Alternative Genetic Diagnoses in Axenfeld–Rieger Syndrome Spectrum
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Identification of UPS9X and JAG1 Variants in Multiple Families with ARS
3.2. Identification of Variants in BCOR and CDK13 and chr X Deletion in Three Unrelated Cases
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shields, M.B. Axenfeld-Rieger syndrome: A theory of mechanism and distinctions from the iridocorneal endothelial syndrome. Trans. Am. Ophthalmol. Soc. 1983, 81, 736–784. [Google Scholar] [PubMed]
- Shields, M.B.; Buckley, E.; Klintworth, G.K.; Thresher, R. Axenfeld-Rieger syndrome. A spectrum of developmental disorders. Surv. Ophthalmol. 1985, 29, 387–409. [Google Scholar] [CrossRef] [PubMed]
- Reis, L.M.; Maheshwari, M.; Capasso, J.; Atilla, H.; Dudakova, L.; Thompson, S.; Zitano, L.; Lay-Son, G.; Lowry, R.B.; Black, J.; et al. Axenfeld-Rieger syndrome: More than meets the eye. J. Med. Genet. 2023, 60, 368–379. [Google Scholar] [CrossRef] [PubMed]
- Reis, L.M.; Tyler, R.C.; Volkmann Kloss, B.A.; Schilter, K.F.; Levin, A.V.; Lowry, R.B.; Zwijnenburg, P.J.; Stroh, E.; Broeckel, U.; Murray, J.C.; et al. PITX2 and FOXC1 spectrum of mutations in ocular syndromes. Eur. J. Hum. Genet. 2012, 20, 1224–1233. [Google Scholar] [CrossRef]
- Garza Flores, A.; Nordgren, I.; Pettersson, M.; Dias-Santagata, D.; Nilsson, D.; Hammarsjo, A.; Lindstrand, A.; Batkovskyte, D.; Wiggs, J.; Walton, D.S.; et al. Case report: Extending the spectrum of clinical and molecular findings in FOXC1 haploinsufficiency syndrome. Front. Genet. 2023, 14, 1174046. [Google Scholar] [CrossRef] [PubMed]
- Coupry, I.; Sibon, I.; Mortemousque, B.; Rouanet, F.; Mine, M.; Goizet, C. Ophthalmological features associated with COL4A1 mutations. Arch. Ophthalmol. 2010, 128, 483–489. [Google Scholar] [CrossRef]
- Sibon, I.; Coupry, I.; Menegon, P.; Bouchet, J.P.; Gorry, P.; Burgelin, I.; Calvas, P.; Orignac, I.; Dousset, V.; Lacombe, D.; et al. COL4A1 mutation in Axenfeld-Rieger anomaly with leukoencephalopathy and stroke. Ann. Neurol. 2007, 62, 177–184. [Google Scholar] [CrossRef]
- Ma, A.; Yousoof, S.; Grigg, J.R.; Flaherty, M.; Minoche, A.E.; Cowley, M.J.; Nash, B.M.; Ho, G.; Gayagay, T.; Lai, T.; et al. Revealing hidden genetic diagnoses in the ocular anterior segment disorders. Genet. Med. 2020, 22, 1623–1632. [Google Scholar] [CrossRef]
- Tanwar, M.; Dada, T.; Dada, R. Axenfeld-Rieger Syndrome Associated with Congenital Glaucoma and Cytochrome P4501B1 Gene Mutations. Case Rep. Med. 2010, 2010, 212656. [Google Scholar] [CrossRef]
- Reis, L.M.; Atilla, H.; Kannu, P.; Schneider, A.; Thompson, S.; Bardakjian, T.; Semina, E.V. Distinct Roles of Histone Lysine Demethylases and Methyltransferases in Developmental Eye Disease. Genes 2023, 14, 216. [Google Scholar] [CrossRef]
- Stathacopoulos, R.A.; Bateman, J.B.; Sparkes, R.S.; Hepler, R.S. The Rieger syndrome and a chromosome 13 deletion. J. Pediatr. Ophthalmol. Strabismus 1987, 24, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Roche, A.; Mora, J.; Perez Mdel, M.; Gean, E.; Perez, B.; O’Callaghan, M.; Catala, J.; De Torres, C.; Cruz, O.; Prat, J.; et al. Axenfeld-Rieger ocular anomaly and retinoblastoma caused by constitutional chromosome 13q deletion. Pediatr. Blood Cancer 2010, 54, 480–482. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, K.; Yamane, S.; Shiota, H.; Naito, E. A case of retinoblastoma associated with Rieger’s anomaly and 13q deletion. Jpn. J. Ophthalmol. 1981, 25, 321–325. [Google Scholar]
- Riise, R.; D’Haene, B.; De Baere, E.; Gronskov, K.; Brondum-Nielsen, K. Rieger syndrome is not associated with PAX6 deletion: A correction to Acta Ophthalmol Scand 2001: 79: 201–203. Acta Ophthalmol. 2009, 87, 923. [Google Scholar] [CrossRef] [PubMed]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef] [PubMed]
- Riggs, E.R.; Andersen, E.F.; Cherry, A.M.; Kantarci, S.; Kearney, H.; Patel, A.; Raca, G.; Ritter, D.I.; South, S.T.; Thorland, E.C.; et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet. Med. 2020, 22, 245–257. [Google Scholar] [CrossRef]
- Jolly, L.A.; Taylor, V.; Wood, S.A. USP9X enhances the polarity and self-renewal of embryonic stem cell-derived neural progenitors. Mol. Biol. Cell 2009, 20, 2015–2029. [Google Scholar] [CrossRef]
- Hamilton, M.J.; Caswell, R.C.; Canham, N.; Cole, T.; Firth, H.V.; Foulds, N.; Heimdal, K.; Hobson, E.; Houge, G.; Joss, S.; et al. Heterozygous mutations affecting the protein kinase domain of CDK13 cause a syndromic form of developmental delay and intellectual disability. J. Med. Genet. 2018, 55, 28–38. [Google Scholar] [CrossRef]
- Jolly, L.A.; Parnell, E.; Gardner, A.E.; Corbett, M.A.; Perez-Jurado, L.A.; Shaw, M.; Lesca, G.; Keegan, C.; Schneider, M.C.; Griffin, E.; et al. Missense variant contribution to USP9X-female syndrome. NPJ Genom. Med. 2020, 5, 53. [Google Scholar] [CrossRef]
- Reijnders, M.R.; Zachariadis, V.; Latour, B.; Jolly, L.; Mancini, G.M.; Pfundt, R.; Wu, K.M.; van Ravenswaaij-Arts, C.M.; Veenstra-Knol, H.E.; Anderlid, B.M.; et al. De Novo Loss-of-Function Mutations in USP9X Cause a Female-Specific Recognizable Syndrome with Developmental Delay and Congenital Malformations. Am. J. Hum. Genet. 2016, 98, 373–381. [Google Scholar] [CrossRef]
- Seo, S.; Singh, H.P.; Lacal, P.M.; Sasman, A.; Fatima, A.; Liu, T.; Schultz, K.M.; Losordo, D.W.; Lehmann, O.J.; Kume, T. Forkhead box transcription factor FoxC1 preserves corneal transparency by regulating vascular growth. Proc. Natl. Acad. Sci. USA 2012, 109, 2015–2020. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Orozco, C.; Boyer, J.; Leglise, M.; Goodale, J.; Batalov, S.; Hodge, C.L.; Haase, J.; Janes, J.; Huss, J.W., III; et al. BioGPS: An extensible and customizable portal for querying and organizing gene annotation resources. Genome Biol. 2009, 10, R130. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, C.P.; Jernigan, K.K.; Diggins, N.L.; Webb, D.J.; MacGurn, J.A. USP9X Deubiquitylates DVL2 to Regulate WNT Pathway Specification. Cell Rep. 2019, 28, 1074–1089.e1075. [Google Scholar] [CrossRef]
- Premarathne, S.; Murtaza, M.; Matigian, N.; Jolly, L.A.; Wood, S.A. Loss of Usp9x disrupts cell adhesion, and components of the Wnt and Notch signaling pathways in neural progenitors. Sci. Rep. 2017, 7, 8109. [Google Scholar] [CrossRef] [PubMed]
- Hendee, K.E.; Sorokina, E.A.; Muheisen, S.S.; Reis, L.M.; Tyler, R.C.; Markovic, V.; Cuturilo, G.; Link, B.A.; Semina, E.V. PITX2 deficiency and associated human disease: Insights from the zebrafish model. Hum. Mol. Genet. 2018, 27, 1675–1695. [Google Scholar] [CrossRef]
- Reis, L.M.; Houssin, N.S.; Zamora, C.; Abdul-Rahman, O.; Kalish, J.M.; Zackai, E.H.; Plageman, T.F., Jr.; Semina, E.V. Novel variants in CDH2 are associated with a new syndrome including Peters anomaly. Clin. Genet. 2020, 97, 502–508. [Google Scholar] [CrossRef]
- Ayoub, M.D.; Kamath, B.M. Alagille Syndrome: Current Understanding of Pathogenesis, and Challenges in Diagnosis and Management. Clin. Liver Dis. 2022, 26, 355–370. [Google Scholar] [CrossRef]
- da Palma, M.M.; Igelman, A.D.; Ku, C.; Burr, A.; You, J.Y.; Place, E.M.; Wang, N.K.; Oh, J.K.; Branham, K.E.; Zhang, X.; et al. Characterization of the Spectrum of Ophthalmic Changes in Patients With Alagille Syndrome. Investig. Ophthalmol. Vis. Sci. 2021, 62, 27. [Google Scholar] [CrossRef]
- Hingorani, M.; Nischal, K.K.; Davies, A.; Bentley, C.; Vivian, A.; Baker, A.J.; Mieli-Vergani, G.; Bird, A.C.; Aclimandos, W.A. Ocular abnormalities in Alagille syndrome. Ophthalmology 1999, 106, 330–337. [Google Scholar] [CrossRef]
- Le Caignec, C.; Lefevre, M.; Schott, J.J.; Chaventre, A.; Gayet, M.; Calais, C.; Moisan, J.P. Familial deafness, congenital heart defects, and posterior embryotoxon caused by cysteine substitution in the first epidermal-growth-factor-like domain of jagged 1. Am. J. Hum. Genet. 2002, 71, 180–186. [Google Scholar] [CrossRef]
- van den Akker, W.M.R.; Brummelman, I.; Martis, L.M.; Timmermans, R.N.; Pfundt, R.; Kleefstra, T.; Willemsen, M.H.; Gerkes, E.H.; Herkert, J.C.; van Essen, A.J.; et al. De novo variants in CDK13 associated with syndromic ID/DD: Molecular and clinical delineation of 15 individuals and a further review. Clin. Genet. 2018, 93, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Ng, D.; Thakker, N.; Corcoran, C.M.; Donnai, D.; Perveen, R.; Schneider, A.; Hadley, D.W.; Tifft, C.; Zhang, L.; Wilkie, A.O.; et al. Oculofaciocardiodental and Lenz microphthalmia syndromes result from distinct classes of mutations in BCOR. Nat. Genet. 2004, 36, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Ragge, N.; Isidor, B.; Bitoun, P.; Odent, S.; Giurgea, I.; Cogne, B.; Deb, W.; Vincent, M.; Le Gall, J.; Morton, J.; et al. Expanding the phenotype of the X-linked BCOR microphthalmia syndromes. Hum. Genet. 2019, 138, 1051–1069. [Google Scholar] [CrossRef] [PubMed]
- Lozic, B.; Ljubkovic, J.; Panduric, D.G.; Saltvig, I.; Kutsche, K.; Krzelj, V.; Zemunik, T. Oculo-facio-cardio-dental syndrome in three succeeding generations: Genotypic data and phenotypic features. Braz. J. Med. Biol. Res. 2012, 45, 1315–1319. [Google Scholar] [CrossRef]
- Verma, G.; Singh, G.K.; Tandon, P.; Verma, S.L. A rare syndrome with unusual dental findings: Oculo-facio-cardio-dental syndrome. J. Oral. Maxillofac. Pathol. 2014, 18, 331. [Google Scholar] [CrossRef]
- Wimplinger, I.; Morleo, M.; Rosenberger, G.; Iaconis, D.; Orth, U.; Meinecke, P.; Lerer, I.; Ballabio, A.; Gal, A.; Franco, B.; et al. Mutations of the mitochondrial holocytochrome c-type synthase in X-linked dominant microphthalmia with linear skin defects syndrome. Am. J. Hum. Genet. 2006, 79, 878–889. [Google Scholar] [CrossRef]
- Weh, E.; Reis, L.M.; Happ, H.C.; Levin, A.V.; Wheeler, P.G.; David, K.L.; Carney, E.; Angle, B.; Hauser, N.; Semina, E.V. Whole exome sequence analysis of Peters anomaly. Hum. Genet. 2014, 133, 1497–1511. [Google Scholar] [CrossRef]
- Lagerstrom, M.; Dahl, N.; Nakahori, Y.; Nakagome, Y.; Backman, B.; Landegren, U.; Pettersson, U. A deletion in the amelogenin gene (AMG) causes X-linked amelogenesis imperfecta (AIH1). Genomics 1991, 10, 971–975. [Google Scholar] [CrossRef]
| Individual | Ocular | Other | Gene | Variant | ACMG Criteria |
|---|---|---|---|---|---|
| 1 | ARA, GL, MY | Mild delay but normal cognition, dysmorphic facial features, palate anomaly, choanal atresia, lines of Blaschko, precocious puberty | USP9X | NM_001039590.2: c.1314+2T>C | LP: PVS1, PM2_supp |
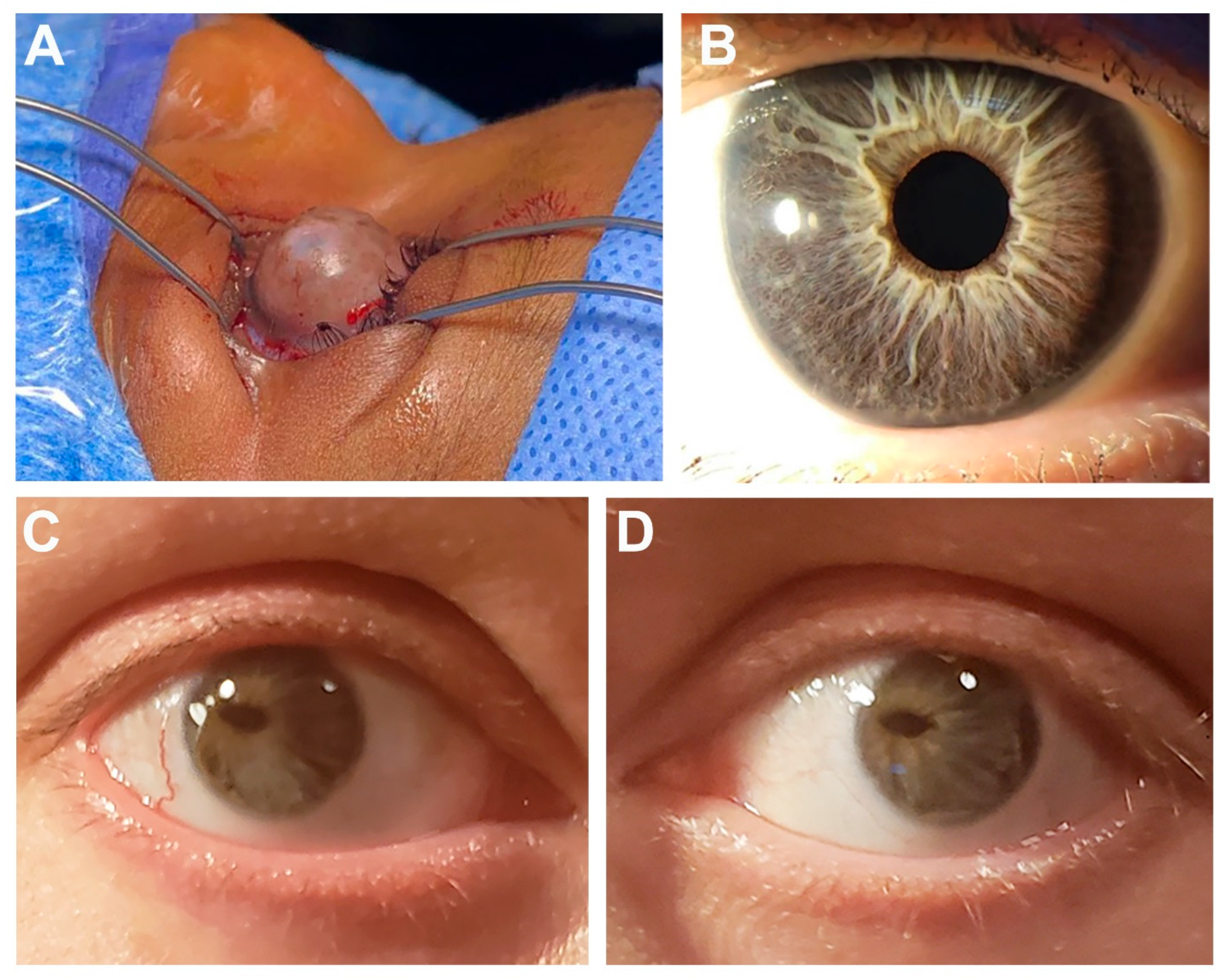
| 2 | Left: ASD, severe IH, CAT, buphthalmos, corneal neovascularization, corneal ectasia with perforation Right: corneal ulcer/scarring, MY, iris hypopigmentation | DA, HL, dysmorphic facial features, CHD, Dandy–Walker malformation, hip dysplasia, umbilical hernia, global delay, short stature | USP9X | c.121G>T; p.(Glu41*) | LP: PVS1, PM2_supp |
| 3 | Corneal scarring/neovascularization, CAT, MY | DA, dysmorphic facial features, CHD, hip dysplasia, feeding difficulties, palate anomaly, vesicoureteral reflux, skin pigment anomaly, scoliosis, gross motor delay but normal cognition | USP9X | c.1603dupA p.(Ile535Asnfs*11) | LP: PVS1, PM2_supp |
| 4 | ARA | DA, dysmorphic facial features, HL, connective tissue anomaly, arachnodactyly | JAG1 | NM_000214.3:c.59dupT p.(Leu21Alafs*52) | LP: PVS1, PM2_supp |
| 5 | ARA, MY | DA, HL, CHD, liver dysfunction, pituitary macroadenoma (prolactinoma) | JAG1 | Gene deletion: 3.01 Mb deletion of 20:10256130-13269324 (hg19) | P: 2A |
| 6 | ARA, CGL, corectopia, HY | DA, heart murmur, PCOS | JAG1 | NM_000214.3: c.2419G>T p.(Glu807*) | P: PVS1, PM2_supp, PP1 |
| 7 | ARA, megalocornea | Dysmorphic facial features, cognitive impairment | CDK13 | NM_003718.5:c.2252G>A p.(Arg751Gln) | LP: PS1, PM1, PM2_supp, PP3 |
| 8 | GL, CAT, ONH, mild MI | DA, HL, dysmorphic facial features, RU, CHD, palate anomaly | BCOR | NM_001123385.2:c.3350_3360dup p.(Ala1121Glnfs*42) | LP: PVS1, PM2_supp |
| 9 | CGL, IH, polycoria, CAT, mild MI | DA, HL, rheumatoid arthritis, connective tissue anomaly | HCCS and AMELX | Gene deletions: 4.08 Mb deletion of X:7370404-11445756 (hg19) | P: 2A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reis, L.M.; Amor, D.J.; Haddad, R.A.; Nowak, C.B.; Keppler-Noreuil, K.M.; Chisholm, S.A.; Semina, E.V. Alternative Genetic Diagnoses in Axenfeld–Rieger Syndrome Spectrum. Genes 2023, 14, 1948. https://doi.org/10.3390/genes14101948
Reis LM, Amor DJ, Haddad RA, Nowak CB, Keppler-Noreuil KM, Chisholm SA, Semina EV. Alternative Genetic Diagnoses in Axenfeld–Rieger Syndrome Spectrum. Genes. 2023; 14(10):1948. https://doi.org/10.3390/genes14101948
Chicago/Turabian StyleReis, Linda M., David J. Amor, Raad A. Haddad, Catherine B. Nowak, Kim M. Keppler-Noreuil, Smith Ann Chisholm, and Elena V. Semina. 2023. "Alternative Genetic Diagnoses in Axenfeld–Rieger Syndrome Spectrum" Genes 14, no. 10: 1948. https://doi.org/10.3390/genes14101948
APA StyleReis, L. M., Amor, D. J., Haddad, R. A., Nowak, C. B., Keppler-Noreuil, K. M., Chisholm, S. A., & Semina, E. V. (2023). Alternative Genetic Diagnoses in Axenfeld–Rieger Syndrome Spectrum. Genes, 14(10), 1948. https://doi.org/10.3390/genes14101948






