Abstract
Climate change and obesity were considered threats to our planet long before the onset of COVID-19. The recent pandemic has enhanced the global burden of both pre-existing crises. The aim of this narrative review is to explore the interaction between the three concurrent crises and the future of our planet should they not be dealt with accordingly. A PubMed and Google Scholar literature search was performed using different combinations of search strategies and using the keywords “obesity”, “climate/temperature change”, “cold/hot temperatures”, and “COVID-19”. High global greenhouse gas (GHG) emissions link obesity and climate change as a result of the interplay between biological and behavioural factors. COVID-19 mitigation measures have indirectly impacted obesity and GHG emissions through the shift in dietary habits, restricted mobility, the impact on healthcare services, and enhanced psychological stress. Furthermore, COVID-19 has a more detrimental effect if acquired by an obese individual, with a higher chance of hospitalization and mechanical ventilation. This leads to higher GHG emissions and negative repercussions on the climate. A tri-directional relationship exists between obesity, climate change, and COVID-19. Various factors contribute to this relationship, but unless urgent global integrated action plans are implemented that target all three calamities, and not just COVID-19, a devastating and unsustainable future may ensue.
1. Introduction
The 21st century has been challenged by two global issues: climate change and obesity. Obesity has long been considered a global pandemic; however, climate change may also be considered a pandemic due to its extensive effects on the health of the human race and the ecosystems we rely on, pertaining to global health [1]. Climate change, however, is not referred to as a pandemic within this paper in order to stick more closely to the classical definitions of ‘epidemic’ and ‘pandemic’ found within the Fourth Edition of A Dictionary of Epidemiology [2].
The effects of climate change were first reported in the late 1950s, as the mean temperature started to rise gradually [3]. This change led to several detrimental effects including desertification, soil degradation, agricultural productivity loss, and others [4]. One of the major contributing factors to climate change is the rising level of GHG emissions, the byproducts of fossil fuel usage [5].
Obesity has been a global crisis for decades, with the World Health Organization declaring it an epidemic in 1997 [6]. Since then, obesity has been a leading health challenge across all continents [7]. Indeed, recently, in March 2021, the European Commission additionally defined obesity as being a chronic disease with potential negative consequences [8]. It has been projected that by the year 2050 the prevalence of obesity will increase, with 18% of men and 21% of women becoming obese worldwide [9]. The link between obesity and climate change is attributed to several factors. Greater metabolic demands, increased food intake, and greater transportation needs are all factors associated with obesity. They are linked to an approximate 20% increase in GHG emissions when compared with normal weight status [10].
It is estimated that the current global burden of obesity causes an excess of around 700 megatons of carbon dioxide-equivalent emissions every year. This equates to circa 1.6% of all global emissions [11]. Replacing physical activity with fossil-fuel-powered modes of transportation as well as sedentary leisure activities is associated with an increased risk of obesity as well as an increased risk of damage to the environment [12]. Increased consumption of processed, energy-dense food further compounds this issue [12]. Recent research argues that obesity is both a result of and a complication of climate change. Excessive consumption of meat and products that are animal-sourced precipitates issues in terms of the incidence of obesity as well as environmental issues, as it is known that pastoral farming is the main contributor to high GHG emissions in the agricultural sector [13].
The year 2020 saw another major epidemic challenge the world, as the novel coronavirus, SARS-CoV-2, emerged. Governments around the world instituted several preventive measures to contain viral spread. These included lockdowns, closure of schools and the halting of leisure activities, among others [14]. Although this period led to a global reduction in transportation and hence theoretically reduced GHG emissions, climate change was still predicted to have been exacerbated through increased food consumption, change in the type of food consumed, and increased sedentary periods [15,16,17]. However, considering that both climate change and the COVID-19 pandemic are still fluid issues, the true impact of both of these global challenges and their interactions is still unknown.
Therefore, it is anticipated that the world is not facing three separate crises (climate change, obesity, and COVID-19) but rather three interconnected issues of great calamity. The aim of this narrative review is to explore the various interactions between these three concerning concurrent, global issues and the inauspicious future that will befall our planet unless urgent action is taken.
2. Materials and Methods
Climate change is the slow and long-term shift of meteorological variables or parameters resulting in temperature changes [18]. For the purposes of this review, extreme types of weather have been considered to reflect our planet’s future predicament should no urgent action be taken.
A literature search though PubMed and Google Scholar was conducted using the following keyword strategies: “obesity” AND “climate change” AND/OR “COVID-19”; “obesity” AND “temperature change” AND/OR “COVID-19”; “obesity” AND “temperature rise” AND/OR “COVID-19”; “obesity” AND “hot temperature” AND/OR “COVID-19”; “obesity” AND “extreme temperature” AND/OR “COVID-19”; “obesity” AND “low temperature” AND/OR “COVID-19”; “obesity” AND “cold temperature” AND/OR “COVID-19”; “obesity” AND “extreme cold” AND/OR “COVID-19”.
Only articles with abstracts that fit the aim of this review were considered. Also, only articles published in English were included. Citations within the literature that fell within this study’s aim and objectives were also explored.
3. Results and Discussion
Climate change has resulted in the occurrence of extreme types of weather. Both climate change and extreme weather have direct and indirect effects on the development of obesity.
3.1. High Temperatures and Obesity
A rise in temperature has been associated with a negative impact on agricultural production, resulting in scarce fresh produce. A healthy diet revolves around the availability of fresh fruit and vegetables. A scarce supply of this fresh produce will inevitably lead to an increase in selling price and thus, food insecurity [9]. A dietary shift to less expensive processed and imported foods is more likely to occur, along with increased production of processed food. GHG emission levels will consequently rise as carbon-intensive production from industries increases as well as food transportation, retail processing, and storage demands [19]. Processed food is known to be energy-dense with high levels of salt, sugars, and fat [20,21,22,23,24]. Regular consumption of such food can lead to the development of a number of non-communicable diseases including obesity [25,26]. Of note, the occurrence of non-communicable diseases increases the burden on healthcare systems as well as hospitalizations [27,28]. It was noted that individuals with non-communicable diseases contributed to a quarter of emergency admissions in the UK. Consequently, this results in higher GHG emissions by the hospital infrastructure [28,29]. In 2016, the global carbon footprint of healthcare was estimated at 4–6% of all emissions [30]. In fact, hospitals and laboratories were found to emit 4.4% of the world’s GHGs and were found to be responsible for more than five million tons of waste each year [31].
Furthermore, as an individual’s body weight increases, a higher metabolism and greater energy cost for moving is required [32]. This results in enhanced daily energy expenditure and gives rise to higher food consumption, which further increases food production and, consequently, GHG emissions [10,33,34,35]. In addition, obesity also increases GHG emissions related to transportation. Transportation of heavier cargo results in increased use of cargo fuel [36]. Thus, transportation of heavier passengers is thought to increase GHG emissions [37]. Indeed, when investigating the global impact of obesity on GHG emissions, Magkos et al. estimated that obesity is associated with an approximate 20% increase in GHG emissions, compared with those emitted with a normal-weight state. This is equivalent to approximately 49 megatons per year CO2eq due to increased metabolic demands, 361 megatons per year CO2eq from food production due to increased intake, and 290 megatons per year CO2eq from transportation due to increased weight, or 1.6% of global GHG emissions per year [10]. Thus, climate change may be said to be exacerbated by obesity.
High temperatures also affect the level of physical activity performed by individuals. Physical activity includes both recreational activity and physical transportation, e.g., walking for errands. A lack of both types of physical activity leads to a sedentary lifestyle, with increased fuel-powered transportation resulting in enhanced GHG emissions and a higher risk of obesity [19].
3.2. Low Temperatures and Obesity
Climate change is mostly associated with a gradual increase in temperature; however, recent anomalous activity occurring in the pan-Arctic regions included low temperature spells and harsher winters over certain regions, especially in the United States (US) [38,39]. Cold temperatures have a physiological impact on the human body as they induce appetite in order to generate and conserve body heat [40]. Cold conditions are likely to reduce physical activity as individuals delay exercising if it is perceived to be too cold [41]. Cold temperatures also deter individuals from going outdoors, resulting in more time spent indoors, thus increasing the opportunity for snacking and sedentary behaviour [42,43]. This predisposes to an increase in adipose tissue with the risk of developing obesity [44]. Increased food production and transportation use consequently occur. This leads to increased GHG emissions and has a direct effect on climate change [19]. Extreme cold temperatures might also have negative implications for agriculture and fresh food production, which enhances the effects of climate change. Therefore, the susceptibility to obesity is present at both extreme temperatures, with the main driving factors being lifestyle habits. However, behavioural attitudes are further enhanced by climate change.
3.3. COVID-19, Obesity, and Climate Change
3.3.1. Indirect Effects of COVID-19 on Obesity and Climate Change
The novel coronavirus (SARS-CoV-2) caused the global spread of COVID-19 infection, resulting in a pandemic. This led governments across the globe to institute several restrictions to curb the spread of the virus. Lockdowns, closure of schools, social isolation, and postponing routine activities as well as suspending elective healthcare services were some of the restrictions put in place [14]. Although these measures resulted in positive outcomes in terms of controlling the community spread of the virus and redistributing hospital resources to COVID-19 in-patient care, they had detrimental effects on the wellbeing of populations and routine healthcare services [45,46,47]. The predisposition to obesity increased as a result of these measures [48,49]. In addition, the world came to a forced stop during the COVID-19 pandemic, due to mitigation measures put in place by governments to curb the spread of the SARS-CoV-2 virus [50]. Inadvertently, global CO2 emissions decreased by 2300 megatons during 2020, a 6.4% decrease compared with the CO2 emissions released during 2019 [51]. Despite this, the drop in CO2 emissions was only transient, as GHG emission levels were observed to rise quickly, especially once restrictions were lifted [52]. A contributing factor may be the fact that the COVID-19 pandemic brought about an unprecedented increase in medically hazardous waste, which has to be incinerated, increasing the amount of GHGs emitted [53].
Lockdowns led to panic buying of long shelf-life food items, which are typically energy-dense and high in preservatives, salt, sugars, and fat [54]. The consumption of these items is known to predispose to obesity [26]. Stockpiling fresh produce resulted in the depletion of perishable, healthy food such as fruits, vegetables, and meat [54]. A shift to grocery shopping that favoured the consumption of preserved food was observed [55,56]. COVID-19 has also led to a high redundancy rate, imposing financial difficulties on the affected families [57,58]. Such families are more likely to opt for an ultra-processed diet since this type of food tends to be much cheaper than what is considered ‘healthy food’ [59]. This was especially relevant at the time of writing since COVID-19 has decreased the availability of fresh dietary food [60].
It needs to be pointed out that the occurrence of a pandemic along with the various mitigation measures that were instituted also imposed psychological stress on individuals [61]. It is known that during stressful situations, there is a physiological release of glucocorticoids, which are linked to increased consumption of food, especially high-energy food [62]. Therefore, mitigation measures have placed a higher demand on the food industry, which is known to emit copious amounts of GHGs. Lockdowns can therefore be said to have exacerbated climate change.
Climate change itself has various effects on mental health. These include high rates of negative emotions such as guilt, demoralization, and anxiety as well as other psychiatric disorders [63]. The impacts of climate change on mental health may be direct or indirect. An example of a direct impact is heat stress as this may cause a deterioration in cognitive function. Indirect effects include economic loss, the thought of threats to health and wellbeing, and alienation from a degraded environment. All these may have an indirect negative impact on mental health [64]. The release of glucocorticoids as a result of the abovementioned stressors increases appetite and may therefore, if sustained, predispose individuals to the possibility of becoming obese [62].
Childhood obesity gained momentum in the pre-COVID-19 era due to increased sedentary lifestyle and high-calorie food consumption [65]. With the abrupt closure of schools due to COVID-19, children were forced to stay at home. This led to longer screen time, a sedentary lifestyle, the possibility of increased snacking, and a greater intake of processed food [66]. A similar experience was encountered by adults who shifted to remote working. Lockdowns may also have had a negative psychological impact as the isolation imposed on the population (children and adults alike) is known to predispose to snacking and erratic, unhealthy dietary patterns [67,68]. Such habits are associated with increased caloric intake and, therefore, an increased risk of obesity. Furthermore, the closure of gyms and recreational areas and the halting of organized sports decreased accessibility to physical activity, making it difficult for individuals to maintain an active lifestyle [61]. It is thus anticipated that the obesity epidemic will soar across populations unless urgent action is taken. This will also impact the climate change crisis.
Most healthcare services were cancelled or suspended during lockdowns, including obesity management and scheduled bariatric surgeries. This could lead to further disease progression and worsening of associated complications [69]. Delaying both management plans and screening for complications is more likely to result in hospitalization at a later stage with a worse outcome and an increased burden on healthcare systems. Placing an added burden on both healthcare systems and infrastructures is known to be linked with increased GHG emissions which aggravate climate change.
The rapid spread of COVID-19 burdened healthcare systems globally as the limited understanding of this novel virus meant that effective measures could not be put into place immediately. The sudden outbreak put a strain on global supplies of manpower and raw materials. The environmental impacts of the pandemic are yet to be fully understood [70]. Although uncertainty regarding the effects of COVID-19 on the natural environment is still prevalent, should the struggle against the pandemic lead to a persistent global recession, the adoption of clean technology will be threatened. This may outweigh any temporary environmental benefits that may have occurred as a result of the pandemic itself. Policy response will determine whether this occurs [71].
Although the pandemic may be said to have wreaked havoc on a global scale, a few of the new habits adopted by societies around the world may also have helped to curb climate change and obesity, even if only temporarily. For instance, the option of working from home could significantly decrease the need for transportation, resulting in less GHG emissions [72]. It would also decrease the need for new buildings such as offices, the construction of which would otherwise increase GHG emissions [73]. Remote working would also decrease the amount of traffic around cities, resulting in less pollution and less respiratory disease exacerbations [74]. Working from home would also result in increased self-leadership and autonomy, which would allow people to have more time for leisure activities, which could translate into physical activity [75].
3.3.2. Direct Effects of COVID-19 on Obesity and Climate Change
COVID-19 is characterized by pathological acute systemic inflammation with high levels of circulatory proinflammatory cytokines [76]. The pathophysiology of obesity is characterized by a low-grade systemic inflammatory reaction [77]. Hence, if obese individuals acquire COVID-19 infection, there is a higher chance of developing a cytokine storm with an escalated systemic inflammation, which could affect multiple organs [78]. This could potentially be fatal [78]. Indeed, a proportion of the obese population that acquired COVID-19 required hospitalization and mechanical ventilation [79,80]. As already discussed, the increased usage of hospital resources leads to increased GHG emissions.
Of note, extreme cold temperatures, which can be a repercussion of climate change, as discussed above, have been reported to be associated with high rates of SARS-CoV-2 transmission within populations [81]. It is thus anticipated that the obese population is more susceptible to such an infection. This will further aggravate the triple global crisis outcome [81]. Figure 1 provides a summary of both the direct and indirect inter-relationships between the three global crises.
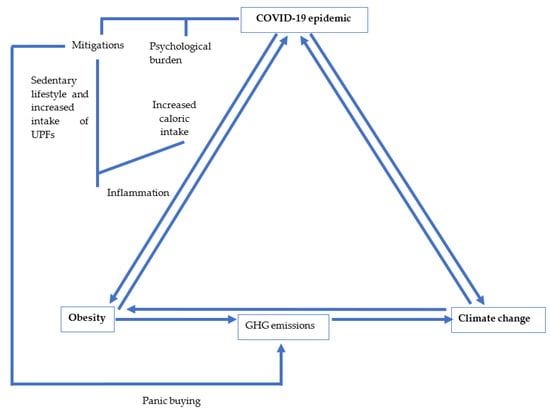
Figure 1.
The interlinked relationships between the three global crises: COVID-19, obesity, and climate change. UPFs—Ultra processed foods.
3.4. Implications for Policy
During these unprecedented times, the two long-standing epidemics (obesity and climate change) should remain a priority in the eyes of policy makers and public health officials. Surveillance for COVID-19 should be carried out simultaneously. Safeguarding the population from COVID-19 infection through timely mitigation measures while encouraging COVID-19 vaccination should continue to be high up on the agenda along with strategies targeting the high-carbon, obesogenic environment, behaviours, and attitudes. Active transport, such as walking or using a bicycle, should be encouraged. This would increase physical activity and reduce GHG emissions related to transport. Such active transport can also help to potentially reduce COVID-19 transmission through transportation modalities. It must be noted that if mask wearing were to be mandated during such activities, it may restrict some individuals from adopting such transportation means, in which case, other forms of physical activity should be encouraged. Indeed, lists of home-based exercises have been made available by the World Health Organization, as well as by other associations, to encourage the population to remain physically active even during restrictions and lockdowns.
A shift to a healthy (fresh and more plant-based) diet should be encouraged, although this calls for different stakeholders to work together to ensure adequate supply and affordability even during precarious periods such as lockdowns. Such dietary availability would hopefully encourage the population to consume less processed food. This could have a tri-factorial benefit regarding the worldwide crises. Over time, this dietary attitude could decrease GHG emissions originating from the food industry and improve body weight. Consequently, should COVID-19 be acquired, a less severe form of COVID-19 infection would be expected. It is important to note that although population knowledge and education are a necessity, it is not always sufficient to simply influence behaviour. Therefore, it is recommended that incentives for leading a healthier lifestyle be implemented. These include subsidizing fresh products and home equipment that would encourage physical activity, among others.
Considering the psychological impact that COVID-19 has had on the population, it is highly recommended that psychological aid should be readily available and accessible to everyone. Such aid will also have an indirect positive effect on obesity and climate change.
Policy makers must also consider the effect that climate change may have on the patterns of pathogens such as COVID-19. If pathogens follow the patterns predicted for other epidemics, it would be logical to expect that some diseases could adapt to the changing environmental conditions brought about by climate change and may thus potentially increase in prevalence. Others, however, may suffer negative repercussions leading to a decreased viral spread and even local extinctions [82].
COVID-19 has provided crucial insight into what could be done to tackle the climate crisis. Governments around the world should keep the climate healthy by reducing the use of GHG-emitting means of transport and invest in innovative solutions to manage medical waste [83]. Indeed, the COVID-19 pandemic has presented world leaders and policy makers with the opportunity to think more strategically. For instance, the COVID-19 pandemic has highlighted issues with global efficiency and equality, which has resulted in many countries restructuring their healthcare facilities. These issues include obesity management, prevention, and screening. In the process, governments can look for innovative ways to decrease waste and emissions [84]. COVID-19 as a global crisis has also reminded humanity to care for the increasingly interdependent and environmentally challenged world that we live in [85].
Governments at all levels may thus take this opportunity to plot a greener, more equitable, and more sustainable course for our future. This can be done by investing in strategies that minimize the risks that arise as a result of climate change as well as the COVID-19 pandemic. Obligations to drastically reduce emissions should be promoted worldwide, in order to achieve sustainable development goals and leave a safe planet for future generations [85].
4. Conclusions
Obesity and climate change have challenged the globe for decades. COVID-19 has imposed an additional stress on our planet as a result of its direct and indirect effects on both pre-existing issues. Indeed, if the COVID-19 virus follows the patterns predicted for other pathogens, it may adapt to the changing environmental conditions and may thus increase in incidence and prevalence. On the other hand, the virus may be unable to adapt to the environmental challenges resulting from climate change. This may lead to a decrease in viral spread or even local extinctions of the virus [82]. The challenge of determining which outcome will apply to COVID-19 lies with modern-day researchers, driving those who endeavour to obtain answers “to strive, to seek to find and not to yield” (Ulysses, Alfred Lord Tennyson).
Policy makers may not yet fully comprehend that the obesity epidemic is a population-wide response to the immense reduction in physical activity as well as the changes in food supply of different countries over the last few decades. These changes are socioeconomically driven, and the health sector will end up shouldering the consequences. Timely action plans to target all three global crises are therefore a must.
Author Contributions
Conceptualization, S.C.; methodology, S.C., E.G., and A.C.; writing—original draft preparation, S.C.; writing—review and editing, E.G. and A.C. All authors have read and agreed to the published version of the manuscript.
Funding
No funding was received.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The global syndemic of obesity, undernutrition, and climate change: The lancet commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Last, J.M. A Dictionary of Epidemiology, 4th ed.; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Houghton, J.T.; Ding, Y.; Griggs, D.J.; Noguer, M.; van der Linden, P.J.; Dai, X.; Maskell, K.; Johnson, C.A. Climate Change 2001: The Scientific Basis Contribution of Working Group I to the Third Assessment Report of the Intergovernmental Panel on Climate Change Published for the Intergovernmental Panel on Climate Change. 2001. Available online: http://www.cambridge.org (accessed on 20 March 2020).
- Rockström, J.; Steffen, W.; Noone, K.; Persson, Å.; Stuart Chapin, F., III; Lambin, E.F.; Lenton, T.M.; Scheffer, M.; Folke, C.; Schellnhuber, H.J.; et al. A safe operating space for humanity. Nature 2009, 461, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Olivier, J.; Janssens-Maenhout, G.; Muntean, M.; Peters, J. Trends in global CO2 Emissions: 2013 Report (PBL Netherlands Environ-Mental Assessment Agency). 2013. Available online: https://www.pbl.nl/en/publications/long-term-trend-in-global-co2-emissions-2011-report (accessed on 20 March 2020).
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Jaacks, L.M.; Vandevijvere, S.; Pan, A.; McGowan, C.; Wallace, C.; Imamura, F.; Mozaffarian, D.; Swinburn, B.; Ezzati, M. The obesity transition: Stages of the global epidemic. Lancet Diabetes Endocrinol. 2019, 7, 231–240. [Google Scholar] [CrossRef]
- Burki, T. European Commission classifies obesity as a chronic disease. Lancet Diabetes Endocrinol. 2021, 9, 418. [Google Scholar] [CrossRef]
- Lobstein, T.; Brinsden, H. Obesity: Missing the 2025 Global Targets. 2020. Available online: www.worldobesity.org (accessed on 19 August 2021).
- Magkos, F.; Tetens, I.; Bügel, S.G.; Felby, C.; Schacht, S.R.; Hill, J.O.; Ravussin, E.; Astrup, A. The environmental foodprint of obesity. Obesity 2019, 28, 73–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Swinburn, B. The obesity and climate change nexus. Obesity 2019, 28, 8. [Google Scholar] [CrossRef] [PubMed]
- Webb, G.J.; Egger, G. Obesity and climate change. Am. J. Lifestyle Med. 2013, 8, 200–204. [Google Scholar] [CrossRef]
- Minos, D.; Butzlaff, I.; Demmler, K.M.; Rischke, R. Economic growth, climate change, and obesity. Curr. Obes. Rep. 2016, 5, 441–448. [Google Scholar] [CrossRef] [Green Version]
- Tabari, P.; Amini, M.; Moghadami, M.; Moosavi, M. International public health responses to COVID-19 outbreak: A rapid review. Iran. J. Med. Sci. 2020, 45, 157–169. [Google Scholar]
- Du, J.; Rakha, H.A.; Filali, F.; Eldardiry, H. COVID-19 pandemic impacts on traffic system delay, fuel consumption and emissions. Int. J. Transp. Sci. Technol. 2021, 10, 184–196. [Google Scholar] [CrossRef]
- Janssen, M.; Chang, B.P.I.; Hristov, H.; Pravst, I.; Profeta, A.; Millard, J. Changes in food consumption during the COVID-19 Pandemic: Analysis of consumer survey data from the first lockdown period in Denmark, Germany, and Slovenia. Front. Nutr. 2021, 8, 635859. [Google Scholar] [CrossRef]
- Amini, H.; Habibi, S.; Islamoglu, A.H.; Isanejad, E.; Uz, C.; Daniyari, H. COVID-19 pandemic-induced physical inactivity: The necessity of updating the Global Action Plan on Physical Activity 2018–2030. Environ. Health Prev. Med. 2021, 26, 1–3. [Google Scholar] [CrossRef]
- National Geographic Society. Climate Change. Natl. Geogr. Soc. 2019. Available online: https://www.nationalgeographic.org/encyclopedia/climate-change/ (accessed on 20 September 2021).
- An, R.; Ji, M.; Zhang, S. Global warming and obesity: A systematic review. Obes. Rev. 2017, 19, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hawk, T.; Aggarwal, A.; Drewnowski, A. Characterizing ultra-processed foods by energy density, nutrient density, and cost. Front. Nutr. 2019, 6, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moubarac, J.-C.; Batal, M.; Louzada, M.L.; Martinez Steele, E.; Monteiro, C.A. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite 2017, 108, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Louzada, M.L.d.C.; Martins, A.P.B.; Canella, D.S.; Baraldi, L.G.; Levy, R.B.; Claro, R.M.; Moubarac, J.-C.; Cannon, G.; Monteiro, C.A. Ultra-processed foods and the nutritional dietary profile in Brazil. Rev. Saude Publica 2015, 49. [Google Scholar] [CrossRef]
- Poti, J.M.; Mendez, M.A.; Ng, S.W.; Popkin, B.M. Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am. J. Clin. Nutr. 2015, 101, 1251–1262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez Steele, E.; Baraldi, L.G.; da Costa Louzada, M.L.; Moubarac, J.-C.; Mozaffarian, D.; Monteiro, C.A. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ Open 2016, 6, e009892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Costa Louzada, M.L.; Baraldi, L.G.; Steele, E.M.; Martins, A.P.B.; Canella, D.S.; Moubarac, J.-C.; Levy, R.B.; Cannon, G.; Afshin, A.; Imamura, F.; et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev. Med. 2015, 81, 9–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, C.A.; Moubarac, J.-C.; Cannon, G.; Ng, S.W.; Popkin, B. Ultra-processed products are becoming dominant in the global food system: Ultra-processed products: Global dominance. Obes. Rev. 2013, 14, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Galdamez, D.H.; González-Block, M.Á.; Romo-Dueñas, D.K.; Lima-Morales, R.; Hernández-Vicente, I.A.; Lumbreras-Guzmán, M.; Méndez-Hernández, P. Increased risk of hospitalization and death in patients with COVID-19 and pre-existing noncommunicable diseases and modifiable risk factors in Mexico. Arch. Med. Res. 2020, 51, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Muka, T.; Imo, D.; Jaspers, L.; Colpani, V.; Chaker, L.; van der Lee, S.; Mendis, S.; Chowdhury, R.; Bramer, W.; Falla, A.; et al. The global impact of non-communicable diseases on healthcare spending and national income: A systematic review. Eur. J. Epidemiology 2015, 30, 251–277. [Google Scholar] [CrossRef] [PubMed]
- Tomson, C. Reducing the carbon footprint of hospital-based care. Futur. Hosp. J. 2015, 2, 57–62. [Google Scholar] [CrossRef]
- Salas, R.N.; Maibach, E.; Pencheon, D.; Watts, N.; Frumkin, H. A pathway to net zero emissions for healthcare. BMJ 2020, 371, m3785. [Google Scholar] [CrossRef] [PubMed]
- Budd, K. Hospitals Race to Save Patients—And the Planet. AAMC. 2019. Available online: https://www.aamc.org/news-insights/hospitals-race-save-patients-and-planet (accessed on 23 September 2021).
- Walpole, S.C.; Prieto-Merino, D.; Edwards, P.; Cleland, J.; Stevens, G.; Roberts, I. The weight of nations: An estimation of adult human biomass. BMC Public Health 2012, 12, 439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pradhan, P.; Reusser, D.E.; Kropp, J. Embodied greenhouse gas emissions in diets. PLoS ONE 2013, 8, e62228. [Google Scholar] [CrossRef] [Green Version]
- Prentice, A.M.; Black, A.E.; Coward, W.A.; Cole, T.J. Energy expenditure in overweight and obese adults in affluent societies: An analysis of 319 doubly-labelled water measurements. Eur. J. Clin. Nutr. 1996, 50, 93–97. [Google Scholar]
- Hiç, C.; Pradhan, P.; Rybski, D.; Kropp, J. Food surplus and its climate burdens. Environ. Sci. Technol. 2016, 50, 4269–4277. [Google Scholar] [CrossRef] [Green Version]
- IPCC. Global Warming of 1.5 °C. Available online: https://www.ipcc.ch/sr15/ (accessed on 19 August 2021).
- Edwards, P.; Roberts, I. Population adiposity and climate change. Int. J. Epidemiology 2009, 38, 1137–1140. [Google Scholar] [CrossRef]
- Kim, J.-S.; Kug, J.-S.; Jeong, S.-J.; Huntzinger, D.N.; Michalak, A.M.; Schwalm, C.; Wei, Y.; Schaefer, K. Reduced North American terrestrial primary productivity linked to anomalous Arctic warming. Nat. Geosci. 2017, 10, 572–576. [Google Scholar] [CrossRef]
- Cohen, J.; Pfeiffer, K.; Francis, J.A. Warm Arctic episodes linked with increased frequency of extreme winter weather in the United States. Nat. Commun. 2018, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Habibzadeh, N. Why Physiologically cold weather can increase obesity rates? Int. Physiol. J. 2018, 2, 11–13. [Google Scholar] [CrossRef]
- Wagner, A.L.; Keusch, F.; Yan, T.; Clarke, P.J. The impact of weather on summer and winter exercise behaviors. J. Sport Health Sci. 2019, 8, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M. The relationship between obesity and seasonal variation in body weight among elementary school children in Tokyo. Econ. Hum. Biol. 2006, 4, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Von Hippel, P.; Benson, R. Obesity and the natural environment across US counties. Am. J. Public Health 2014, 104, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, K.M.; Pereira, M.A.; Jacobs, D.R.; Sidney, S.; Odegaard, A.O. sedentary behavior, physical activity, and abdominal adipose tissue deposition. Med. Sci. Sports Exerc. 2017, 49, 450–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutherland, K.; Chessman, J.; Zhao, J.; Sara, G.; Went, A.; Dyson, S.; Levesque, J.-F. Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Res. Pr. 2020, 30. [Google Scholar] [CrossRef]
- Mercier, G.; Arquizan, C.; Roubille, F. Understanding the effects of COVID-19 on health care and systems. Lancet Public Health 2020, 5, e524. [Google Scholar] [CrossRef]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Jia, P.; Zhang, L.; Yu, W.; Yu, B.; Liu, M.; Zhang, D.; Yang, S. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: The COVID-19 impact on lifestyle change survey (COINLICS). Int. J. Obes. 2021, 45, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Mulugeta, W.; Desalegn, H.; Solomon, S. Impact of the COVID-19 pandemic lockdown on weight status and factors associated with weight gain among adults in Massachusetts. Clin. Obes. 2021, 11, e12453. [Google Scholar] [CrossRef] [PubMed]
- Le Quéré, C.; Jackson, R.B.; Jones, M.W.; Smith, A.; Abernethy, S.; Andrew, R.M.; De-Gol, A.J.; Willis, D.R.; Shan, Y.; Canadell, J.G.; et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat. Clim. Chang. 2020, 10, 647–653. [Google Scholar] [CrossRef]
- Tollefson, J. COVID curbed carbon emissions in 2020—But not by much. Nat. Cell Biol. 2021, 589, 343. [Google Scholar] [CrossRef]
- Carbon Dioxide Levels Continue at Record Levels, Despite COVID-19 Lockdown; The World Meteorological Organization: Geneva, Switzerland, 2020.
- Maalouf, A.; Maalouf, H. Impact of COVID-19 pandemic on medical waste management in Lebanon. Waste Manag. Res. 2021, 39, 45–55. [Google Scholar] [CrossRef]
- Galanakis, C.M. The food systems in the era of the Coronavirus (COVID-19) pandemic crisis. Foods 2020, 9, 523. [Google Scholar] [CrossRef]
- Fanelli, R. Changes in the food-related behaviour of Italian consumers during the COVID-19 pandemic. Foods 2021, 10, 169. [Google Scholar] [CrossRef]
- Public Health England. Impact of COVID-19 Pandemic on Grocery Shopping Behaviours. London: 2020. Available online: www.facebook.com/PublicHealthEngland (accessed on 20 September 2021).
- Posel, D.; Oyenubi, A.; Kollamparambil, U. Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa. PLoS ONE 2021, 16, e0249352. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Coronavirus and Redundancies in the UK Labour Market. Off. Natl. Stat. 2020. Available online: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/articles/labourmarketeconomicanalysisquarterly/december2020 (accessed on 20 September 2021).
- Vandevijvere, S.; Pedroni, C.; De Ridder, K.; Castetbon, K. The cost of diets according to their caloric share of ultraprocessed and minimally processed foods in Belgium. Nutrition 2020, 12, 2787. [Google Scholar] [CrossRef]
- Allabadi, H.; Dabis, J.; Aghabekian, V.; Khader, A.; Khammash, U. Impact of COVID-19 lockdown on dietary and lifestyle behaviours among adolescents in Palestine. Dynam. Hum. Health 2020, 7, 2170. [Google Scholar] [CrossRef]
- Clemmensen, C.; Petersen, M.B.; Sørensen, T.I.A. Will the COVID-19 pandemic worsen the obesity epidemic? Nat. Rev. Endocrinol. 2020, 16, 469–470. [Google Scholar] [CrossRef]
- Ulrich-Lai, Y.; Ryan, K.K. Neuroendocrine circuits governing energy balance and stress regulation: Functional overlap and therapeutic implications. Cell Metab. 2014, 19, 910–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marazziti, D.; Cianconi, P.; Mucci, F.; Foresi, L.; Chiarantini, I.; Della Vecchia, A. Climate change, environment pollution, COVID-19 pandemic and mental health. Sci. Total Environ. 2021, 773, 145182. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; Wong, M. Global climate change and mental health. Curr. Opin. Psychol. 2020, 32, 12–16. [Google Scholar] [CrossRef]
- Hills, A.P.; King, N.A.; Armstrong, T.P. The contribution of physical activity and sedentary behaviours to the growth and development of children and adolescents: Implications for overweight and obesity. Sports Med. 2007, 37, 533–545. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Public Health. Childhood obesity beyond COVID-19. Lancet Public Health 2021, 6, e534. [Google Scholar] [CrossRef]
- Scully, M.; Dixon, H.; Wakefield, M. Association between commercial television exposure and fast-food consumption among adults. Public Health Nutr. 2009, 12, 105–110. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Zakka, K.; Chidambaram, S.; Mansour, S.; Mahawar, K.; Salminen, P.; Almino, R.; Schauer, P.; Kinross, J.; Purkayastha, S.; on behalf of the PanSurg Collaborative; Chidambaram, S. SARS-CoV-2 and obesity: “CoVesity”—A pandemic within a pandemic. Obes. Surg. 2021, 31, 1–10. [Google Scholar] [CrossRef]
- Klemeš, J.J.; Van Fan, Y.; Jiang, P. The energy and environmental footprints of COVID-19 fighting measures—PPE, disinfection, supply chains. Energy 2020, 211, 118701. [Google Scholar] [CrossRef] [PubMed]
- Gillingham, K.T.; Knittel, C.R.; Li, J.; Ovaere, M.; Reguant, M. The Short-run and Long-run Effects of Covid-19 on Energy and the Environment. Joule 2020, 4, 1337–1341. [Google Scholar] [CrossRef] [PubMed]
- Laverty, A.A.; Millett, C.; Majeed, A.; Vamos, E.P. COVID-19 presents opportunities and threats to transport and health. J. R. Soc. Med. 2020, 113, 251–254. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Shen, Q.; Fan, L.C.; Wang, Y.; Zhang, L. Greenhouse gas emissions in building construction: A case study of One Peking in Hong Kong. Build. Environ. 2010, 45, 949–955. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.; Barbour, W.; Samaranayake, S.; Work, D. Impacts of Covid-19 mode shift on road traffic. arXiv 2020, arXiv:2005.01610. [Google Scholar]
- Galanti, T.; Guidetti, G.; Mazzei, E.; Zappalà, S.; Toscano, F. Work from home during the COVID-19 outbreak. J. Occup. Environ. Med. 2021, 63, e426–e432. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, T.; Ackerman, S.E.; Shen, L.; Engleman, E. Role of innate and adaptive immunity in obesity-associated metabolic disease. J. Clin. Investig. 2017, 127, 5–13. [Google Scholar] [CrossRef] [Green Version]
- Cuschieri, S.; Grech, S. Obesity population at risk of COVID-19 complications. Glob. Health Epidemiol. Genom. 2020, 5. [Google Scholar] [CrossRef]
- Simonnet, A.; Chetboun, M.; Poissy, J.; Raverdy, V.; Noulette, J.; Duhamel, A.; Labreuche, J.; Mathieu, D.; Pattou, F.; Jourdain, M.; et al. High prevalence of obesity in severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity 2020, 28, 1195–1199. [Google Scholar] [CrossRef]
- Senthilingam, M. Covid-19 has made the obesity epidemic worse, but failed to ignite enough action. BMJ 2021, 372, n411. [Google Scholar] [CrossRef] [PubMed]
- Landier, J.; Paireau, J.; Rebaudet, S.; Legendre, E.; Lehot, L.; Fontanet, A.; Cauchemez, S.; Gaudart, J. Cold and dry winter conditions are associated with greater SARS-CoV-2 transmission at regional level in western countries during the first epidemic wave. Sci. Rep. 2021, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.B. Epidemics on the move: Climate change and infectious disease. PLoS Biol. 2020, 18, e3001013. [Google Scholar] [CrossRef] [PubMed]
- Usman, M.; Husnain, M.; Riaz, A.; Riaz, A.; Ali, Y. Climate change during the COVID-19 outbreak: Scoping future perspectives. Environ. Sci. Pollut. Res. 2021, 28, 49302–49313. [Google Scholar] [CrossRef] [PubMed]
- Mckeever, A. Why climate change is still the greatest threat to human health. National Geographic Magazine, 19 August 2021. [Google Scholar]
- Tong, S.; Ebi, K.; Olsen, J. Infectious disease, the climate, and the future. Environ. Epidemiol. 2021, 5, e133. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).