Abstract
The Southwestern USA has been identified as one of the most persistent dust-producing regions of North America, where exposure to inhalable particulate matter (PM10) originating from desertic landscape during dust events/dust exposures (DEs) can reach hazardous levels. El Paso, Texas’s ambient air has reached hazardous levels of PM10 from dust with near zero visibility due to these natural events originating in the surrounding Chihuahuan Desert. The aim of this study was to investigate whether dust exposures in El Paso (generally acute, short-term exposures from nearby source areas) are associated with significant increases in hospitalizations on the day of the exposure and up to seven days afterwards. Using a Poisson regression, it was found that the relative risks of hospitalizations due to a variety of conditions were associated with dust exposures (through increases of 100 μg/m3 maximum hourly PM10 and/or increases of 4.5 m/s maximum hourly wind speed) in El Paso County, Texas between 2010 and 2014. Valley fever, coronary atherosclerosis, genitourinary diseases, neurodegenerative diseases, injury and poisoning, circulatory system conditions, respiratory system diseases, births, septicemia, Associated Diseases (the aggregation of hospital admissions for all causes, each associated with at least 5% of hospitalizations), and all ICD-9 admissions were significantly positively associated with dust exposures, indicated from higher to lower significant risk, at different lag periods after exposure. These findings, showing that an association does exist between dust exposures and hospitalizations, have important implications for residents of the world’s dryland cities.
Keywords:
dust; wind; hospitalizations; quasi-Poisson regression analysis; health effects; aerosols; PM10 1. Introduction
Desert dust, emitted and transported in a process of soil erosion by strong winds [1], is a major natural source of particulate matter (PM) worldwide, especially in arid and semiarid regions [2,3]. Windblown dust activity is frequent in the city and surrounding county of El Paso, Texas, USA, the northern part of a large binational urban area contiguous with Ciudad Juarez, Chihuahua, Mexico. As of 2010, the population of El Paso County was approximately 800,000 and for Ciudad Juarez was estimated at 1.3 million, forming a conurbation of 2.1 million people. El Paso and Ciudad Juarez are located in the Chihuahuan Desert, one of the dust hotspots of the Western Hemisphere [2], and are surrounded by dust source areas, many ~100 km or less upwind of the urban area (Figure 1). Residents are exposed to these dust events on average approximately 15 times throughout the year, especially in the dry, windy season (November–May) [4]; the average length of a dust event in El Paso is approximately two hours [4], thus providing a short-term exposure to high concentrations of particulate matter. In addition to desert dust (sometimes exceeding the USA national ambient air quality standards (NAAQS) for particulate matter) [5], El Paso experiences unhealthy levels of PM from other sources, with road dust from unpaved roads being an important contributor [6]. The high percentage of unpaved roads in Ciudad Juárez, which is typically upwind of El Paso during the dry season [4], leads to an additional PM exposure from fugitive road dust during windy periods [7].
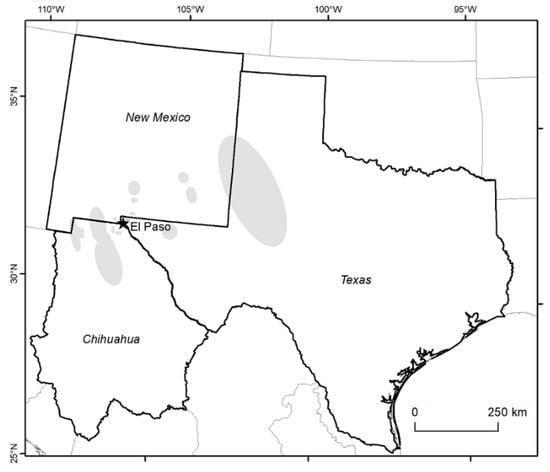
Figure 1.
Location of El Paso, Texas with regards to the surrounding states. Major dust source regions impacting the city [8,9] are shaded.
During dust events, atmospheric PM10 (particulate matter with mean aerodynamic diameter 10 µm or smaller) levels in El Paso often display marked peaks [10] that lead to acute doses of PM10 to anyone exposed [11]. The dust can penetrate inside buildings and can be enriched with potentially hazardous metals and other pollutants from anthropogenic sources [12]. Dust particles in wind events at El Paso are accompanied by even greater mass fractions of sand-sized grains predominantly composed of quartz [13], which is a form of crystalline silica, in itself recognized as a health hazard when inhaled [14]. The frequency of windblown dust events in the Southwestern USA was reported to have increased 240% from 1988 to 2011 [15] and is expected to continue to rise as climate changes [16]. Therefore, exposures to dust events and their particulate matter are likely to be an increasing hazard to human health in El Paso.
There are many studies that have sought to examine the effects of anthropogenic/urban (industrial, motor vehicle, and combustion by-products) sources of PM on human health, including hospital admissions [17], and some have found increases in PM10 to be associated with hospitalizations for all causes, cardiovascular and respiratory diseases [18,19]. Road dust also has widely documented human health effects [20]. Somewhat fewer studies have considered the specific health impacts of windblown dust [21]. A number of studies suggest that exposure to coarse particles [22] or PM10 in the form of desert dust can lead to serious health effects, including all-cause mortality [23,24,25], cardiovascular disease [26], respiratory diseases [14,15,16,27,28], diabetes [29], impacts on the central nervous system [30], fungal infections such as coccidioidomycosis (Valley fever) [15], various diseases [31], and injuries from visibility-related vehicular crashes [32]. Other investigations have looked at the associations of desert dust events specifically with hospitalization for specific conditions or diseases, such as respiratory and cardiovascular diseases [33,34], chronic obstructive pulmonary disease [35], asthma [36], and stroke [37]. No association was found for all-cause hospitalizations with the intense dust storm of 23 September 2009 in Sydney, Australia [38], a case where the dust was transported to the coastal metropolis from desert regions hundreds of kilometers inland [39]. However, few if any prior studies have evaluated the specific association of desert dust exposure with all-cause hospitalizations over a period of years in a desert city adjacent to dust sources.
Several previous studies have investigated the health effects of dust in the Chihuahuan Desert: Grineski et al. [27] showed a significant increase in asthma and bronchitis in association with dust events in El Paso, and Rodopoulou et al. [33] indicated that increased concentrations of particulate matter in Las Cruces, New Mexico, predominantly caused by dust events, were associated with increased emergency room visits for cardiovascular disease. Staniswalis et al. [11] determined that a 10 μg/m3 increment in the daily average PM10 in El Paso corresponded with a 2.06% increase in mortality 3 days after the increment.
The aim of this study is to investigate whether acute, short-term dust exposures (DE) in El Paso, Texas are associated with significant increases in hospitalizations on the day of the DE and up to seven days afterwards. Associations with DE are investigated for hospitalizations in the county of El Paso, Texas for all International Classification of Diseases, Ninth Revision (ICD-9) codes (aggregated together); individual ICD-9 category code groups; Neurodegenerative Diseases (ND); Mental Illness (MI); Valley Fever (VF); asthma; coronary atherosclerosis; other Associated Diseases (AD) (the aggregation of hospital admissions for all causes, each associated with at least 5% of hospitalizations), and each component of AD (births, respiratory system diseases, circulatory system diseases, digestive system diseases, genitourinary system diseases, encounter for antineoplastic chemotherapy, unspecified septicemia, other chest pain, dehydration, cellulitis and abscess of leg, osteoarthrosis, diabetes mellitus, and mental disorders) over a five-year period.
2. Materials and Methods
2.1. Data Sources
2.1.1. Hospital Admissions
Five years of hospitalizations and aftercare services data were obtained from the Texas Hospital Inpatient Research Data Files (RDF) from the Texas Department of State Health Services (TDSHS), Center for Health Statistics, Austin, Texas, USA for a five-year period for El Paso County—a total of 299,804 hospitalization registrations. The years 2010- 2014 were chosen because they included periods of relatively high and low dust event frequency [13]. Data included the following variables: date of admission, census block group of the patient, patient’s age, gender, and the principal ICD-9 diagnostic code. Principal diagnostic code was preferred over other diagnostic codes because it better captures the exacerbations of disease as opposed to other diagnostics due to existing diseases [40].
2.1.2. PM and Weather Data
Data for hourly average PM10 concentrations (µg/m3), hourly average wind speed (mph, reported here in m/s), hourly and daily average temperature (°F, reported here in °C), and hourly average and daily average relative humidity (%) measured at a Continuous Air Monitoring Station (CAMS) number 12 (CAMS-12) near the University of Texas at El Paso (UTEP) in El Paso, Texas, from 2010–2014 were obtained from the website of the site operator, the Texas Commission on Environmental Quality (TCEQ). The location of CAMS-12 within El Paso County is shown in Figure 2. For days in which the UTEP CAMS-12 site was not operating, data were obtained from the TCEQ CAMS 41 at Chamizal in El Paso, approximately 4 km east-southeast of CAMS-12. TCEQ reports meteorological data including temperature and wind speed using English units, and we analyzed the data in their native format. It was assumed that a DE had occurred on a day in which the maximum hourly average PM10 was at least 100 µg/m3 higher than the previous day or the maximum hourly average wind speed was at least 10 mph (4.5 m/s) higher than the previous day.
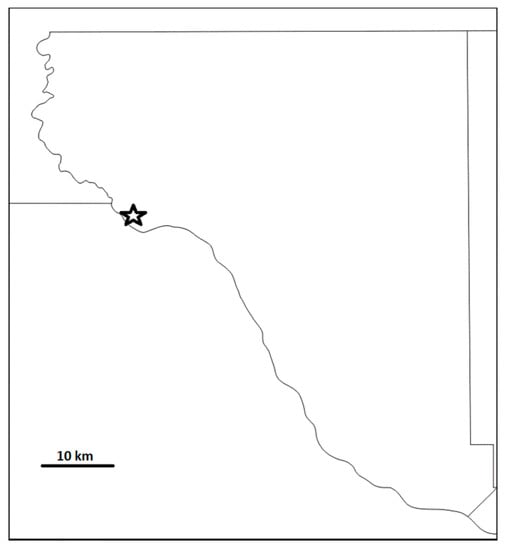
Figure 2.
Location of CAMS-12 monitoring site (star) within El Paso County, Texas.
Hourly maxima in PM10 concentrations and wind speeds were used because dust concentrations in El Paso often display high short-term peaks [10] from windblown dust events that average approximately 2 h in length [4], resulting in short-term acute DEs, and using the daily mean could underestimate these effects. These drastic changes in atmospheric particle concentration often exceed an order of magnitude increase over a few hours. High wind speed indicates the predominance of coarse particles and can be used as a surrogate variable for the PM10 in El Paso [11].
Because of the evidence of the prolonged health effects of a DE [41], the day with the DE (defined by maximum hourly increase in PM10 > 100 µg/m3 or wind speed > 10 mph/4.5 m/s) and the following seven days were identified for analysis. We estimated the effects of the current day’s DEs (lag 0) on hospitalizations and the effects of the DEs on admissions for the following seven days (lags 1–7).
2.2. Statistical Analyses
Relationships among dust exposures defined by meteorological parameters and hospital admissions were investigated by using a quasi-Poisson regression model, the regression model with an overdispersed Poisson family. Statistical analyses were performed by data analysis with Python and R (version 4.0.5) using the dlnm package sequentially; statistical significance was determined by p < 0.05.
Model
A generalized linear model with quasi-Poisson or Poisson family was generated to determine the associations between DE and hospitalizations due to ND, MI, VF, asthma, coronary atherosclerosis, AD and its components, and all ICD-9 categories and their components, during an eight-day period (the day of the DE and each of the seven days after the dust exposure). Cross-basis matrices for maximum PM10, maximum wind speed, daily average of temperature, and daily average humidity were included in the regression model to account for the lagged effects of the predictors. Natural splines were used as smoothing function of time for any time-dependent outcome predictors or confounders with long-term trends and seasonal patterns not explicitly included in the model [42]. Long-term trends and seasonal patterns (time with 7 degrees of freedom/year and day of the year) were analyzed with a natural cubic regression spline.
where E[Y] is the expected value of the Poisson distributed variable, Y, indicating the daily admissions count on a day for each diagnosis with Var(Y); refers to the intercept of the hospital admissions; refers to the coefficients associated with the PM10 concentration and wind speed (i = 1, 2); the coefficients associated with other covariates (j = 1, 2, ⋯, 11); is the cross-basis matrices of PM10 maximum hourly level on day with lags up to seven days; is the cross-basis matrices of wind speed maximum hourly average level on day with lags up to seven days; is the cross-basis matrices of average temperature by two lag strata, 0 and 1–3; is the cross-basis matrices of average relative humidity on day with lags up to five days; DustStorm is the dummy variable for dust storm days, defined by maximum hourly average PM10 of 150 µg/m3 and/or the maximum hourly average wind speed of 10 mph on day ; is the dummy variable for dust storm day plus the seven following days; season is the indicator variable for cold (October–March) and hot (April–September) period; holiday is indicator of a holiday; Weekday is the five working days from Monday to Friday; Weekend is Saturday and Sunday; Population is the estimated population increase or decrease; and s(∙) denotes the smooth function of the variable. Several models were run for each outcome of interest, that is, ND, MI, VF, asthma, coronary atherosclerosis, AD (independently and aggregated), and ICD-9 categories (independently and aggregated).
This description is as a full model. The stepwise variable selection technique was performed to select the best model from the full model for each disease. Relative risk (RR) for each associated diagnosis was calculated (e.g., RR per 100 μg/m3 increase in day-to-day maximum hourly PM10 or 10 mph (4.5 m/s) increase in day-to-day maximum hourly wind speed) based on the final selected regression model. The β1 represents the log of expected counts of hospital admission per 100 μg/m3 unit change in PM10, and β2 represents the log of expected counts of hospital admission per 10 mph (4.5 m/s) increase in wind speed, which can be estimated from the Poisson regression analysis.
3. Results
During the study period, there were a total of 299,804 hospitalizations. The daily average admissions for AD were 73.30 ± 29.76 with a minimum of 0 and a maximum of 320 hospitalizations. The greatest daily average admission was for Circulatory System Diseases, with 17.17 ± 7.03 with a minimum of 0 and a maximum of 68 hospitalizations. The fewest admissions were for Valley fever, with only 44 hospital admissions from 2010–2014. The descriptive analysis of the dependent variables (diseases) is shown in Table 1.

Table 1.
Descriptive analysis of disease categories and associated hospitalizations. El Paso County, TX, 2010–2014. Categories in bold were found by the analyses to have some significant association with specified increases in PM10 concentration and/or wind speed at some lag between 0 and 7 days. Categories in italics are part of AD; those in bold were individually significant.
The estimated average daily hourly maximum PM10 concentration was 94.14 ± 178.11 μg/m3 and the minimum and maximum values were 7.8 μg/m3 and 4739.3 μg/m3, respectively. The estimated maximum daily hourly average wind speed was 5.53 ± 2.24 m/s and the minimum and maximum values were 1.12 m/s and 15.29 m/s, respectively. Wind roses for the hour of maximum PM10 on dust exposure days (defined by PM10) for meteorological cold and warm seasons are shown in Figure 3. During high-wind events, the wind direction at CAMS-12 tends to be displaced slightly to the north compared to El Paso Airport [4] by the urban environment and local topography. The average daily temperature was 19.58 ± 8.59 °F, and the minimum and maximum daily averages were −11.8 and 34.7 °F, respectively. The descriptive analysis of the independent variables is shown in Table 2.
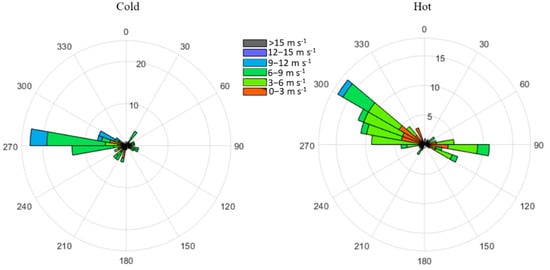
Figure 3.
Wind roses representing velocity and direction of sustained wind for hour of maximum PM10 concentration at TCEQ site CAMS-12, El Paso, Texas, on dust exposure dates defined by PM10 during 2010–2014. Cold season (left) includes October through March; hot season (right) includes April through September.

Table 2.
Descriptive analysis of maximum hourly wind speed (m/s), maximum hourly PM10 (μg/m3), maximum and average temperature (°C), maximum and average relative humidity (%) at TCEQ CAMS 12, El Paso, TX, 2010–2014.
Summary of Significant Associations
Results showing significant associations (all of them being increases) with dust exposures defined by the specified daily increases in maximum hourly PM10 and maximum hourly average wind speed, in terms of relative risks and upper and lower 95% confidence intervals, are given in Table 3 and illustrated in Figure 4. Significant associations were found for Associated Diseases on days 0, 1, and 2 after 100 μg/m3 increase in max hourly PM10; genitourinary diseases on day 0 with 4.5 m/s increase in max hourly wind speed; coronary atherosclerosis on day 0 with 4.5 m/s increase in max hourly wind speed; Valley fever on day 6 after a 4.5 m/s increase in max hourly wind speed; neurodegenerative diseases during the 7th day after a 100 μg/m3 increase in max hourly PM10; and antineoplastic chemotherapy and rehabilitation procedure during the 7th day after 100 μg/m3 increase in max hourly PM10. Borderline significant increases (defined as a lower CI >1.001 but <1.01 in the relative risk) were found for all hospitalizations (all ICD-9 categories) during the day of DE defined by 100 μg/m3 increase in max hourly PM10; septicemia during the day of DE defined by 100 μg/m3 increase in max hourly PM10; and births on day 3 after a 100 μg/m3 increase in max hourly PM10.

Table 3.
Significant associations between the diseases and DE-related variables, and the corresponding relative risk with 100-unit increase in maximum hourly PM10 and 4.5-unit increase in maximum hourly wind speed, El Paso, TX, 2010–2014.
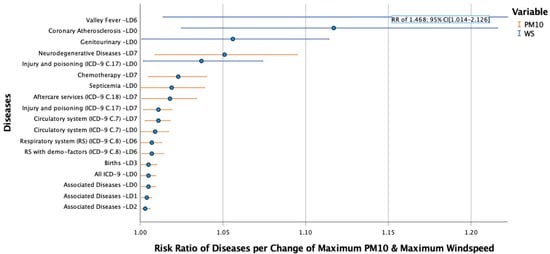
Figure 4.
Risk ratios after dust exposures defined by daily 100 µg/m3 increase in maximum hourly PM10 or daily 4.5 m/s increase in maximum wind speed with their respective lag days.
The quasi-Poisson regression results with the maximum hourly PM10 concentration and maximum hourly average wind speed, including meteorological variables, estimated population increase or decrease, seasonality, holidays, and weekdays between the diseases, are shown in Table 3 with their respective lag day (LD), relative risk (RR), and 95% confidence interval (CI). The hospitalizations for ND (LD 7), AD (LD 0–2), chemotherapy (LD 7), respiratory diseases (LD 6), births (LD 3), and septicemia (LD 0) were positively correlated (p-values < 0.05) with maximum PM10, and weekday (p < 0.01). The hospitalizations due to chemotherapy (LD 7), AD (LD 0–2), and respiratory diseases (LD 6) decreased in the cold season and holidays compared to hot season and non-holidays (p < 0.01). The hospitalizations due to births (LD 3) decreased during the holidays compared to non-holidays (p < 0.01). Cases of all ICD-9 diseases (LD 0), circulatory system diseases (LD 0 and 7), aftercare services (LD 7), and injury and poisoning (LD 7) were positively correlated (p < 0.05) with maximum PM10 and weekday (p < 0.01) and decreased in the cold season and holidays compared to hot season and non-holidays (p < 0.01); hospitalizations for all ICD-9 diseases decreased on holidays compared to non-holidays (p < 0.01). The hospitalizations for genitourinary diseases (LD 0), Valley fever (LD 6), and coronary atherosclerosis (LD 0) were positively correlated (p < 0.05) with maximum wind speed and weekday (p < 0.01) with exception of Valley fever. The hospital admissions due to coronary atherosclerosis (LD 0) decreased on holidays compared to non-holidays (p < 0.01). Hospitalizations for all ICD-9 categories and injury and poisoning were positively correlated (p < 0.05) with maximum wind speed on LD 0, increased on weekday compared to weekend (p < 0.01), and decreased in the cold season and holidays compared to hot season and non-holidays (p < 0.01).
4. Discussion
Small but significant increases in relative risk for hospitalization for multiple conditions on the day of or within a seven-day period after a dust exposure were found for El Paso County, Texas for the period 2010–2014. Some of the associations were modulated by seasonal and/or day-of-week effects. Lag effects of particulate matter on human health could be the result of the time needed for a human to develop inflammation triggering a disease process after a short-term acute exposure to a pollutant [43,44]. Signs of acute inflammation may take hours or days to accumulate and become severe, depending on the cause, severity of the exposure, body system affected, and individual factors such as co-morbidities. In addition, different kinds of diseases associated with particulate matter exposures in different locations may have clinical manifestations with different severities, affecting time lags of medical attendance [45].
4.1. Associations with Increased PM10
Significant associations with AD (the aggregation of individual diagnostic categories, each causing at least 5% of admissions) were found with increased PM10 on LD 0–2, then becoming non-significant and diminishing, and finally slightly increasing on the 7th day. Significant associations were also found for all ICD-9 category hospitalizations (aggregated) with increased PM10 on LD 0. Rublee et al. [46] analyzed the association between dust storms (defined by National Weather Service storm data, not particulate matter concentrations) and hospital intensive care unit admissions across the United States and also found a significant increase in total ICU admissions on the day of the event (LD 0).
In the case of individual components of AD, septicemia (LD 0), encounter for antineoplastic chemotherapy (LD 7), and births (LD 3) were found to be significantly associated with dust exposure through PM10. In regard to individual ICD-9 categories, aftercare services (LD 7), injury and poisoning (LD 7), respiratory system (LD 6), and circulatory system (LD 0, 7) were found to be significantly associated with dust exposure through PM10. Other individual disease categories did not have a significant association with PM10 increases on the day of or immediately following the exposure. This could be because the associations of individual conditions on day 0 might have been enough to result in an increase in hospitalizations, but not enough to be significant, perhaps because there were too few individual cases in a day.
In El Paso, hospitalizations for respiratory diseases were found to be significantly associated with DE via PM10 on lag day 6. Several other studies found dust, defined variously, to be associated with respiratory-related hospitalizations on slightly shorter lag days. Rublee et al.’s [46] nationwide analysis of dust-ICU admission relationships in the USA based on storm reports found an association with respiratory admissions on LD 0 and LD 5. A study in Taiwan found a significant increase in overall tracheitis (a respiratory disease) hospital admissions on lag days 3 and 5 after Asian dust was advected to the island [47]. In Hong Kong, Tam et al. [28] found a significant increase in emergency hospital admissions for COPD on LD 2 after Asian dust storm episodes, but no significant associations for “any respiratory disease,” pneumonia, or influenza. Saharan dust transported across the Atlantic was associated with significant increases in acute exacerbations of COPD in Miami, Florida from lag days 0 through 15 [48], although that study considered not only hospitalizations but also outpatient and emergency room visits. Alessandrini et al. [49] also found an enhanced effect of the coarse fraction of PM10 on respiratory disease hospitalization (and of PM10 on cerebrovascular hospitalizations) during African dust-affected days in Rome, Italy. However, Asian and African dust exposures in Hong Kong, Taiwan, Miami and Rome tend to be dominated by smaller particles and tend to last for many hours to days, as opposed to the predominantly short-term exposures [4,10] to coarser dust and sand [13] in El Paso. Lai and Cheng [50] found that long-duration (multiple day) Asian dust exposures were associated with the most significant onsets of increases in respiratory hospitalizations. Therefore, those results may not be directly comparable to the morbidity effects of DEs in El Paso County.
Exposure to an increment of 100 μg/m3 of maximum hourly PM10 in El Paso County was associated with significantly increased admissions for births on LD 3. Inflammatory responses may be associated with the onset of labor [51], and Schifano et al. [52] showed a relationship between increases in PM10 and delivery in several European cities. Other studies have shown a relationship between DE during pregnancy and conditions including low birth weight, premature birth, as well to toxemia of pregnancy [53]. An acute DE may cause inflammation which would lead to labor and delivery several days later.
Exposure to an increment of 100 μg/m3 of maximum hourly PM10 was associated with significantly increased risk of patient admission in El Paso County on LD 7 due to encounter for antineoplastic chemotherapy and for aftercare services. Encounters for antineoplastic chemotherapy and aftercare services are based on prior appointments, and lag effects may be explained by patients preferring to delay their hospital visit by one week because of a dusty day.
In El Paso, septicemia hospitalizations were found to be significantly associated with dust exposure through PM10 on the day of the event (LD 0). Relatively few studies appear to have been performed of the association between particulate matter and septicemia. A nationwide study in Spain [54] did show that exposure to higher concentrations of PM10 was associated with a higher risk of hospital admissions for sepsis-related pneumonia.
Exposure to an increment of 100 μg/m3 of maximum hourly PM10 was associated with significantly increased risk of patient admission on LD 7 due to neurodegenerative diseases, circulatory system diseases (LD 0 and 7), and injury and poisoning. These diseases have a common RR graph pattern, a non-significant increase in hospitalization on the day of DE with the curve then lowering non-significantly before showing a significant increase on LD 7. The significant increase in hospitalizations on day 7 could represent the amount of time after a dust exposure required to develop or exacerbate a health problem significant enough to require hospital admission. During a DE, in addition to particulate matter originating in the surrounding Chihuahuan Desert, the atmosphere contains resuspensions of dust from unpaved roads (which could contain combustion by-products, materials from brake, tire and engine wear, etc.), as well as potential resuspensions of soil-associated metals, organic compounds, and other potentially harmful substances previously emitted from several point sources at El Paso [6,11,12]. Wind-deposited dust in El Paso also contains some ultrafine particles [13], which are believed to be most important PM for neurotoxicity because of their biological characteristics and their ability to gain access to the central nervous system [55]. Our finding of a significant increase in hospitalization risk for circulatory system diseases with PM10 increase on lag days 0 and 7 are in accord with Xu et al. [45], who stated that the strongest effects of PM10 exposure on ischemic heart disease were at lag day 0 and lag day 7. A short-term, acute exposure to PM10, after the initial shock, might contribute to the risk of disease or injury aggravation through inflammation that is sufficiently acute to result in hospitalization one week later.
4.2. Associations with Increased Wind Speed
Exposure to maximum hourly average wind speed with increments of 4.5 m/s was associated with significantly increased risk of patients’ admission due to coronary atherosclerosis, genitourinary system diseases (as a component of AD), and injury and poisoning (a component ICD-9 category) on LD 0, and Valley fever on LD 6 (Figure 1). Wind speed, as a variable in itself, has only rarely been investigated for association with hospitalizations. An increase in wind speed was associated with a significant increase in COPD medical consultations at LD 1 in one portion of the German province of Bavaria, but not the other [56]. Takagi et al. [57] performed a meta-analysis of multiple studies which found a significant correlation between increased wind speed and coronary artery disease and suggested some possibilities that could explain their findings. Strong wind in itself can cause falls, vehicular accidents and other events resulting in injuries [58], potentially consistent with the increase in injury and poisoning on lag day 0 defined by wind.
In El Paso, high wind speed indicates the predominance of coarse particles including desert dust and local fugitive dust and can be used as a surrogate variable for PM10 [11]; thus, patients were most likely exposed to higher doses of coarse particulate matter and dust on windy days, and symptoms of coronary atherosclerosis, genitourinary system diseases (as a component of AD), and injury and poisoning (a component ICD-9 category) appeared on the day of the wind exposure. It could be that regardless of PM10 source and concentration, increased wind lifts and disperses particulate matter which may include crystalline silica, metals, organic contaminants, microbes, and other materials causing adverse health effects immediately upon exposure. Fasola et al. [59] found similar results for particulate matter in Pisa and Cascina, Tuscany, Italy, with the strongest effects of PM10 associated with cardiovascular hospitalizations immediately at lag 0 (odds ratio (OR) = 1.137, 95% CI= [1.023–1.264]) from 2011–2015. Genitourinary system conditions have also been found to be associated with coarse particulate matter exposures in other recent studies [60]. In the case of Valley fever, a predominantly respiratory fungal infection, symptoms usually appear at least one week after exposure, but our study showed an association on the 6th day after an exposure to increased wind, which may either represent a prompt development of symptoms or exacerbation of a subclinical infection. Note that respiratory diseases in general also showed a significant association with hospitalization on LD 6 when a dust exposure was defined through PM10. Valley fever had a very small incidence of 44 cases during the study period, which could have led to an inaccurate estimation of the association of a dust exposure with Valley fever hospitalization.
4.3. Weekend, Season, and Holiday Associations
Hospitalizations due to ND (LD 7), AD (LD 0–2), all ICD-9 categories (LD 0), circulatory system disease (LD 0, 7), respiratory system disease (LD 6), births (LD 3), septicemia (LD 0), aftercare services (LD 7), chemotherapy (LD 7) (associated to 100 μg/m3 increase in PM10), genitourinary disease, coronary atherosclerosis (associated to 4.5 m/s increase in max wind speed on LD 0), and injury and poisoning (associated to both increases of wind speed and PM10 on LD 0, 7) increased on weekdays as compared to weekends (p < 0.01). This could be because patients prefer to go to the hospital in El Paso during a weekday more so than during a weekend and because most of the appointments for aftercare services and chemotherapy are during the week.
Hospitalizations due to chemotherapy (LD 7), circulatory system disease (LD 0, 7), births (LD 3), aftercare services (LD 7), all ICD-9 categories (LD 0), AD (LD 0–2) (associated to 100 μg/m3 increase in PM10), coronary atherosclerosis (associated to 4.5 m/s increase in wind speed on LD 0), and injury and poisoning (associated to both increases of wind speed and PM10 on LD 0, 7) decreased in the cold season and holidays compared to in hot season and non-holidays (p < 0.01), thus indicating that there is an increase in hospitalizations during the hot season and non-holidays. Dust events in the hot season may increase these hospitalizations. People in El Paso, acclimated to its hot desert climate, may avoid going to the hospital during the cold season as well as on holidays.
4.4. Limitations
Limitations of the dataset used included that only the principal diagnosis was obtained and considered, which does not indicate pre-existing conditions/comorbidities of the patient. There also is a difference between emergency room (ER) visits and hospital admissions (HAs). These differences may affect the results and interpretation of observed air pollution-health associations. For example, HAs are less frequent than ER visits; HAs may represent more severe events than ER; and the ER may be used for primary care by patients with low income [61]. Additional research should be pursued exploring the effects of PM, wind, and/or dust exposures in El Paso on ER visits.
The limitation of considering the maximum hourly PM10 average value during the day can underestimate the effect of daily hospitalizations, because the daily maximum value describes acute exposures but does not explain chronic exposures/lower-intensity dust exposures which may be happening over much longer periods of time in dust-prone cities. This study does not consider the potential chronic health effects of dust exposures, which will be long-term and may be significant for residents of windy desert cities such as El Paso. Additional research into chronic exposures to geogenic contaminants such as windblown desert dust, involving close cooperation between Earth scientists, toxicologists, and epidemiologists, is needed throughout the globe [62]: additional research should be pursued exploring the effects of longer-term exposures to dust and PM in El Paso.
Although we were able to identify a pattern of association between neurodegenerative diseases and dust exposure, we did not find an association with mental illness. Several other recent studies have found significant increases in hospitalizations for mental disorders associated with increased concentrations of PM10 and coarse particles [63,64], as would be most elevated in dust events. Persons experiencing symptoms consistent with neurodegenerative or mental conditions, especially anxiety and depression, often have their disorder go unrecognized, because they do not explain their psychological symptoms explicitly and because they commonly consult their primary physician and/or mental health provider instead of going to the hospital [65,66]. In addition, ~50% of people with depression never consult a health care provider, 95% never enter secondary mental health services, and many more are unrecognized and untreated [67]. Consultations with mental health providers, rather than hospitalizations, may more accurately capture mental health associations with dust exposure.
5. Conclusions
Dust exposures were positively associated with hospitalizations for a variety of conditions in El Paso County, Texas between 2010 and 2014 at various lag periods from the day of exposure to seven days thereafter. From highest to lowest risk, these conditions included Valley fever, coronary atherosclerosis, genitourinary diseases, neurodegenerative diseases, injury and poisoning, chemotherapy, septicemia, aftercare services, circulatory system diseases, injury and poisoning, respiratory system diseases, Associated Diseases, births, and all ICD-9 categories considered together. Valley fever had the highest hospitalization risk (RR of 1.468), though the lowest number of cases: it is known to have a direct relationship with Coccidioides fungus in the soil and exposure from airborne dust [15]. The second-highest association was with coronary atherosclerosis, followed by genitourinary diseases and neurodegenerative diseases. Associated Diseases, representing in aggregate the most common causes of hospital admission in El Paso (births, respiratory system diseases, asthma, circulatory system diseases, digestive system diseases, genitourinary diseases, chemotherapy, septicemia, other chest pain, dehydration, cellulitis and abscess of leg, osteoarthrosis, diabetes mellitus, and mental disorders) and all ICD-9 categories considered together showed associations at lag 0 (and lag 1–2 for AD), with a low RR (1.005); these associations could be due to a subtle effect that shows up as a result of the aggregations but not for individual diagnoses, yet they were still significant and demonstrate some short-term association of hospitalizations, broadly considered, with dust exposure in El Paso.
These findings have important implications because ~92% of the world’s population resides in areas where particulate matter concentrations are greater than the WHO guidelines, and about 41% of the world’s population resides in drylands [68]; therefore, the association between dust events and disease cannot be ignored. Poor people in global drylands, where dust events are most prevalent, are numerous and particularly vulnerable to their adverse effects [69]. About half of all dryland inhabitants on Earth are poor, on the order of a billion people in total, and they have been dubbed the “forgotten billion” because they have habitually been neglected in development processes [69].
Public policies and individual actions are essential to reduce the human health effects of dust events. Since dust events in El Paso appear to be largely originated from wind erosion of natural desert landforms in large, remote portions of the Chihuahuan Desert (Figure 1) [2,5,8,9,10], physical dust control measures within the urban area will not stop DEs. Individual actions to reduce dust exposure could be accomplished by avoiding exertion and outdoor activities during a DE and wearing protective equipment that is sufficient to reduce dust exposure on days with increased particulate matter counts or wind speed, even inside a building [70]. In El Paso County, forecasts and warnings/advisories for dust weather are provided by the USA National Weather Service office [71] and disseminated to the public as well as local authorities and emergency managers. The TCEQ also issues daily air quality forecasts and statements for the public and stakeholders and includes advisories for when PM10 and PM2.5 levels from dust are expected to be elevated and/or cause health concerns [72]. Given the associations between dust events and hospitalizations, individuals, public agencies such as school districts, and employers (especially of outdoor workers) should pay close heed to them. The efficacy of these advisories should be investigated.
The findings of this study have multiple implications for future research on dust exposures and health. A future study could consider both ED visits and HA, along with mortality, as well as both PM2.5 and PM10 during dust event days, in order to perform comparisons of potential similarities or differences to other investigations and to have a broader examination of dust exposure associations with health in the El Paso/ Ciudad Juarez area. It is also advisable to consider a way to capture information about acute exposures occurring over even shorter periods of time than an hour, in order to estimate the immediate health effects that coarse PM could be causing. Additional investigations of these kinds should also be pursued in other dust-prone desert cities, in order to determine potential geographic variability in the health effects of dust exposures.
In many societies, income and other socio-economic factors may be determinant factors for a person to seek hospitalization for a medical condition. Families with high income are more likely to take their children to the doctor or keep them at home on highly polluted days [73]. Collins et al. [74] have demonstrated how ethnicity, class, gender, and age status amplify health risks from air toxics in El Paso, a majority Hispanic community, and Grineski et al. [27] indicated that the strongest respiratory health effects associated with dust events in El Paso were among children, especially girls, and low-income adults. With this in mind, we plan to evaluate how age, socio-economic status, and education level may modulate the health effects of dust exposure in El Paso County.
Author Contributions
Conceptualization, E.H.-M. and T.E.G.; methodology, E.H.-M., T.E.G., G.I.-M. and S.J.; validation, E.H.-M., T.E.G., G.I.-M. and S.J.; formal analysis, S.J.; investigation, E.H.-M.; writing—original draft preparation, E.H.-M.; writing—review and editing, T.E.G., E.H.-M., G.I.-M. and S.J.; supervision, T.E.G., G.I.-M. and S.J.; project administration, T.E.G. and G.I.-M.; funding acquisition, E.H.-M. and T.E.G. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by support to the first author from the Environmental Science and Engineering Program and the Graduate School at The University of Texas at El Paso and a dissertation scholarship from the Society of Hispanic Professional Engineers; and support to the second author by the National Oceanic and Atmospheric Administration, Office of Education—Educational Partnership Program under Agreement No. NA16SEC4810006. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the U.S. Department of Commerce, National Oceanic and Atmospheric Administration. The funding sources had no role in designing or conducting the study or preparing the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approval was obtained from the Institutional Review Board of the University of Texas at El Paso with permit #00001224.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data of the Texas Hospital Inpatient Discharge Research Data File are not publicly available because they belong to the Texas Department of State Health Services (TDSHS), Center for Health Statistics, Austin, Texas. Data on meteorological and particulate matter variables are publicly available online from the Texas Commission on Environmental Quality at https://www.tceq.texas.gov/cgi-bin/compliance/monops/daily_summary.pl (accessed on 25 October 2021). Statistical analyses based on these data are available at doi:10.17632/rrd36wdngb.1.
Acknowledgments
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kok, J.F.; Parteli, E.J.R.; Michaels, T.I.; Bou Karam, D. The physics of wind-blown sand and dust. Rep. Prog. Phys. 2012, 75, 106901. [Google Scholar] [CrossRef] [PubMed]
- Prospero, J.M.; Ginoux, P.; Torres, O.; Nicholson, S.E.; Gill, T.E. Environmental characterization of global sources of atmospheric soil dust identified with the Nimbus-7 total ozone mapping spectrometer (TOMS) absorbing aerosol product. Rev. Geophys. 2002, 40, 1002. [Google Scholar] [CrossRef]
- Ginoux, P.; Prospero, J.M.; Gill, T.E.; Hsu, N.C.; Zhao, M. Global-scale attribution of anthropogenic and natural dust sources and their emission rates based on MODIS Deep Blue aerosol products. Rev. Geophys. 2012, 50, RG3005. [Google Scholar] [CrossRef]
- Novlan, D.J.; Hardiman, M.; Gill, T.E. A Synoptic Climatology of Blowing Dust Events in El Paso, Texas from 1932–2005. In Proceedings of the 16th Symposium on Applied Climatology, San Antonio, TX, USA, 14–18 January 2007; American Meteorological Society: Boston, MA, USA, 2007. [Google Scholar]
- Rivera Rivera, N.I.; Gill, T.E.; Bleiweiss, M.P.; Hand, J.L. Source characteristics of hazardous Chihuahuan Desert dust outbreaks. Atmos. Environ. 2010, 44, 2457–2468. [Google Scholar] [CrossRef]
- Li, W.-W.; Orquiz, R.; Garcia, J.H.; Espino, T.; Pingitore, N.E.; Gardea-Torresdey, J.; Watson, J.G. Analysis of temporal and spatial dichotomous PM air samples in the El Paso-Cd. Juarez air quality basin. J. Air Waste Manag. Assoc. 2001, 51, 1551–1560. [Google Scholar] [CrossRef]
- Kavouras, I.G.; DuBois, D.W.; Nikolich, G.; Corral Avittia, A.Y.; Etyemezian, V. Particulate dust emission factors from unpaved roads in the U.S.-Mexico border semi-arid region. J. Arid Environ. 2016, 124, 189–192. [Google Scholar] [CrossRef]
- Baddock, M.C.; Gill, T.E.; Bullard, J.E.; Dominguez Acosta, M.; Rivera Rivera, N.I. Geomorphology of the Chihuahuan Desert based on potential dust emissions. J. Maps 2011, 7, 249–259. [Google Scholar] [CrossRef]
- Kandakji, T.; Gill, T.E.; Lee, J.A. Drought and land use/land cover impact on dust sources in Southern Great Plains and Chihuahuan Desert of the US: Inferring anthropogenic effect. Sci. Total Environ. 2021, 755, 142461. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.A.; Gill, T.E.; Mulligan, K.R.; Dominguez Acosta, M.; Perez, A.E. Land use/land cover and point sources of the 15 December 2003 dust storm in southwestern North America. Geomorphology 2009, 105, 18–27. [Google Scholar] [CrossRef]
- Staniswalis, J.G.; Parks, N.J.; Bader, J.O.; Muñoz-Maldonado, Y. Temporal Analysis of Airborne Particulate Matter Reveals a Dose-Rate Effect on Mortality in El Paso: Indications of Differential Toxicity for Different Particle Mixtures. J. Air Waste Manag. Assoc. 2005, 55, 893–902. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Pelt, R.S.; Shekhter, E.G.; Barnes, M.A.; Duke, S.E.; Gill, T.E.; Pannell, K.H. Spatial and temporal patterns of heavy metal deposition resulting from a smelter in El Paso, Texas. J. Geochem. Explor. 2020, 210, 106414. [Google Scholar] [CrossRef]
- Rivas, J.A. Dust Storms and the Dispersal of Aquatic Invertebrates in the Chihuahuan Desert Ecoregion. Ph.D. Thesis, University of Texas at El Paso, El Paso, TX, USA, 2019. Available online: https://scholarworks.utep.edu/dissertations/AAI27667795 (accessed on 25 October 2021).
- Ghio, A.J. Particle exposures and infections. Infection 2014, 42, 459–467. [Google Scholar] [CrossRef]
- Tong, D.Q.; Wang, J.; Gill, T.E.; Lei, H.; Wang, B. Intensified dust storm activity and Valley fever infection in the southwestern United States. Geophys. Res. Lett. 2017, 44, 4304–4312. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, M.D.; Calzadilla, A.S.; Salamo, O.; Sharifi, A.; Kumar, N.; Holt, G.; Campos, M.; Mirsaeidi, M. Lung health in era of climate change and dust storms. Environ. Res. 2018, 163, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Qiu, H.; Wang, L.; Duan, Z.; Yu, H.; Deng, R.; Zhan, D.; Zhou, L. Risks of hospital admissions from a spectrum of causes associated with particulate matter pollution. Sci. Total Environ. 2019, 656, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.; Wang, Y.; Williams, C.; Xu, C.; Kartsonaki, C.; Lin, Y.; Zhang, P.; Yin, P.; Lam, K.B.H. The association between high particulate matter pollution and daily cause-specific hospital admissions: A time-series study in Yichang, China. Environ. Sci. Pollut. Res. 2020, 27, 5240–5250. [Google Scholar] [CrossRef] [PubMed]
- Maciejewska, K. Short-term impact of PM2.5, PM10, and PMc on mortality and morbidity in the agglomeration of Warsaw, Poland. Air Qual. Atmos. Health 2020, 13, 659–672. [Google Scholar] [CrossRef]
- Khan, R.K.; Strand, M.A. Road dust and its effect on human health: A literature review. Epidemiol. Health 2018, 40, e2018013. [Google Scholar] [CrossRef]
- Morman, S.A.; Plumlee, G.S. Dust and human health. In Mineral Dust: A Key Player in The Earth System; Knippertz, P., Stuut, J.B.W., Eds.; Springer: Dordrecht, The Netherlands, 2014; pp. 385–409. [Google Scholar]
- Qiu, H.; Wang, L.; Zhou, L.; Pan, J. Coarse particles (PM2.5-10) and cause-specific hospitalizations in southwestern China: Association, attributable risk and economic costs. Environ. Res. 2020, 190, 110004. [Google Scholar] [CrossRef]
- Al-Taiar, A.; Thalib, L. Short-term effect of dust storms on the risk of mortality due to respiratory, cardiovascular and all-causes in Kuwait. Int. J. Biometeorol. 2014, 58, 69–77. [Google Scholar] [CrossRef]
- Wang, Y.C.; Lin, Y.K. Mortality associated with particulate concentration and Asian dust storms in Metropolitan Taipei. Atmos. Environ. 2015, 117, 32–40. [Google Scholar] [CrossRef]
- Shahsavani, A.; Tobías, A.; Querol, X.; Stafoggia, M.; Abdolshahnejad, M.; Mayvaneh, F.; Guo, Y.; Hadei, M.; Hashemi, S.S.; Khosravi, A.; et al. Short-term effects of particulate matter during desert and non-desert dust days on mortality in Iran. Environ. Int. 2020, 134, 105299. [Google Scholar] [CrossRef] [PubMed]
- Domínguez-Rodríguez, A.; Báez-Ferrer, N.; Abreu-González, P.; Rodríguez, S.; Díaz, R.; Avanzas, P.; Hernández-Vaquero, D. Impact of Desert Dust Events on the Cardiovascular Disease: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 727. [Google Scholar] [CrossRef]
- Grineski, S.E.; Staniswalis, J.G.; Bulathsinhala, P.; Peng, Y.; Gill, T.E. Hospital admissions for asthma and acute bronchitis in El Paso, Texas: Do age, sex, and insurance status modify the effects of dust and low wind events? Environ. Res. 2011, 111, 1148–1155. [Google Scholar] [CrossRef]
- Tam, W.W.; Wong, T.W.; Wong, A.H.; Hui, D.S. Effect of dust storm events on daily emergency admissions for respiratory diseases. Respirology 2012, 17, 143–148. [Google Scholar] [CrossRef]
- Chan, Y.S.; Teng, J.C.Y.; Liu, T.C.; Peng, Y.I. Asian dust storms and diabetes hospitalization: A nationwide population-based study. Air Qual. Atmos. Health 2018, 11, 1243–1250. [Google Scholar] [CrossRef]
- Badeenezhad, A.; Baghapour, M.A.; Sorooshian, A.; Keshavarz, M.; Azhdarpoor, A.; Goudarzi, G.; Hoseini, M. Investigating the relationship between central nervous system biomarkers and short-term exposure to PM10-bound metals during dust storms. Atmos. Pollut. Res. 2020, 11, 2022–2029. [Google Scholar] [CrossRef]
- Zhang, X.; Zhao, L.; Tong, D.; Wu, G.; Dan, M.; Teng, B. A Systematic Review of Global Desert Dust and Associated Human Health Effects. Atmosphere 2016, 7, 158. [Google Scholar] [CrossRef]
- Li, J.; Kandakji, T.; Lee, J.A.; Tatarko, J.; Blackwell, J.; Gill, T.E.; Collins, J.D. Blowing dust and highway safety in the southwestern United States: Characteristics of dust emission “hotspots” and management implications. Sci. Total Environ. 2018, 621, 1023–1032. [Google Scholar] [CrossRef]
- Rodopoulou, S.; Chalbot, M.C.; Samoli, E.; DuBois, D.W.; San Filippo, B.D.; Kavouras, I.G. Air pollution and hospital emergency room and admissions for cardiovascular and respiratory diseases in Doña Ana County, New Mexico. Environ. Res. 2014, 129, 39–46. [Google Scholar] [CrossRef]
- Al-Hemoud, A.; Al-Dousari, A.; Al-Shatti, A.; Al-Khayat, A.; Behbehani, W.; Malak, M. Health Impact Assessment Associated with Exposure to PM10 and Dust Storms in Kuwait. Atmosphere 2018, 9, 6. [Google Scholar] [CrossRef]
- Khaniabadi, Y.O.; Daryanoosh, S.M.; Amrane, A.; Polosa, R.; Hopke, P.K.; Goudarzi, G.; Mohammadi, M.J.; Sicard, P.; Armin, H. Impact of Middle Eastern Dust Storms on Human Health. Atmos. Pollut. Res. 2017, 8, 606–613. [Google Scholar] [CrossRef]
- Ueda, K.; Nitta, H.; Odajima, H. The effects of weather, air pollutants, and Asian dust on hospitalization for asthma in Fukuoka. Environ. Health Prev. Med. 2010, 15, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Liu, T.C.; Keller, J.; Lin, H.C. Asian dust storm events are associated with an acute increase in stroke hospitalisation. J. Epidemiol. Community Health 2013, 67, 125–131. [Google Scholar] [CrossRef]
- Merrifield, A.; Schindeler, S.; Jalaludin, B.; Smith, W. Health effects of the September 2009 dust storm in Sydney, Australia: Did emergency department visits and hospital admissions increase? Environ. Health 2013, 12, 1–7. [Google Scholar] [CrossRef]
- Leys, J.F.; Heidenreich, S.K.; Strong, C.L.; McTainsh, G.H.; Quigley, S. PM10 concentrations and mass transport during “Red Dawn”–Sydney 23 September 2009. Aeolian Res. 2011, 3, 327–342. [Google Scholar] [CrossRef]
- American Hospital Association; American Medical Record Association; Health Care Financing Administration; National Center for Health Statistics. ICD-9-CM coding and reporting official guidelines. J. Am. Med Rec. Assoc. 1990, 61, 1–17. [Google Scholar]
- Meng, Z.; Lu, B. Dust events as a risk factor for daily hospitalization for respiratory and cardiovascular diseases in Minqin, China. Atmos. Environ. 2007, 41, 7048–7058. [Google Scholar] [CrossRef]
- Touloumi, G.; Atkinson, R.; Le Tertre, A.; Samoli, E.; Schwartz, J.; Schindler, C. Analysis of health outcome time series data in epidemiological studies. Environmetrics 2004, 15, 101–117. [Google Scholar] [CrossRef]
- Santos, U.P.; Terra-Filho, M.; Lin, C.A.; Pereira, L.A.; Vieira, T.C.; Saldiva, P.H.; Braga, A.L. Cardiac arrhythmia emergency room visits and environmental air pollution in Sao Paulo, Brazil. J. Epidemiol. Community Health 2008, 62, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ma, Y.; Feng, F.; Cheng, B.; Wang, H.; Shen, J.; Jiao, H. Association between PM10 and specific circulatory system diseases in China. Sci. Rep. 2021, 11, 12129. [Google Scholar] [CrossRef] [PubMed]
- Xu, A.; Mu, Z.; Jiang, B.; Wang, W.; Yu, H.; Zhang, L.; Li, J. Acute Effects of Particulate Air Pollution on Ischemic Heart Disease Hospitalizations in Shanghai, China. Int. J. Environ. Res. Public Health 2017, 14, 168. [Google Scholar] [CrossRef] [PubMed]
- Rublee, C.S.; Sorensen, C.J.; Lemery, J.; Wade, T.J.; Sams, E.A.; Hilborn, E.D.; Crooks, J.L. Associations Between Dust Storms and Intensive Care Admissions in the United States, 2000–2015. Geohealth 2020, 4, e2020GH000260. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.S.; Chan, Y.S.; Liu, T.C. Tracheitis hospital admissions are associated with Asia dust storm. Int. J. Environ. Health Res. 2021. [Google Scholar] [CrossRef]
- Gutierrez, M.P.; Zuidema, P.; Mirsaeidi, M.; Campos, M.; Kumar, N. Association between African Dust Transport and Acute Exacerbations of COPD in Miami. J. Clin. Med. 2020, 9, 2496. [Google Scholar] [CrossRef]
- Allessandrini, E.R.; Stafoggia, M.; Faustini, A.; Gobbi, G.P.; Forastiere, F. Saharan dust and the association between particulate matter and hospitalizations in Rome, Italy. Occup. Environ. Med. 2013, 70, 432–434. [Google Scholar] [CrossRef]
- Lai, L.W.; Cheng, W.L. The impact of air quality on respiratory admissions during Asian dust storm periods. Int. J. Environ. Health Res. 2008, 18, 429–450. [Google Scholar] [CrossRef]
- Golightly, E.; Jabbour, H.N.; Norman, J.E. Endocrine immune interactions in human parturition. Mol. Cell. Endocrinol. 2011, 335, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Schifano, P.; Asta, F.; Dadvand, P.; Davoli, M.; Basagana, X.; Michelozzi, P. Heat and air pollution exposure as triggers of delivery: A survival analysis of population-based pregnancy cohorts in Rome and Barcelona. Environ. Int. 2016, 88, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Kelley, M.C.; Ardon-Dryer, K. Analyzing two decades of dust events on the Southern Great Plains region of West Texas. Atmos. Pollut. Res. 2021, 12, 101091. [Google Scholar] [CrossRef]
- Álvaro-Meca, A.; Sánchez-López, A.; Resino, R.; Tamayo, E.; Resino, S. Environmental factors are associated with hospital admissions for sepsis-related pneumonia: A bidirectional case-crossover design. Environ. Res. 2020, 191, 110102. [Google Scholar] [CrossRef]
- Costa, L.G.; Cole, T.B.; Dao, K.; Chang, Y.C.; Coburn, J.; Garrick, J.M. Effects of air pollution on the nervous system and its possible role in neurodevelopmental and neurodegenerative disorders. Pharmacol. Ther. 2020, 210, 107523. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, U.; Exner, T.; Wanka, E.R.; Bergemann, C.; Meyer-Arnek, J.; Hildenbrand, B.; Tufman, A.; Heumann, C.; Huber, R.M.; Bittner, M.; et al. Influence of air pressure, humidity, solar radiation, temperature, and wind speed on ambulatory visits due to chronic obstructive pulmonary disease in Bavaria, Germany. Int. J. Biometeorol. 2012, 56, 137–143. [Google Scholar] [CrossRef]
- Takagi, H.; Hari, Y.; Nakashima, K.; Kuno, T.; Ando, T. Wind and coronary artery disease. Eur. J. Prev. Cardiol. 2020, 27, 2259–2263. [Google Scholar] [CrossRef] [PubMed]
- Goldman, A.; Eggen, B.; Golding, B.; Murray, V. The health impacts of windstorms: A systematic literature review. Public Health 2014, 128, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Fasola, S.; Maio, S.; Baldacci, S.; La Grutta, S.; Ferrante, G.; Forastiere, F.; Stafoggia, M.; Gariazzo, C.; Silibello, C.; Carlino, G.; et al. Short-Term Effects of Air Pollution on Cardiovascular Hospitalizations in the Pisan Longitudinal Study. Int. J. Environ. Res. Public Health 2021, 18, 1164. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.R.; Chen, Y.M.; Chen, S.Y.; Chan, C.C. Associations between long-term particulate matter exposure and adult renal function in the Taipei metropolis. Environ. Health Perspect. 2017, 125, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Winquist, A.; Klein, M.; Tolbert, P.; Flanders, W.D.; Hess, J.; Sarnat, S.E. Comparison of emergency department and hospital admissions data for air pollution time-series studies. Environ. Health 2020, 11, 70. [Google Scholar] [CrossRef]
- Bundschuh, J.; Maity, J.P.; Mushtaq, S.; Vithanage, M.; Seneweera, S.; Schneider, J.; Bhattacharya, P.; Islam Khan, N.; Hamawand, I.; Guilherme, L.R.G.; et al. Medical geology in the framework of the sustainable development goals. Sci. Total Environ. 2017, 581, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Xu, Q.; Guo, X.H.; Fan, H.; Zhu, H. Particulate matter air pollution associated with hospital admissions for mental disorders: A time-series study in Beijing, China. Eur. Psychiatry 2017, 44, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Zhu, X.; Wang, L.; Pan, J.; Pu, X.; Zeng, X.; Zhang, L.; Peng, Z.; Zhou, L. Attributable risk of hospital admissions for overall and specific mental disorders due to particulate matter pollution: A time-series study in Chengdu, China. Environ. Res. 2019, 170, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, J.; McLeod, D.; Dowell, A. Do patients want to disclose psychological problems to GPs? Fam. Pract. 2005, 22, 631–637. [Google Scholar] [CrossRef]
- Tylee, A.; Walters, P. Under-recognition of anxiety and mood disorders in primary care: Why does the problem exist and what can be done? J. Clin. Psychiatry 2007, 68, 27–30. [Google Scholar] [PubMed]
- National Institute for Health and Care Excellence, UK (NICE). Depression in Adults: Recognition and Management. 2009. Available online: https://guidance.nice.org.uk/CG90 (accessed on 25 October 2021).
- World Health Organization (WHO). Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease. 2016. Available online: https://apps.who.int/iris/handle/10665/250141 (accessed on 25 October 2021).
- Middleton, N.; Kang, U. Sand and dust storms: Impact mitigation. Sustainability 2017, 9, 1053. [Google Scholar] [CrossRef]
- Middleton, N. Health in dust belt cities and beyond—An essay by Nick Middleton. BMJ 2020, 371, m3089. [Google Scholar] [CrossRef]
- National Weather Service. National Weather Service El Paso Weather Forecast Office. 2021. Available online: https://www.weather.gov/epz (accessed on 25 October 2021).
- Texas Commission on Environmental Quality. Today’s Texas Air Quality Forecast. 2021. Available online: https://www.tceq.texas.gov/airquality (accessed on 25 October 2021).
- Hofflinger, A.; Boso, A. Another one breathes the dust. The relation between severe air pollution episodes and school attendance in southern Chile. Local Environ. 2021, 26, 252–263. [Google Scholar] [CrossRef]
- Collins, T.W.; Grineski, S.E.; Chakraborty, J.; McDonald, Y.J. Understanding environmental health inequalities through comparative intracategorical analysis: Racial/ethnic disparities in cancer risks from air toxics in El Paso County, Texas. Health Place 2011, 17, 335–344. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).