Abstract
International air quality indexes (AQIs) are derived from air pollution and are essential global tools for mitigating diseases such as asthma, as they are used to reduce exposure to triggers. The aim of this article is to systematically review the global literature on the use of AQIs in asthma-related studies. To evaluate the importance of the variables considered, a citation frequency index (Q) was used. The results suggest that the most frequently reported air pollutants related to asthma are PM (Q3) > NO2 (Q3) > O3 (Q3) > CO (Q3) > NO (Q3) > SO2 (Q3). In addition, climate variables play a relevant role in asthma research. Temperature (Q4) emerged as the most relevant climate variable, followed by atmospheric pressure (Q3) > wind direction (Q3) > solar radiation (Q3) > precipitation (Q3) > wind speed (Q3). AQIs, specifically the U.S.EPA Air Quality Index and the Air Quality Health Index, are directly associated with air pollution and the prevalence, severity and exacerbation of asthma. The findings also suggest that climate change presents additional challenges in relation to asthma by influencing the environmental conditions that affect the disease. Finally, this study provides a comprehensive view of the relationships among air quality, air pollutants and asthma and highlights the need for further research in this field to develop public health policies and environmental regulations.
1. Introduction
Increasing urbanization has exacerbated public health problems related to air quality [1,2]. Urban dwellers are exposed to pollutants such as nitrogen dioxide (NO2), volatile organic compounds (VOCs), sulfur dioxide (SO2), carbon monoxide (CO), ozone (O3) and particulate matter (PM), which increase the risk of cardiovascular and respiratory diseases, causing premature death [3]. Air quality is a global problem since pollutants can be dispersed through wind and atmospheric conditions, affecting less polluted areas and causing harm to humans, plants and animals [4,5]. Factors such as population density and health, environmental, economic and climatic characteristics also increase urban air pollution, generating adverse impacts on human health [6]. Since 2005, approximately 35 million people have died from chronic respiratory diseases, and an increase in the number of deaths associated with these diseases, especially asthma, is expected [7]. Undoubtedly, air pollution is a significant risk factor for human health and affects quality of life [8,9].
To mitigate diseases caused by air pollution and improve quality of life, international air quality indexes (AQIs) have been implemented globally [10]. AQIs, which are dimension less values calculated from one or more criteria air pollutants, represent the atmospheric concentration and its possible effects on human health, facilitating community understanding of air quality in a specific place and time [11,12]. These indexes provide information on the permitted limits, which are distributed at different levels and represented by a color coding that can vary according to the country [13]. AQIs inform the community about air quality and offer recommendations for the general well-being of the population [14]. However, in developing countries, there is little information on the relationship between asthma health factors (AHFs) and medical exacerbations (e.g., respiratory and cardiovascular diseases) due to exposure to air pollution [15,16]. Current AQIs do not allow the prediction or detection of increases in emergency room admissions for asthma exacerbations, as they are based on concentrations measured in real time at automated monitoring stations [17,18]. According to Rosser et al. [19], given that these indexes are obtained by calculating the concentrations measured daily without considering the temporal and spatial variations in air pollution, it is likely that certain exposure will be incorrectly categorized. This situation could be the main reason for the lack of connection between AQIs and public health [20].
Air pollution, defined by the World Health Organization (WHO) as the presence of harmful substances in the atmosphere, has intensified with economic, social and political development; these changes thus affect air quality and human health [21]. This phenomenon, together with climate conditions, has emerged as a critical factor that can compromise public health, increasing the incidence of respiratory diseases [22]. AQIs play an important role in protecting public health, especially in regard to respiratory diseases such as asthma and chronic obstructive pulmonary disease. These indexes evaluate the levels of pollutants in the air, allowing the population and authorities to take informed preventive measures [23]. For conditions such as asthma, where air quality can trigger and aggravate symptoms, AQIs offer a useful guide for reducing exposure to triggers. By providing up-to-date and accurate information on air quality and its effects on human health, they allow communities to make conscious decisions about their health [24].
At the global level, AQIs have been established to assess air pollution and its possible impact on human health [13,14]. Among the most recognized AQIs are the World Health Organization Air Quality Index (WHO-AQI), the U.S.EPA Air Quality Index (U.S.EPA-AQI), the European Union Air Quality Index (EU-AQI) and the China Air Quality Index (CN-AQI) [25,26]. The widely used U.S.EPA-AQI considers parameters such as PM2.5, PM10, O3, NO2, SO2 and CO. The WHO-AQI is based on the WHO guidelines and evaluates the same pollutants [27]. Although these indexes share the objective of providing understandable information on air quality, the differences in their thresholds and methodologies have prevented their total unification in the context of public health [28,29]. The variability of these indexes at the global level is due to factors such as heterogeneity in exposure to pollutants, epidemiological profiles and country-specific regulations, which makes it difficult to unify criteria in relation to risks to human health [30]. The most cited AQIs worldwide, such as the U.S.EPA-AQI and the WHO-AQI, have been used in various regions to assess and report on air pollution levels and their effects on public health [31]. In China, the CN-AQI has been used as part of government efforts to address serious air pollution in cities such as Beijing. This index has contributed to increasing awareness of the health risks associated with air quality and has promoted mitigation measures to reduce exposure to air pollutants [32].
In Europe, the European Union uses the EU-AQI to report on air quality in various regions, facilitating informed decisions by citizens about their outdoor activities [11]. In Canada, the AQHI has been effective in alerting people with respiratory problems to potential risks and promoting protective behaviors such as limiting outdoor exposure during periods of poor air quality [33]. These experiences highlight the usefulness of AQIs for generating public awareness and promoting preventive measures against air pollution [34]. However, they also emphasize the importance of adapting these indexes to local conditions and the needs of the population, recognizing the differences in pollutant profiles and risk levels in different parts of the world [30,35].
The main objective of this article is to systematically review the literature worldwide on the use of AQIs in asthma-related studies. The main air pollutants associated with asthma are identified based on their citation frequency in scientific databases. The climate variables most considered by the AQIs are also identified. Lastly, a worldwide spatiotemporal analysis is carried out based on the use of the different AQIs. In the context of air pollution and asthma, this study is relevant because of the following practical aspects: (1) it deepens the knowledge associated with the application of AQIs in asthma studies; (2) it considers critical air pollutants from mitigation and public health intervention perspectives; (3) it analyzes the relevance of climate variables to better understand their interactions with air pollution and their effects on public health; (4) it provides relevant information to visualize AQI optimization strategies in relation to asthma.
2. Materials and Methods
2.1. Bibliographic Search System
A systematic review of the literature was carried out to analyze the use of AQIs, air pollutants and climate variables in studies on asthma worldwide between 2011 and 2022. Various scientific databases, including Google Scholar, Science Direct, Springer Link and Taylor & Francis, were used. These databases were selected because of the significant number of documents detected according to the main objective of this study and because of their use in literature review studies on air pollution and asthma [36,37,38]. The review process was carried out following the methodology proposed by Zafra et al. [39]. During this review, the total content of the documents detected in the databases selected for this study was exhaustively considered.
2.2. Bibliographic Analysis System
The bibliographic analysis was structured in four phases: (I) a general search, (II) the detection of the most studied air pollutants in the context of asthma, (III) the identification of the main climate variables and (IV) the classification of the existing air quality indexes. These phases were based on a citation frequency index (Q) and were used to study the importance of the detected air quality and asthma variables [40]. The Q indexes were averaged, and the following four quartile ranges were established: Q1 = 0.00–0.24, Q2 = 0.25–0.49, Q3 = 0.50–0.74 and Q4 = 0.75–1.0. In this study, it was assumed that the relationship between air quality and asthma could depend on the frequency of citations in the databases consulted. That is, the Q1 quartile could be associated with less important air quality and asthma assessment methods, while the Q4 quartile could be linked to issues of greater relevance worldwide.
Phases of Bibliographic Analysis
Phase 1: In the initial phase of the bibliographic search, the following keywords were used: (I) index, (II) air pollution and (III) asthma. During this phase, the following information inclusion criteria were applied in line with the objectives of this study: (I) articles related to air quality and asthma, (II) articles related to air pollution, (III) articles related to asthma and (IV) articles related to AHFs and asthma. These information inclusion criteria were assumed based on the main objective of this study: air quality indexes and asthma. In this phase of analysis, 32,665 relevant documents were identified in all the selected databases (information universe). The database that registered the largest number of documents was Google Scholar, with a total of 20,800 documents, which represented 63.7% of the total information (Table 1). The Science Direct database had 4859 documents (14.9%). The Springer scientific database contributed 4497 documents (13.8%), while Taylor & Francis contributed 2509 documents (7.68%).
Phase 2: From the keywords selected during phase 1, the search filters (keywords) of the Springer, Science Direct and Taylor & Francis databases were used. This approach was used to detect additional keywords in the context of the main air pollutants reported in asthma studies. The keywords detected were as follows (Table 1): nitrogen dioxide, ozone, nitric oxide, particulate matter, sulfur dioxide and carbon monoxide. In addition, in this phase, a stratified sample was selected from the total number of documents detected in phase 1 for each database considered. The sample size assumed was 50 documents in total. Thus, 63.7% (31 documents), 14.9% (7 documents), 13.8% (7 documents) and 7.68% (4 documents) of the first 50 documents detected according to their relevance in the Google Scholar, Science Direct, Springer Link and Taylor & Francis databases, respectively, were selected. The final sample size established then corresponded to 49 documents. Based on these documents, the main air pollutants in asthma studies were analyzed again (Table S1).
Phase 3: The third phase of the review was carried out to organize the subcategories of analyses related to climate variables in studies on asthma and, thus, to establish their relationships with the detected AQIs. Once again, the citation frequency index (Q) was used [39]. During this phase, the following additional keywords were detected and incorporated (Table 1): precipitation, wind speed, wind direction, temperature, atmospheric pressure and solar radiation. The information inclusion criterion during this phase was based on studies that addressed the climate variables used in AQIs. During this phase, the 49 documents selected in phase 2 were again analyzed (Table S1).
Phase 4: During this phase, an analysis was carried out on the spatiotemporal trends of the detected variables [41]. This trend analysis considered the citation frequency index (Q) and the classification obtained for the AQIs in studies on asthma on a global scale. This trend analysis was performed from the 49 documents selected (sample size according to its relevance) from the databases considered (Table S1).
2.3. Statistical Analysis
Statistical tests were carried out to study the main variables of interest in the context of air pollution and asthma. A database was built in Microsoft Excel (V.2017) to analyze the spatiotemporal distribution of the documents detected (Table S1) [42]. Descriptive statistics and reasons were used to establish an order of hierarchy in the AQIs and to study their spatiotemporal trend [43]. Finally, a cluster analysis [44] was performed by using SPSS V.25 software [45] to group the variables considered in the context of this study (construction of a dendrogram).

Table 1.
Order of world importance for air pollutants, variables used and air quality indexes detected.
Table 1.
Order of world importance for air pollutants, variables used and air quality indexes detected.
| Phase | Keywords | Science Direct | Springer Link | Google Scholar | Taylor & Francis | Total Documents Detected | Average Q Index | Mean Quartile | Quartile Variation | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Detected Documents | Q Index | Detected Documents | Q Index | Detected Documents | Q Index | Detected Documents | Q Index | ||||||
| Information universe | Index, Air Pollution and Asthma | 4859 | 1.00 | 4497 | 1.00 | 20,800 | 1.00 | 2509 | 1.00 | 32,665 | 1.00 | Q4 | Q4,Q4,Q4,Q4 |
| Air pollutants | Index, air pollution, asthma and nitrogen dioxide | 1602 | 0.33 | 1469 | 0.33 | 17,900 | 0.86 | 748 | 0.30 | 21,719 | 0.66 | Q3 | Q2,Q2,Q4,Q2 |
| Index, air pollution, asthma and ozone | 1651 | 0.34 | 1503 | 0.33 | 16,500 | 0.79 | 809 | 0.32 | 20,463 | 0.63 | Q3 | Q2,Q2,Q4,Q2 | |
| Index, air pollution, asthma and nitric oxide | 892 | 0.18 | 785 | 0.17 | 17,600 | 0.85 | 479 | 0.19 | 19,756 | 0.60 | Q3 | Q1,Q1,Q4,Q1 | |
| Index, air pollution, asthma and particulate matter | 2636 | 0.54 | 2001 | 0.44 | 17,200 | 0.83 | 1021 | 0.41 | 22,858 | 0.70 | Q3 | Q3,Q2,Q4,Q2 | |
| Index, air pollution, asthma and sulfur dioxide | 1206 | 0.25 | 1159 | 0.26 | 15,700 | 0.75 | 651 | 0.26 | 18,716 | 0.57 | Q3 | Q2,Q2,Q4,Q2 | |
| Index, air pollution, asthma and carbon monoxide | 1191 | 0.25 | 1070 | 0.24 | 17,100 | 0.82 | 627 | 0.25 | 19,988 | 0.61 | Q3 | Q2,Q1,Q4,Q2 | |
| Climate variables | Index, air pollution, asthma and precipitation | 782 | 0.16 | 1007 | 0.22 | 15,200 | 0.73 | 494 | 0.20 | 17,483 | 0.54 | Q3 | Q1,Q1,Q3,Q2 |
| Index, air pollution, asthma and wind speed | 898 | 0.18 | 1233 | 0.27 | 14,900 | 0.72 | 320 | 0.13 | 17,351 | 0.53 | Q3 | Q1,Q2,Q3,Q1 | |
| Index, air pollution, asthma and wind direction | 681 | 0.14 | 1181 | 0.26 | 16,800 | 0.81 | 195 | 0.08 | 18,857 | 0.58 | Q3 | Q1,Q2,Q4,Q1 | |
| Index, air pollution, asthma and temperature | 2806 | 0.58 | 2812 | 0.63 | 17,100 | 0.82 | 1275 | 0.51 | 23,993 | 0.73 | Q4 | Q3,Q3,Q4,Q3 | |
| Index, air pollution, asthma and atmospheric pressure | 931 | 0.19 | 1218 | 0.27 | 17,900 | 0.86 | 651 | 0.26 | 20,700 | 0.63 | Q3 | Q1,Q2,Q4,Q2 | |
| Index, air pollution, asthma and solar radiation | 498 | 0.10 | 710 | 0.16 | 17,600 | 0.85 | 172 | 0.07 | 18,980 | 0.58 | Q3 | Q1,Q1,Q4,Q1 | |
| Air quality indexes | Index, air pollution, asthma and Common Air Quality Index | 2672 | 0.55 | 3167 | 0.70 | 18,300 | 0.88 | 1286 | 0.51 | 25,425 | 0.78 | Q4 | Q3,Q3,Q4,Q3 |
| Index, air pollution, asthma and Air Quality Index | 3899 | 0.80 | 3926 | 0.87 | 19,000 | 0.91 | 1831 | 0.73 | 28,656 | 0.88 | Q4 | Q4,Q4,Q4,Q3 | |
| Index, air pollution, asthma and Air Quality Health Index | 3805 | 0.78 | 3873 | 0.86 | 9010 | 0.43 | 1273 | 0.51 | 17,961 | 0.55 | Q3 | Q4,Q4,Q2,Q3 | |
| Index, air pollution, asthma and Air Pollution Tolerance Index | 743 | 0.15 | 1067 | 0.24 | 15,400 | 0.74 | 266 | 0.11 | 17,476 | 0.54 | Q1 | Q1,Q1,Q4,Q1 | |
| Index, air pollution, asthma and Arithmetically Aggregated Pollutant Index | 25 | 0.01 | 13 | 0.00 | 88 | 0.00 | 1 | 0.00 | 127 | 0.00 | Q1 | Q1,Q1,Q1,Q1 | |
3. Results and Discussion
3.1. AQIs, Air Pollutants and Asthma
During the initial phase of the bibliographic review, 32,665 relevant documents were identified. These documents were linked to the following keywords: (I) index (38.8%), (II) air pollution (36.7%) and (III) asthma (24.5%). The search was carried out in four selected databases: (I) Science Direct, (II) Springer Link, (III) Google Academic and (IV) Taylor & Francis. Google Scholar provided the highest volume of documents, with a total of 20,800 (63.7%). It was followed by Science Direct, which contributed 4859 papers (14.9%). Springer Link and Taylor & Francis contributed 4497 (13.8%) and 2509 documents (7.68%), respectively (Table 1).
The results show that the most frequently reported atmospheric pollutants related to asthma were suspended particles (PM2.5 and PM10), NO2, O3, SO2, CO and NOx (Table 2). PM, which originate from various sources, such as the burning of fuels and vehicular traffic, was associated with lung irritation and the induction of asthma attacks [46]. O3, formed by the reaction of nitrogen oxides and volatile organic compounds, was associated with irritation of the respiratory tract and reduced lung function [47]. SO2, whose generation is attributed mainly to the combustion of fossil fuels such as oil and coal, was identified as a potential irritant of the respiratory tract, exacerbating asthma symptoms [48,49]. NOx, which is produced by the combustion of fossil fuels in vehicles and power plants, was identified as a contributor to the formation of tropospheric ozone and fine particles, which aggravate asthma symptoms [4]. Finally, CO, which results from the incomplete combustion of fossil fuels, although not identified as a main trigger of asthma, was associated with the worsening of respiratory symptoms in individuals with preexisting asthma who were exposed to high levels of it [50].

Table 2.
Air pollutants, climate variables and air quality indexes in asthma studies.
The results show that PM and O3 were reported in 85.7% and 73.5% of the studies, respectively (Table 2). PM is a significant risk factor for people with asthma, as it can exacerbate symptoms, increase the frequency of asthma attacks and contribute to airway inflammation and damage [2]. O3, known for its irritant capacity in the respiratory tract, has various effects on human health depending on the concentration and duration of exposure [14]. NO2, which was mentioned in 75.5% of the studies, emerged as the main pollutant associated with asthma. This primary pollutant, emitted mainly by the combustion of gasoline in motor vehicles, was associated with irritation of the respiratory tract, causing symptoms such as coughing, chest pain and bronchitis [51]. SO2, present in 63.3% of the studies, was identified as an irritating gas for the respiratory tract that decreases lung function in patients with asthma [52], triggering symptoms such as shortness of breath and persistent cough. NO, reported in 14.3% of the studies, was related to shortness of breath, chest tightness, cough and wheezing [14]. Lastly, CO, a product of the incomplete combustion of organic material in oxygen-deficient environments, was also addressed in the reviewed literature [53]. Although it was not identified as a major trigger for asthma, it contributes to the disease by reducing the body’s ability to transport oxygen to tissues.
The results show the following order of importance for the air pollutants in the asthma studies: PM (85.7%) > NO2 (75.5%) > O3 (73.5%) > SO2 (63.3%) > CO (30.6%) > NO (14.3%). These data were obtained from the selected documents (Table 2). Regarding the climate variables, the following order of importance was observed: temperature (53.1%) > precipitation (24.5%) > wind speed (24.5%) > wind direction (16.3%) > solar radiation (16.3%) > atmospheric pressure (12.2%). Regarding the classification of AQIs, the order of importance detected was as follows: Air Quality Index (U.S.EPA-AQI; 46.9%), Air Quality Health Index (AQHI; 46.9%), Common Air Quality Index (CAQI; 10.2%), Arithmetically Aggregated Pollutant Index (AAPI; 4.1%) and Air Pollution Tolerance Index (APTI; 4.1%). Thus, these orders of importance offer a perspective on the most relevant air pollutants in relation to asthma and on the climate variables and the AQIs most used in research. This information can be used to guide future research and public health policies.
The results show that air pollution worldwide has had a significant impact on public health, exacerbating respiratory diseases such as asthma [54]. This problem has been intensified by social inequalities, with the most vulnerable populations being exposed to high levels of air pollutants [55]. This exposure increases the economic burden of asthma, representing a challenge for health systems and national economies [56]. However, air pollution mitigation faces political and regulatory challenges [57]. This situation elucidates the need for concerted political action and a collective commitment to promote stricter environmental regulations [58]. Addressing these challenges requires a global and collaborative response involving multiple stakeholders [59]. For example, in Latin America, the dynamics of air pollutants and their relationships with asthma are complex and influenced by factors such as accelerated urbanization, ongoing industrialization and limitations in environmental regulation [60]. Latin American cities face increases in air pollution due to the concentration of emissions from vehicular traffic, industry and residential heating [61]. Continuous industrialization has increased the emissions of pollutants such as SO2, NOx and PM [62]. Limitations in environmental regulation in some developing countries have resulted in high levels of air pollution in urban and industrial areas, increasing the exposure of the population to the risk of asthma and other respiratory diseases [50].
The results suggest that the socioeconomic vulnerability of certain groups, such as low-income groups, contributes to increased risks of exposure to air pollution, thus increasing the prevalence and severity of asthma [63]. Climate change influences the distribution and concentration of atmospheric pollutants in Latin America, affecting the formation of tropospheric ozone and other polluting particles, which has impacted the respiratory health of the population and the prevalence of asthma in the region [54]. Understanding the relationship between air pollutants and asthma is critical to addressing public health challenges on a global scale. The need to analyze both the spatial and temporal trends of these pollutants was highlighted. Such analyses can offer a comprehensive view of how air pollution affects the prevalence and severity of asthma in different regions of the world. Table 3 presents a detailed summary of the main spatiotemporal trends observed worldwide, elucidating the influence of various factors on air quality and respiratory health.

Table 3.
Spatiotemporal trend of air pollutants in the context of asthma.
The identification and understanding of the main air pollutants associated with asthma are fundamental for the effective management of this respiratory disease [71]. Exposure to pollutants such as SO2, PM2.5 and PM10 was associated with an increased risk of developing or worsening asthma [72]. This information has enabled the implementation of adequate preventive measures, such as stricter environmental policies and air quality monitoring programs [73]. Furthermore, it is essential to tailor asthma treatment according to environmental conditions, improve disease management and reduce the burden of symptoms for patients [74]. Public awareness of the health risks associated with air pollution can promote changes in individual behavior and more effective public health policies [75]. Lastly, the identification of air pollutants related to asthma has prompted ongoing research to develop more effective interventions and reduce the global burden of the disease [76].
3.2. AQIs, Climate Variables and Asthma
The results reveal the following six key climate variables in studies on asthma: precipitation (Q3), wind speed and direction (Q3), temperature (Q3), atmospheric pressure (Q4) and solar radiation (Q3). These climate variables are considered by the following AQIs: Common Air Quality index—CAQI (Q3); Air Quality Index—U.S.EPA-AQI (Q4); Air Quality Health Index—AQHI (Q4); Air Pollution Tolerance Index—APTI (Q3); and Arithmetically Aggregated Pollutant Index—AAPI (Q3) (Figure 1). Thus, temperature was the most frequently cited climate variable (Q3). It was followed, in order of importance, by precipitation (Q3) and wind speed (Q3) (Table 2). Solar radiation (Q3) was also mentioned with a significant frequency, while atmospheric pressure (Q4) was the least mentioned variable. These findings support the importance of considering a variety of climate variables in asthma studies to better understand their relationships with environmental and public health factors.
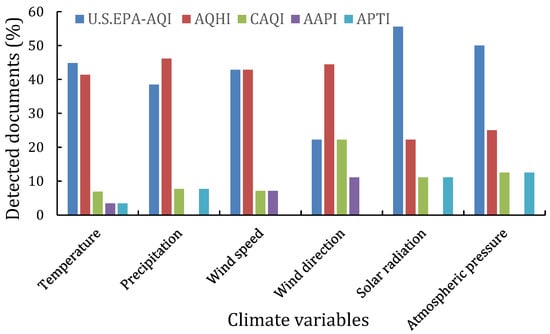
Figure 1.
Climate variables associated with air quality indexes in asthma studies (selected documents, n = 50). U.S.EPA-AQI = Air Quality Index, AQHI = Air Quality Health Index, CAQI = Common Air Quality Index, AAPI = Arithmetically Aggregated Pollutant Index and APTI = Air Pollution Tolerance Index.
The findings show that in asthma studies, it is relevant to consider various climate variables that influence the prevalence, severity and exacerbation of asthma (Figure 1) [77]. Temperature plays a significant role in the development and exacerbation of asthma, with extreme temperatures triggering symptoms in some people [78]. Air humidity in seasons of increased precipitation also influences asthma, as high humidity increases the concentration of allergens in the air. Conversely, in seasons of low precipitation and air humidity, airways tend to dry out [79]. Precipitation is able to wash pollen out of the air, benefiting some people with allergic asthma, but thunderstorms trigger symptoms in some people due to changes in atmospheric pressure and the release of allergens into the air [80]. Changes in atmospheric pressure, such as those that occur before a storm, trigger asthma attacks in some people [81]. Wind-transported allergens such as pollen or air pollution influence the appearance of asthma symptoms [82]. Exposure to air pollutants such as NO2, O3 and PM2.5 worsen asthma symptoms and increase the risk of exacerbations [72]. The relationships between these climate variables and asthma are complex and varied according to the person and their individual sensitivity [83]. Other factors, such as geography, season and exposure patterns, also influence how these climate variables affect people with asthma [84].
The asthma studies chosen considered climate variables due to their relevance in understanding this disease [85]. These variables, along with other asthma triggers, such as environmental allergens, air pollutants and respiratory infections, interact with and affect respiratory health [86]. The temporal and geographic variabilities in climate conditions play important roles in the manifestation of asthma [87]. Numerous epidemiological studies have demonstrated associations between climate variables and the incidence, prevalence and severity of asthma [88]. The findings revealed the pathophysiological mechanisms by which climate variables influence the development and exacerbation of asthma [89]. The consideration of climate variables in asthma studies was based on a combination of epidemiological evidence, pathophysiological knowledge and the need to understand and mitigate the risks associated with the disease to improve respiratory health and the quality of life of affected people [90].
The dendrogram based on the cluster analysis is a visual representation that groups the climate variables and air pollutants, showing complex patterns of interactions among the variables considered (Figure 2). A tendency to cluster in the direction and speed of wind was observed, which suggests an association with the dispersion of pollutants, where the wind could influence the direction and speed of propagation of atmospheric pollutants [91]. Similarly, a close grouping was observed among air pollutants, such as CO, NO2 and SO2, and PM and O3, which could have common emission sources or be influenced by similar climate factors. In addition, climate variables such as temperature, solar radiation, atmospheric pressure and precipitation showed a close association with air pollutants in the dendrogram, suggesting that climate could play a significant role in the dispersion and concentration of atmospheric pollutants, where factors such as temperature and solar radiation could affect chemical reactions and the formation of pollutants [92]. Additionally, a close grouping was observed between AQIs such as the U.S.EPA-AQI and the AQHI and air pollutants, indicating their direct association with air quality and its impact on public health [93]. Taken together, this cluster analysis provided a deeper understanding of the complex interactions between climate variables and air pollutants, elucidating the importance of considering multiple factors in assessing air quality and its impact on human health [94].
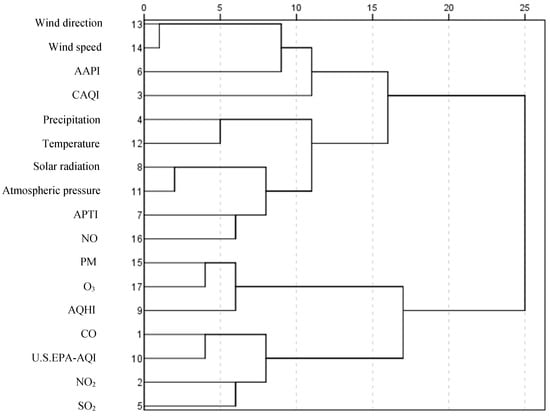
Figure 2.
Dendrogram of climate variables, air pollutants and AQIs in asthma studies. Dendrogram using a Ward linkage. Combination of rescaled distance clusters. U.S.EPA-AQI = Air Quality Index, AQHI = Air Quality Health Index, CAQI = Common Air Quality Index, AAPI = Arithmetically Aggregated Pollutant Index and APTI = Air Pollution Tolerance Index.
The results suggest that climate change presents additional challenges in relation to asthma by influencing the environmental conditions that affect the disease. Climate change was associated with an increase in the occurrence of phenomena such as heat waves, electrical storms and episodes of air pollution, which can trigger asthma exacerbations and increase the burden of the disease [95]. In addition, climate change can influence the distribution and season of environmental allergens such as pollen and mold, increasing the exposure of people with asthma to allergic triggers and potentially the prevalence and severity of the disease [96]. Likewise, climate change can affect air quality by influencing the formation of atmospheric pollutants such as ozone and fine particles, thus increasing the risk of asthma exacerbations and possibly contributing to the development of the disease in some people [97]. Global temperature rise and urbanization also play important roles in creating warmer urban environments and increasing exposure to heat and air pollution in urban areas, which could have negative consequences for people with asthma, especially those who live in disadvantaged environments or who have limited access to health care [95]. In terms of public health, climate change could increase the burden of respiratory diseases, including asthma, posing additional challenges for health care systems and public health in general [98]. Therefore, it is essential to develop adaptation and mitigation strategies to protect vulnerable populations and reduce the risks associated with asthma and other climate-related health problems [99].
The results show that the complex interaction among urban heterogeneity, climate conditions and air quality configures a challenging scenario for the study of asthma, especially in densely populated urban environments [100,101]. Thus, detailed characterization of urban heterogeneity, including land use typology, population density and urban infrastructure, is critical to understanding the spatial distribution of emission sources (anthropogenic and natural) and the dispersion patterns of air pollutants [102]. Natural and urban landscapes vary significantly in their ability to mitigate or exacerbate pollution. Green areas, such as parks and forests, area able to act as sinks for pollutants, while industrial and heavily trafficked areas contribute to their accumulation [103]. Climatic factors cannot be overlooked. The analysis of climate conditions, including weather patterns, primary pollutant concentrations and secondary pollutant formation, is instrumental in determining their influence on the transport, transformation and persistence of pollutants in the urban atmosphere. For example, thermal inversion episodes, which trap pollutants close to the ground, can aggravate air quality in densely populated urban areas [2,104]. Therefore, continuous air quality monitoring and calculation of AQIs, using standardized methodologies and considering relevant pollutants to understand and mitigate risks associated with asthma, provide essential information on air pollution exposure [14,105].
3.3. Spatiotemporal Trends
The research findings reveal that the most frequently examined AQIs, which comprised 46.9% of cases, considered both air pollution and asthma and included the U.S.EPA-AQI (Table 2). This index was placed in the fourth quartile (Q4), which indicated high relevance and frequency in research. Another AQI that also examines the relationship between air pollution and asthma was found, the AQHI. This index was found in the fourth quartile (Q4), covering the same percentage as the previous quartile (46.9%). However, other less common AQIs were detected but had equal relevance. One of them, the CAQI, which accounted for 10.2% of the cases, was linked to asthma and air pollution and was classified in the third quartile (Q3). This indicated that despite being less studied, it still holds considerable importance in research. In addition, less frequent AHFs were identified, each representing 4.1% of the cases. One of them, the AAPI, examined the relationships among air pollution and asthma, while the other focused on asthma and air pollution tolerance (the APTI). Both were classified in the first (Q1) and third quartiles (Q3). This analysis revealed the diversity of approaches to investigating the relationship between air quality and asthma, highlighting the importance of considering multiple dimensions in this field of study.
In relation to the temporal trend, the findings show a variation in the number of documents published annually, with peaks occurring in 2020 and 2021. In 2011, 2013 and 2016, 8% of the documents were published, while in 2012, 2014 and 2015, only 2% of the documents were published. These data were obtained from the documents selected in this study (Table S1). In 2017, an upward trend was observed; a total of 4% of the documents were published in 2017 and 2018, followed by a significant increase in 2019, when 14% of the documents were published. However, the most notable increases were recorded in 2020 and 2021, when 18% and 28% of the documents, respectively, were published. This increase in the last two selected years suggests a growing interest in the subject and greater research activity in this field. In relation to the spatial trend, a diversity of countries and continental areas were represented in the studies, with greater concentrations in North America (36%) and Asia (38%). When analyzing how the variables temporarily changed, an increase in the frequency of citations of certain air pollutants and climate variables was observed in recent years. For example, nitrogen dioxide (NO2), particulate matter (PM) and ozone (O3) have been increasingly studied, as evidenced by reports published in 2020 and 2021. In addition, variables such as wind speed and temperature have become relevant in recent research, as evidenced by published studies.
The results show that the continents with the greatest number of documents related to AQIs in the context of asthma were Asia > North America > Europe > Africa (Table S1). The Asian continent ranked first, with 57.1% of the documents, which were distributed mainly in countries such as China and India. It was followed by North America with a total of 36.7% of the documents, associated mainly with the United States. Europe and Africa made smaller contributions, 16.3% and 2% of the documents, respectively. This disparity in the production of documents possibly suggests differences in care and research on air quality and asthma in different regions of the world.
The findings suggest that air quality assessment is essential to understanding the impact of air quality on human health [106]. AQIs, which consider a variety of atmospheric pollutants, such as O3, NO2, SO2, PM2.5, PM10 and CO (Table S1), play essential roles in this process [107]. These pollutants were selected for their known adverse effects on respiratory health, including their ability to trigger or aggravate diseases such as asthma [108]. The indexes provide information on the concentration levels of these pollutants, which can be compared with air quality standards established by regulatory agencies to evaluate air quality and its possible impact on health [14]. The calculation methods used by the indexes are varied and specific; they combine information on different pollutants to generate a composite measure of air quality [26]. The results are interpreted and communicated in an understandable way for the public by classifying air quality into categories such as “good”, “moderate”, “bad” or “dangerous for health” [109].
The results suggest that data availability and access are essential for air quality indexes to be effective. These data are based on monitoring data provided by networks of government monitoring stations or other sources [110]. These indexes are essential for the evaluation and understanding of air pollution and its impact on human health [13]. Considering the variety of technical criteria, they provide an accurate measure of air quality and are valuable for the research and development of public health policies [106]. The accessibility of these data is relevant for their generation, updating and application in research and public health policies [111]. Lastly, they are essential to ensuring a healthy and sustainable environment for present and future generations [112].
Air pollution is a serious public health problem worldwide and has a great impact on the morbidity and mortality of the population. The most effective measures for reducing the impact of air pollution on the development of asthma and its burden of morbidity and mortality are those related to reducing emissions [46]. The expansion of public transport and the use of cleaner fuels in vehicles, industries and homes are feasible and necessary measures for reducing global warming and its direct effects on human health [113]. It is estimated that reducing emission levels to those recommended by the WHO can lead to an annual decrease of up to 60% in pollution-related deaths [114].
4. Conclusions
The findings of this study allowed us to draw the following conclusions.
The results show that the most frequently reported air pollutants related to asthma are PM (Q3) > NO2 (Q3) > O3 (Q3) > CO (Q3) > NO (Q3) > SO2 (Q3). These pollutants, generated mainly by the combustion of fossil fuels and vehicular traffic, are possibly associated with irritation of the respiratory tract and exacerbation of asthma symptoms. The findings suggest that this order of importance changes slightly when considering the use of AQIs in asthma studies: PM > NO2 > O3 > SO2 > CO > NO.
These findings suggest that climate variables and AQIs play relevant roles in asthma research. Temperature (Q4) was the most relevant climate variable, followed by atmospheric pressure (Q3), wind direction (Q3), solar radiation (Q3), precipitation (Q3) and wind speed (Q3). The influence of the concentration and dispersion of air pollutants and, therefore, the prevalence and severity of asthma are relevant to asthma research.
The results suggest a complex interaction between climate variables and air pollutants. Factors such as temperature and solar radiation can affect chemical reactions and pollutant formation, while the direction and speed of wind can influence pollutant dispersion. AQIs such as the U.S.EAPA-AQI and the AQHI are directly associated with air quality and the incidence, severity and exacerbation of asthma.
The findings suggest that climate change presents additional challenges in relation to asthma by influencing the environmental conditions that affect the disease. Phenomena such as heat waves, electrical storms and episodes of air pollution can trigger asthma exacerbations and increase the burden of the disease. Climate change can also influence the distribution and season of environmental allergens, as well as the formation of air pollutants, affecting the prevalence and severity of asthma.
Finally, these conclusions provide a comprehensive view of the relationships among AQIs, air pollutants and asthma and highlight the need for continued research in this field to develop public health policies and environmental regulations. Importantly, these findings should be interpreted in the context of the literature and the inherent limitations of observational studies. Indeed, more research is required to deepen our understanding of the mechanisms that link exposure to air pollution with asthma and to develop effective mitigation strategies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/atmos15070847/s1, Table S1: Spatiotemporal trends for air pollutants, climate variables and AQIs in asthma studies [115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154].
Funding
Ministerio de Ciencia, Tecnología e Innovación de Colombia, MinCiencias, research contract number: 120389784742, 645-2021.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors wish to thank Universidad Distrital Francisco José de Caldas (Colombia), Universidad Pontificia Javeriana (Colombia), Universidad Nacional de Colombia (Colombia) and Hospital Universitario San Ignacio (Colombia) for their support.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zhang, X.; Han, L.; Wei, H.; Tan, X.; Zhou, W.; Li, W.; Qian, Y. Linking Urbanization and Air Quality Together: A Review and a Perspective on the Future Sustainable Urban Development. J. Clean. Prod. 2022, 346, 130988. [Google Scholar] [CrossRef]
- Zafra, C.; Suárez, J.; Pachón, J.E. Public Health Considerations for PM10 in a High-Pollution Megacity: Influences of Atmospheric Condition and Land Coverage. Atmosphere 2021, 12, 118. [Google Scholar] [CrossRef]
- Desarkar, A.; Das, A. A Smart Air Pollution Analytics Framework. In Proceedings of the Information and Communication Technology; Mishra, D.K., Azar, A.T., Joshi, A., Eds.; Springer: Singapore, 2018; pp. 197–205. [Google Scholar]
- Saxena, P.; Sonwani, S. Criteria Air Pollutants and Their Impact on Environmental Health; Springer: Singapore, 2019; ISBN 9789811399916. [Google Scholar]
- Robichaud, A. An Overview of Selected Emerging Outdoor Airborne Pollutants and Air Quality Issues: The Need to Reduce Uncertainty about Environmental and Human Impacts. J. Air Waste Manag. Assoc. 2020, 70, 341–378. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Singh, S.; Mall, R.K. Chapter 17—Urban Ecology and Human Health: Implications of Urban Heat Island, Air Pollution and Climate Change Nexus. In Urban Ecology; Verma, P., Singh, P., Singh, R., Raghubanshi, A.S., Eds.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 317–334. ISBN 978-0-12-820730-7. [Google Scholar]
- GBD 2015 Chronic Respiratory Disease Collaborators. Global, Regional, and National Deaths, Prevalence, Disability-Adjusted Life Years, and Years Lived with Disability for Chronic Obstructive Pulmonary Disease and Asthma, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 2017, 5, 691–706. [Google Scholar] [CrossRef] [PubMed]
- Darçın, M. Association between Air Quality and Quality of Life. Environ. Sci. Pollut. Res. 2014, 21, 1954–1959. [Google Scholar] [CrossRef] [PubMed]
- Vanegas, S.; Trejos, E.M.; Aristizábal, B.H.; Pereira, G.M.; Hernández, J.M.; Murillo, J.H.; Ramírez, O.; Amato, F.; Silva, L.F.O.; Rojas, N.Y.; et al. Spatial Distribution and Chemical Composition of Road Dust in Two High-Altitude Latin American Cities. Atmosphere 2021, 12, 1109. [Google Scholar] [CrossRef]
- Jiang, W.; Wang, Y.; Tsou, M.-H.; Fu, X. Using Social Media to Detect Outdoor Air Pollution and Monitor Air Quality Index (AQI): A Geo-Targeted Spatiotemporal Analysis Framework with Sina Weibo (Chinese Twitter). PLoS ONE 2015, 10, e0141185. [Google Scholar] [CrossRef] [PubMed]
- Fino, A.; Vichi, F.; Leonardi, C.; Mukhopadhyay, K. An Overview of Experiences Made and Tools Used to Inform the Public on Ambient Air Quality. Atmosphere 2021, 12, 1524. [Google Scholar] [CrossRef]
- Wong, T.W.; Tam, W.W.S.; Yu, I.T.S.; Lau, A.K.H.; Pang, S.W.; Wong, A.H.S. Developing a Risk-Based Air Quality Health Index. Atmos. Environ. 2013, 76, 52–58. [Google Scholar] [CrossRef]
- Kumar, P. A Critical Evaluation of Air Quality Index Models (1960–2021). Environ. Monit. Assess 2022, 194, 324. [Google Scholar] [CrossRef]
- Tan, X.; Han, L.; Zhang, X.; Zhou, W.; Li, W.; Qian, Y. A Review of Current Air Quality Indexes and Improvements under the Multi-Contaminant Air Pollution Exposure. J. Environ. Manag. 2021, 279, 111681. [Google Scholar] [CrossRef] [PubMed]
- Adams, R.J.; Fuhlbrigge, A.L.; Finkelstein, J.A.; Weiss, S.T. Intranasal Steroids and the Risk of Emergency Department Visits for Asthma. J. Allergy Clin. Immunol. 2002, 109, 636–642. [Google Scholar] [CrossRef]
- McCloud, E.; Papoutsakis, C. A Medical Nutrition Therapy Primer for Childhood Asthma: Current and Emerging Perspectives. J. Am. Diet. Assoc. 2011, 111, 1052–1064. [Google Scholar] [CrossRef] [PubMed]
- Mauderly, J.L.; Burnett, R.T.; Castillejos, M.; Özkaynak, H.; Samet, J.M.; Stieb, D.M.; Vedal, S.; Wyzga, R.E. Is the Air Pollution Health Research Community Prepared to Support a Multipollutant Air Quality Management Framework? Inhal. Toxicol. 2010, 22, 1–19. [Google Scholar] [CrossRef]
- Honkoop, P.J.; Simpson, A.; Bonini, M.; Snoeck-Stroband, J.B.; Meah, S.; Chung, K.F.; Usmani, O.S.; Fowler, S.; Sont, J.K. MyAirCoach: The Use of Home-Monitoring and mHealth Systems to Predict Deterioration in Asthma Control and the Occurrence of Asthma Exacerbations; Study Protocol of an Observational Study. BMJ Open 2017, 7, e013935. [Google Scholar] [CrossRef]
- Rosser, F.J.; Rothenberger, S.D.; Han, Y.-Y.; Forno, E.; Celedón, J.C. Air Quality Index and Childhood Asthma: A Pilot Randomized Clinical Trial Intervention. Am. J. Prev. Med. 2023, 64, 893–897. [Google Scholar] [CrossRef]
- Chen, R.; Wang, X.; Meng, X.; Hua, J.; Zhou, Z.; Chen, B.; Kan, H. Communicating Air Pollution-Related Health Risks to the Public: An Application of the Air Quality Health Index in Shanghai, China. Environ. Int. 2013, 51, 168–173. [Google Scholar] [CrossRef]
- Weltgesundheitsorganisation; WHO. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021; ISBN 978-92-4-003422-8. [Google Scholar]
- Grigorieva, E.; Lukyanets, A. Combined Effect of Hot Weather and Outdoor Air Pollution on Respiratory Health: Literature Review. Atmosphere 2021, 12, 790. [Google Scholar] [CrossRef]
- Jiang, X.-Q.; Mei, X.-D.; Feng, D. Air Pollution and Chronic Airway Diseases: What Should People Know and Do? J. Thorac. Dis. 2016, 8, E31–E40. [Google Scholar] [CrossRef] [PubMed]
- Schraufnagel, D.E. The Health Effects of Ultrafine Particles. Exp. Mol. Med. 2020, 52, 311–317. [Google Scholar] [CrossRef]
- Plaia, A.; Ruggieri, M. Air Quality Indices: A Review. Rev. Environ. Sci. Biotechnol. 2011, 10, 165–179. [Google Scholar] [CrossRef]
- Kanchan; Gorai, A.K.; Goyal, P. A Review on Air Quality Indexing System. Asian J. Atmos. Environ. 2015, 9, 101–113. [Google Scholar] [CrossRef]
- Perlmutt, L.D.; Cromar, K.R. Comparing Associations of Respiratory Risk for the EPA Air Quality Index and Health-Based Air Quality Indices. Atmos. Environ. 2019, 202, 1–7. [Google Scholar] [CrossRef]
- Hime, N.J.; Marks, G.B.; Cowie, C.T. A Comparison of the Health Effects of Ambient Particulate Matter Air Pollution from Five Emission Sources. Int. J. Environ. Res. Public Health 2018, 15, 1206. [Google Scholar] [CrossRef] [PubMed]
- van Kamp, I.; Leidelmeijer, K.; Marsman, G.; de Hollander, A. Urban Environmental Quality and Human Well-Being: Towards a Conceptual Framework and Demarcation of Concepts; a Literature Study. Landsc. Urban. Plan. 2003, 65, 5–18. [Google Scholar] [CrossRef]
- Bell, M.L.; Cifuentes, L.A.; Davis, D.L.; Cushing, E.; Gusman Telles, A.; Gouveia, N. Environmental Health Indicators and a Case Study of Air Pollution in Latin American Cities. Environ. Res. 2011, 111, 57–66. [Google Scholar] [CrossRef]
- Cheng, W.-L.; Chen, Y.-S.; Zhang, J.; Lyons, T.J.; Pai, J.-L.; Chang, S.-H. Comparison of the Revised Air Quality Index with the PSI and AQI Indices. Sci. Total Environ. 2007, 382, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Sheng, N.; Tang, U.W. The First Official City Ranking by Air Quality in China—A Review and Analysis. Cities 2016, 51, 139–149. [Google Scholar] [CrossRef]
- Yao, J.; Stieb, D.M.; Taylor, E.; Henderson, S.B. Assessment of the Air Quality Health Index (AQHI) and Four Alternate AQHI-Plus Amendments for Wildfire Seasons in British Columbia. Can. J. Public Health 2020, 111, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Sinha, A.; Sengupta, T.; Alvarado, R. Interplay between Technological Innovation and Environmental Quality: Formulating the SDG Policies for next 11 Economies. J. Clean. Prod. 2020, 242, 118549. [Google Scholar] [CrossRef]
- Radisic, S.; Newbold, K.B. Factors Influencing Health Care and Service Providers’ and Their Respective “at Risk” Populations’ Adoption of the Air Quality Health Index (AQHI): A Qualitative Study. BMC Health Serv. Res. 2016, 16, 107. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Han, K.; Ran, Z.; Wang, X.; Wu, Q.; Zhan, N.; Yi, Z.; Jin, T. Traffic-Related Organic and Inorganic Air Pollution and Risk of Development of Childhood Asthma: A Meta-Analysis. Environ. Res. 2021, 194, 110493. [Google Scholar] [CrossRef] [PubMed]
- Shahriyari, H.A.; Nikmanesh, Y.; Jalali, S.; Tahery, N.; Zhiani Fard, A.; Hatamzadeh, N.; Zarea, K.; Cheraghi, M.; Mohammadi, M.J. Air Pollution and Human Health Risks: Mechanisms and Clinical Manifestations of Cardiovascular and Respiratory Diseases. Toxin Rev. 2022, 41, 606–617. [Google Scholar] [CrossRef]
- Nandan, A.; Siddiqui, N.A.; Singh, C.; Aeri, A. Occupational and Environmental Impacts of Indoor Air Pollutant for Different Occupancy: A Review. Toxicol. Environ. Health Sci. 2021, 13, 303–322. [Google Scholar] [CrossRef]
- Rodríguez-Santamaría, K.; Zafra-Mejía, C.A.; Rondón-Quintana, H.A. Macro-Morphological Traits of Leaves for Urban Tree Selection for Air Pollution Biomonitoring: A Review. Biosensors 2022, 12, 812. [Google Scholar] [CrossRef] [PubMed]
- Zafra, C.; Temprano, J.; Tejero, I. The Physical Factors Affecting Heavy Metals Accumulated in the Sediment Deposited on Road Surfaces in Dry Weather: A Review. Urban. Water J. 2017, 14, 639–649. [Google Scholar] [CrossRef]
- Vinasco, J.P.S.; Nastar, T.R.C. Variación Espacial y Temporal de Concentraciones de PM10 En El Área Urbana De Santiago De Cali, Colombia. Ing. Recur. Nat. Ambiente 2013, 12, 129–141. [Google Scholar]
- İnce, Ö.B.; Şevik, M.; Şener, R.; Türk, T. Spatiotemporal Analysis of Foot and Mouth Disease Outbreaks in Cattle and Small Ruminants in Türkiye between 2010 and 2019. Vet. Res. Commun. 2024, 48, 923–939. [Google Scholar] [CrossRef] [PubMed]
- Campo, E.; Ballester, J.; Langlois, J.; Dacremont, C.; Valentin, D. Comparison of Conventional Descriptive Analysis and a Citation Frequency-Based Descriptive Method for Odor Profiling: An Application to Burgundy Pinot Noir Wines. Food Qual. Prefer. 2010, 21, 44–55. [Google Scholar] [CrossRef]
- Ye, W.-F.; Ma, Z.-Y.; Ha, X.-Z.; Yang, H.-C.; Weng, Z.-X. Spatiotemporal Patterns and Spatial Clustering Characteristics of Air Quality in China: A City Level Analysis. Ecol. Indic. 2018, 91, 523–530. [Google Scholar] [CrossRef]
- El Haddad, C.; Gerbaka, N.-E.; Hallit, S.; Tabet, C. Association between Exposure to Ambient Air Pollution and Occurrence of Inflammatory Acne in the Adult Population. BMC Public Health 2021, 21, 1664. [Google Scholar] [CrossRef] [PubMed]
- Tiotiu, A.I.; Novakova, P.; Nedeva, D.; Chong-Neto, H.J.; Novakova, S.; Steiropoulos, P.; Kowal, K. Impact of Air Pollution on Asthma Outcomes. Int. J. Environ. Res. Public Health 2020, 17, 6212. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wei, Y.; Fang, Z. Ozone Pollution: A Major Health Hazard Worldwide. Front. Immunol. 2019, 10, 2518. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, N.; Carel, R.S.; Derazne, E.; Tiktinsky, A.; Tzur, D.; Portnov, B.A. Modeling Long-Term Effects Attributed to Nitrogen Dioxide (NO2) and Sulfur Dioxide (SO2) Exposure on Asthma Morbidity in a Nationwide Cohort in Israel. J. Toxicol. Environ. Health Part A 2017, 80, 326–337. [Google Scholar] [CrossRef]
- Liu, F.; Zhao, Y.; Liu, Y.-Q.; Liu, Y.; Sun, J.; Huang, M.-M.; Liu, Y.; Dong, G.-H. Asthma and Asthma Related Symptoms in 23,326 Chinese Children in Relation to Indoor and Outdoor Environmental Factors: The Seven Northeastern Cities (SNEC) Study. Sci. Total Environ. 2014, 497–498, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Chatkin, J.; Correa, L.; Santos, U. External Environmental Pollution as a Risk Factor for Asthma. Clin. Rev. Allerg. Immunol. 2022, 62, 72–89. [Google Scholar] [CrossRef]
- Khreis, H.; Kelly, C.; Tate, J.; Parslow, R.; Lucas, K.; Nieuwenhuijsen, M. Exposure to Traffic-Related Air Pollution and Risk of Development of Childhood Asthma: A Systematic Review and Meta-Analysis. Environ. Int. 2017, 100, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Kocot, K.; Barański, K.; Melaniuk-Wolny, E.; Zajusz-Zubek, E.; Kowalska, M. Exercise under Exposure to Air Pollution and Spirometry in Healthy Adults with and without Allergy. Atmosphere 2021, 12, 1168. [Google Scholar] [CrossRef]
- Hsiao, Y.-L.; Chen, Y.-S. Pricing the Haze Option with the PM2.5 Index. Asia Pac. Manag. Rev. 2019, 24, 27–36. [Google Scholar] [CrossRef]
- D’Amato, G.; Baena-Cagnani, C.E.; Cecchi, L.; Annesi-Maesano, I.; Nunes, C.; Ansotegui, I.; D’Amato, M.; Liccardi, G.; Sofia, M.; Canonica, W.G. Climate Change, Air Pollution and Extreme Events Leading to Increasing Prevalence of Allergic Respiratory Diseases. Multidiscip. Respir. Med. 2013, 8, 12. [Google Scholar] [CrossRef]
- American Lung Association. Urban Air Pollution and Health Inequities: A Workshop Report. Environ. Health Perspect. 2001, 109, 357–374. [Google Scholar] [CrossRef]
- Chanel, O.; Perez, L.; Künzli, N.; Medina, S.; Aphekom group. The Hidden Economic Burden of Air Pollution-Related Morbidity: Evidence from the Aphekom Project. Eur. J. Health Econ. 2016, 17, 1101–1115. [Google Scholar] [CrossRef]
- Lu, X.; Zhang, S.; Xing, J.; Wang, Y.; Chen, W.; Ding, D.; Wu, Y.; Wang, S.; Duan, L.; Hao, J. Progress of Air Pollution Control in China and Its Challenges and Opportunities in the Ecological Civilization Era. Engineering 2020, 6, 1423–1431. [Google Scholar] [CrossRef]
- Dockery, D.W.; Pope, C.A.; Xu, X.; Spengler, J.D.; Ware, J.H.; Fay, M.E.; Ferris, B.G.; Speizer, F.E. An Association between Air Pollution and Mortality in Six U.S. Cities. New Engl. J. Med. 1993, 329, 1753–1759. [Google Scholar] [CrossRef] [PubMed]
- Kaginalkar, A.; Kumar, S.; Gargava, P.; Niyogi, D. Stakeholder Analysis for Designing an Urban Air Quality Data Governance Ecosystem in Smart Cities. Urban. Clim. 2023, 48, 101403. [Google Scholar] [CrossRef]
- Laborde, A.; Tomasina, F.; Bianchi, F.; Bruné, M.-N.; Buka, I.; Comba, P.; Corra, L.; Cori, L.; Duffert, C.M.; Harari, R.; et al. Children’s Health in Latin America: The Influence of Environmental Exposures. Environ. Health Perspect. 2014, 123, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Molina, M.J.; Molina, L.T. Megacities and Atmospheric Pollution. J. Air Waste Manag. Assoc. 2004, 54, 644–680. [Google Scholar] [CrossRef] [PubMed]
- Jyethi, D.S. Air Quality: Global and Regional Emissions of Particulate Matter, SOx, and NOx. In Plant Responses to Air Pollution; Kulshrestha, U., Saxena, P., Eds.; Springer: Singapore, 2016; pp. 5–19. ISBN 978-981-10-1201-3. [Google Scholar]
- Levy, J.I.; Quirós-Alcalá, L.; Fabian, M.P.; Basra, K.; Hansel, N.N. Established and Emerging Environmental Contributors to Disparities in Asthma and Chronic Obstructive Pulmonary Disease. Curr. Epidemiol. Rep. 2018, 5, 114–124. [Google Scholar] [CrossRef]
- Gupta, V. Vehicle-Generated Heavy Metal Pollution in an Urban Environment and Its Distribution into Various Environmental Components. In Environmental Concerns and Sustainable Development: Volume 1: Air, Water and Energy Resources; Shukla, V., Kumar, N., Eds.; Springer: Singapore, 2020; pp. 113–127. ISBN 9789811358890. [Google Scholar]
- Kushta, J.; Georgiou, G.K.; Proestos, Y.; Christoudias, T.; Thunis, P.; Savvides, C.; Papadopoulos, C.; Lelieveld, J. Evaluation of EU Air Quality Standards through Modeling and the FAIRMODE Benchmarking Methodology. Air Qual. Atmos. Health 2019, 12, 73–86. [Google Scholar] [CrossRef]
- Pope, R.J.; Butt, E.W.; Chipperfield, M.P.; Doherty, R.M.; Fenech, S.; Schmidt, A.; Arnold, S.R.; Savage, N.H. The Impact of Synoptic Weather on UK Surface Ozone and Implications for Premature Mortality. Environ. Res. Lett. 2016, 11, 124004. [Google Scholar] [CrossRef]
- Brauer, M.; Freedman, G.; Frostad, J.; van Donkelaar, A.; Martin, R.V.; Dentener, F.; van Dingenen, R.; Estep, K.; Amini, H.; Apte, J.S.; et al. Ambient Air Pollution Exposure Estimation for the Global Burden of Disease 2013. Environ. Sci. Technol. 2016, 50, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, D. Distributional Effects of Environmental and Energy Policy; Routledge: London, UK, 2017; ISBN 978-1-351-94346-8. [Google Scholar]
- Landrigan, P.J.; Vicini, A. Ethical Challenges in Global Public Health: Climate Change, Pollution, and the Health of the Poor; Wipf and Stock Publishers: Eugene, OR, USA, 2021; ISBN 978-1-72529-174-4. [Google Scholar]
- Kelly, G.; Idubor, O.I.; Binney, S.; Schramm, P.J.; Mirabelli, M.C.; Hsu, J. The Impact of Climate Change on Asthma and Allergic-Immunologic Disease. Curr. Allergy Asthma Rep. 2023, 23, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.-J.; Zheng, X.-Y.; Chung, K.F.; Zhong, N.-S. Impact of Air Pollution on the Burden of Chronic Respiratory Diseases in China: Time for Urgent Action. Lancet 2016, 388, 1939–1951. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Pan, J.; Zhang, H.; Shi, C.; Li, G.; Peng, Z.; Ma, J.; Zhou, Y.; Zhang, L. Short-Term Exposure to Ambient Air Pollution and Asthma Mortality. Am. J. Respir. Crit. Care Med. 2019, 200, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Krieger, J.K.; Takaro, T.K.; Allen, C.; Song, L.; Weaver, M.; Chai, S.; Dickey, P. The Seattle-King County Healthy Homes Project: Implementation of a Comprehensive Approach to Improving Indoor Environmental Quality for Low-Income Children with Asthma. Environ. Health Perspect. 2002, 110, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Pfeffer, P.E.; Mudway, I.S.; Grigg, J. Air Pollution and Asthma: Mechanisms of Harm and Considerations for Clinical Interventions. Chest 2021, 159, 1346–1355. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, A.S.; Ramondt, S.; Bogart, K.V.; Perez-Zuniga, R. Public Awareness of Air Pollution and Health Threats: Challenges and Opportunities for Communication Strategies To Improve Environmental Health Literacy. J. Health Commun. 2019, 24, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Abramson, M.J.; Koplin, J.; Hoy, R.; Dharmage, S.C. Population-Wide Preventive Interventions for Reducing the Burden of Chronic Respiratory Disease. Int. J. Tuberc. Lung Dis. 2015, 19, 1007–1018. [Google Scholar] [CrossRef] [PubMed]
- Altzibar, J.M.; Tamayo-Uria, I.; De Castro, V.; Aginagalde, X.; Albizu, M.V.; Lertxundi, A.; Benito, J.; Busca, P.; Antepara, I.; Landa, J.; et al. Epidemiology of Asthma Exacerbations and Their Relation with Environmental Factors in the Basque Country. Clin. Exp. Allergy 2015, 45, 1099–1108. [Google Scholar] [CrossRef]
- Han, A.; Deng, S.; Yu, J.; Zhang, Y.; Jalaludin, B.; Huang, C. Asthma Triggered by Extreme Temperatures: From Epidemiological Evidence to Biological Plausibility. Environ. Res. 2023, 216, 114489. [Google Scholar] [CrossRef]
- Wolkoff, P. Indoor Air Humidity, Air Quality, and Health—An Overview. Int. J. Hyg. Environ. Health 2018, 221, 376–390. [Google Scholar] [CrossRef]
- Oh, J.W. Climate Change and Allergy, An Issue of Immunology and Allergy Clinics of North America; Elsevier Health Sciences: Amsterdam, The Netherlands, 2020; ISBN 978-0-323-79386-5. [Google Scholar]
- D’Amato, G.; Chong-Neto, H.J.; Monge Ortega, O.P.; Vitale, C.; Ansotegui, I.; Rosario, N.; Haahtela, T.; Galan, C.; Pawankar, R.; Murrieta-Aguttes, M.; et al. The Effects of Climate Change on Respiratory Allergy and Asthma Induced by Pollen and Mold Allergens. Allergy 2020, 75, 2219–2228. [Google Scholar] [CrossRef]
- D’Amato, G.; Liccardi, G.; D’Amato, M.; Holgate, S. Environmental Risk Factors and Allergic Bronchial Asthma. Clin. Exp. Allergy 2005, 35, 1113–1124. [Google Scholar] [CrossRef]
- Ayres-Sampaio, D.; Teodoro, A.C.; Sillero, N.; Santos, C.; Fonseca, J.; Freitas, A. An Investigation of the Environmental Determinants of Asthma Hospitalizations: An Applied Spatial Approach. Appl. Geogr. 2014, 47, 10–19. [Google Scholar] [CrossRef]
- D’Amato, G.; Holgate, S.T.; Pawankar, R.; Ledford, D.K.; Cecchi, L.; Al-Ahmad, M.; Al-Enezi, F.; Al-Muhsen, S.; Ansotegui, I.; Baena-Cagnani, C.E.; et al. Meteorological Conditions, Climate Change, New Emerging Factors, and Asthma and Related Allergic Disorders. A Statement of the World Allergy Organization. World Allergy Organ. J. 2015, 8, 1–52. [Google Scholar] [CrossRef]
- Cecchi, L.; D’Amato, G.; Ayres, J.G.; Galan, C.; Forastiere, F.; Forsberg, B.; Gerritsen, J.; Nunes, C.; Behrendt, H.; Akdis, C.; et al. Projections of the Effects of Climate Change on Allergic Asthma: The Contribution of Aerobiology. Allergy 2010, 65, 1073–1081. [Google Scholar] [CrossRef]
- Eguiluz-Gracia, I.; Mathioudakis, A.G.; Bartel, S.; Vijverberg, S.J.H.; Fuertes, E.; Comberiati, P.; Cai, Y.S.; Tomazic, P.V.; Diamant, Z.; Vestbo, J.; et al. The Need for Clean Air: The Way Air Pollution and Climate Change Affect Allergic Rhinitis and Asthma. Allergy 2020, 75, 2170–2184. [Google Scholar] [CrossRef]
- D’Amato, G.; Vitale, C.; De Martino, A.; Viegi, G.; Lanza, M.; Molino, A.; Sanduzzi, A.; Vatrella, A.; Annesi-Maesano, I.; D’Amato, M. Effects on Asthma and Respiratory Allergy of Climate Change and Air Pollution. Multidiscip. Respir. Med. 2015, 10, 39. [Google Scholar] [CrossRef]
- Hales, S.; Lewis, S.; Slater, T.; Crane, J.; Pearce, N. Prevalence of Adult Asthma Symptoms in Relation to Climate in New Zealand. Environ. Health Perspect. 1998, 106, 607–610. [Google Scholar] [CrossRef]
- Murrison, L.B.; Brandt, E.B.; Myers, J.B.; Hershey, G.K.K. Environmental Exposures and Mechanisms in Allergy and Asthma Development. J. Clin. Investig. 2019, 129, 1504–1515. [Google Scholar] [CrossRef] [PubMed]
- Dharmage, S.C.; Perret, J.L.; Custovic, A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019, 7, 246. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Kwok, K.C.S.; Liu, X.P.; Zhang, Y. Air Pollutant Dispersion around High-Rise Buildings under Different Angles of Wind Incidence. J. Wind. Eng. Ind. Aerodyn. 2017, 167, 51–61. [Google Scholar] [CrossRef]
- Khodakarami, J.; Ghobadi, P. Urban Pollution and Solar Radiation Impacts. Renew. Sustain. Energy Rev. 2016, 57, 965–976. [Google Scholar] [CrossRef]
- Olstrup, H.; Johansson, C.; Forsberg, B.; Tornevi, A.; Ekebom, A.; Meister, K. A Multi-Pollutant Air Quality Health Index (AQHI) Based on Short-Term Respiratory Effects in Stockholm, Sweden. Int. J. Environ. Res. Public Health 2019, 16, 105. [Google Scholar] [CrossRef] [PubMed]
- Govender, P.; Sivakumar, V. Application of k-Means and Hierarchical Clustering Techniques for Analysis of Air Pollution: A Review (1980–2019). Atmos. Pollut. Res. 2020, 11, 40–56. [Google Scholar] [CrossRef]
- Deng, S.-Z.; Jalaludin, B.B.; Antó, J.M.; Hess, J.J.; Huang, C.-R. Climate Change, Air Pollution, and Allergic Respiratory Diseases: A Call to Action for Health Professionals. Chin. Med. J. 2020, 133, 1552. [Google Scholar] [CrossRef] [PubMed]
- Demain, J.G. Climate Change and the Impact on Respiratory and Allergic Disease: 2018. Curr. Allergy Asthma Rep. 2018, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- D ’Amato, M.; Cecchi, L.; Annesi-Maesano, I.; d’Amato, G. News on Climate Change, Air Pollution, and Allergic Triggers of Asthma. J. Investig. Allergol. Clin. Immunol. 2018, 28, 91. [Google Scholar] [CrossRef] [PubMed]
- Mirsaeidi, M.; Motahari, H.; Taghizadeh Khamesi, M.; Sharifi, A.; Campos, M.; Schraufnagel, D.E. Climate Change and Respiratory Infections. Ann. ATS 2016, 13, 1223–1230. [Google Scholar] [CrossRef]
- Delpla, I.; Diallo, T.A.; Keeling, M.; Bellefleur, O. Tools and Methods to Include Health in Climate Change Adaptation and Mitigation Strategies and Policies: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 2547. [Google Scholar] [CrossRef]
- Eisenman, T.S.; Churkina, G.; Jariwala, S.P.; Kumar, P.; Lovasi, G.S.; Pataki, D.E.; Weinberger, K.R.; Whitlow, T.H. Urban Trees, Air Quality, and Asthma: An Interdisciplinary Review. Landsc. Urban. Plan. 2019, 187, 47–59. [Google Scholar] [CrossRef]
- Pala, D.; Pagán, J.; Parimbelli, E.; Rocca, M.T.; Bellazzi, R.; Casella, V. Spatial Enablement to Support Environmental, Demographic, Socioeconomics, and Health Data Integration and Analysis for Big Cities: A Case Study With Asthma Hospitalizations in New York City. Front. Med. 2019, 6, 84. [Google Scholar] [CrossRef]
- Liang, L.; Gong, P. Urban and Air Pollution: A Multi-City Study of Long-Term Effects of Urban Landscape Patterns on Air Quality Trends. Sci. Rep. 2020, 10, 18618. [Google Scholar] [CrossRef] [PubMed]
- Lai, Y.; Kontokosta, C.E. The Impact of Urban Street Tree Species on Air Quality and Respiratory Illness: A Spatial Analysis of Large-Scale, High-Resolution Urban Data. Health Place 2019, 56, 80–87. [Google Scholar] [CrossRef]
- Wallace, J.; Corr, D.; Kanaroglou, P. Topographic and Spatial Impacts of Temperature Inversions on Air Quality Using Mobile Air Pollution Surveys. Sci. Total Environ. 2010, 408, 5086–5096. [Google Scholar] [CrossRef] [PubMed]
- To, T.; Shen, S.; Atenafu, E.G.; Guan, J.; McLimont, S.; Stocks, B.; Licskai, C. The Air Quality Health Index and Asthma Morbidity: A Population-Based Study. Environ. Health Perspect. 2013, 121, 46–52. [Google Scholar] [CrossRef]
- Sokhi, R.S.; Moussiopoulos, N.; Baklanov, A.; Bartzis, J.; Coll, I.; Finardi, S.; Friedrich, R.; Geels, C.; Grönholm, T.; Halenka, T.; et al. Advances in Air Quality Research—Current and Emerging Challenges. Atmos. Chem. Phys. 2022, 22, 4615–4703. [Google Scholar] [CrossRef]
- Xiao, K.; Wang, Y.; Wu, G.; Fu, B.; Zhu, Y. Spatiotemporal Characteristics of Air Pollutants (PM10, PM2.5, SO2, NO2, O3, and CO) in the Inland Basin City of Chengdu, Southwest China. Atmosphere 2018, 9, 74. [Google Scholar] [CrossRef]
- Bălă, G.-P.; Râjnoveanu, R.-M.; Tudorache, E.; Motișan, R.; Oancea, C. Air Pollution Exposure—The (in)Visible Risk Factor for Respiratory Diseases. Environ. Sci. Pollut. Res. 2021, 28, 19615–19628. [Google Scholar] [CrossRef] [PubMed]
- Ośródka, L.; Kowalska, M.; Zejda, J.E.; Krajny, E.; Klejnowski, K.; Wojtylak, M. Air Quality Index and Its Significance in Environmental Health Risk Communication. Arch. Environ. Prot. 2009, 35, 13–21. [Google Scholar]
- Mak, H.W.L.; Lam, Y.F. Comparative Assessments and Insights of Data Openness of 50 Smart Cities in Air Quality Aspects. Sustain. Cities Soc. 2021, 69, 102868. [Google Scholar] [CrossRef]
- Messer, L.C.; Jagai, J.S.; Rappazzo, K.M.; Lobdell, D.T. Construction of an Environmental Quality Index for Public Health Research. Environ. Health 2014, 13, 39. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, R.; Kaur, H.; Alankar, B. Air Quality Forecast Using Convolutional Neural Network for Sustainable Development in Urban Environments. Sustain. Cities Soc. 2021, 75, 103239. [Google Scholar] [CrossRef]
- Shaheen, S.A.; Lipman, T.E. Reducing Greenhouse Emissions and Fuel Consumption: Sustainable Approaches for Surface Transportation. IATSS Res. 2007, 31, 6–20. [Google Scholar] [CrossRef]
- de Paula Santos, U.; Arbex, M.A.; Braga, A.L.F.; Mizutani, R.F.; Cançado, J.E.D.; Terra-Filho, M.; Chatkin, J.M. Environmental Air Pollution: Respiratory Effects. J. Bras. Pneumol. 2021, 47, e20200267. [Google Scholar] [CrossRef] [PubMed]
- Cook, Q.; Argenio, K.; Lovinsky-Desir, S. The Impact of Environmental Injustice and Social Determinants of Health on the Role of Air Pollution in Asthma and Allergic Disease in the United States. J. Allergy Clin. Immunol. 2021, 148, 1089–1101.e5. [Google Scholar] [CrossRef] [PubMed]
- Razavi-Termeh, S.V.; Sadeghi-Niaraki, A.; Choi, S.-M. Effects of Air Pollution in Spatio-Temporal Modeling of Asthma-Prone Areas Using a Machine Learning Model. Environ. Res. 2021, 200, 111344. [Google Scholar] [CrossRef] [PubMed]
- Pierangeli, I.; Nieuwenhuijsen, M.J.; Cirach, M.; Rojas-Rueda, D. Health Equity and Burden of Childhood Asthma—Related to Air Pollution in Barcelona. Environ. Res. 2020, 186, 109067. [Google Scholar] [CrossRef] [PubMed]
- Nordeide Kuiper, I.; Svanes, C.; Markevych, I.; Accordini, S.; Bertelsen, R.J.; Bråbäck, L.; Heile Christensen, J.; Forsberg, B.; Halvorsen, T.; Heinrich, J.; et al. Lifelong Exposure to Air Pollution and Greenness in Relation to Asthma, Rhinitis and Lung Function in Adulthood. Environ. Int. 2021, 146, 106219. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.-J.; Chen, C.-H.; Chen, B.-Y.; Chin, W.-S.; Guo, Y.L. Ambient Air Pollution and Asthma Onset in Taiwanese Adults. Respir. Med. 2020, 172, 106133. [Google Scholar] [CrossRef]
- Lau, N.; Smith, M.J.; Sarkar, A.; Gao, Z. Effects of Low Exposure to Traffic Related Air Pollution on Childhood Asthma Onset by Age 10 Years. Environ. Res. 2020, 191, 110174. [Google Scholar] [CrossRef] [PubMed]
- Squalli Houssaini, A.S.; Messaouri, H.; Nasri, I.; Roth, M.P.; Nejjari, C.; Benchekroun, M.N. Air Pollution as a Determinant of Asthma among Schoolchildren in Mohammedia, Morocco. Int. J. Environ. Health Res. 2007, 17, 243–257. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Xu, X.; Thompson, L.A.; Gross, H.E.; Shenkman, E.A.; DeWalt, D.A.; Huang, I.-C. Longitudinal Effect of Ambient Air Pollution and Pollen Exposure on Asthma Control: The Patient-Reported Outcomes Measurement Information System (PROMIS) Pediatric Asthma Study. Acad. Pediatr. 2019, 19, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Li, V.O.K.; Lam, J.C.K.; Han, Y.; Chow, K. A Big Data and Artificial Intelligence Framework for Smart and Personalized Air Pollution Monitoring and Health Management in Hong Kong. Environ. Sci. Policy 2021, 124, 441–450. [Google Scholar] [CrossRef]
- Li, Z.; Liang, D.; Ye, D.; Chang, H.H.; Ziegler, T.R.; Jones, D.P.; Ebelt, S.T. Application of High-Resolution Metabolomics to Identify Biological Pathways Perturbed by Traffic-Related Air Pollution. Environ. Res. 2021, 193, 110506. [Google Scholar] [CrossRef] [PubMed]
- Bahadoran, M.; Mortazavi, S.N.; Hajizadeh, Y. Evaluation of Anticipated Performance Index, Biochemical, and Physiological Parameters of Cupressus Arizonica Greene and Juniperus Excelsa Bieb for Greenbelt Development and Biomonitoring of Air Pollution. Int. J. Phytoremediation 2019, 21, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Kaya, İ.; Kahraman, C. Air Pollution Control Using Fuzzy Process Capability Indices in the Six-Sigma Approach. Hum. Ecol. Risk Assess. Int. J. 2009, 15, 689–713. [Google Scholar] [CrossRef]
- Yamazaki, S.; Shima, M.; Yoda, Y.; Oka, K.; Kurosaka, F.; Shimizu, S.; Takahashi, H.; Nakatani, Y.; Nishikawa, J.; Fujiwara, K.; et al. Association between PM2.5 and Primary Care Visits Due to Asthma Attack in Japan: Relation to Beijing’s Air Pollution Episode in January 2013. Environ. Health Prev. Med. 2014, 19, 172–176. [Google Scholar] [CrossRef]
- Kelly, F.J.; Mudway, I.S.; Fussell, J.C. Air Pollution and Asthma: Critical Targets for Effective Action. Pulm. Ther. 2021, 7, 9–24. [Google Scholar] [CrossRef]
- Karakatsani, A.; Analitis, A.; Perifanou, D.; Ayres, J.G.; Harrison, R.M.; Kotronarou, A.; Kavouras, I.G.; Pekkanen, J.; Hämeri, K.; Kos, G.P.; et al. Particulate Matter Air Pollution and Respiratory Symptoms in Individuals Having Either Asthma or Chronic Obstructive Pulmonary Disease: A European Multicentre Panel Study. Environ. Health 2012, 11, 75. [Google Scholar] [CrossRef]
- Reddy, K.R.B.K.; Gupta, N.; Bhattacharya, B.G.; Deka, N.M.; Chandane, P.; Kapoor, R.; Gupta, S.; Nagarajan, S.A.; Basavaraja, G.V.; Parekh, B.J. Impact of Air Pollution on Allergic Rhinitis and Asthma: Consensus Statement by Indian Academy of Pediatrics. Indian. Pediatr. 2021, 58, 765–770. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.-W.; Chen, S.-C.; Tu, H.-P.; Wang, C.-W.; Hung, C.-H.; Chen, H.-C.; Kuo, T.-Y.; Wang, C.-F.; Lai, B.-C.; Chen, P.-S.; et al. The Impact of the Synergistic Effect of Temperature and Air Pollutants on Chronic Lung Diseases in Subtropical Taiwan. J. Pers. Med. 2021, 11, 819. [Google Scholar] [CrossRef]
- Zhang, S.; He, Y.; Liang, H.; Gao, J.; Li, Y.; Li, Y.; Wang, L.; Xie, X.; Sun, M.; Yuan, C.; et al. Higher Environmental Composite Quality Index Score and Risk of Asthma and Allergy in Northeast China. Allergy 2021, 76, 1875–1879. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.; Wang, X.; Yi, W.; Wei, Q.; Gao, J.; Xu, Z.; Duan, J.; He, Y.; Tang, C.; Liu, X.; et al. Interactions between Climate Factors and Air Quality Index for Improved Childhood Asthma Self-Management. Sci. Total Environ. 2020, 723, 137804. [Google Scholar] [CrossRef] [PubMed]
- Mirabelli, M.C.; Ebelt, S.; Damon, S.A. Air Quality Index and Air Quality Awareness among Adults in the United States. Environ. Res. 2020, 183, 109185. [Google Scholar] [CrossRef] [PubMed]
- Olstrup, H.; Johansson, C.; Forsberg, B.; Åström, C. Association between Mortality and Short-Term Exposure to Particles, Ozone and Nitrogen Dioxide in Stockholm, Sweden. Int. J. Environ. Res. Public Health 2019, 16, 1028. [Google Scholar] [CrossRef] [PubMed]
- Mason, T.G.; Schooling, C.M.; Chan, K.P.; Tian, L. An Evaluation of the Air Quality Health Index Program on Respiratory Diseases in Hong Kong: An Interrupted Time Series Analysis. Atmos. Environ. 2019, 211, 151–158. [Google Scholar] [CrossRef]
- Kim, H.; Park, Y.; Park, K.; Yoo, B. Association between Pollen Risk Indexes, Air Pollutants, and Allergic Diseases in Korea. Osong Public Health Res. Perspect. 2016, 7, 172–179. [Google Scholar] [CrossRef]
- Carreiro-Martins, P.; Papoila, A.L.; Caires, I.; Azevedo, S.; Cano, M.M.; Virella, D.; Leiria-Pinto, P.; Teixeira, J.P.; Rosado-Pinto, J.; Annesi-Maesano, I.; et al. Effect of Indoor Air Quality of Day Care Centers in Children with Different Predisposition for Asthma. Pediatr. Allergy Immunol. 2016, 27, 299–306. [Google Scholar] [CrossRef]
- Spurr, K.; Pendergast, N.; MacDonald, S. Assessing the Use of the Air Quality Health Index by Vulnerable Populations in a ‘Low-Risk’ Region: A Pilot Study. Can. J. Respir. Ther. 2014, 50, 45–49. [Google Scholar]
- Belanger, K.; Holford, T.R.; Gent, J.F.; Hill, M.E.; Kezik, J.M.; Leaderer, B.P. Household Levels of Nitrogen Dioxide and Pediatric Asthma Severity. Epidemiology 2013, 24, 320. [Google Scholar] [CrossRef] [PubMed]
- Abelsohn, A.; Stieb, D.M. Health Effects of Outdoor Air Pollution: Approach to Counseling Patients Using the Air Quality Health Index. Can. Fam. Physician 2011, 57, 881–887. [Google Scholar] [PubMed]
- Sicard, P.; Lesne, O.; Alexandre, N.; Mangin, A.; Collomp, R. Air Quality Trends and Potential Health Effects—Development of an Aggregate Risk Index. Atmos. Environ. 2011, 45, 1145–1153. [Google Scholar] [CrossRef]
- Anwar, M.N.; Shabbir, M.; Tahir, E.; Iftikhar, M.; Saif, H.; Tahir, A.; Murtaza, M.A.; Khokhar, M.F.; Rehan, M.; Aghbashlo, M.; et al. Emerging Challenges of Air Pollution and Particulate Matter in China, India, and Pakistan and Mitigating Solutions. J. Hazard. Mater. 2021, 416, 125851. [Google Scholar] [CrossRef]
- Zeng, Q.; Fan, L.; Ni, Y.; Li, G.; Gu, Q. Construction of AQHI Based on the Exposure Relationship between Air Pollution and YLL in Northern China. Sci. Total Environ. 2020, 710, 136264. [Google Scholar] [CrossRef]
- Das, N.; Sutradhar, S.; Ghosh, R.; Mondal, P. Asymmetric Nexus between Air Quality Index and Nationwide Lockdown for COVID-19 Pandemic in a Part of Kolkata Metropolitan, India. Urban. Clim. 2021, 36, 100789. [Google Scholar] [CrossRef] [PubMed]
- Fu, G.Q.; Jiang, Y.F.; Liu, L.P.; Liu, H.Y.; Zhou, J.; Cui, X.W.; Wang, S.G. Effects of PM2.5 Exposure in Different Air Quality Grades on Daily Outpatient Visits for Childhood Asthma in Shijiazhuang, China. Biomed. Environ. Sci. 2018, 31, 888–892. [Google Scholar] [CrossRef]
- Janarthanan, R.; Partheeban, P.; Somasundaram, K.; Navin Elamparithi, P. A Deep Learning Approach for Prediction of Air Quality Index in a Metropolitan City. Sustain. Cities Soc. 2021, 67, 102720. [Google Scholar] [CrossRef]
- Suman Air Quality Indices: A Review of Methods to Interpret Air Quality Status. Mater. Today Proc. 2021, 34, 863–868. [CrossRef]
- Park, Y.; Koo, J.H.; Jeong, H.; Jung, J.Y.; Kim, C.; Kang, D.R. Evaluation of an Air Quality Warning System for Vulnerable and Susceptible Individuals in Korea: An Interrupted Time Series Analysis. Epidemiol. Health 2023, 45, e2023020. [Google Scholar] [CrossRef]
- Zhu, S.; Lian, X.; Liu, H.; Hu, J.; Wang, Y.; Che, J. Daily Air Quality Index Forecasting with Hybrid Models: A Case in China. Environ. Pollut. 2017, 231, 1232–1244. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Zhou, H.; Bai, L.; Zhou, P. Does Foreign Direct Investment Drive Environmental Degradation in China? An Empirical Study Based on Air Quality Index from a Spatial Perspective. J. Clean. Prod. 2018, 176, 864–872. [Google Scholar] [CrossRef]
- Hirabayashi, S.; Nowak, D.J. Comprehensive National Database of Tree Effects on Air Quality and Human Health in the United States. Environ. Pollut. 2016, 215, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xiao, J.; Lin, H.; Liu, T.; Qian, Z.; Zeng, W.; Guo, L.; Ma, W. The Construction and Validity Analysis of AQHI Based on Mortality Risk: A Case Study in Guangzhou, China. Environ. Pollut. 2017, 220, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Baklanov, A.; Molina, L.T.; Gauss, M. Megacities, Air Quality and Climate. Atmos. Environ. 2016, 126, 235–249. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).