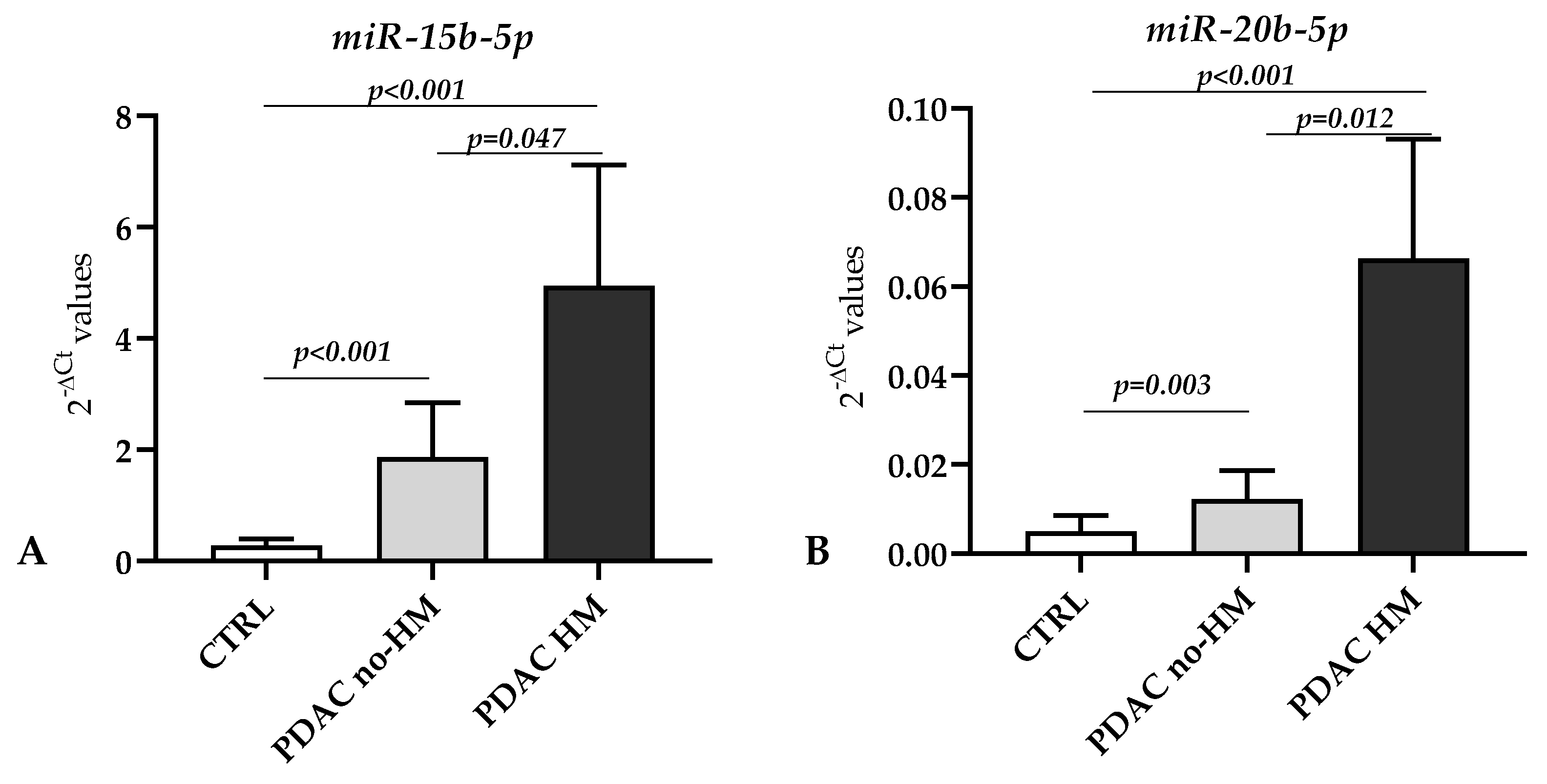
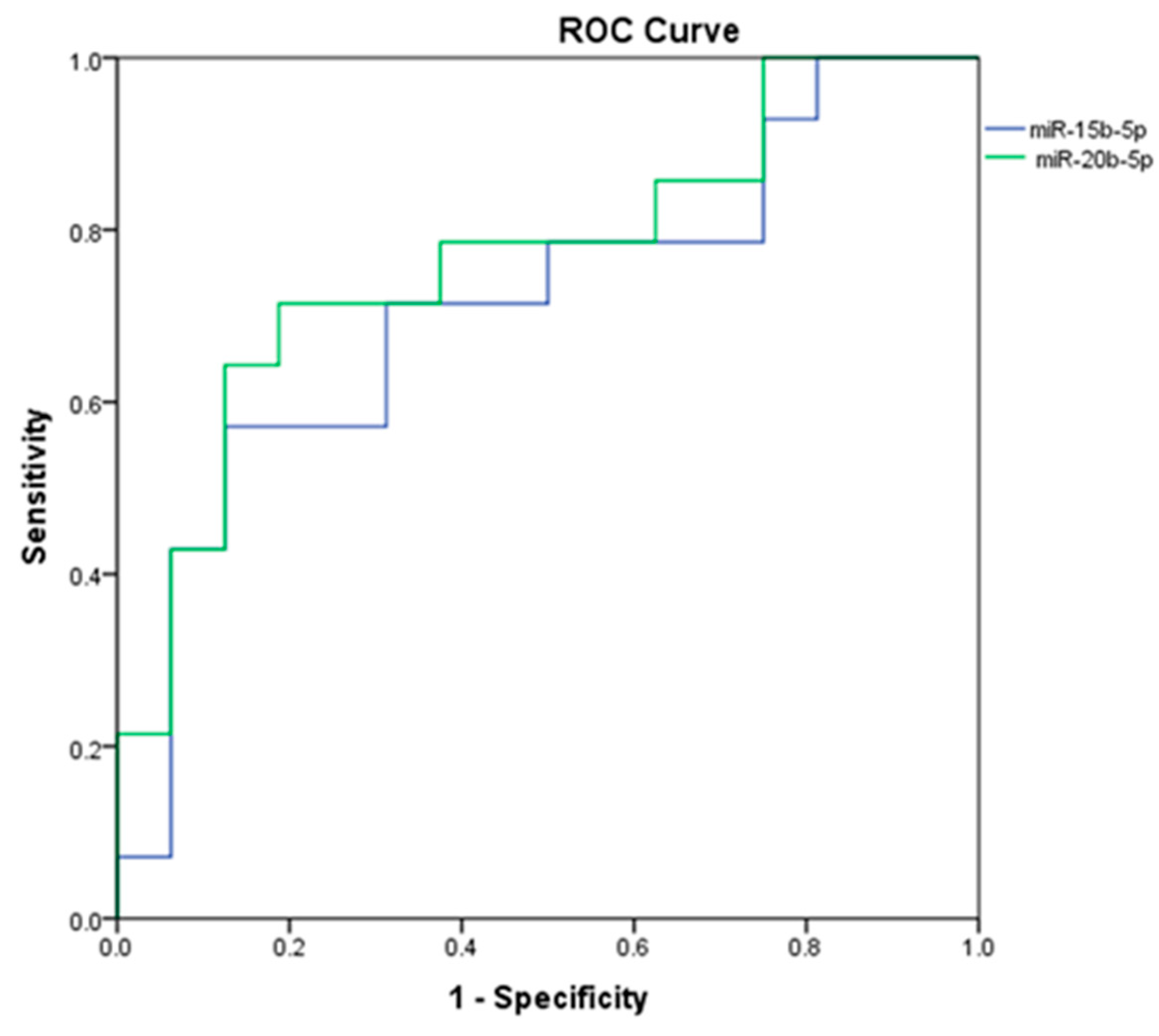
Increased Levels of miR-15b-5p and miR-20b-5p in Pancreatic Ductal Adenocarcinoma with Hepatic Metastases
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Evaluation of miRNAs
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures 2023; American Cancer Society: Atlanta, GA, USA, 2023. [Google Scholar]
- Khalaf, N.; El-Serag, H.B.; Abrams, H.R.; Thrift, A.P. Burden of Pancreatic Cancer: From Epidemiology to Practice. Clin. Gastroenterol. Hepatol. 2021, 19, 876–884. [Google Scholar] [CrossRef]
- Iguchi, E.; Safgren, S.L.; Marks, D.L.; Olson, R.L.; Fernandez-Zapico, M.E. Pancreatic Cancer, A Mis-Interpreter of the Epigenetic Language. Yale J. Biol. Med. 2016, 89, 575–590. [Google Scholar]
- Bracci, P.M. Obesity and Pancreatic Cancer: Overview of Epidemiologic Evidence and Biologic Mechanisms. Mol. Carcinog. 2012, 51, 53–63. [Google Scholar] [CrossRef]
- De La Cruz, M.S.D.; Young, A.P.; Ruffin, M.T. Diagnosis and Management of Pancreatic Cancer. Am. Fam. Physician 2014, 89, 626–632. [Google Scholar]
- Smaglo, B.G. Role for Neoadjuvant Systemic Therapy for Potentially Resectable Pancreatic Cancer. Cancers 2023, 15, 2377. [Google Scholar] [CrossRef]
- Conroy, T.; Hammel, P.; Hebbar, M.; Ben Abdelghani, M.; Wei, A.C.; Raoul, J.-L.; Choné, L.; Francois, E.; Artru, P.; Biagi, J.J.; et al. FOLFIRINOX or Gemcitabine as Adjuvant Therapy for Pancreatic Cancer. N. Engl. J. Med. 2018, 379, 2395–2406. [Google Scholar] [CrossRef]
- Zhang, Y.; Xu, J.; Hua, J.; Liu, J.; Liang, C.; Meng, Q.; Ni, Q.; Shi, S.; Yu, X. Nab-Paclitaxel plus Gemcitabine as First-Line Treatment for Advanced Pancreatic Cancer: A Systematic Review and Meta-Analysis. J. Cancer 2019, 10, 4420–4429. [Google Scholar] [CrossRef]
- Sturm, N.; Ettrich, T.J.; Perkhofer, L. The Impact of Biomarkers in Pancreatic Ductal Adenocarcinoma on Diagnosis, Surveillance and Therapy. Cancers 2022, 14, 217. [Google Scholar] [CrossRef]
- Martínez-Bosch, N.; Cristóbal, H.; Iglesias, M.; Gironella, M.; Barranco, L.; Visa, L.; Calafato, D.; Jiménez-Parrado, S.; Earl, J.; Carrato, A.; et al. Soluble AXL Is a Novel Blood Marker for Early Detection of Pancreatic Ductal Adenocarcinoma and Differential Diagnosis from Chronic Pancreatitis. EBioMedicine 2022, 75, 103797. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.-H.; Wang, W.-Q.; Han, X.; Gao, H.-L.; Li, T.-J.; Xu, S.-S.; Li, S.; Xu, H.-X.; Li, H.; Ye, L.-Y.; et al. Advances on Diagnostic Biomarkers of Pancreatic Ductal Adenocarcinoma: A Systems Biology Perspective. Comput. Struct. Biotechnol. J. 2020, 18, 3606–3614. [Google Scholar] [CrossRef] [PubMed]
- Dobre, M.; Herlea, V.; Vlăduţ, C.; Ciocîrlan, M.; Balaban, V.D.; Constantinescu, G.; Diculescu, M.; Milanesi, E. Dysregulation of MiRNAs Targeting the IGF-1R Pathway in Pancreatic Ductal Adenocarcinoma. Cells 2021, 10, 1856. [Google Scholar] [CrossRef] [PubMed]
- Daoud, A.Z.; Mulholland, E.J.; Cole, G.; McCarthy, H.O. MicroRNAs in Pancreatic Cancer: Biomarkers, Prognostic, and Therapeutic Modulators. BMC Cancer 2019, 19, 1130. [Google Scholar] [CrossRef] [PubMed]
- Jin, T.; Dai, C.; Xu, F. Surgical and Local Treatment of Hepatic Metastasis in Pancreatic Ductal Adenocarcinoma: Recent Advances and Future Prospects. Ther. Adv. Med. Oncol. 2020, 12, 175883592093303. [Google Scholar] [CrossRef]
- Kim, J.; Yao, F.; Xiao, Z.; Sun, Y.; Ma, L. MicroRNAs and Metastasis: Small RNAs Play Big Roles. Cancer Metastasis Rev. 2018, 37, 5–15. [Google Scholar] [CrossRef]
- Prinz, C.; Fehring, L.; Frese, R. MicroRNAs as Indicators of Malignancy in Pancreatic Ductal Adenocarcinoma (PDAC) and Cystic Pancreatic Lesions. Cells 2022, 11, 2374. [Google Scholar] [CrossRef]
- Guz, M.; Jeleniewicz, W.; Cybulski, M.; Kozicka, J.; Kurzepa, J.; Mądro, A. Serum MiR-210-3p Can Be Used to Differentiate between Patients with Pancreatic Ductal Adenocarcinoma and Chronic Pancreatitis. Biomed. Rep. 2020, 14, 10. [Google Scholar] [CrossRef]
- Xie, F.; Xiao, P.; Chen, D.; Xu, L.; Zhang, B. MiRDeepFinder: A MiRNA Analysis Tool for Deep Sequencing of Plant Small RNAs. Plant Mol. Biol. 2012, 80, 75–84. [Google Scholar] [CrossRef]
- Livak, K.J.; Schmittgen, T.D. Analysis of Relative Gene Expression Data Using Real-Time Quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001, 25, 402–408. [Google Scholar] [CrossRef]
- Kehl, T.; Kern, F.; Backes, C.; Fehlmann, T.; Stöckel, D.; Meese, E.; Lenhof, H.-P.; Keller, A. MiRPathDB 2.0: A Novel Release of the MiRNA Pathway Dictionary Database. Nucleic Acids Res. 2020, 48, D142–D147. [Google Scholar] [CrossRef]
- Chen, C.; Gong, X.; Yang, X.; Shang, X.; Du, Q.; Liao, Q.; Xie, R.; Chen, Y.; Xu, J. The Roles of Estrogen and Estrogen Receptors in Gastrointestinal Disease (Review). Oncol. Lett. 2019, 18, 5673–5680. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Liu, M.; Ding, Q.; Ji, X.; Hao, Y.; Wu, X.; Xiong, J. The Direct Effect of Estrogen on Cell Viability and Apoptosis in Human Gastric Cancer Cells. Mol. Cell. Biochem. 2014, 395, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, H.R.; Doucet, K.; Duke, V.; Morra, A.; Johnson, N. Estrogen Prevents Sustained COLO-205 Human Colon Cancer Cell Growth by Inducing Apoptosis, Decreasing c-Myb Protein, and Decreasing Transcription of the Anti-Apoptotic Protein Bcl-2. Tumor Biol. 2010, 31, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.; Borgquist, S.; Jirström, K. Hormonal Factors and Pancreatic Cancer Risk in Women: The Malmö Diet and Cancer Study. Int. J. Cancer 2018, 143, 52–62. [Google Scholar] [CrossRef]
- Stanciu, S.; Ionita-Radu, F.; Stefani, C.; Miricescu, D.; Stanescu-Spinu, I.-I.; Greabu, M.; Ripszky Totan, A.; Jinga, M. Targeting PI3K/AKT/MTOR Signaling Pathway in Pancreatic Cancer: From Molecular to Clinical Aspects. Int. J. Mol. Sci. 2022, 23, 10132. [Google Scholar] [CrossRef]
- Baer, R.; Cintas, C.; Therville, N.; Guillermet-Guibert, J. Implication of PI3K/Akt Pathway in Pancreatic Cancer: When PI3K Isoforms Matter? Adv. Biol. Regul. 2015, 59, 19–35. [Google Scholar] [CrossRef]
- Selvarajoo, N.; Stanslas, J.; Islam, M.K.; Sagineedu, S.R.; Lian, H.K.; Lim, J.C.W. Pharmacological Modulation of Apoptosis and Autophagy in Pancreatic Cancer Treatment. Mini-Rev. Med. Chem. 2022, 22, 2581–2595. [Google Scholar] [CrossRef]
- Qin, R.-F.; Zhang, J.; Huo, H.-R.; Yuan, Z.-J.; Xue, J.-D. MiR-205 Mediated APC Regulation Contributes to Pancreatic Cancer Cell Proliferation. World J. Gastroenterol. 2019, 25, 3775–3786. [Google Scholar] [CrossRef]
- Ali, S.; Dubaybo, H.; Brand, R.E. Differential Expression of Micrornas in Tissues and Plasma Co-Exists as a Biomarker for Pancreatic Cancer. J. Cancer Sci. Ther. 2015, 7, 336–346. [Google Scholar] [CrossRef]
- Michael Traeger, M.; Rehkaemper, J.; Ullerich, H.; Steinestel, K.; Wardelmann, E.; Senninger, N.; Abdallah Dhayat, S. The Ambiguous Role of MicroRNA-205 and Its Clinical Potential in Pancreatic Ductal Adenocarcinoma. J. Cancer Res. Clin. Oncol. 2018, 144, 2419–2431. [Google Scholar] [CrossRef]
- Wang, J.; Raimondo, M.; Guha, S.; Chen, J.; Diao, L.; Dong, X.; Wallace, M.B.; Killary, A.M.; Frazier, M.L.; Woodward, T.A.; et al. Circulating MicroRNAs in Pancreatic Juice as Candidate Biomarkers of Pancreatic Cancer. J. Cancer 2014, 5, 696–705. [Google Scholar] [CrossRef]
- Zhuang, L.; Guo, J.; Yao, Y.; Li, Z. MiR-205 Targets Runt-related Transcription Factor 2 to Inhibit Human Pancreatic Cancer Progression. Oncol. Lett. 2018, 17, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Chitkara, D.; Kumar, V.; Behrman, S.W.; Mahato, R.I. MiRNA Profiling in Pancreatic Cancer and Restoration of Chemosensitivity. Cancer Lett. 2013, 334, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Yu, W.; Lin, S.; Zhang, M.; Wang, T.; Guo, S.; Wang, H. LncRNA ADPGK-AS1 Promotes Pancreatic Cancer Progression through Activating ZEB1 -Mediated Epithelial–Mesenchymal Transition. Cancer Biol. Ther. 2018, 19, 573–583. [Google Scholar] [CrossRef]
- Karamitopoulou, E.; Haemmig, S.; Baumgartner, U.; Schlup, C.; Wartenberg, M.; Vassella, E. MicroRNA Dysregulation in the Tumor Microenvironment Influences the Phenotype of Pancreatic Cancer. Mod. Pathol. 2017, 30, 1116–1125. [Google Scholar] [CrossRef]
- Zhu, H.; Shan, Y.; Ge, K.; Lu, J.; Kong, W.; Jia, C. LncRNA CYTOR Promotes Pancreatic Cancer Cell Proliferation and Migration by Sponging MiR-205-5p. Pancreatology 2020, 20, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Lu, X.; Shi, Z.; Li, X.; Zhang, Y.; Zhao, S.; Liu, H. MiR-205-5p Regulates Epithelial-Mesenchymal Transition by Targeting PTEN via PI3K/AKT Signaling Pathway in Cisplatin-Resistant Nasopharyngeal Carcinoma Cells. Gene 2019, 710, 103–113. [Google Scholar] [CrossRef]
- Tao, Q.; Qi, Y.; Gu, J.; Yu, D.; Lu, Y.; Liu, J.; Liang, X. Breast Cancer Cells-Derived Von Willebrand Factor Promotes VEGF-A-Related Angiogenesis through PI3K/Akt-MiR-205-5p Signaling Pathway. Toxicol. Appl. Pharmacol. 2022, 440, 115927. [Google Scholar] [CrossRef]
- Zhu, F.; Ren, Z. Icariin Inhibits the Malignant Progression of Lung Cancer by Affecting the PI3K/Akt Pathway through the MiR-205-5p/PTEN Axis. Oncol. Rep. 2022, 47, 115. [Google Scholar] [CrossRef]
- Li, Y.; Deng, X.; Zeng, X.; Peng, X. The Role of Mir-148a in Cancer. J. Cancer 2016, 7, 1233–1241. [Google Scholar] [CrossRef]
- Idichi, T.; Seki, N.; Kurahara, H.; Fukuhisa, H.; Toda, H.; Shimonosono, M.; Okato, A.; Arai, T.; Kita, Y.; Mataki, Y.; et al. Molecular Pathogenesis of Pancreatic Ductal Adenocarcinoma: Impact of Passenger Strand of Pre- MiR-148a on Gene Regulation. Cancer Sci. 2018, 109, 2013–2026. [Google Scholar] [CrossRef]
- Hanoun, N.; Delpu, Y.; Suriawinata, A.A.; Bournet, B.; Bureau, C.; Selves, J.; Tsongalis, G.J.; Dufresne, M.; Buscail, L.; Cordelier, P.; et al. The Silencing of MicroRNA 148a Production by DNA Hypermethylation Is an Early Event in Pancreatic Carcinogenesis. Clin. Chem. 2010, 56, 1107–1118. [Google Scholar] [CrossRef]
- Fu, X.; Hong, L.; Yang, Z.; Tu, Y.; Xin, W.; Zha, M.; Tu, S.; Sun, G.; Li, Y.; Xiao, W. MicroRNA-148a-3p Suppresses Epithelial-to-mesenchymal Transition and Stemness Properties via Wnt1-mediated Wnt/Β-catenin Pathway in Pancreatic Cancer. J. Cell. Mol. Med. 2020, 24, 13020–13035. [Google Scholar] [CrossRef] [PubMed]
- Liffers, S.-T.; Munding, J.B.; Vogt, M.; Kuhlmann, J.D.; Verdoodt, B.; Nambiar, S.; Maghnouj, A.; Mirmohammadsadegh, A.; Hahn, S.A.; Tannapfel, A. MicroRNA-148a Is down-Regulated in Human Pancreatic Ductal Adenocarcinomas and Regulates Cell Survival by Targeting CDC25B. Lab. Investig. 2011, 91, 1472–1479. [Google Scholar] [CrossRef]
- Szabo, A.; Gurlich, R.; Liberko, M.; Soumarova, R.; Vernerova, Z.; Mandys, V.; Popov, A. Expression of Selected MicroRNAs in Pancreatic Ductal Adenocarcinoma: Is There a Relation to Tumor Morphology, Progression, and Patient’s Outcome? Neoplasma 2020, 67, 1170–1181. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, M.; Wang, H.; Fisher, W.E.; Lin, P.H.; Yao, Q.; Chen, C. Profiling of 95 MicroRNAs in Pancreatic Cancer Cell Lines and Surgical Specimens by Real-Time PCR Analysis. World J. Surg. 2009, 33, 698–709. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Sun, S.; Song, C.; Li, N.; Li, N.; Xu, L.; Yang, T.; Lan, Y.; Li, M. Screening Potential MicroRNAs Associated with Pancreatic Cancer: Data Mining Based on RNA Sequencing and Microarrays. Exp. Ther. Med. 2020, 20, 2705–2715. [Google Scholar] [CrossRef]
- ZHANG, W.-L.; ZHANG, J.-H.; WU, X.-Z.; YAN, T.; LV, W. MiR-15b Promotes Epithelial-Mesenchymal Transition by Inhibiting SMURF2 in Pancreatic Cancer. Int. J. Oncol. 2015, 47, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- Zu, F.; Liu, P.; Wang, H.; Zhu, T.; Sun, J.; Sheng, W.; Tan, X. Integrated Analysis Identifies a Pathway-Related Competing Endogenous RNA Network in the Progression of Pancreatic Cancer. BMC Cancer 2020, 20, 958. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wu, L.; Tan, W.; Zhang, K.; Lin, Q.; Zhu, J.; Tu, C.; Lv, X.; Jiang, C. MiR-20b-5p Promotes Hepatocellular Carcinoma Cell Proliferation, Migration and Invasion by down-Regulating CPEB3. Ann. Hepatol. 2021, 23, 100345. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Liu, X.; Wu, J.; Wang, Y.; Zhou, K.; Chen, W.; Chen, J.; Chen, C.; Chen, L. LncRNA WWOX-AS1 Sponges MiR-20b-5p in Hepatocellular Carcinoma and Represses Its Progression by Upregulating WWOX. Cancer Biol. Ther. 2020, 21, 927–936. [Google Scholar] [CrossRef] [PubMed]


| PDAC (n = 30) | |
|---|---|
| Anatomic Location | Head = 20 |
| Neck = 4 | |
| Body = 2 | |
| Body-Tail = 2 | |
| Tail = 2 | |
| Stage (UICC) IA/IB/IIA/IIB/III/IV | 1/4/4/1/6/14 |
| Lymph Node Involvement | Yes = 22 (73.3%) |
| No = 8 (26.7%) | |
| Hepatic Metastasis | Yes = 14 (46.7%) |
| No = 16 (53.3%) | |
| Lung Metastasis | Yes = 2 (6.7%) |
| No = 28 (93.3%) | |
| Diabetes | Yes = 12 |
| No = 18 | |
| Smokers | Yes = 15 |
| No = 12 | |
| Not available data = 3 | |
| Alcohol consumers | Yes = 4 |
| No = 23 | |
| Not available data = 3 | |
| Vegetarian diet | Yes = 1 |
| No = 29 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dobre, M.; Poenaru, R.C.; Niculae, A.M.; Vladut, C.; Herlea, V.; Milanesi, E.; Hinescu, M.E. Increased Levels of miR-15b-5p and miR-20b-5p in Pancreatic Ductal Adenocarcinoma with Hepatic Metastases. Genes 2023, 14, 1577. https://doi.org/10.3390/genes14081577
Dobre M, Poenaru RC, Niculae AM, Vladut C, Herlea V, Milanesi E, Hinescu ME. Increased Levels of miR-15b-5p and miR-20b-5p in Pancreatic Ductal Adenocarcinoma with Hepatic Metastases. Genes. 2023; 14(8):1577. https://doi.org/10.3390/genes14081577
Chicago/Turabian StyleDobre, Maria, Radu Cristian Poenaru, Andrei Marian Niculae, Catalina Vladut, Vlad Herlea, Elena Milanesi, and Mihail Eugen Hinescu. 2023. "Increased Levels of miR-15b-5p and miR-20b-5p in Pancreatic Ductal Adenocarcinoma with Hepatic Metastases" Genes 14, no. 8: 1577. https://doi.org/10.3390/genes14081577
APA StyleDobre, M., Poenaru, R. C., Niculae, A. M., Vladut, C., Herlea, V., Milanesi, E., & Hinescu, M. E. (2023). Increased Levels of miR-15b-5p and miR-20b-5p in Pancreatic Ductal Adenocarcinoma with Hepatic Metastases. Genes, 14(8), 1577. https://doi.org/10.3390/genes14081577





