Complementary Gene Therapy after Revascularization with the Saphenous Vein in Diabetic Foot Syndrome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Cohort
- (a)
- A small ulceration, necrosis of the finger(s) or a non-healing wound after finger amputation.
- (b)
- All were categorized as grade IV on the Fontaine scale.
- (c)
- They had received previous intensive treatment with no improvement for at least 14 days.
- (d)
- They had a confirmed ischemic DFS variant with TcPo2 (transcutaneous oxygen pressure) ≤ 40 mmHg or ABI (ankle-brachial index) ≤ 0.4. Glycated hemoglobin (Hba1c) was determined in all patients at the start of treatment.
- (e)
- At 2–5 days after revascularization surgery, venous by-pass function was assessed using ultrasonography, and ABI and TcPo2 at ankle level were performed.
- (a)
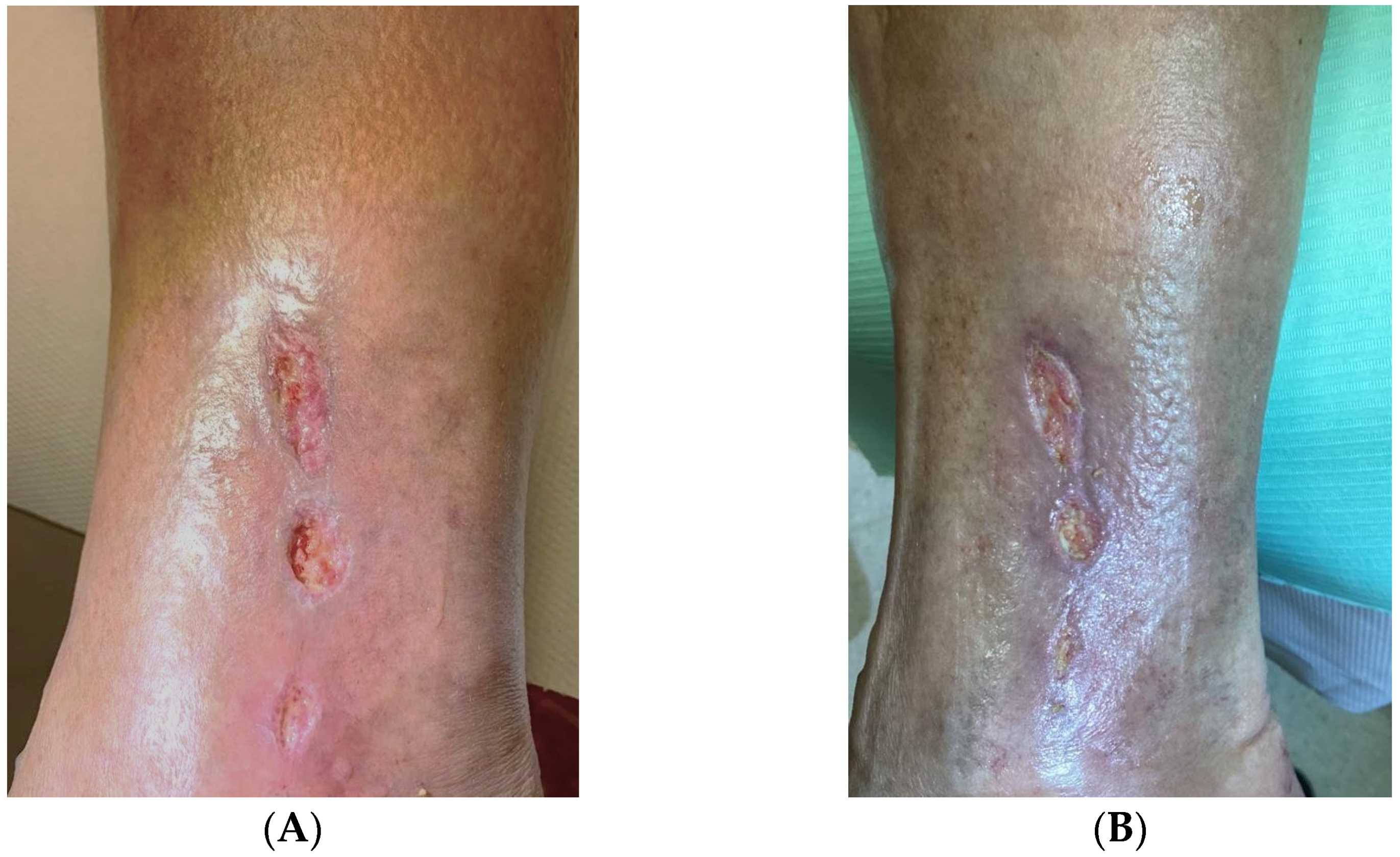
- The status of the ischemic lesion (extent, demarcation, presence of necrosis, and infiltration of adjacent tissues/ulceration (extent, depth, activity-granulation, or anergy)). All lesions were documented with photographs and descriptions.
- (b)
- ABI—the ratio of the highest pressure from the anterior or posterior tibial artery to the highest systolic pressure in the arm.
- (c)
- TcPO2—the Medicap Precise 8001 device was used for these measurements.
- (d)
- CDU (color duplex ultrasonography).
2.2. Preparation and Administration of Plasmid DNA
2.3. Statistical Analysis
3. Results
3.1. Group A (the Gene Therapy Group)
3.2. Group B (Control Group)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cannon, M.J.; Masalovich, S.; Ng, B.P.; Soler, R.E.; Jabrah, R.; Ely, E.K.; Smith, B.D. Retention Among Participants in the National Diabetes Prevention Program Lifestyle Change Program, 2012–2017. Diabetes Care 2020, 43, 2042–2049. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef]
- Deshpande, A.D.; Harris-Hayes, M.; Schootman, M. Epidemiology of diabetes and diabetes-related complications. Phys. Ther. 2008, 88, 1254–1264. [Google Scholar] [CrossRef]
- Van Netten, J.J.; Bus, S.A.; Apelqvist, J.; Lipsky, B.A.; Hinchliffe, R.J.; Game, F.; Rayman, G.; Lazzarini, P.A.; Forsythe, R.O.; Peters, E.J.G.; et al. Definitions and criteria for diabetic foot disease. Diabetes Metab. Res. Rev. 2020, 36 (Suppl. 1), e3268. [Google Scholar] [CrossRef] [PubMed]
- Russell, J.W.; Zilliox, L.A. Diabetic neuropathies. Continuum 2014, 20, 1226–1240. [Google Scholar] [CrossRef] [PubMed]
- Volmer-Thole, M.; Lobmann, R. Neuropathy and Diabetic Foot Syndrome. Int. J. Mol. Sci. 2016, 17, 917. [Google Scholar] [CrossRef] [PubMed]
- Hobizal, K.B.; Wukich, D.K. Diabetic foot infections: Current concept review. Diabet. Foot Ankle 2012, 3, 18409. [Google Scholar] [CrossRef]
- Dick, F.; Diehm, N.; Galimanis, A.; Husmann, M.; Schmidli, J.; Baumgartner, I. Surgical or endovascular revascularization in patients with critical limb ischemia: Influence of diabetes mellitus on clinical outcome. J. Vasc. Surg. 2007, 45, 751–761. [Google Scholar] [CrossRef]
- Pedras, S.; Carvalho, R.; Pereira, M.G. Predictors of quality of life in patients with diabetic foot ulcer: The role of anxiety, depression, and functionality. J. Health Psychol. 2018, 23, 1488–1498. [Google Scholar] [CrossRef]
- Ragnarson Tennvall, G.; Apelqvist, J. Health-related quality of life in patients with diabetes mellitus and foot ulcers. J. Diabetes Complicat. 2000, 14, 235–241. [Google Scholar] [CrossRef]
- Hinchliffe, R.J.; Andros, G.; Apelqvist, J.; Bakker, K.; Friederichs, S.; Lammer, J.; Lepantalo, M.; Mills, J.L.; Reekers, J.; Shearman, C.P.; et al. A systematic review of the effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral arterial disease. Diabetes Metab. Res. Rev. 2012, 28 (Suppl. 1), 179–217, Erratum in Diabetes Metab. Res. Rev. 2012, 28, 376. Fiedrichs, S [corrected to Friederichs, S]. [Google Scholar] [CrossRef] [PubMed]
- Pecoraro, R.E.; Reiber, G.E.; Burgess, E.M. Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care 1990, 13, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Brownrigg, J.R.; Apelqvist, J.; Bakker, K.; Schaper, N.C.; Hinchliffe, R.J. Evidence-based management of PAD & the diabetic foot. Eur. J. Vasc. Endovasc. Surg. 2013, 45, 673–681. [Google Scholar] [CrossRef]
- Yammine, K.; Boulos, K.; Assi, C.; Hayek, F. Amputation and mortality frequencies associated with diabetic Charcot foot arthropathy: A meta-analysis. Foot Ankle Surg. 2022, 28, 1170–1176. [Google Scholar] [CrossRef] [PubMed]
- Chammas, N.K.; Hill, R.L.; Edmonds, M.E. Increased Mortality in Diabetic Foot Ulcer Patients: The Significance of Ulcer Type. J. Diabetes Res. 2016, 2016, 2879809. [Google Scholar] [CrossRef]
- Lynar, S.A.; Robinson, C.H.; Boutlis, C.S.; Commons, R.J. Risk factors for mortality in patients with diabetic foot infections: A prospective cohort study. Intern. Med. J. 2019, 49, 867–873. [Google Scholar] [CrossRef]
- Boyko, E.J.; Ahroni, J.H.; Smith, D.G.; Davignon, D. Increased mortality associated with diabetic foot ulcer. Diabet. Med. 1996, 13, 967–972. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Swerdlow, M.A.; Armstrong, A.A.; Conte, M.S.; Padula, W.V.; Bus, S.A. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J. Foot Ankle Res. 2020, 13, 16. [Google Scholar] [CrossRef]
- Conte, M.S.; Bradbury, A.W.; Kolh, P.; White, J.V.; Dick, F.; Fitridge, R.; Mills, J.L.; Ricco, J.B.; Suresh, K.R.; Murad, M.H.; et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. Eur. J. Vasc. Endovasc. Surg. 2019, 58, S1–S109, Erratum in Eur. J. Vasc. Endovasc. Surg. 2019, 70, 662. [Google Scholar] [CrossRef]
- Klomp, H.M.; Steyerberg, E.W.; Habbema, J.D.; van Urk, H.; ESES study group. What is the evidence on efficacy of spinal cord stimulation in (subgroups of) patients with critical limb ischemia? Ann. Vasc. Surg. 2009, 23, 355–363. [Google Scholar] [CrossRef]
- Robertson, I.; Kessel, D.O.; Berridge, D.C. Fibrinolytic agents for peripheral arterial occlusion. Cochrane Database Syst Rev. 2013, 19, CD001099. [Google Scholar] [CrossRef] [PubMed]
- Fedorko, L.; Bowen, J.M.; Jones, W.; Oreopoulos, G.; Goeree, R.; Hopkins, R.B.; O’Reilly, D.J. Hyperbaric Oxygen Therapy Does Not Reduce Indications for Amputation in Patients with Diabetes with Nonhealing Ulcers of the Lower Limb: A Prospective, Double-Blind, Randomized Controlled Clinical Trial. Diabetes Care 2016, 39, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Bocci, V.; Zanardi, I.; Travagli, V. The irrationality of a non-specific immunomodulation therapy used in cardiovascular diseases deserves a critical comment. Atherosclerosis 2010, 211, 38–39. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, S.; Mermi, E.U.; Zobaci, E.; Aksoy, E.; Yastı, Ç. Augmentation of arterial blood velocity with electrostimulation in patients with critical limb ischemia unsuitable for revascularization. Vascular 2017, 25, 137–141. [Google Scholar] [CrossRef]
- Dalla Paola, L.; Cimaglia, P.; Carone, A.; Boscarino, G.; Scavone, G. Use of Integra Dermal Regeneration Template for Limb Salvage in Diabetic Patients with No-Option Critical Limb Ischemia. Int. J. Low. Extrem. Wounds 2021, 20, 128–134. [Google Scholar] [CrossRef]
- Setacci, C.; de Donato, G.; Teraa, M.; Moll, F.L.; Ricco, J.B.; Becker, F.; Robert-Ebadi, H.; Cao, P.; Eckstein, H.H.; De Rango, P.; et al. Chapter IV: Treatment of critical limb ischaemia. Eur. J. Vasc. Endovasc. Surg. 2011, 42 (Suppl. 2), S43–S59. [Google Scholar] [CrossRef]
- Ho, V.T.; Gologorsky, R.; Kibrik, P.; Chandra, V.; Prent, A.; Lee, J.; Dua, A. Open, percutaneous, and hybrid deep venous arterialization technique for no-option foot salvage. J. Vasc. Surg. 2020, 71, 2152–2160. [Google Scholar] [CrossRef]
- Skóra, J.; Barć, P.; Pupka, A.; Dawiskiba, T.; Korta, K.; Albert, M.; Szyber, P. Transplantation of autologous bone marrow mononuclear cells with VEGF gene improves diabetic critical limb ischaemia. Endokrynol. Pol. 2013, 64, 129–138. [Google Scholar]
- Sengupta, S.; Gherardi, E.; Sellers, L.A.; Wood, J.M.; Sasisekharan, R.; Fan, T.P. Hepatocyte growth factor/scatter factor can induce angiogenesis independently of vascular endothelial growth factor. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 69–75. [Google Scholar] [CrossRef]
- Sadakierska-Chudy, A.; Skóra, J.; Barć, P.; Baczyńska, D.; Kasprzykowska, U.; Pupka, A.; Ussowicz, M.; Szyber, P.; Dobosz, T. Angiogenic therapy for critical lower limb ischemia. Adv. Clin. Exp. Med. 2010, 19, 347–359. [Google Scholar]
- Sadakierska-Chudy, A.; Baczyńska, D.; Skóra, J.P. Transfection Efficiency and Cytotoxicity of Transfection Reagents in Human Umbilical Vein Endothelial Cells. Adv. Clin. Exp. Med. 2008, 17, 625–634. [Google Scholar]
- Rosengart, T.K.; Bishawi, M.M.; Halbreiner, M.S.; Fakhoury, M.; Finnin, E.; Hollmann, C.; Shroyer, A.L.; Crystal, R.G. Long-term follow-up assessment of a phase 1 trial of angiogenic gene therapy using direct intramyocardial administration of an adenoviral vector expressing the VEGF121 cDNA for the treatment of diffuse coronary artery disease. Hum. Gene Ther. 2013, 24, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Barć, P.; Antkiewicz, M.; Śliwa, B.; Frączkowska, K.; Guziński, M.; Dawiskiba, T.; Małodobra-Mazur, M.; Witkiewicz, W.; Kupczyńska, D.; Strzelec, B.; et al. Double VEGF/HGF Gene Therapy in Critical Limb Ischemia Complicated by Diabetes Mellitus. J. Cardiovasc. Transl. Res. 2021, 14, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Creager, M.A.; Olin, J.W.; Belch, J.J.; Moneta, G.L.; Henry, T.D.; Rajagopalan, S.; Annex, B.H.; Hiatt, W.R. Effect of hypoxia-inducible factor-1alpha gene therapy on walking performance in patients with intermittent claudication. Circulation 2011, 124, 1765–1773. [Google Scholar] [CrossRef] [PubMed]
- Rajagopalan, S.; Olin, J.; Deitcher, S.; Pieczek, A.; Laird, J.; Grossman, P.M.; Goldman, C.K.; McEllin, K.; Kelly, R.; Chronos, N. Use of a constitutively active hypoxia-inducible factor-1alpha transgene as a therapeutic strategy in no-option critical limb ischemia patients: Phase I dose-escalation experience. Circulation 2007, 115, 1234–1243. [Google Scholar] [CrossRef]
- Grossman, P.M.; Mendelsohn, F.; Henry, T.D.; Hermiller, J.B.; Litt, M.; Saucedo, J.F.; Weiss, R.J.; Kandzari, D.E.; Kleiman, N.; Anderson, R.D.; et al. Results from a phase II multicenter, double-blind placebo-controlled study of Del-1 (VLTS-589) for intermittent claudication in subjects with peripheral arterial disease. Am. Heart J. 2007, 153, 874–880. [Google Scholar] [CrossRef]
- Hammad, T.A.; Rundback, J.; Bunte, M.; Miller, L.; Patel, P.D.; Sadanandan, S.; Fitzgerald, M.; Pastore, J.; Kashyap, V.; Henry, T.D.; et al. Stromal Cell-Derived Factor-1 Plasmid Treatment for Patients with Peripheral Artery Disease (STOP-PAD) Trial: Six-Month Results. J. Endovasc. Ther. 2020, 27, 669–675. [Google Scholar] [CrossRef]
- Mac Gabhann, F.; Qutub, A.A.; Annex, B.H.; Popel, A.S. Systems biology of pro-angiogenic therapies targeting the VEGF system. Wiley Interdiscip. Rev. Syst. Biol. Med. 2010, 2, 694–707. [Google Scholar] [CrossRef]
- Mac Gabhann, F.; Annex, B.H.; Popel, A.S. Gene therapy from the perspective of systems biology. Curr. Opin. Mol. Ther. 2010, 12, 570–577. [Google Scholar]
- Hedman, M.; Hartikainen, J.; Syvänne, M.; Stjernvall, J.; Hedman, A.; Kivelä, A.; Vanninen, E.; Mussalo, H.; Kauppila, E.; Simula, S.; et al. Safety and feasibility of catheter-based local intracoronary vascular endothelial growth factor gene transfer in the prevention of postangioplasty and in-stent restenosis and in the treatment of chronic myocardial ischemia: Phase II results of the Kuopio Angiogenesis Trial (KAT). Circulation 2003, 107, 2677–2683. [Google Scholar] [CrossRef] [PubMed]
- Isner, J.M.; Pieczek, A.; Schainfeld, R.; Blair, R.; Haley, L.; Asahara, T.; Rosenfield, K.; Razvi, S.; Walsh, K.; Symes, J.F. Clinical evidence of angiogenesis after arterial gene transfer of phVEGF165 in patient with ischaemic limb. Lancet 1996, 348, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Muona, K.; Mäkinen, K.; Hedman, M.; Manninen, H.; Ylä-Herttuala, S. 10-year safety follow-up in patients with local VEGF gene transfer to ischemic lower limb. Gene Ther. 2012, 19, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Shyu, K.G.; Chang, H.; Wang, B.W.; Kuan, P. Intramuscular vascular endothelial growth factor gene therapy in patients with chronic critical leg ischemia. Am. J. Med. 2003, 114, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Barć, P.; Antkiewicz, M.; Frączkowska-Sioma, K.; Kupczyńska, D.; Lubieniecki, P.; Witkiewicz, W.; Małodobra-Mazur, M.; Baczyńska, D.; Janczak, D.; Skóra, J.P. Two-Stage Gene Therapy (VEGF, HGF and ANG1 Plasmids) as Adjunctive Therapy in the Treatment of Critical Lower Limb Ischemia in Diabetic Foot Syndrome. Int. J. Environ. Res. Public. Health. 2022, 19, 12818. [Google Scholar] [CrossRef]
- Gu, Y.; Zhang, J.; Guo, L.; Cui, S.; Li, X.; Ding, D.; Kim, J.M.; Ho, S.H.; Hahn, W.; Kim, S. A phase I clinical study of naked DNA expressing two isoforms of hepatocyte growth factor to treat patients with critical limb ischemia. J. Gene Med. 2011, 13, 602–610. [Google Scholar] [CrossRef]
- Henry, T.D.; Hirsch, A.T.; Goldman, J.; Wang, Y.L.; Lips, D.L.; McMillan, W.D.; Duval, S.; Biggs, T.A.; Keo, H.H. Safety of a non-viral plasmid-encoding dual isoforms of hepatocyte growth factor in critical limb ischemia patients: A phase I study. Gene Ther. 2011, 18, 788–794. [Google Scholar] [CrossRef] [PubMed]
- Chauvet, S.; Burk, K.; Mann, F. Navigation rules for vessels and neurons: Cooperative signaling between VEGF and neural guidance cues. Cell. Mol. Life Sci. 2013, 70, 1685–1703. [Google Scholar] [CrossRef]
- Mukouyama, Y.S.; Shin, D.; Britsch, S.; Taniguchi, M.; Anderson, D.J. Sensory nerves determine the pattern of arterial differentiation and blood vessel branching in the skin. Cell 2002, 109, 693–705. [Google Scholar] [CrossRef]
- Mukouyama, Y.S.; Gerber, H.P.; Ferrara, N.; Gu, C.; Anderson, D.J. Peripheral nerve-derived VEGF promotes arterial differentiation via neuropilin 1-mediated positive feedback. Development 2005, 132, 941–952. [Google Scholar] [CrossRef]
- Carmeliet, P.; Tessier-Lavigne, M. Common mechanisms of nerve and blood vessel wiring. Nature 2005, 436, 193–200. [Google Scholar] [CrossRef]
- Larrivée, B.; Freitas, C.; Suchting, S.; Brunet, I.; Eichmann, A. Guidance of vascular development: Lessons from the nervous system. Circ. Res. 2009, 104, 428–441. [Google Scholar] [CrossRef] [PubMed]
| Sex | W | M | M | M | M | M | W | M | W |
|---|---|---|---|---|---|---|---|---|---|
| Age | 66 | 60 | 78 | 57 | 77 | 75 | 59 | 72 | 63 |
| Hba1c | 9.0 | 8.8 | 9.6 | 10.3 | 8.5 | 9.9 | 10.4 | 13.3 | 11.2 |
| Type of trophic changes | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 4 | 4 |
| ABI | 0.33 | 0.55 | 0.3 | 0.5 | 0.4 | 0.31 | 0.3 | 0.2 | 0.35 |
| ABI after 3 months | 0.65 | 0.9 | 0.67 | 0.72 | 0.7 | 0.6 | 0.72 | - | 0.5 |
| TcPO2 [mmHg] | 35 | 30 | 29 | 40 | 33 | 32 | 46 | 25 | 41 |
| TcPO2 after 3 months [mmHg] | 76 | 89 | 68 | 80 | 48 | 91 | 75 | - | 58 |
| Healing up to 12 weeks | Y | Y | Y | Y | N | Y | Y | N | N |
| Healing more than 12 weeks | N | N | N | N | N | N | N | N | N |
| Type of treatment | 1 | 1 | 3 | 1 | 3 | 3 | 1 | 3 | 3 |
| Patency of a venous graft after surgery | Y | Y | Y | Y | Y | Y | Y | N | Y |
| Patency of a venous graft after 3 months | Y | Y | Y | Y | N | Y | Y | N | Y |
| Stationary ulceration | N | N | N | N | Y | N | N | N | Y |
| Major amputation | N | N | N | N | N | N | N | Y | N |
| Amount of previous open surgical revascularizations | 1 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 0 |
| Amount of previous endovascular revascularizations | 3 | 1 | 2 | 2 | 1 | 3 | 4 | 1 | 2 |
| Sex | W | M | M | W | M | W | M | M |
|---|---|---|---|---|---|---|---|---|
| Age | 60 | 65 | 61 | 72 | 70 | 78 | 62 | 59 |
| Hba1c | 8.4 | 9.7 | 8.8 | 9.2 | 9.4 | 10.1 | 12.3 | 10.6 |
| Type of trophic changes | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 3 |
| ABI | 0.45 | 0.55 | 0.2 | 0.4 | 0.42 | 0.43 | 0.35 | 0.45 |
| ABI after 3 months | 0.59 | 0.7 | 0.45 | 0.66 | 0.85 | - | 0.5 | 0.64 |
| TcPO2 [mmHg] | 34 | 30 | 26 | 49 | 25 | 29 | 40 | 35 |
| TcPO2 after 3 months [mmHg] | 70 | 65 | 60 | 71 | 82 | - | 85 | 52 |
| Healing up to 12 weeks | Y | Y | N | N | Y | N | N | Y |
| Healing more than 12 weeks | N | N | N | N | N | N | N | N |
| Type of treatment | 1 | 3 | 1 | 2 | 3 | 2 | 1 | 1 |
| Patency of a venous graft after surgery | Y | Y | Y | Y | Y | N | Y | Y |
| Patency of a venous graft after 3 months | Y | Y | Y | Y | Y | N | Y | Y |
| Stationary ulceration | N | N | Y | Y | N | N | Y | N |
| Major amputation | N | N | N | N | N | Y | N | N |
| Amount of previous open surgical revascularizations | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| Amount of previous endovascular revascularizations | 2 | 3 | 2 | 1 | 4 | 5 | 4 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kupczyńska, D.; Lubieniecki, P.; Antkiewicz, M.; Barć, J.; Frączkowska-Sioma, K.; Dawiskiba, T.; Dorobisz, T.; Małodobra-Mazur, M.; Baczyńska, D.; Pańczak, K.; et al. Complementary Gene Therapy after Revascularization with the Saphenous Vein in Diabetic Foot Syndrome. Genes 2023, 14, 1968. https://doi.org/10.3390/genes14101968
Kupczyńska D, Lubieniecki P, Antkiewicz M, Barć J, Frączkowska-Sioma K, Dawiskiba T, Dorobisz T, Małodobra-Mazur M, Baczyńska D, Pańczak K, et al. Complementary Gene Therapy after Revascularization with the Saphenous Vein in Diabetic Foot Syndrome. Genes. 2023; 14(10):1968. https://doi.org/10.3390/genes14101968
Chicago/Turabian StyleKupczyńska, Diana, Paweł Lubieniecki, Maciej Antkiewicz, Jan Barć, Katarzyna Frączkowska-Sioma, Tomasz Dawiskiba, Tadeusz Dorobisz, Małgorzata Małodobra-Mazur, Dagmara Baczyńska, Konrad Pańczak, and et al. 2023. "Complementary Gene Therapy after Revascularization with the Saphenous Vein in Diabetic Foot Syndrome" Genes 14, no. 10: 1968. https://doi.org/10.3390/genes14101968
APA StyleKupczyńska, D., Lubieniecki, P., Antkiewicz, M., Barć, J., Frączkowska-Sioma, K., Dawiskiba, T., Dorobisz, T., Małodobra-Mazur, M., Baczyńska, D., Pańczak, K., Witkiewicz, W., Janczak, D., Skóra, J. P., & Barć, P. (2023). Complementary Gene Therapy after Revascularization with the Saphenous Vein in Diabetic Foot Syndrome. Genes, 14(10), 1968. https://doi.org/10.3390/genes14101968







