Abstract
Leukemia is the most common childhood cancer and its etiology could be related to various environmental contaminants such as particulate matter (PM). The objective of our study is to evaluate the potential association between exposure to PM during pregnancy and the incidence of childhood leukemia. We established a population-based nationwide cohort using the Spanish Birth Registry Statistics database of the National Statistics Institute. We used spatiotemporal land use random forest models to estimate the concentrations of PM10 and PM2.5 for the entire pregnancy and by trimesters. We conducted logistic regression analyses adjusted for various covariates. In addition, we fitted generalized additive models (GAMs) to estimate the non-linear relationship between PM levels and leukemia incidence. The study included 3,112,123 children and 1066 cases of leukemia. The results for the continuous variable of PM10 exposure levels suggested an increased risk of childhood leukemia to be associated with higher exposure. The results for the categorized PM10 variable suggest an increased risk of childhood leukemia among pregnant women whose exposure levels were higher than the median (third and fourth quartiles). The results for PM2.5 were weaker. We found association between exposure to PM10 during pregnancy and an increased risk of childhood leukemia. Our findings indicate that public health interventions should aim to reduce air pollution to lower the incidence of childhood leukemia.
Keywords:
PM10; PM2.5; environmental factors; childhood cancer; childhood leukemia; incidence; epidemiology 1. Introduction
In Spain, the annual childhood cancer incidence is 155.5 cases per million for children aged 0–14 years old. Among childhood cancer, leukemia is the most common childhood cancer type, representing approximately one-third of all cancer cases in children aged 0–14 years [1], with an incidence rate in both sexes of 4.8 cases per 100,000 in children (0–14 years old) and 2.9 cases per 100,000 in adolescents (15–19 years old) [2,3]. These rates are similar to other western European countries [4].
The etiology of childhood leukemia is unknown in approximately 90% of cases [5]. The majority of these cases with unknown etiology could be due to a multifactorial etiology in which complex genetic–environmental mechanisms interact [6]. Risk factors described for childhood leukemia include age, gender, race/ethnicity, prenatal exposure to X-rays, exposure to radiation or chemotherapeutic agents, and some genetic syndromes [6,7]. Other potential risk factors include exposure to benzene and polycyclic aromatic hydrocarbons, as well as other traffic emission components [6,8,9]. The role of socioeconomic status as a risk factor for childhood leukemia is controversial, with some authors suggesting it as a possible confounding factor in future epidemiological studies [6]. The role of parental smoking is also controversial; results from an international consortium suggested an association with childhood AML, and a meta-analysis also suggested an association with ALL, but both studies showed an association with paternal smoking but not with maternal [10,11].
For years, growing urban and industrial development has increased economic activity and, in turn, raised pollution levels in cities [12]. There is increasing evidence pointing to the risks associated with living near polluted city air [13,14]. Consequently, air pollution, with PM as the main component, is a global public health problem. Airborne particulate matter (PM) is not a single pollutant, but rather a mixture of many chemical species. It is a complex mixture of solids and aerosols composed of small liquid droplets, dry solid fragments, and solid cores with liquid coatings [15]. Most of these chemical species are products of traffic emissions resulting from motor vehicle combustion. PM can be classified based on size into PM2.5, if it has aerodynamic diameters equal to or less than 2.5 μm, and PM10, if it has aerodynamic diameters equal to or less than 10 μm. PM2.5 is considered more toxic than PM10 because the smaller diameter of PM2.5 allows it to enter the respiratory system [16]. Prenatal exposure to PM is biologically plausible since PM can cross the placenta and circulate through fetal blood and organs [17,18], potentially causing health problems during pregnancy (such as low birth weight, intrauterine growth retardation, and/or premature birth [19,20,21]) or the later development of other conditions such as respiratory, immune, cardiometabolic, or neurodevelopmental [22]. In addition, among PM microscopic particles, it is possible to find benzene and polycyclic aromatic hydrocarbons (PAHs), which are listed as carcinogenic by the International Agency for Research on Cancer (IARC) [23]. For instance, benzene has been linked to an increased risk of leukemia in adults that are occupationally exposed to it and to acute lymphoblastic leukemia (ALL) in their offspring [24]. And some epidemiological studies have shown an increased risk of childhood cancer related to traffic exposure [25,26,27].
Focusing on PM, the International Agency for Research on Cancer (IARC) classified PM as a Group 1 carcinogen, posing a greater risk of lung cancer [28]. Despite this classification as an environmental carcinogen, few studies have evaluated the relationship between PM exposure and childhood cancer. In a systematic review by Filippini et al. in 2019 [29], which included 29 case–control and cohort studies reporting an association between air pollution and childhood leukemia, only four of them studied the association between PM exposure and childhood leukemia, and one of them found a statistically significant association between maternal exposure during pregnancy to PM2.5 and astrocytoma [30]. As observed, the existing literature on the relationship between environmental exposure and childhood cancer is scarce and inconclusive, and study results are diverse, partly due to variations in measuring PM exposure and the use of different exposure times [31].
This study aims to examine the possible relationship between exposure to PM during pregnancy and the increased risk of childhood leukemia. In addition, we aim to identify critical windows of susceptibility to PM exposure across the three trimesters of the pregnancy.
2. Methods
2.1. Study Design
We set up a population-based, nation-wide cohort using the Spanish Birth Registry Statistics database of the National Statistics Institute. Population data for the entire at-risk population were obtained from the birth registry of the Spanish Statistical Office (INE), resulting in information for a total of 5,307,443 children for the period from 2004 to 2016 [32]. We studied the population of 14 autonomous communities in Spain, as follows: Andalusia, Asturias, Aragon, Cantabria, Castilla-La Mancha, Catalonia, the Valencian Community, Extremadura, Galicia, La Rioja, Madrid, Murcia, Navarre, the Basque Country, and the Balearic Islands. All children born in the selected regions within the studied period and with available residential data were entered in the study, totaling 3,112,123 children. The autonomous community of Castilla y León and four provinces of Andalusia (Córdoba, Seville, Cádiz, and Huelva) were not included in the study, because we did not have a completed register of all leukemia cases for these regions. And the Canary Islands, Ceuta, and Melilla were excluded because we did not have exposure measurements.
The cases were patients with a diagnostic of childhood leukemia that is classified as Group I of the third edition of the ‘‘International Classification of Childhood Cancer’’ (ICCC-3): ALL, Acute myeloid leukemia (AML), chronic myeloproliferative diseases, myelodysplastic syndrome and other myeloproliferative syndromes, and unspecified and other-specified leukemia [33]. For the studied period 2004–2016, there were 2414 entries of leukemia cases in children (0–14 years old) in the Spanish Registry of Childhood Tumours (RETI-SEHOP). RETI-SEHOP is the cancer registry for the hospital pediatric onco-hematology units in Spain and it collaborates with the regional registries [34]. However, for our study, we just included 1066 leukemia cases corresponding to those children in the studied regions with the same home addresses at birth and at diagnosis time to allow us to match with the exposure during pregnancy measurement. Furthermore, due to the availability of PM2.5 estimations, for this pollutant the studied period was 2009–2016 with 536 cases and 1,923,581 controls.
2.2. Residence-Based Information
For the cases, the geographical coordinates were obtained from the postal addresses at the time of the diagnosis, which are included in the RETI-SEHOP database. This methodology was presented in another study, in which a spatial analysis of childhood cancer was performed, and we replicated it for this work [35]. The coordinates of the reference population were provided by the INE, which collects the mother’s address at the birth of the child. For the anonymization of personal data, these coordinates were altered by introducing a random error of 30 m.
2.3. Air Pollution Concentration Measures
We used spatiotemporal land use random forest models to estimate the concentrations of PM10 and PM2.5 for all Spanish territories except the Canary Islands, Ceuta, and Melilla. We estimated PM10 for the period 2004–2016 and PM2.5 for 2009–2016, because, in Spain, PM10 network monitoring was set up in 2004 and PM2.5 in 2009. These models linked ground-level air pollution and satellite-based measures of aerosol optical depth, land-use, meteorological, and traffic variables to estimate PM over 1 km × 1 km grid cells, and they were used previously in studies in Italy, Sweden, and Spain [36,37,38]—a full description of the methodology can be found in the paper of Stafoggia et al. [36]. Daily estimation of PM10 and PM2.5 concentrations was performed for each day of the entire pregnancy period (from conception until birth) at the maternal address at the time of the child’s delivery. We assumed that women did not change their residence during pregnancy. Daily PM exposure concentrations were used to calculate pregnancy-average exposure levels and trimester-average exposure concentrations across pregnancy. For the analysis, PM10 and PM2.5 concentrations were used as continuous and categorized variables. The continuous variables were defined using the estimated concentrations in μg/m3 units. For the categorized variables, we computed the quartiles of the continuous variables in the control population, in which quintile 1 (Q1) represented the lowest level and was defined as the reference group.
2.4. Potential Confounding Variables
As potential confounding variables, we included the deprivation index of the census track of the mother’s residence. Census tracks are the smallest administrative unit in Spain [32]. The deprivation index uses six indicators (manual and temporary workers, unemployment, insufficient education overall and in young people [16–29 years], and no access to internet) from the 2011 Population and Housing Census of Spain to estimate deprivation levels for 35,917 enumeration districts. The deprivation index ranges from −2.58 (lower deprivation) to 4.88 (higher deprivation), meaning that the interpretation of the deprivation index is directly proportional to the number—the higher the number, the greater the deprivation [39]. The region of each child, at diagnosis for cases and at birth for controls, was included in the model as a random effect to control for the differences between Spain’s different regions.
2.5. Statistical Analysis
Before the association analysis and to evaluate the potential bias for the exclusion of those cases with different residential address at birth and at diagnosis, we performed a descriptive analysis between the included-cases group and the excluded-cases group.
For the analysis, the association between the estimation of PM exposure and cancer incidence was estimated by calculating the OR and its 95% confidence interval using logistic regression models for the continuous and categorical variables. We included in the model the following covariates: year of birth, sex, deprivation index, and Autonomous Region. These models were fitted for total leukemia cases, ALL cases, AML cases, and, under 5 years, all cases. To explore a potential dose–response relationship, we computed the trend p-value of the estimated ORs for the categorical variable. In addition, we fitted generalized additive models (GAMs) to estimate the non-linear relationship between PM levels and leukemia incidence. We set statistical significance to a p-value < 0.05. For this analysis, we used the software package R, Version 3.6.2 (12 December 2019).
2.6. Data Protection
The protection of confidential data has been carried out in accordance with the provisions of Chapter V of Regulation (EC) No. 223/2009 of the European Parliament and of the Council of 11 March 2009.
3. Results
The initial descriptive analysis between the included and not-included cases showed that the number of included cases was 1066 up to 2414—44%. This percentage of included cases was fairly constant along the covariates; for example, the percentage of males included was 56%, while the percentage of male in the RETI-SEHOP register for the studied period was 54%. In respect of year of birth, the percentage of included cases varied from 38% to 50%, with 44% as the mean. The same occurred with the Autonomous Region, where the mean percentage was 43%, with a wider variation in the smaller regions.
This study included 3,112,123 children. Table 1 presents the descriptive values of our main variables, as follows: frequencies and percentages for qualitative variables, and the mean and standard deviation for quantitative variables. In summary, slightly more boys (51.60%) than girls (48.40%) were included. The average age at cancer diagnosis was 4.5 years old for all leukemias and also for ALL. In the case of AML, the average age was lower, at 4.25 years. Regarding the deprivation index, children with leukemia had a slightly lower index of −0.35, while the controls had −0.29, as shown in Table 1.

Table 1.
Descriptive values of the sample, including percentages with frequencies of responses, and the mean with its standard deviation.
Table 2 shows the mean exposure to PM10 and PM2.5 for the controls and cases (separated into total leukemia, ALL, and AML). It can be observed that PM10 exposure levels for cases are higher than those for the controls for total leukemias and for ALL and AML.

Table 2.
Descriptive values of PM10 and PM2.5 exposure levels with mean and standard deviation for controls and leukemia (separated into ALL and AML) during total pregnancy and by trimesters.
Table 3 shows the results of the logistic regressions models for total leukemia. Both analyses with continuous and categorized variables are included. The results for the continuous variable of PM10 exposure levels indicate an increased risk of childhood leukemia to be associated with higher exposure. The results for the categorized PM10 variable suggest an increased risk of childhood leukemia among pregnant women whose exposure level were higher than the median, third, and fourth quartiles, compared to those women who were less exposed. For all trimesters, the OR in Q4 was statistically significant. The trending p-value was < 0.05 for the total pregnancy and for the second and third trimester. The estimated OR for PM2.5 showed increased risk values; nevertheless, these were not statistically significant. This happened for both continuous and categorical variables and for the average exposure during the total pregnancy, and for the first and second trimester.

Table 3.
Odds ratios (ORs) and their respective 95% confidence interval (95%CI) for PM10 and PM2.5 average exposure levels as continuous and categorical variables during total pregnancy and by trimester. “Cont” stands for continuous variable and “Cat” for categorical. * Reference category for categorical variables. p stands for p-value. Trend p-value < 0.05.
Figure 1 shows the results from the non-linear model that illustrates the change in total leukemia risk with increasing levels of PM10 exposure for the pregnancy-average. A growing trend can be seen starting from lower values (<0 s(PM10)) to risk values (>0 s(PM10)) when exposure levels exceed approximately 25 μg/m3.
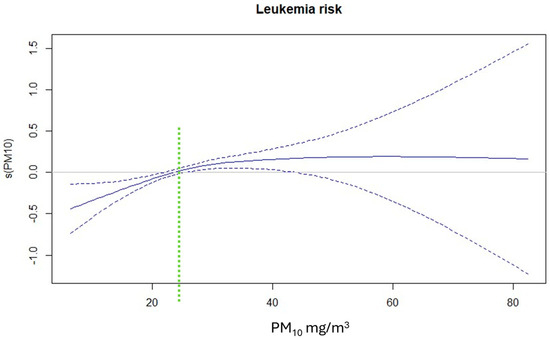
Figure 1.
Non-linear relationship between PM10 exposure levels in μg/m3 and risk of childhood leukemia.
Table 4 shows the results of logistic regressions conducted for ALL, ALM, and children under 5 years old. Both continuous and categorized variable analyses are included. The results for the continuous variable in cases of ALL indicate an increased risk associated with the average exposure during the entire pregnancy and in the third trimester. The results for the categorized variable reflect patterns similar to those found in total leukemias (Table 3), with an increased risk of childhood leukemia in pregnant women whose exposure levels were in the third and fourth quartiles, observed in both the total duration of pregnancy and by trimesters. For PM2.5, the estimated OR showed a very similar behavior to that in the analysis with all leukemia cases, suggesting an increased risk, but not one of statistical significance. The trending p-value was statistically significant for both PM10 and PM2.5 for the total pregnancy, and for PM10 for the three trimesters.

Table 4.
Odds ratios (ORs) and their respective 95% confidence interval (95% CI) for PM10 and PM2.5 exposure levels as continuous and categorical variables, and for ALL, AML, and children under five years of age during total pregnancy and by trimester. * Reference Category for Categorical Variables. “Cont” stands for continuous variable and “Cat” for categorical. * Reference category for categorical variables. p stands for p-value. Trend p-value < 0.05.
Regarding the results for AML cases, estimated ORs for PM10 indicated no association, while ORs for PM2.5 showed an excess of risk; nevertheless, these estimations were not statistically significant, but the trend was. Finally, for the results of the group of children under 5 years old, estimated ORs for both PM10 and PM2.5 showed an increased risk to be observed throughout the entire pregnancy and in the first trimester for both continuous and categorical variables; however, only the ORs for PM10 were statistically significant. The trend was significant for the total pregnancy and for the firth and second trimester.
4. Discussion
In this population-based cohort study, we examined the effects of exposure to particulate matter (PM) during pregnancy on the risk of childhood leukemia in several Spanish regions. Our findings support the hypothesis of an association between exposure to higher concentrations of PM and the incidence of childhood leukemia. Both continuous and categorial variables showed an increased risk that was stronger among pregnant women exposed to the highest levels. We observed similar results in cases of ALL and leukemias in children under five years of age. The association was stronger in PM10 than PM2.5 and only PM10 showed a statistical significance. In relation to the exposure window results, PM10 presented similar results among the trimesters, suggesting that there is not a critical exposure window. For AML, the results for PM10 and PM2.5 showed opposite effects—while exposure to PM10 did not suggest an increased risk of AML, exposure to PM2.5 did suggest it. In any case, these estimations were not statistically significant, most possibly because of the low number of cases—157 cases for PM10 and 64 for PM2.5.
Previous studies have shown these potential associations. For example, in a recent study published in 2022, conducted by Min Lee et al. in South Korea [40], their results showed that an increase of 10 μg/m3 in PM2.5 exposure levels lead to an increase in the risk of childhood cancer, but no association was found for PM10 exposure. In the analysis, they found an association between PM2.5 exposure and ALL, but no association with AML. These results showed a stronger association for PM2.5 exposure than our study. However, we observed an association between PM10 exposure and childhood leukemia, both overall and for ALL and AML separately. This discrepancy in the results obtained from both studies could be due to the different methodologies employed. In the South Korean study, exposures were not evaluated during pregnancy, but during the children’s lifetime, leading them to exclude all cases of children under five years old at diagnosis, which are more closely related to prenatal environmental exposures. Another study by Lavigne et al. in Canada, published in 2016 [30], showed no association between PM2.5 exposure and childhood leukemia. The methodology used differed from ours, as it included exposures during the first year of the child’s life in their analysis. And results were different too, since we found a weak association, but they we did not find an association with PM2.5 exposure.
More studies have focused on air pollution where PM was one of the studied pollutants. For instance, in a study conducted in California, they found an association between traffic-related air pollution and ALL, but not with LMA. This study included CO, NO, and PM2.5 as traffic-related pollutants. We found a weak association between leukemia and PM2.5, suggesting that the association found in this study could also be due to the effect of NO and CO [41]. Also, in another Californian study of prenatal exposure to traffic-related air pollution and an increased risk of childhood tumors [31], they found an association between traffic-related air pollution exposure and an increased risk of ALL, with a stronger association during the first and second trimesters. They did not measure PM exposure though, but NO2, yet their results align with ours, as we found associations across all trimesters and for overall exposure during pregnancy. These findings support the hypothesis of a prenatal origin of ALL, given that preleukemic cells have been detected in blood samples from newborns who were later diagnosed with ALL [42].
The results of our linear analysis suggested that exposure levels of PM10 above 25 μg/m3 could increase the risk of childhood leukemia. Currently, the EU air quality standards set the yearly average limit at 40 μg/m3 [43], while the WHO-recommended limit is 15 μg/m3. Our results align with the WHO recommendations, suggesting that the current EU limits are far too high [44].
Regarding the methodology of measuring PM environmental exposure, we found that studies with different methodologies often yield contradictory results, which could partly be due this fact. For example, in the previously cited South Korean study [40], PM10 exposure was calculated by collecting data from air quality monitoring stations throughout the country. But more recent studies have used satellite data to estimate PM exposure, such as the study conducted in Mexico published in 2024, which used a model combining satellite data and meteorological variables and land use variable [45], similar to the models used in our research [36]. These kinds of models exhibited a good performance and allow for the simulation and prediction of air quality in different regions and periods, using this data to estimate PM2.5 exposure levels at residential addresses [46]. In addition to the method of PM estimation, the estimation period is also variable between studies. Some studies focus on the pregnancy period [41], like ours, and others estimated the exposure after birth [40]. These heterogenous methodologies limit the comparison of the result between studies.
Along with what we just mentioned, another important limitation of the present study is the non-inclusion of individual data relating to possible confounding factors that might be related to the PM, such as socio-economic status or lifestyle-related factors, because of their unavailability at an individual level. Yet, to minimize this limitation, we included in the analysis the deprivation index at the census-track level. Furthermore, we did not have information about address changes between birth and diagnosis; therefore, we limited the analysis to those cases with the same address at birth and at diagnosis. This could introduce a potential bias if those children that moved had a different PM exposure than those that did not move, but as we showed in the initial descriptive analysis, the two groups did not differ significantly according to the covariates. In our sensitivity analysis with the under 5-year-olds cases, where the percentage of same address was higher, we did not find substantial differences in the estimated ORs either. Nevertheless, this problem would limit the capacity to find positive results, but in no way does it invalidate the associations found.
This study has several strengths such as the large case group and, in particular, the very large control group, that in this case is the cohort of newborns in the studied period for most of the Spanish territory. This large group provides a much more realistic image of the spatial distribution of the at-risk population. Another strength is the availability of detailed individual concentrations of PM during pregnancy, which was estimated using standardized and validated methods.
5. Conclusions
The findings of this study suggest an association between exposure to PM10 during pregnancy and an increased risk of childhood total leukemia and ALL, but not for AML. Also, our results suggest that it could be a possible dose–response relationship, where higher exposure levels correspond to a greater risk, but there would be no critical exposure window. In this context, we established that the increased risk of childhood leukemia occurs when exposure levels of PM10 exceed 25 μg/m3. Consequently, we suggest that the WHO’s recommendations on exposure levels should be reviewed. In connection with PM2.5, this study suggests a potential association with AML, but there are less data supported than there are for PM10. Therefore, our findings indicate that public health interventions should aim to reduce air pollution to lower the incidence of childhood leukemia. Finally, this work is the first to study the relationship between PM10 exposure during pregnancy and the risk of childhood leukemia, suggesting that our findings should be confirmed with future research.
Author Contributions
Conceptualization, R.R.; methodology, M.G. and R.R.; validation, E.S.O. and R.R.; formal analysis, E.S.O. and R.R.; investigation, E.S.O. and R.R.; resources, R.R. and M.G.; data curation, E.S.O.; writing—original draft preparation, E.S.O.; writing—review and editing, ALL; visualization, E.S.O.; supervision, R.R.; project administration, R.R.; funding acquisition, R.R. and M.G. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Carlos III Institute of Health, Spain (grant numbers PI19CIII/00025 and PI16CIII/00009); Spain’s Health Research Fund (Fondo de Investigación Sanitaria-FIS grant number 12/01416); and by the Spanish Consortium for Research on Epidemiology and Public Health (ESP20PI01/2020). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Carlos III Institute of Health (CEI PI 72_2016-v2, 6 February 2017).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to keeping the subjects’ privacy.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. This article presents independent research. The views expressed are those of the authors and not necessarily those of the Carlos III Institute of Health.
References
- Peris-Bonet, R.; Salmerón, D.; Martínez-Beneito, M.A.; Galceran, J.; Marcos-Gragera, R.; Felipe, S.; González, V.; Codina, J.S.d.T. Childhood cancer incidence and survival in Spain. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. ESMO 2010, 21 (Suppl. 3), iii103–iii110. [Google Scholar] [CrossRef] [PubMed]
- Pardo Romaguera, E.; Munoz López, A.; Valero Poveda, S.; Porta Cebolla, S.; Fernandez-Delgado, R.; Barreda Reines, M.S.; Peris Bonet, R. Cancer infantil en España. Estadísticas 1980–2017. In Registro Español de Tumores Infantiles (RETI-SEHOP); Universitat de València: Valencia, Spain, 2018. [Google Scholar]
- Marcos-Gragera, R.; Galceran, J.; Martos, C.; Quirós-Garcia, J.R.; Sánchez, M.-J.; Ardanaz, E.; Ramos, M.; Mateos, A.; Salmerón, D.; Felipe, S.; et al. Incidence and survival time trends for Spanish children and adolescents with leukaemia from 1983 to 2007. Clin. Transl. Oncol. 2017, 19, 301–316. [Google Scholar] [CrossRef] [PubMed]
- Coebergh, J.W.W.; Reedijk, A.M.J.; de Vries, E.; Martos, C.; Jakab, Z.; Steliarova-Foucher, E.; Kamps, W.A. Leukaemia incidence and survival in children and adolescents in Europe during 1978–1997. Report from the Automated Childhood Cancer Information System project. Eur. J. Cancer 2006, 42, 2019–2036. [Google Scholar] [CrossRef] [PubMed]
- Greaves, M.F.; Alexander, F.E. An infectious etiology for common acute lymphoblastic leukemia in childhood? Leukemia 1993, 7, 349–360. [Google Scholar] [PubMed]
- Buffler, P.A.; Kwan, M.L.; Reynolds, P.; Urayama, K.Y. Environmental and genetic risk factors for childhood leukemia: Appraising the evidence. Cancer Investig. 2005, 23, 60–75. [Google Scholar] [CrossRef]
- Gurney, J.G.; Severson, R.K.; Davis, S.; Robison, L.L. Incidence of cancer in children in the United States. Sex-, race-, and 1-year age-specific rates by histologic type. Cancer 1995, 75, 2186–2195. [Google Scholar] [CrossRef] [PubMed]
- Shu, X.O.; Perentesis, J.P.; Wen, W.; Buckley, J.D.; Boyle, E.; Ross, J.A.; Robison, L.L. Parental exposure to medications and hydrocarbons and ras mutations in children with acute lymphoblastic leukemia: A report from the Children’s Oncology Group. Cancer Epidemiology Biomarkers Prev. 2004, 13, 1230–1235. [Google Scholar] [CrossRef]
- Castro-Jiménez, M.Á.; Orozco-Vargas, L.C. Parental exposure to carcinogens and risk for childhood acute lymphoblastic leukemia, Colombia, 2000–2005. Prev. Chronic. Dis. 2011, 8, A106. [Google Scholar] [PubMed]
- Metayer, C.; Petridou, E.; Aranguré, J.M.M.; Roman, E.; Schüz, J.; Magnani, C.; Mora, A.M.; Mueller, B.A.; de Oliveira, M.S.P.; Dockerty, J.D.; et al. Parental Tobacco Smoking and Acute Myeloid Leukemia: The Childhood Leukemia International Consortium. Am. J. Epidemiol. 2016, 184, 261–273. [Google Scholar] [CrossRef]
- Chunxia, D.; Meifang, W.; Jianhua, Z.; Ruijuan, Z.; Xiue, L.; Zhuanzhen, Z.; Linhua, Y. Tobacco smoke exposure and the risk of childhood acute lymphoblastic leukemia and acute myeloid leukemia: A meta-analysis. Medicine 2019, 98, e16454. [Google Scholar] [CrossRef]
- Wheeler, D. Racing to the Bottom? Foreign Investment and Air Pollution in Developing Countries. J. Environ. Dev. 2001, 10, 225–245. [Google Scholar] [CrossRef]
- Brunekreef, B.; Holgate, S.T. Air pollution and health. Lancet 2002, 360, 1233–1242. [Google Scholar] [CrossRef] [PubMed]
- GBD 2013 Risk Factors Collaborators; Forouzanfar, M.H.; Alexander, L.; Anderson, H.R.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Burnett, R.; Casey, D.; Coates, M.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Hu, J.; Li, J.; Gong, K.; Wang, X.; Ying, Q.; Qin, M.; Liao, H.; Guo, S.; Hu, M.; et al. Modelling air quality during the EXPLORE-YRD campaign—Part II. Regional source apportionment of ozone and PM2.5. Atmos Environ. 2021, 247, 118063. [Google Scholar] [CrossRef]
- Miller, F.J.; Gardner, D.E.; Graham, J.A.; Lee, R.E., Jr.; Wilson, W.E.; Bachmann, J.D. Size Considerations for Establishing a Standard for Inhalable Particles. J. Air. Pollut. Control Assoc. 1979, 29, 610–615. [Google Scholar] [CrossRef]
- Bongaerts, E.; Lecante, L.L.; Bové, H.; Roeffaers, M.B.J.; Ameloot, M.; Fowler, P.A.; Nawrot, T.S. Maternal exposure to ambient black carbon particles and their presence in maternal and fetal circulation and organs: An analysis of two independent population-based observational studies. Lancet Planet Health 2022, 6, e804–e811. [Google Scholar] [CrossRef]
- Zanini, M.J.; Domínguez, C.; Fernández-Oliva, T.; Sánchez, O.; Toda, M.T.; Foraster, M.; Dadvand, P.; Llurba, E. Urban-Related Environmental Exposures during Pregnancy and Placental Development and Preeclampsia: A Review. Curr. Hypertens. Rep. 2020, 22, 81. [Google Scholar] [CrossRef]
- Trasande, L.; Malecha, P.; Attina, T.M. Particulate Matter Exposure and Preterm Birth: Estimates of U.S. Attributable Burden and Economic Costs. Environ. Health Perspect. 2016, 124, 1913–1918. [Google Scholar] [CrossRef]
- Hjortebjerg, D.; Andersen, A.M.N.; Ketzel, M.; Pedersen, M.; Raaschou-Nielsen, O.; Sørensen, M. Associations between maternal exposure to air pollution and traffic noise and newborn’s size at birth: A cohort study. Environ. Int. 2016, 95, 1–7. [Google Scholar] [CrossRef]
- Dadvand, P.; Parker, J.; Bell, M.L.; Bonzini, M.; Brauer, M.; Darrow, L.A.; Gehring, U.; Glinianaia, S.V.; Gouveia, N.; Ha, E.-H.; et al. Maternal exposure to particulate air pollution and term birth weight: A multi-country evaluation of effect and heterogeneity. Environ. Health Perspect. 2013, 121, 267–373. [Google Scholar] [CrossRef]
- Johnson, N.M.; Hoffmann, A.R.; Behlen, J.C.; Lau, C.; Pendleton, D.; Harvey, N.; Shore, R.; Li, Y.; Chen, J.; Tian, Y.; et al. Air pollution and children’s health-a review of adverse effects associated with prenatal exposure from fine to ultrafine particulate matter. Environ. Health Prev. Med. 2021, 26, 72. [Google Scholar] [CrossRef] [PubMed]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Some Non-Heterocyclic Polycyclic Aromatic Hydrocarbons and Some Related Exposures; IARC Press: Lyon, France, 2010; Volume 92, 853p. [Google Scholar]
- Vlaanderen, J.; Lan, Q.; Kromhout, H.; Rothman, N.; Vermeulen, R. Occupational benzene exposure and the risk of chronic myeloid leukemia: A meta-analysis of cohort studies incorporating study quality dimensions. Am. J. Ind. Med. 2012, 55, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, P.; Von Behren, J.; Gunier, R.B.; Goldberg, D.E.; Hertz, A.; Smith, D. Traffic patterns and childhood cancer incidence rates in California, United States. Cancer Causes Control 2002, 13, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Feychting, M.; Svensson, D.; Ahlbom, A. Exposure to motor vehicle exhaust and childhood cancer. Scand. J. Work Environ. Health 1998, 24, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Elliott, E.G.; Trinh, P.; Ma, X.; Leaderer, B.P.; Ward, M.H.; Deziel, N.C. Unconventional oil and gas development and risk of childhood leukemia: Assessing the evidence. Sci. Total Environ. 2017, 576, 138–147. [Google Scholar] [CrossRef] [PubMed]
- IARC. Outdoor Air Pollution. Available online: https://publications.iarc.fr/Book-And-Report-Series/Iarc-Monographs-On-The-Identification-Of-Carcinogenic-Hazards-To-Humans/Outdoor-Air-Pollution-2015 (accessed on 6 June 2024).
- Filippini, T.; Hatch, E.E.; Rothman, K.J.; Heck, J.E.; Park, A.S.; Crippa, A.; Orsini, N.; Vinceti, M. Association between Outdoor Air Pollution and Childhood Leukemia: A Systematic Review and Dose-Response Meta-Analysis. Environ. Health Perspect. 2019, 127, 46002. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, É.; Bélair, M.A.; Do, M.T.; Stieb, D.M.; Hystad, P.; van Donkelaar, A.; Martin, R.V.; Crouse, D.L.; Crighton, E.; Chen, H.; et al. Maternal exposure to ambient air pollution and risk of early childhood cancers: A population-based study in Ontario, Canada. Environ. Int. 2017, 100, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, J.K.C.; Heck, J.E.; Cockburn, M.; Su, J.; Jerrett, M.; Ritz, B. Prenatal exposure to traffic-related air pollution and risk of early childhood cancers. Am. J. Epidemiol. 2013, 178, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- INE. Instituto Nacional de Estadística. Available online: https://ine.es/ (accessed on 9 April 2024).
- Steliarova-Foucher, E.; Stiller, C.; Lacour, B.; Kaatsch, P. International Classification of Childhood Cancer, third edition. Cancer 2005, 103, 1457–1467. [Google Scholar] [CrossRef]
- Registro Español de Tumores Infantiles RETI-SEHOP. Available online: https://www.uv.es/rnti/cifrasCancer.html (accessed on 19 March 2024).
- Ramis, R.; Gómez-Barroso, D.; Tamayo, I.; García-Pérez, J.; Morales, A.; Romaguera, E.P.; López-Abente, G. Spatial analysis of childhood cancer: A case/control study. PLoS ONE 2015, 10, e0127273. [Google Scholar] [CrossRef]
- Stafoggia, M.; Johansson, C.; Glantz, P.; Renzi, M.; Shtein, A.; de Hoogh, K.; Kloog, I.; Davoli, M.; Michelozzi, P.; Bellander, T. A Random Forest Approach to Estimate Daily Particulate Matter, Nitrogen Dioxide, and Ozone at Fine Spatial Resolution in Sweden. Atmosphere 2020, 11, 239. [Google Scholar] [CrossRef]
- Stafoggia, M.; Bellander, T.; Bucci, S.; Davoli, M.; de Hoogh, K.; Donato, F.D.; Gariazzo, C.; Lyapustin, A.; Michelozzi, P.; Renzi, M.; et al. Estimation of daily PM10 and PM2.5 concentrations in Italy, 2013-2015, using a spatiotemporal land-use random-forest model. Environ. Int. 2019, 124, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Whitworth, K.W.; Rector-Houze, A.M.; Chen, W.J.; Ibarluzea, J.; Swartz, M.; Symanski, E.; Iniguez, C.; Lertxundi, A.; Valentin, A.; González-Safont, L.; et al. Relation of prenatal and postnatal PM2.5 exposure with cognitive and motor function among preschool-aged children. Int. J. Hyg. Environ. Health 2024, 256, 114317. [Google Scholar] [CrossRef] [PubMed]
- Duque, I.; Domínguez-Berjón, M.F.; Cebrecos, A.; Prieto-Salceda, M.D.; Esnaola, S.; Sánchez, M.C.; Marí-Dell’olmo, M. Deprivation index by enumeration district in Spain, 2011. Gac. Sanit. 2021, 35, 113–122. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Lee, T.H.; Kim, S.; Song, M.; Bae, S. Association between long-term exposure to particulate matter and childhood cancer: A retrospective cohort study. Environ. Res. 2022, 205, 112418. [Google Scholar] [CrossRef] [PubMed]
- Heck, J.E.; Wu, J.; Lombardi, C.; Qiu, J.; Meyers, T.J.; Wilhelm, M.; Cockburn, M.; Ritz, B. Childhood cancer and traffic-related air pollution exposure in pregnancy and early life. Environ. Health Perspect. 2013, 121, 1385–1391. [Google Scholar] [CrossRef] [PubMed]
- Rossig, C.; Juergens, H. Aetiology of childhood acute leukaemias: Current status of knowledge. Radiat. Prot. Dosim. 2008, 132, 114–118. [Google Scholar] [CrossRef] [PubMed]
- EU Air Quality Standards—European Commission. Available online: https://environment.ec.europa.eu/topics/air/air-quality/eu-air-quality-standards_en (accessed on 3 June 2024).
- World Health Organization. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide. World Health Organization: Geneva, Switzerland, 2021; Available online: https://iris.who.int/handle/10665/345329 (accessed on 10 May 2024).
- McGuinn, L.A.; Gutiérrez-Avila, I.; Rosa, M.J.; Just, A.; Coull, B.; Kloog, I.; Ortiz, M.T.; Harari, H.; Martinez, S.; Osorio-Valencia, E.; et al. Association between prenatal and childhood PM2.5 exposure and preadolescent anxiety and depressive symptoms. Environ. Epidemiol. 2023, 8, e283. [Google Scholar] [CrossRef]
- Gutiérrez-Avila, I.; Arfer, K.B.; Carrión, D.; Rush, J.; Kloog, I.; Naeger, A.R.; Grutter, M.; Páramo-Figueroa, V.H.; Riojas-Rodríguez, H.; Just, A.C. Prediction of daily mean and one-hour maximum PM2.5 concentrations and applications in Central Mexico using satellite-based machine-learning models. J. Expo. Sci. Environ. Epidemiol. 2022, 32, 917–925. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).