Associations between Dust Exposure and Hospitalizations in El Paso, Texas, USA
Abstract
1. Introduction
2. Materials and Methods
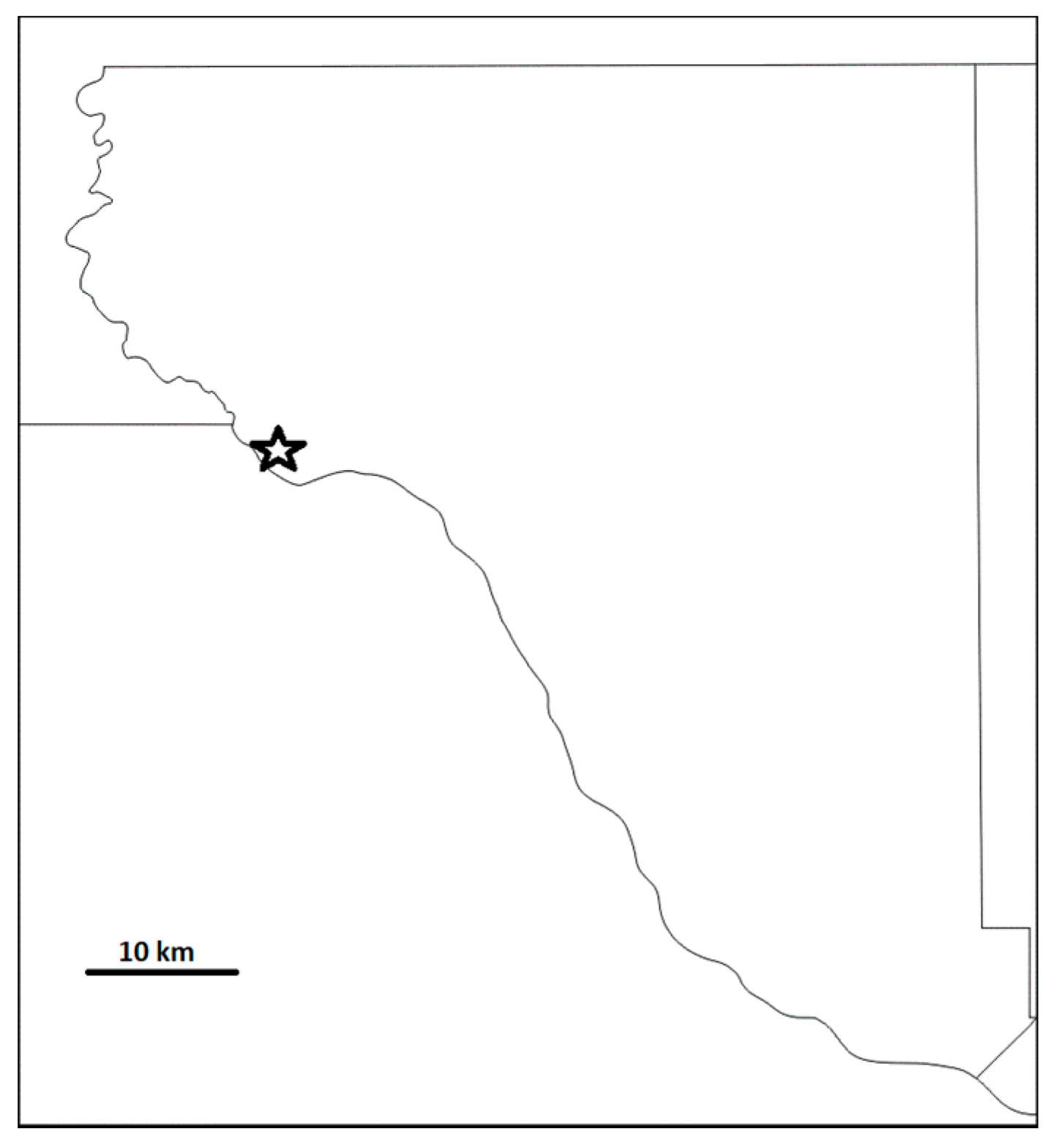
2.1. Data Sources
2.1.1. Hospital Admissions
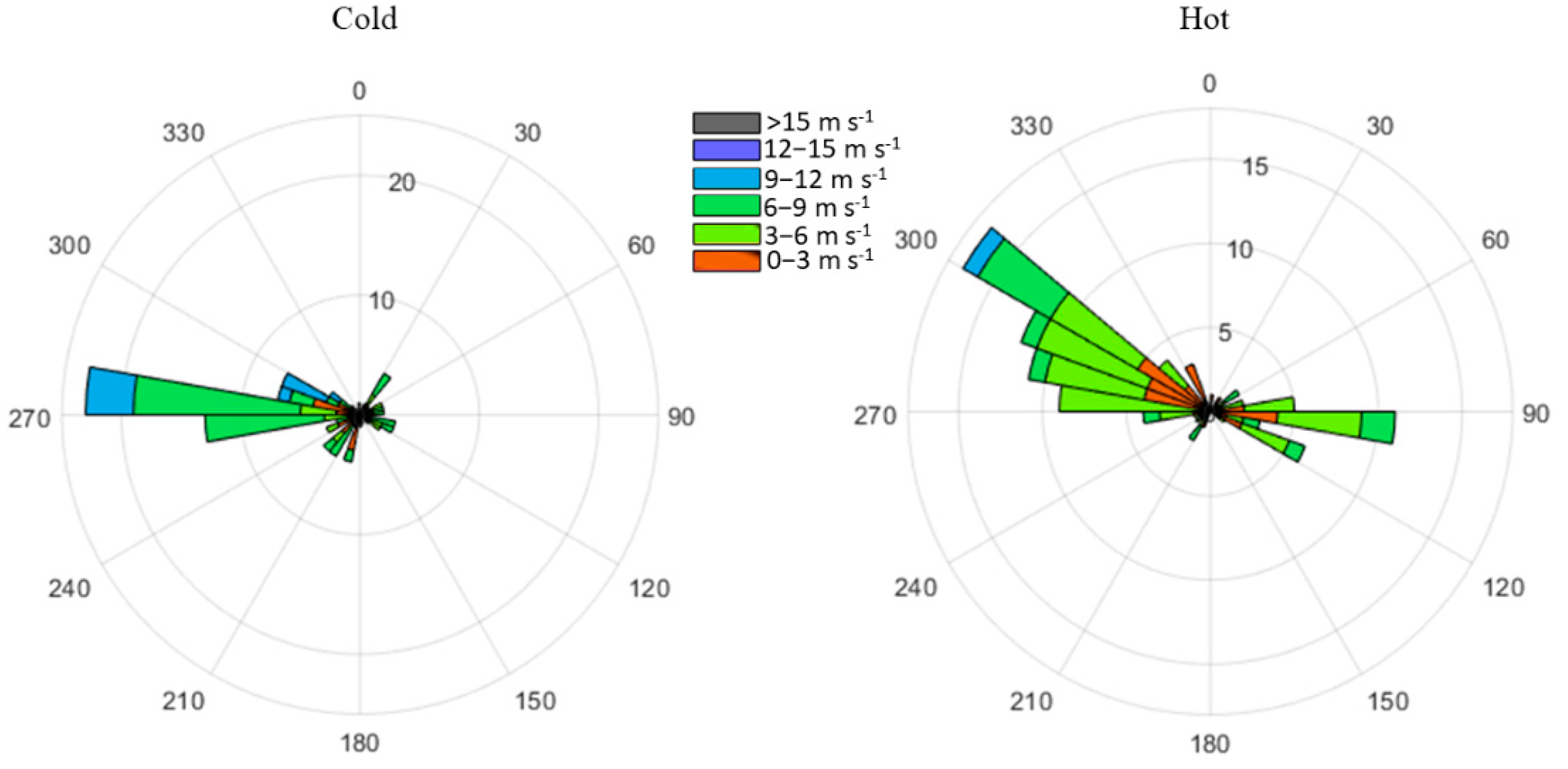
2.1.2. PM and Weather Data
2.2. Statistical Analyses
Model
3. Results
Summary of Significant Associations
4. Discussion
4.1. Associations with Increased PM10
4.2. Associations with Increased Wind Speed
4.3. Weekend, Season, and Holiday Associations
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kok, J.F.; Parteli, E.J.R.; Michaels, T.I.; Bou Karam, D. The physics of wind-blown sand and dust. Rep. Prog. Phys. 2012, 75, 106901. [Google Scholar] [CrossRef] [PubMed]
- Prospero, J.M.; Ginoux, P.; Torres, O.; Nicholson, S.E.; Gill, T.E. Environmental characterization of global sources of atmospheric soil dust identified with the Nimbus-7 total ozone mapping spectrometer (TOMS) absorbing aerosol product. Rev. Geophys. 2002, 40, 1002. [Google Scholar] [CrossRef]
- Ginoux, P.; Prospero, J.M.; Gill, T.E.; Hsu, N.C.; Zhao, M. Global-scale attribution of anthropogenic and natural dust sources and their emission rates based on MODIS Deep Blue aerosol products. Rev. Geophys. 2012, 50, RG3005. [Google Scholar] [CrossRef]
- Novlan, D.J.; Hardiman, M.; Gill, T.E. A Synoptic Climatology of Blowing Dust Events in El Paso, Texas from 1932–2005. In Proceedings of the 16th Symposium on Applied Climatology, San Antonio, TX, USA, 14–18 January 2007; American Meteorological Society: Boston, MA, USA, 2007. [Google Scholar]
- Rivera Rivera, N.I.; Gill, T.E.; Bleiweiss, M.P.; Hand, J.L. Source characteristics of hazardous Chihuahuan Desert dust outbreaks. Atmos. Environ. 2010, 44, 2457–2468. [Google Scholar] [CrossRef]
- Li, W.-W.; Orquiz, R.; Garcia, J.H.; Espino, T.; Pingitore, N.E.; Gardea-Torresdey, J.; Watson, J.G. Analysis of temporal and spatial dichotomous PM air samples in the El Paso-Cd. Juarez air quality basin. J. Air Waste Manag. Assoc. 2001, 51, 1551–1560. [Google Scholar] [CrossRef]
- Kavouras, I.G.; DuBois, D.W.; Nikolich, G.; Corral Avittia, A.Y.; Etyemezian, V. Particulate dust emission factors from unpaved roads in the U.S.-Mexico border semi-arid region. J. Arid Environ. 2016, 124, 189–192. [Google Scholar] [CrossRef]
- Baddock, M.C.; Gill, T.E.; Bullard, J.E.; Dominguez Acosta, M.; Rivera Rivera, N.I. Geomorphology of the Chihuahuan Desert based on potential dust emissions. J. Maps 2011, 7, 249–259. [Google Scholar] [CrossRef]
- Kandakji, T.; Gill, T.E.; Lee, J.A. Drought and land use/land cover impact on dust sources in Southern Great Plains and Chihuahuan Desert of the US: Inferring anthropogenic effect. Sci. Total Environ. 2021, 755, 142461. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.A.; Gill, T.E.; Mulligan, K.R.; Dominguez Acosta, M.; Perez, A.E. Land use/land cover and point sources of the 15 December 2003 dust storm in southwestern North America. Geomorphology 2009, 105, 18–27. [Google Scholar] [CrossRef]
- Staniswalis, J.G.; Parks, N.J.; Bader, J.O.; Muñoz-Maldonado, Y. Temporal Analysis of Airborne Particulate Matter Reveals a Dose-Rate Effect on Mortality in El Paso: Indications of Differential Toxicity for Different Particle Mixtures. J. Air Waste Manag. Assoc. 2005, 55, 893–902. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Pelt, R.S.; Shekhter, E.G.; Barnes, M.A.; Duke, S.E.; Gill, T.E.; Pannell, K.H. Spatial and temporal patterns of heavy metal deposition resulting from a smelter in El Paso, Texas. J. Geochem. Explor. 2020, 210, 106414. [Google Scholar] [CrossRef]
- Rivas, J.A. Dust Storms and the Dispersal of Aquatic Invertebrates in the Chihuahuan Desert Ecoregion. Ph.D. Thesis, University of Texas at El Paso, El Paso, TX, USA, 2019. Available online: https://scholarworks.utep.edu/dissertations/AAI27667795 (accessed on 25 October 2021).
- Ghio, A.J. Particle exposures and infections. Infection 2014, 42, 459–467. [Google Scholar] [CrossRef]
- Tong, D.Q.; Wang, J.; Gill, T.E.; Lei, H.; Wang, B. Intensified dust storm activity and Valley fever infection in the southwestern United States. Geophys. Res. Lett. 2017, 44, 4304–4312. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, M.D.; Calzadilla, A.S.; Salamo, O.; Sharifi, A.; Kumar, N.; Holt, G.; Campos, M.; Mirsaeidi, M. Lung health in era of climate change and dust storms. Environ. Res. 2018, 163, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Qiu, H.; Wang, L.; Duan, Z.; Yu, H.; Deng, R.; Zhan, D.; Zhou, L. Risks of hospital admissions from a spectrum of causes associated with particulate matter pollution. Sci. Total Environ. 2019, 656, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.; Wang, Y.; Williams, C.; Xu, C.; Kartsonaki, C.; Lin, Y.; Zhang, P.; Yin, P.; Lam, K.B.H. The association between high particulate matter pollution and daily cause-specific hospital admissions: A time-series study in Yichang, China. Environ. Sci. Pollut. Res. 2020, 27, 5240–5250. [Google Scholar] [CrossRef] [PubMed]
- Maciejewska, K. Short-term impact of PM2.5, PM10, and PMc on mortality and morbidity in the agglomeration of Warsaw, Poland. Air Qual. Atmos. Health 2020, 13, 659–672. [Google Scholar] [CrossRef]
- Khan, R.K.; Strand, M.A. Road dust and its effect on human health: A literature review. Epidemiol. Health 2018, 40, e2018013. [Google Scholar] [CrossRef]
- Morman, S.A.; Plumlee, G.S. Dust and human health. In Mineral Dust: A Key Player in The Earth System; Knippertz, P., Stuut, J.B.W., Eds.; Springer: Dordrecht, The Netherlands, 2014; pp. 385–409. [Google Scholar]
- Qiu, H.; Wang, L.; Zhou, L.; Pan, J. Coarse particles (PM2.5-10) and cause-specific hospitalizations in southwestern China: Association, attributable risk and economic costs. Environ. Res. 2020, 190, 110004. [Google Scholar] [CrossRef]
- Al-Taiar, A.; Thalib, L. Short-term effect of dust storms on the risk of mortality due to respiratory, cardiovascular and all-causes in Kuwait. Int. J. Biometeorol. 2014, 58, 69–77. [Google Scholar] [CrossRef]
- Wang, Y.C.; Lin, Y.K. Mortality associated with particulate concentration and Asian dust storms in Metropolitan Taipei. Atmos. Environ. 2015, 117, 32–40. [Google Scholar] [CrossRef]
- Shahsavani, A.; Tobías, A.; Querol, X.; Stafoggia, M.; Abdolshahnejad, M.; Mayvaneh, F.; Guo, Y.; Hadei, M.; Hashemi, S.S.; Khosravi, A.; et al. Short-term effects of particulate matter during desert and non-desert dust days on mortality in Iran. Environ. Int. 2020, 134, 105299. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Rodríguez, A.; Báez-Ferrer, N.; Abreu-González, P.; Rodríguez, S.; Díaz, R.; Avanzas, P.; Hernández-Vaquero, D. Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 727. [Google Scholar] [CrossRef]
- Grineski, S.E.; Staniswalis, J.G.; Bulathsinhala, P.; Peng, Y.; Gill, T.E. Hospital admissions for asthma and acute bronchitis in El Paso, Texas: Do age, sex, and insurance status modify the effects of dust and low wind events? Environ. Res. 2011, 111, 1148–1155. [Google Scholar] [CrossRef]
- Tam, W.W.; Wong, T.W.; Wong, A.H.; Hui, D.S. Effect of dust storm events on daily emergency admissions for respiratory diseases. Respirology 2012, 17, 143–148. [Google Scholar] [CrossRef]
- Chan, Y.S.; Teng, J.C.Y.; Liu, T.C.; Peng, Y.I. Asian dust storms and diabetes hospitalization: A nationwide population-based study. Air Qual. Atmos. Health 2018, 11, 1243–1250. [Google Scholar] [CrossRef]
- Badeenezhad, A.; Baghapour, M.A.; Sorooshian, A.; Keshavarz, M.; Azhdarpoor, A.; Goudarzi, G.; Hoseini, M. Investigating the relationship between central nervous system biomarkers and short-term exposure to PM10-bound metals during dust storms. Atmos. Pollut. Res. 2020, 11, 2022–2029. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, L.; Tong, D.; Wu, G.; Dan, M.; Teng, B. A Systematic Review of Global Desert Dust and Associated Human Health Effects. Atmosphere 2016, 7, 158. [Google Scholar] [CrossRef]
- Li, J.; Kandakji, T.; Lee, J.A.; Tatarko, J.; Blackwell, J.; Gill, T.E.; Collins, J.D. Blowing dust and highway safety in the southwestern United States: Characteristics of dust emission “hotspots” and management implications. Sci. Total Environ. 2018, 621, 1023–1032. [Google Scholar] [CrossRef]
- Rodopoulou, S.; Chalbot, M.C.; Samoli, E.; DuBois, D.W.; San Filippo, B.D.; Kavouras, I.G. Air pollution and hospital emergency room and admissions for cardiovascular and respiratory diseases in Doña Ana County, New Mexico. Environ. Res. 2014, 129, 39–46. [Google Scholar] [CrossRef]
- Al-Hemoud, A.; Al-Dousari, A.; Al-Shatti, A.; Al-Khayat, A.; Behbehani, W.; Malak, M. Health Impact Assessment Associated with Exposure to PM10 and Dust Storms in Kuwait. Atmosphere 2018, 9, 6. [Google Scholar] [CrossRef]
- Khaniabadi, Y.O.; Daryanoosh, S.M.; Amrane, A.; Polosa, R.; Hopke, P.K.; Goudarzi, G.; Mohammadi, M.J.; Sicard, P.; Armin, H. Impact of Middle Eastern Dust Storms on Human Health. Atmos. Pollut. Res. 2017, 8, 606–613. [Google Scholar] [CrossRef]
- Ueda, K.; Nitta, H.; Odajima, H. The effects of weather, air pollutants, and Asian dust on hospitalization for asthma in Fukuoka. Environ. Health Prev. Med. 2010, 15, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Liu, T.C.; Keller, J.; Lin, H.C. Asian dust storm events are associated with an acute increase in stroke hospitalisation. J. Epidemiol. Community Health 2013, 67, 125–131. [Google Scholar] [CrossRef]
- Merrifield, A.; Schindeler, S.; Jalaludin, B.; Smith, W. Health effects of the September 2009 dust storm in Sydney, Australia: Did emergency department visits and hospital admissions increase? Environ. Health 2013, 12, 1–7. [Google Scholar] [CrossRef]
- Leys, J.F.; Heidenreich, S.K.; Strong, C.L.; McTainsh, G.H.; Quigley, S. PM10 concentrations and mass transport during “Red Dawn”–Sydney 23 September 2009. Aeolian Res. 2011, 3, 327–342. [Google Scholar] [CrossRef]
- American Hospital Association; American Medical Record Association; Health Care Financing Administration; National Center for Health Statistics. ICD-9-CM coding and reporting official guidelines. J. Am. Med Rec. Assoc. 1990, 61, 1–17. [Google Scholar]
- Meng, Z.; Lu, B. Dust events as a risk factor for daily hospitalization for respiratory and cardiovascular diseases in Minqin, China. Atmos. Environ. 2007, 41, 7048–7058. [Google Scholar] [CrossRef]
- Touloumi, G.; Atkinson, R.; Le Tertre, A.; Samoli, E.; Schwartz, J.; Schindler, C. Analysis of health outcome time series data in epidemiological studies. Environmetrics 2004, 15, 101–117. [Google Scholar] [CrossRef]
- Santos, U.P.; Terra-Filho, M.; Lin, C.A.; Pereira, L.A.; Vieira, T.C.; Saldiva, P.H.; Braga, A.L. Cardiac arrhythmia emergency room visits and environmental air pollution in Sao Paulo, Brazil. J. Epidemiol. Community Health 2008, 62, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, Y.; Feng, F.; Cheng, B.; Wang, H.; Shen, J.; Jiao, H. Association between PM10 and specific circulatory system diseases in China. Sci. Rep. 2021, 11, 12129. [Google Scholar] [CrossRef] [PubMed]
- Xu, A.; Mu, Z.; Jiang, B.; Wang, W.; Yu, H.; Zhang, L.; Li, J. Acute Effects of Particulate Air Pollution on Ischemic Heart Disease Hospitalizations in Shanghai, China. Int. J. Environ. Res. Public Health 2017, 14, 168. [Google Scholar] [CrossRef] [PubMed]
- Rublee, C.S.; Sorensen, C.J.; Lemery, J.; Wade, T.J.; Sams, E.A.; Hilborn, E.D.; Crooks, J.L. Associations Between Dust Storms and Intensive Care Admissions in the United States, 2000–2015. Geohealth 2020, 4, e2020GH000260. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.S.; Chan, Y.S.; Liu, T.C. Tracheitis hospital admissions are associated with Asia dust storm. Int. J. Environ. Health Res. 2021. [Google Scholar] [CrossRef]
- Gutierrez, M.P.; Zuidema, P.; Mirsaeidi, M.; Campos, M.; Kumar, N. Association between African Dust Transport and Acute Exacerbations of COPD in Miami. J. Clin. Med. 2020, 9, 2496. [Google Scholar] [CrossRef]
- Allessandrini, E.R.; Stafoggia, M.; Faustini, A.; Gobbi, G.P.; Forastiere, F. Saharan dust and the association between particulate matter and hospitalizations in Rome, Italy. Occup. Environ. Med. 2013, 70, 432–434. [Google Scholar] [CrossRef]
- Lai, L.W.; Cheng, W.L. The impact of air quality on respiratory admissions during Asian dust storm periods. Int. J. Environ. Health Res. 2008, 18, 429–450. [Google Scholar] [CrossRef]
- Golightly, E.; Jabbour, H.N.; Norman, J.E. Endocrine immune interactions in human parturition. Mol. Cell. Endocrinol. 2011, 335, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Schifano, P.; Asta, F.; Dadvand, P.; Davoli, M.; Basagana, X.; Michelozzi, P. Heat and air pollution exposure as triggers of delivery: A survival analysis of population-based pregnancy cohorts in Rome and Barcelona. Environ. Int. 2016, 88, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Kelley, M.C.; Ardon-Dryer, K. Analyzing two decades of dust events on the Southern Great Plains region of West Texas. Atmos. Pollut. Res. 2021, 12, 101091. [Google Scholar] [CrossRef]
- Álvaro-Meca, A.; Sánchez-López, A.; Resino, R.; Tamayo, E.; Resino, S. Environmental factors are associated with hospital admissions for sepsis-related pneumonia: A bidirectional case-crossover design. Environ. Res. 2020, 191, 110102. [Google Scholar] [CrossRef]
- Costa, L.G.; Cole, T.B.; Dao, K.; Chang, Y.C.; Coburn, J.; Garrick, J.M. Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol. Ther. 2020, 210, 107523. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, U.; Exner, T.; Wanka, E.R.; Bergemann, C.; Meyer-Arnek, J.; Hildenbrand, B.; Tufman, A.; Heumann, C.; Huber, R.M.; Bittner, M.; et al. Influence of air pressure, humidity, solar radiation, temperature, and wind speed on ambulatory visits due to chronic obstructive pulmonary disease in Bavaria, Germany. Int. J. Biometeorol. 2012, 56, 137–143. [Google Scholar] [CrossRef]
- Takagi, H.; Hari, Y.; Nakashima, K.; Kuno, T.; Ando, T. Wind and coronary artery disease. Eur. J. Prev. Cardiol. 2020, 27, 2259–2263. [Google Scholar] [CrossRef] [PubMed]
- Goldman, A.; Eggen, B.; Golding, B.; Murray, V. The health impacts of windstorms: A systematic literature review. Public Health 2014, 128, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Fasola, S.; Maio, S.; Baldacci, S.; La Grutta, S.; Ferrante, G.; Forastiere, F.; Stafoggia, M.; Gariazzo, C.; Silibello, C.; Carlino, G.; et al. Short-Term Effects of Air Pollution on Cardiovascular Hospitalizations in the Pisan Longitudinal Study. Int. J. Environ. Res. Public Health 2021, 18, 1164. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.R.; Chen, Y.M.; Chen, S.Y.; Chan, C.C. Associations between long-term particulate matter exposure and adult renal function in the Taipei metropolis. Environ. Health Perspect. 2017, 125, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Winquist, A.; Klein, M.; Tolbert, P.; Flanders, W.D.; Hess, J.; Sarnat, S.E. Comparison of emergency department and hospital admissions data for air pollution time-series studies. Environ. Health 2020, 11, 70. [Google Scholar] [CrossRef]
- Bundschuh, J.; Maity, J.P.; Mushtaq, S.; Vithanage, M.; Seneweera, S.; Schneider, J.; Bhattacharya, P.; Islam Khan, N.; Hamawand, I.; Guilherme, L.R.G.; et al. Medical geology in the framework of the sustainable development goals. Sci. Total Environ. 2017, 581, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Xu, Q.; Guo, X.H.; Fan, H.; Zhu, H. Particulate matter air pollution associated with hospital admissions for mental disorders: A time-series study in Beijing, China. Eur. Psychiatry 2017, 44, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Zhu, X.; Wang, L.; Pan, J.; Pu, X.; Zeng, X.; Zhang, L.; Peng, Z.; Zhou, L. Attributable risk of hospital admissions for overall and specific mental disorders due to particulate matter pollution: A time-series study in Chengdu, China. Environ. Res. 2019, 170, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, J.; McLeod, D.; Dowell, A. Do patients want to disclose psychological problems to GPs? Fam. Pract. 2005, 22, 631–637. [Google Scholar] [CrossRef]
- Tylee, A.; Walters, P. Under-recognition of anxiety and mood disorders in primary care: Why does the problem exist and what can be done? J. Clin. Psychiatry 2007, 68, 27–30. [Google Scholar] [PubMed]
- National Institute for Health and Care Excellence, UK (NICE). Depression in Adults: Recognition and Management. 2009. Available online: https://guidance.nice.org.uk/CG90 (accessed on 25 October 2021).
- World Health Organization (WHO). Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease. 2016. Available online: https://apps.who.int/iris/handle/10665/250141 (accessed on 25 October 2021).
- Middleton, N.; Kang, U. Sand and dust storms: Impact mitigation. Sustainability 2017, 9, 1053. [Google Scholar] [CrossRef]
- Middleton, N. Health in dust belt cities and beyond—An essay by Nick Middleton. BMJ 2020, 371, m3089. [Google Scholar] [CrossRef]
- National Weather Service. National Weather Service El Paso Weather Forecast Office. 2021. Available online: https://www.weather.gov/epz (accessed on 25 October 2021).
- Texas Commission on Environmental Quality. Today’s Texas Air Quality Forecast. 2021. Available online: https://www.tceq.texas.gov/airquality (accessed on 25 October 2021).
- Hofflinger, A.; Boso, A. Another one breathes the dust. The relation between severe air pollution episodes and school attendance in southern Chile. Local Environ. 2021, 26, 252–263. [Google Scholar] [CrossRef]
- Collins, T.W.; Grineski, S.E.; Chakraborty, J.; McDonald, Y.J. Understanding environmental health inequalities through comparative intracategorical analysis: Racial/ethnic disparities in cancer risks from air toxics in El Paso County, Texas. Health Place 2011, 17, 335–344. [Google Scholar] [CrossRef] [PubMed]


| Diseases | Total | Min | Max | Average | SD |
|---|---|---|---|---|---|
| Valley fever | 44 | 0 | 1 | 0.02 | 0.15 |
| ND | 435 | 0 | 4 | 0.24 | 0.51 |
| Coronary atherosclerosis | 2974 | 0 | 16 | 1.63 | 1.60 |
| Asthma | 3030 | 0 | 18 | 1.66 | 1.59 |
| MI | 4107 | 0 | 14 | 2.25 | 1.73 |
| Aftercare services (ICD-9 C.18) | 8258 | 0 | 28 | 4.52 | 3.21 |
| Injury and poisoning (ICD-9 C.17) | 21,398 | 0 | 63 | 11.72 | 4.89 |
| Respiratory system (ICD-9 C.8) | 23,401 | 0 | 96 | 12.82 | 8.93 |
| Circulatory system (ICD-9 C.7) | 31,345 | 0 | 68 | 17.17 | 7.03 |
| AD | 133,848 | 0 | 320 | 73.30 | 29.76 |
| All ICD-9 | 299,804 | 0 | 632 | 61.51 | 164.19 |
| AD (Associated Diseasses) | |||||
| Diabetes mellitus | 1069 | 0 | 6 | 0.59 | 0.81 |
| Cellulitis and abscess of leg | 2128 | 0 | 7 | 1.17 | 1.15 |
| Dehydration | 2254 | 0 | 11 | 1.23 | 1.29 |
| Osteoarthrosis | 3324 | 0 | 12 | 1.82 | 2.15 |
| Other chest pain | 3667 | 0 | 18 | 2.01 | 1.60 |
| Unspecified septicemia | 3834 | 0 | 9 | 2.10 | 1.52 |
| Mental Disorders | 3882 | 0 | 31 | 2.13 | 1.88 |
| Encounter for antineoplastic chemotherapy | 7056 | 0 | 18 | 3.86 | 2.84 |
| Genitourinary System | 8772 | 0 | 24 | 4.80 | 2.67 |
| Digestive System | 10,067 | 0 | 22 | 5.51 | 2.94 |
| Circulatory System | 12,361 | 0 | 34 | 6.77 | 3.37 |
| Respiratory System | 14,914 | 0 | 75 | 8.17 | 6.45 |
| Births | 60,520 | 0 | 192 | 33.14 | 17.13 |
| Max Hourly Wind Speed | Max Hourly PM10 | Max Temp | Avg Temp | Max RH | Avg RH | |
|---|---|---|---|---|---|---|
| Min | 1.12 | 7.8 | −9.6 | −11.77 | 8.7 | 4.40 |
| Max | 15.29 | 4739.3 | 41.1 | 34.67 | 100 | 89.3 |
| Average | 5.53 | 94.14 | 25.36 | 19.58 | 51.29 | 33.39 |
| SD | 2.24 | 178.11 | 8.71 | 8.59 | 20.87 | 16.14 |
| Data | Variable | Diseases | Lag Day | Higher Risk | ||
|---|---|---|---|---|---|---|
| RR | Lower 95% CI | Upper 95% CI | ||||
| Diseases with high hospitalization frequency | PM10 | ND | 7 | 1.051 | 1.009 | 1.095 |
| AD | 0 | 1.005 | 1.001 | 1.009 | ||
| 1 | 1.004 | 1.001 | 1.007 | |||
| 2 | 1.003 | 1.001 | 1.006 | |||
| Chemotherapy | 7 | 1.023 | 1.005 | 1.040 | ||
| Births | 3 | 1.005 | 1.00006 | 1.010 | ||
| Septicemia | 0 | 1.019 | 1.00005 | 1.039 | ||
| WS | Genitourinary | 0 | 1.056 | 1.001 | 1.114 | |
| Valley fever | 6 | 1.468 | 1.014 | 2.126 | ||
| Coronary atherosclerosis | 0 | 1.117 | 1.025 | 1.216 | ||
| ICD9 Category | PM10 | Circulatory system | 0 | 1.009 | 1.0004 | 1.017 |
| 7 | 1.011 | 1.003 | 1.018 | |||
| Aftercare services | 7 | 1.018 | 1.001 | 1.034 | ||
| All ICD-9 | 0 | 1.005 | 1.00022 | 1.009 | ||
| Injury and poisoning | 7 | 1.011 | 1.002 | 1.019 | ||
| Respiratory system | 6 | 1.007 | 1.000 | 1.013 | ||
| WS | Injury and poisoning | 0 | 1.037 | 1.002 | 1.074 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrera-Molina, E.; Gill, T.E.; Ibarra-Mejia, G.; Jeon, S. Associations between Dust Exposure and Hospitalizations in El Paso, Texas, USA. Atmosphere 2021, 12, 1413. https://doi.org/10.3390/atmos12111413
Herrera-Molina E, Gill TE, Ibarra-Mejia G, Jeon S. Associations between Dust Exposure and Hospitalizations in El Paso, Texas, USA. Atmosphere. 2021; 12(11):1413. https://doi.org/10.3390/atmos12111413
Chicago/Turabian StyleHerrera-Molina, Estrella, Thomas E. Gill, Gabriel Ibarra-Mejia, and Soyoung Jeon. 2021. "Associations between Dust Exposure and Hospitalizations in El Paso, Texas, USA" Atmosphere 12, no. 11: 1413. https://doi.org/10.3390/atmos12111413
APA StyleHerrera-Molina, E., Gill, T. E., Ibarra-Mejia, G., & Jeon, S. (2021). Associations between Dust Exposure and Hospitalizations in El Paso, Texas, USA. Atmosphere, 12(11), 1413. https://doi.org/10.3390/atmos12111413







