities > 1.5 m/s), both connected to an M-LOG multi-data logger (model ELO009) from L.S.I. Thermal comfort assessment utilized PMV and PPD indices. The method is based on measuring microclimatic parameters and, after establishing variables such as physical activity performed/metabolic rate and type of clothing according to UNI EN ISO 7730:2006, it is possible to determine the human thermal comfort sensation using Fanger indices [
25,
26,
27]. This involved selecting, from a specific menu, the energy expenditure (MET) of individuals present in the operating room (both operators and patients) and the thermal resistance provided by their clothing (CLO). The values assumed for this study were MET = 1.4 and CLO = 0.7 [
28,
29]. For optimal thermal comfort values, the PPD should be ≤10%, while the PMV has a scale of values ranging from −3 (very cold) to +3 (very hot) with the value 0 intended as optimal.
The measurement of the differential pressure between the OR and the surrounding environments was performed using a Testo Model 512 manometer, type 2 hPa (measurement range: 0 ¸+2 hPa; accuracy: 0.5% of full-scale reading ± 1 digit; resolution: 0.001 hPa), following the guidelines [
30,
31]. The measurement was conducted with all openings of the room sealed towards the surrounding environments. The assessment of the room’s overpressure level was carried out between the interior of the room and the surgical washing area or any adjacent space. The minimum pressure difference between the OR and surrounding environments must be at least 5 Pascal, as stipulated by the “Guidelines for Defining Safety and Hygiene Standards in the Operating Department (I.S.P.E.S.L. 2009)” [
31].
To determine the airborne particle concentration, a particle counter, model Lighthouse Solair 3100 Gene A.M. Instruments, was used. This device is an active sampler, capable of aspirating an air volume of 28.3 L/min and simultaneous particle counting in six channels (0.3–0.5–1.0–3.0–5.0–10 µm). The counter is completed with an isokinetic sample probe, which must be directed towards the air flow: if the direction of the air flow to be sampled cannot be determined (e.g., non-unidirectional air flows), it is necessary to position the probe vertically.
The volume of each individual sample, V
s, per sampling point is determined with the following equation:
where:
V
s is minimum volume of each single sample per point, expressed in liters (L); C
n,
m represents the class limit (number of particles/m
3) for particles having the largest dimension considered, specified for the relative class; 20 is the defined number of particles that could be counted if the concentration was at the class limit; and 1000 is the conversion factor to express the volume in liters (L) [
30]. For the determination of airborne particles, the regulation indicated that for each sampling point, an air sample volume of at least 2 L had to be aspirated, with a minimum sampling time of 1 min.
The measurement of ambient concentrations of gaseous and volatile anesthetics involved the use of a Brüel & Kjaer Model 1302 (Ballerup, Denmark) active multigas sampler, a portable, automatic, and continuous analyzer based on the principle of “infrared photoacoustic” technology. This sampler was connected to a Brüel & Kjaer Model 1302 (Ballerup, Denmark) multipoint sampler, an additional instrument enabling real-time monitoring of anesthetic concentrations in multiple zones of the ORs. The aforementioned equipment has a quantification limit of 0.03 ppm for nitrous oxide (with a repeatability of 1%) and a quantification limit of 0.01 ppm for sevoflurane and desflurane (with a repeatability of 1%). In ORs, the measurement of ambient concentrations of gaseous and volatile anesthetics was conducted by placing the multigas analyzer in a fixed position, as close as possible to the surgical field, specifically near the anesthesia cart in the area most occupied by OR personnel. For the evaluation of anesthetic gas concentrations, the average sampling time during the operating session had to be at least 180 min, while in the simulation, the average sampling time had to be at least one hour. The inlet tubing for pollutant capture was positioned at a height as close as possible to the respiratory pathways of the surgical team, with data acquisition programmed at 2 min intervals.
Table S1 details the technical specifications of all instruments used for measuring the environmental parameters in operating rooms. The instruments used for the environmental monitoring are subject to annual calibration as required by ACCREDIA Italian Accreditation, at accredited calibration centres. In the
Supplementary Materials,
Table S1 provides information about the instruments used, including the instrument model, measurement range, and the date of the last calibration.
Data Analysis
The acquired data were processed using advanced tools equipped with sophisticated software. The measurement of air changes per hour was conducted using the M-LOG multi-data logger (model ELO009) from L.S.I. To calculate the number of air changes per hour, the ratio between the volume of air supplied by the system per hour and the volume of the analyzed environment was considered. Measurement of the supply air volume flow rate is carried out to ascertain the air volume supplied to the cleanroom. The supply air volume flow rate is measured downstream of the final filters, approximately 150 mm to 300 mm from the filter face. The air velocity was measured on the outer surface of the terminal filters of the duct (outlets). To avoid overestimating and to obtain a more accurate measurement of the air velocity and, consequently, of the number of air changes, multiple sampling points across the surface of the duct’s filters were used. The measurement points had to be sufficient in number to determine the supply air flow rate: the total flow rate was given by the sum of the flow rates measured at each supply outlet. The air velocity measurement was conducted at a number of points n of the outlet according to the following formula:
where S is the area (m
2) affected by the flow.
In general, whether the ventilation and air conditioning system was unidirectional (laminar flow) or non-unidirectional (turbulent flow), the sampling time had to be sufficient to ensure the repeatability of the reading [
31,
32].
The method relies upon the measurement of the velocity of air passing through a known area, the air volume flow rate being the product of velocity and area (Equation (3)):
where:
Ac: cell area, which is defined as the free area of the media divided by the number of measuring points in m2.
Q: total air volume flow rate in m3/s.
Vn: air flow velocity at each cell centre in m/s.
The microclimate parameters (air temperature, relative humidity, and air velocity values) were processed with Gidas-Tea software (version 1.8.0.0) integrated into a BABUC system to obtain the PMV and PPD values. The measured differential pressure between the OR and the surrounding areas was processed following the guidelines outlined in the UNI EN ISO 14644-1 standard [
30]. To quantify the airborne particle concentration, LMS XChange software (version 1.6) was used. Data regarding the concentrations of gaseous and volatile anesthetics were recorded and analyzed with the instrument used to collect the samples (Brüel & Kjaer Model 1302, (Ballerup, Denmark) active multigas sampler). Data were managed with Microsoft Excel 2010. The average air quality values obtained were compared with the reference limits (RLs) defined by the recommended standards.
3. Results
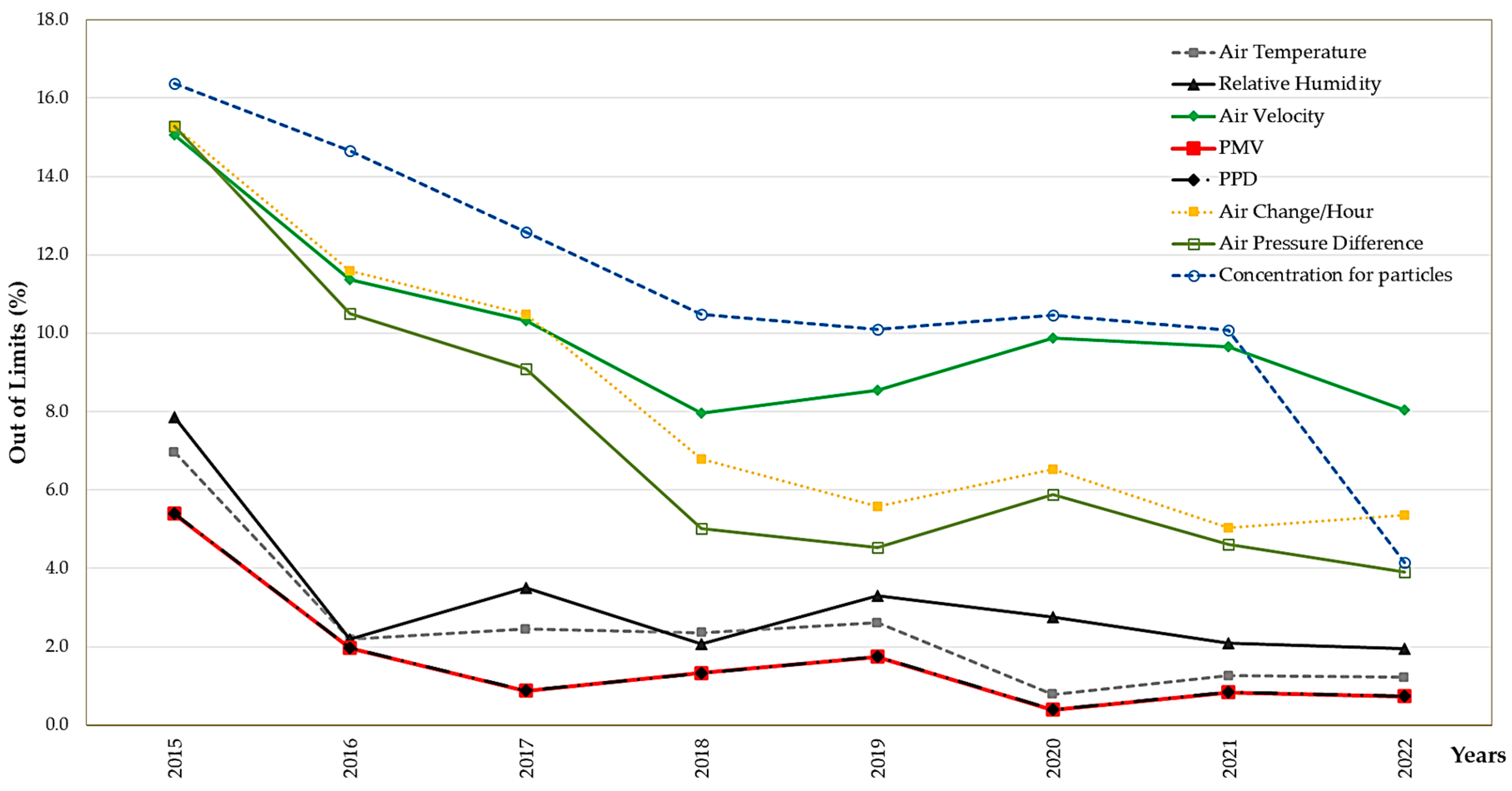
In the period 2015–2022, environmental monitoring was conducted in a total of 141 ORs in Campania Region, southern Italy. Due to technical and organizational factors (such as the room’s specialization, maintenance activities, air conditioning system upgrades, etc.), the number of investigations conducted per room varied annually, as indicated in
Figure 1 and
Table 1 and
Table 2.
In fact,
Table 1 and
Table 2 indicate the type, number, and data of air monitoring control measurements carried out in 141 ORs, while the percentage trend of the environmental parameters analyzed as unfitted values are shown in
Figure 1.
The total number of control measurements conducted in the ORs corresponds to 3627, among which microclimatic parameters (
n = 720) were the most frequently monitored. As reported in
Table 1, among the analyzed parameters, values out of limits for lower (mean value 19.4 ± 0.43) and upper air temperature limits (mean value 24.8 ± 0.5) were found.
Relative humidity (RH) data, indicated in
Table 1, show that the median values for relative humidity deemed unsuitable in ORs due to surpassing both the upper (60%) and lower limits (40%) were 66 and 36.1, respectively (
Figure 2). In general, the air velocity (AV) samples evaluated were deemed unsuitable, with the median values surpassing the lower limit for air speed (0.05 m/s) recorded as 0.03 m/s and the upper limit (0.10 m/s) recorded as 0.19.
Figure 2 shows the concentrations and out-of-limit values obtained for the determination of air speed, relative humidity, and PPD.
Figure 2 shows the results and limits of air temperature and air velocity from monitoring conducted during the study years 2015–2022, while those of relative humidity, PPD, and PMV are displayed in
Figure 3. The Fanger indices developed for healthcare professionals indicated thermal discomfort in 2.0% of cases. In particular, for PMV values (
Table 1,
Figure 3) the percentage of out of limits for the lower limit was 0.8% and for the upper limit 1.2% of the number of total cases. Moreover, about 8.4% of the total examined air changes/hour did not conform to the reference values (
Table 1;
Figure 1); in particular, the unsuitable ORs had an air changes median of 6 ± 3.
Figure S2 shows the concentrations of air pressure difference (Pa) found in monitored ORs, with out-of-limit values of approximately 7% across the total number of cases.
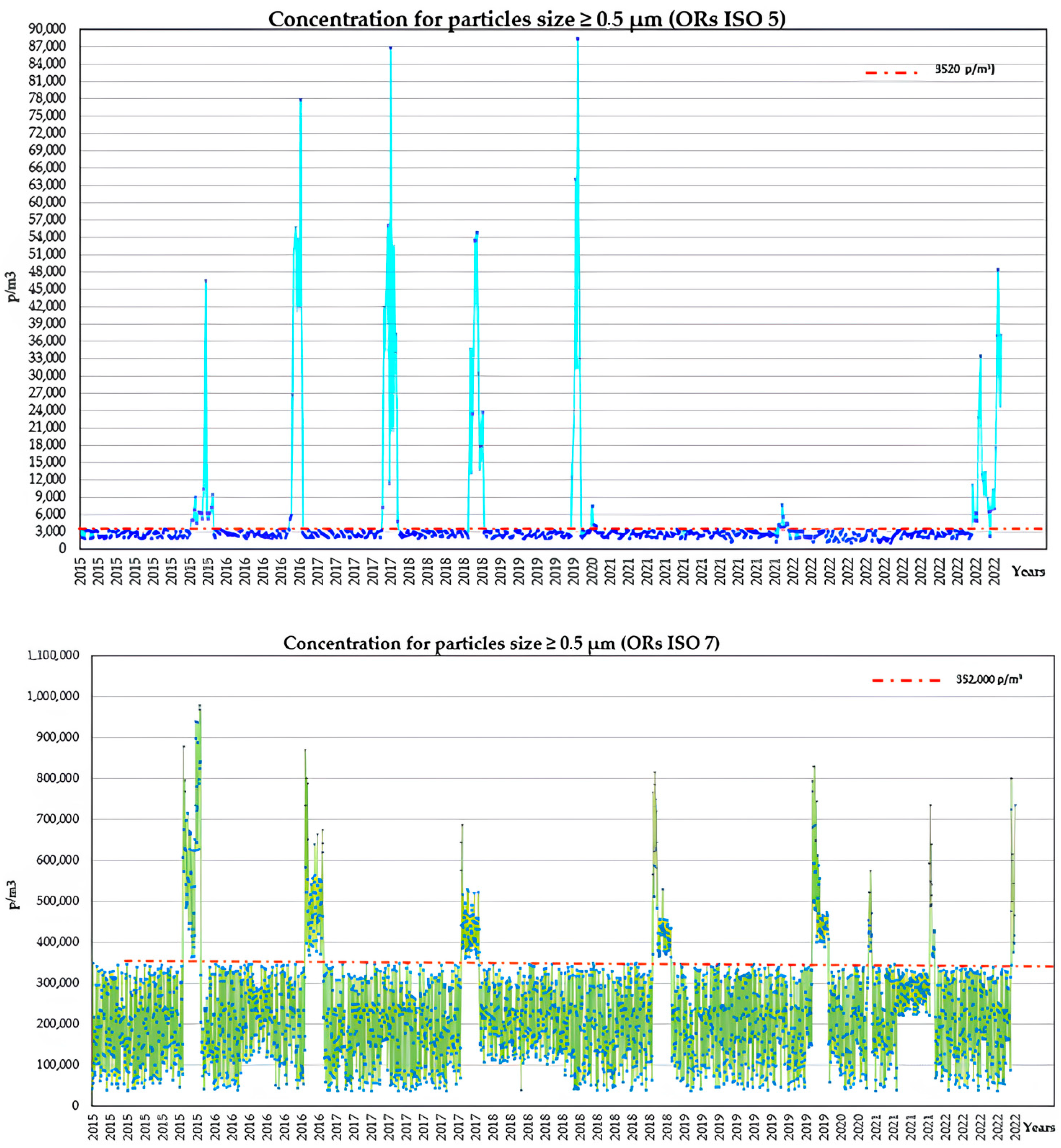
Regarding particle concentration,
Table 1 and
Figure 4 indicated that for ISO 5 cleanrooms out of 656 measurements, an unsuitability percentage of 12.7% (N = 83) was found, referring to the maximum allowed limit of 3520 p/m
3 for particles ≥ 0.5 µm. Meanwhile, for ISO 7 cleanrooms out of 2971 measurements, an unsuitability percentage of 11.1% (N = 331) was found, referring to the maximum allowed limit of 352,000 p/m
3 for particles ≥ 0.5 µm [
25,
30,
32]. In the unsuitable ISO 5 cleanrooms, the average observed particle concentration was 22,686 ± 20,982 (range: 3776 ÷ 88,394), whereas in the unsuitable ISO 7 cleanrooms, the average observed particle concentration was 507,017 ± 133,431 (range: 360,382 ÷ 977.831).
Finally, 5578 measurements of anesthetic gas (N
2O, sevoflurane and desflurane) were made (
Figure 5 and
Table 1 and
Table 2). An evaluation of the results indicated that, for the identification of N
2O, it is possible to estimate a non-conformity condition regarding the TLV-TWA 50 ppm assumed as the limit for ORs built and/or rebuilt after 1989. In fact, for 1951 measurements, an unsuitability percentage of 4.5% (N = 87) was found, and the average observed N
2O concentration was 142.92 ± 31.82 (range 54.7 ÷ 197.31) [
35]. There was an estimated non-conformity for sevoflurane control in 5.6% (N = 13) of samples compared with the TLV ceiling (2 ppm).
According to the results of the monitoring conducted only during weekdays, the ORs under investigation exhibited varying air quality indices depending on the type of surgery being performed and the size of the space. Specifically, the air temperature differed based on the type of surgical procedure; for instance, cardiothoracic operating rooms required lower temperatures for patient comfort during operations, while orthopedic operating rooms preferred slightly higher temperatures to facilitate the handling of medical instruments. Air velocity, crucial for maintaining a sterile and comfortable environment, varied according to the layout and size of the room: larger operating rooms or those with more complex equipment required higher air velocity to ensure adequate air exchange. Relative humidity, generally maintained at around 50–60% in all operating rooms, showed no significant variations as it was regulated to prevent mucosal dehydration and ensure patient comfort, regardless of the room type. Air changes per hour varied depending on the type of surgical procedure, with high-risk operating rooms requiring more frequent air changes to maintain optimal safety conditions. The concentration of particles of specific sizes depended on the efficiency of the air filtration systems. Particularly, operating rooms with very high sterility requirements (such as prosthetic surgery, ophthalmology, vascular surgery, spinal surgery, thoracic surgery, etc.) belonged to ISO 5 cleanroom standards, while operating rooms without prosthetic implants (such as delivery rooms, urology, gynecology, hemodynamics, etc.) conformed to ISO 7 cleanroom standards. The concentration of anesthetic gases varied based on the type of procedure and the room’s ventilation: operating rooms for long procedures required advanced gas recovery systems. The air quality of the different operating rooms was evaluated in two modes: “at rest” (empty room) and “in operation” (during procedures). Environmental monitoring, such as air changes and particulate concentration, was conducted only in “at rest” mode, while the evaluation of microclimatic conditions, such as relative humidity, air velocity, and air temperature (used to calculate Fanger indices), within the ORs was conducted in both “at rest” and “in operation” modes. The PMV and PPD values obtained did not show significant variations related to the evaluation mode. Anesthetic gas monitoring was performed in both modes for each measure because, in the case of out-of-limit values, the causes could be attributed to multiple factors detectable only with this type of monitoring. These causes could include leaks from high-pressure circuits (connections between the central distribution system outlets and the anesthesia machine) or leaks from low-pressure circuits (anesthesia machine circuits from the flowmeters to the patient) detected during the initial monitoring phase in “at rest” mode, and gas leaks during inhalation anesthesia when the mask did not fit the patient’s face correctly, measured during the second monitoring phase in “in operation” mode.
4. Discussion
The results of this study emphasize the critical importance of strict adherence to established protocols within operating rooms to maintain high safety standards. This study’s findings highlight several key areas of concern and provide insight into how to better manage operating room environments for both patient and staff safety.
The study highlights the necessity of educating staff on proper procedures such as thorough handwashing, environmental sanitization, and the appropriate use of personal protective equipment (PPE). These protocols are essential for reducing risks and ensuring effective facility maintenance. Adherence to these procedures helps prevent the spread of infections and maintains a sterile environment, which is crucial in a surgical setting.
The microclimatic monitoring results revealed that out of 3627 checks conducted, 720 (19%) were outside the acceptable limits. This finding underscores the need for rigorous monitoring and control of environmental parameters within operating rooms. Air velocity was the parameter most frequently found to be out of compliance, influencing the need for air changes. Specifically, 303 (8%) of the checks exceeded the threshold value for air changes per hour. This finding aligns with other studies, which emphasize the im-portance of continuous monitoring of environmental parameters to improve air quality and for effective management: enhancing air quality is essential for the comfort and work quality of healthcare staff and patients. Inadequate air changes can lead to a buildup of contaminants, potentially increasing the risk of infection [
9,
35,
36]. The ISPESL guidelines emphasize maintaining specific temperature (20–24 °C), humidity (40–60%), air velocity (<0.15 m/s), and at least 20 air changes per hour in ORs. This study focused on internal controls, finding that deviations from these parameters were due to HVAC malfunctions, not external conditions, stressing the need for regular system maintenance to ensure optimal operation and isolation from outside influences [
32].
The study also assessed the thermal comfort status in the operating rooms using the Fanger indices (PMV and PPD). Out of 3627 microclimatic controls, 71 (2%) values exceeded the limits. This indicates challenges in balancing thermal comfort and environmental conditions in healthcare facilities. Maintaining an optimal thermal environment in operating rooms is particularly difficult due to the diverse activities and varying needs of patients and surgical staff. The different physiological characteristics and attire of individuals further complicate maintaining optimal thermal comfort levels [
10,
27,
37]. Thermal comfort is crucial not only for the well-being of the staff but also for ensuring that patients are not subjected to unnecessary stress or discomfort during surgical procedures.
Additionally, the study evaluated the concentration of halogenated anesthetic gases (sevoflurane and desflurane) and nitrous oxide to assess occupational exposure levels. The results showed that the highest concentrations exceeding the limits were found for halogenated anesthetic gases, with sevoflurane showing 12.8% and desflurane 13.2% of values above the limit. This highlights the need for effective ventilation and regular monitoring to ensure the safety of healthcare personnel, which could be further controlled by analyzing individual exposure through the detection of metabolites in urine. Exposure to high concentrations of anesthetic gases can have serious health implications for staff, including respiratory issues and other long-term health problems. It is important to note that there is currently conflicting information regarding recommended exposure limits among European Union countries and beyond. This is likely due to the inability to determine safety levels for direct exposure to these halogenated anesthetic gases [
38]. For instance, in England, the time-weighted average (TWA) exposure limits for an 8 h working period have been set at 50 ppm for halogenated anesthetic gases, while in other European countries, recommended limit values range from 2 to 10 ppm for an 8 h work exposure [
39]. Finally, the American NIOSH guidelines recommend a limit value of 2 ppm for the administration of individual halogenated anesthetic gases [
9,
40,
41]. Therefore, it is imperative to implement effective strategies for controlling and reducing anesthetic gas concentrations in the operating room environment. In this study, the Italian national standards were referenced to ensure the relevance and applicability of the results to the local context. Although the valuable guidance provided bycited legislation is acknowledged, the Italian standards were chosen due to their alignment with local climatic, cultural, and legislative conditions [
42,
43,
44,
45].