HELIX Syndrome, a Claudinopathy with Relevant Dermatological Manifestations: Report of Two New Cases
Abstract
1. Introduction
2. Materials and Methods
3. Results
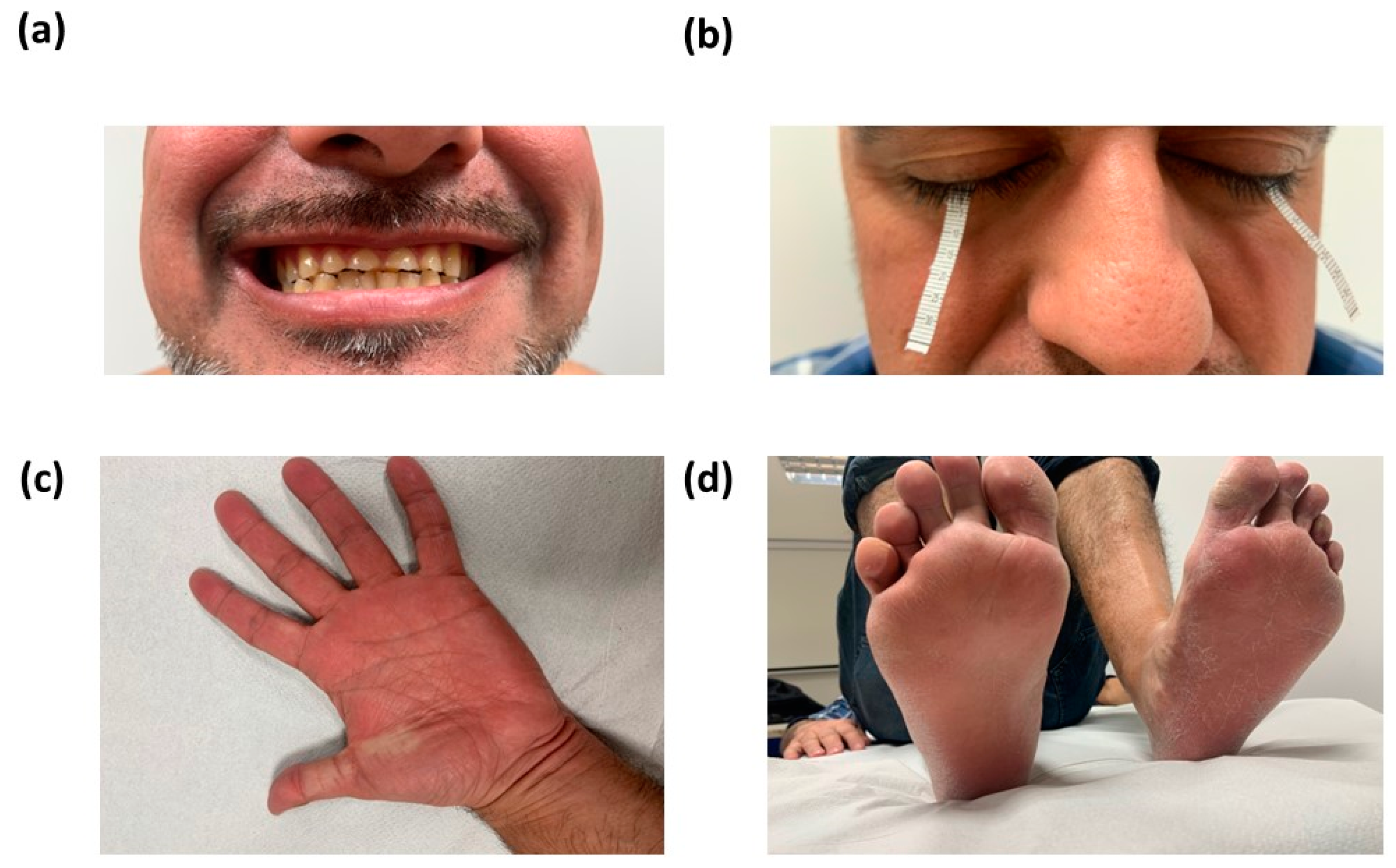
3.1. Clinical Phenotype of the Cases Reported
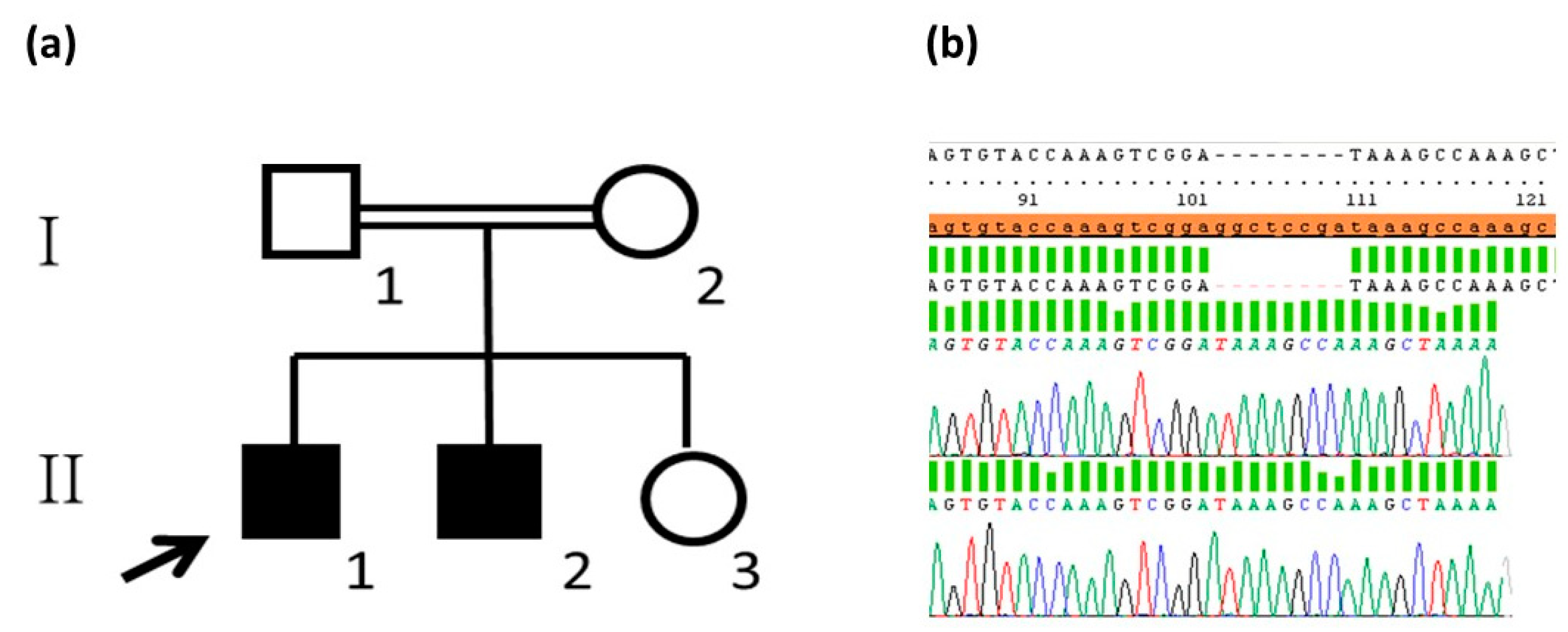
3.2. Analysis of the Variant Detected
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hadj-Rabia, S.; Brideau, G.; Al-Sarraj, Y.; Maroun, R.C.; Figueres, M.L.; Leclerc-Mercier, S.; Olinger, E.; Baron, S.; Chaussain, C.; Nochy, D.; et al. Multiplex epithelium dysfunction due to CLDN10 mutation: The HELIX syndrome. Genet. Med. 2018, 20, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Van Itallie, C.M.; Rogan, S.; Yu, A.; Vidal, L.S.; Holmes, J.; Anderson, J.M. Two splice variants of claudin-10 in the kidney create paracellular pores with different ion selectivities. Am. J. Physiol. Renal Physiol. 2006, 291, F1288–F1299. [Google Scholar] [CrossRef] [PubMed]
- Klar, J.; Piontek, J.; Milatz, S.; Tariq, M.; Jameel, M.; Breiderhoff, T.; Schuster, J.; Fatima, A.; Asif, M.; Sher, M.; et al. Altered paracellular cation permeability due to a rare CLDN10B variant causes anhidrosis and kidney damage. PLoS Genet. 2017, 13, e1006897. [Google Scholar] [CrossRef] [PubMed]
- Bongers, E.; Shelton, L.M.; Milatz, S.; Verkaart, S.; Bech, A.P.; Schoots, J.; Cornelissen, E.; Bleich, M.; Hoenderop, J.; Wetzels, J.; et al. A Novel Hypokalemic-Alkalotic Salt-Losing Tubulopathy in Patients with CLDN10 Mutations. J. Am. Soc. Nephrol. 2017, 28, 3118–3128. [Google Scholar] [CrossRef] [PubMed]
- Meyers, N.; Nelson-Williams, C.; Malaga-Dieguez, L.; Kaufmann, H.; Loring, E.; Knight, J.; Lifton, R.P.; Trachtman, H. Hypokalemia Associated With a Claudin 10 Mutation: A Case Report. Am. J. Kidney Dis. 2019, 73, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, A.S.; Hussein, M.; Alswailem, M.; Mouna, A.; Albalawi, L.; Moria, Y.; Abdel Jabbar, M.; Shi, Y.; Günzel, D.; Dasouki, M. A novel claudin-10 mutation with a unique mechanism in two unrelated families with HELIX syndrome. Kidney Int. 2021, 100, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Milatz, S. A Novel Claudinopathy Based on Claudin-10 Mutations. Int. J. Mol. Sci. 2019, 20, 5396. [Google Scholar] [CrossRef] [PubMed]
- Sewerin, S.; Piontek, J.; Schönauer, R.; Grunewald, S.; Rauch, A.; Neuber, S.; Bergmann, C.; Günzel, D.; Halbritter, J. Defective claudin-10 causes a novel variation of HELIX syndrome through compromised tight junction strand assembly. Genes. Dis. 2022, 9, 1301–1314. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Romero, M.C.; Ballesta-Martinez, M.J.; Lopez-Gonzalez, V.; Sanchez-Soler, M.J.; Serrano-Anton, A.T.; Barreda-Sanchez, M.; Rodriguez-Peña, L.; Carbonell-Meseguer, P.; Glover-López, G.; Guillén-Navarro, E.; et al. EDA, EDAR, EDARADD and WNT10A allelic variants in patients with ectodermal derivative impairment in the Spanish population. Orphanet. J. Rare Dis. 2019, 14, 281. [Google Scholar] [CrossRef] [PubMed]
- Bech, A.P.; Wetzels, J.F.; Bongers, E.M.; Nijenhuis, T. Thiazide Responsiveness Testing in Patients with Renal Magnesium Wasting and Correlation With Genetic Analysis: A Diagnostic Test Study. Am. J. Kidney Dis. 2016, 68, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Verhave, J.C.; Bech, A.P.; Wetzels, J.F.; Nijenhuis, T. Hepatocyte Nuclear Factor 1β-Associated Kidney Disease: More than Renal Cysts and Diabetes. J. Am. Soc. Nephrol. 2016, 27, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Poussou, R. Pathophysiological aspects of the thick ascending limb and novel genetic defects: HELIX syndrome and transient antenatal Bartter syndrome. Pediatr. Nephrol. 2022, 37, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Breiderhoff, T.; Himmerkus, N.; Stuiver, M.; Mutig, K.; Will, C.; Meij, I.C.; Bachmann, S.; Bleich, M.; Willnow, T.E.; Müller, D.; et al. Deletion of claudin-10 (Cldn10) in the thick ascending limb impairs paracellular sodium permeability and leads to hypermagnesemia and nephrocalcinosis. Proc. Natl. Acad. Sci. USA 2012, 109, 14241–14246. [Google Scholar] [CrossRef] [PubMed]
- Plain, A.; Wulfmeyer, V.C.; Milatz, S.; Klietz, A.; Hou, J.; Bleich, M.; Himmerkus, N. Corticomedullary difference in the effects of dietary Ca²⁺ on tight junction properties in thick ascending limbs of Henle’s loop. Pflug. Arch. 2016, 468, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Chiba, Y.; Jia, L.; Yoshizaki, K.; Saito, K.; Yamada, A.; Qin, M.; Fukumoto, S. Expression Patterns of Claudin Family Members During Tooth Development and the Role of Claudin-10 (Cldn10) in Cytodifferentiation of Stratum Intermedium. Front. Cell. Dev. Biol. 2020, 8, 595593. [Google Scholar] [CrossRef] [PubMed]
- Stenson, P.D.; Ball, E.V.; Mort, M.; Phillips, A.D.; Shiel, J.A.; Thomas, N.S.; Abeysinghe, S.; Krawczak, M.; Cooper, D.N. Human Gene Mutation Database (HGMD): 2003 update. Hum. Mutat. 2003, 21, 577–581. [Google Scholar] [CrossRef]
| Laboratory Data | Case 1 | Case 2 | Reference Values |
|---|---|---|---|
| Age | 41 years | 38 years | |
| Serum values | |||
| Plasma creatinine | 1.60 mg/dL | 1.14 mg/dL | 0.70–1.20 mg/dL |
| Glomerular filtration (CKD-EPI mL/min) | 52.73 mL/min/1.73 m2 | 82 mL/min/1.73 m2 | >90 mL/min/1.73 m2 |
| Plasma values | |||
| Na+ | 141 mEq/L | normal | 136–145 mEq/L |
| K+ | 3.3 mEq/L | 2.5 mEq/L | 3.5–5.1 mEq/L |
| Cl− | 95 mEq/L | 90 mEq/L | 98–107 mEq/L |
| Mg2+ | 2.66 mEq/L | normal | 1.60–2.60 mEq/L |
| Ca2+ | 9.4 mg/dL | 9.5 mg/dL | 8.6–10 mg/dL |
| Phosphorus | 3.5 mg/dL | 3.5 mg/dL | 2.5–4.5 mg/dL |
| PTH | 63.2 pg/mL | 25 pg/mL | 18.5–88 pg/mL |
| Aldosterone | 348 pg/mL | NA | 7.0–150 pg/mL |
| Renin | 2.0 ng/mL/h | NA | 0.8–2.1 |
| Lipase activity | 100 U/L | NA | 13–69 U/L |
| Amylase | 57 U/L | NA | 13–53 U/L |
| 25-OH vitamin D | 11.3 μg/L | NA | 30–100 μg/L |
| Blood pH | 7.42 | 7.43 | 7.3–7.4 |
| Bicarbonate | 36.1 mEq/L | NA | 22–26 mEq/L |
| Urine values | |||
| Na+ | 161 mEq/L | NA | 40–150 mEq/L |
| K+ | 29.1 mEq/L | NA | 25–80 mEq/L |
| Cl− | 138 mEq/L | >25 mEq | 46–168 mEq/L |
| Mg2+ | 3.4 mg/dL | NA | 25.7–131.9 mg/dL |
| Ca2+ | 0.9 mg/dL | <0.01 mg/dL | 5–35 mg/dL |
| References | This Report | Meyers et al., 2019 | Bongers et al., 2017 | Klar et al., 2017 | Hadj-Rabia et al., 2018 | Alzahrani et al., 2021 | Sewerin et al., 2022 |
| Origin | Spain | Ecuador | The Netherlands | Pakistan | North Africa | Saudi Arabia | Afghanistan |
| Patients/Families | 2/1 | 1/1 | 2/2 | 13/2 | 6/2 | 12/2 | 1/1 |
| Genotype CLDN10b (NM_006984.4) | c.322_329del8 (p.G108fs*) | c.238A>G (p.R80G) | c.446C>G; c.465-1G>A (p.P149R; p.E157_Y192del) c.446C>G; c.217G>A (p.P149R; p.D73N) | c.144C>G (p.N48K) | c.2T>C (p.M1?) c.392C>T (p.S131L) | c.653delC (p.P218Lfs*21) | c.494C>G (p.G165A) |
| Hypohidrosis | 2/2 | 1/1 | ND | 13/13 | 6/6 | 12/12 | 1/1 |
| Lachrymal dysfunction | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Xerosis, xerostomia | 2/2 | 1/1 | ND | 13/13 | 6/6 | 12/12 | 0/1 |
| Ichthyosis | 2/2 | 0/1 | ND | ND | 6/6 | 11/12 | 0/1 |
| Impairment of enamel wear | Yes | ND | ND | ND | Yes | ND | Yes |
| Hypokalemia | 2/2 | 1/1 | 2/2 | 0/7 | 3/6 | 12/12 | 1/1 |
| Hypermagnesemia | 2/2 | 1/1 | 1/2 | 6/7 | 6/6 | 12/12 | 1/1 |
| Abnormal glomerular filtration | 2/2 | 1/1 | 1/2 | 0/3 | 1/6 | 12/12 | 1/1 |
| Secondary hyperaldosteronism | Hyperaldosteronism w/o hyperreninism 2/2 | Hyperaldosteronism w/o hyperreninism | ND | ND | 6/6 | 12/12 | Hyperaldosteronism w hyperreninism |
| Nephrolithiasis | 0/2 | 0/1 | 0/2 | 4/13 | 0/6 | ND | 0/1 |
| Intolerance to high temperatures and physical exercise | 2/2 | ND | ND | 13/13 | 6/6 | ND | ND |
| Disease reported | HELIX syndrome | HELIX syndrome | Salt-losing tubulopathy | Anhidrosis, heat intolerance, kidney damage | HELIX syndrome | HELIX syndrome | HELIX syndrome |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Romero, M.C.; Hernández-Contreras, M.E.; Bafalliu-Vidal, J.A.; Barreda-Sánchez, M.; Martínez-Menchón, T.; Cabello-Chaves, V.; Guillén-Navarro, E. HELIX Syndrome, a Claudinopathy with Relevant Dermatological Manifestations: Report of Two New Cases. Genes 2024, 15, 687. https://doi.org/10.3390/genes15060687
Martínez-Romero MC, Hernández-Contreras ME, Bafalliu-Vidal JA, Barreda-Sánchez M, Martínez-Menchón T, Cabello-Chaves V, Guillén-Navarro E. HELIX Syndrome, a Claudinopathy with Relevant Dermatological Manifestations: Report of Two New Cases. Genes. 2024; 15(6):687. https://doi.org/10.3390/genes15060687
Chicago/Turabian StyleMartínez-Romero, María Carmen, María Encarnación Hernández-Contreras, Juan Antonio Bafalliu-Vidal, María Barreda-Sánchez, Teresa Martínez-Menchón, Virginia Cabello-Chaves, and Encarna Guillén-Navarro. 2024. "HELIX Syndrome, a Claudinopathy with Relevant Dermatological Manifestations: Report of Two New Cases" Genes 15, no. 6: 687. https://doi.org/10.3390/genes15060687
APA StyleMartínez-Romero, M. C., Hernández-Contreras, M. E., Bafalliu-Vidal, J. A., Barreda-Sánchez, M., Martínez-Menchón, T., Cabello-Chaves, V., & Guillén-Navarro, E. (2024). HELIX Syndrome, a Claudinopathy with Relevant Dermatological Manifestations: Report of Two New Cases. Genes, 15(6), 687. https://doi.org/10.3390/genes15060687






