Clinical Presentation and Characteristics of the Upper Extremity in Patients with Musculocontractural Ehlers–Danlos Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Protocol
2.3. Radiological Measurement
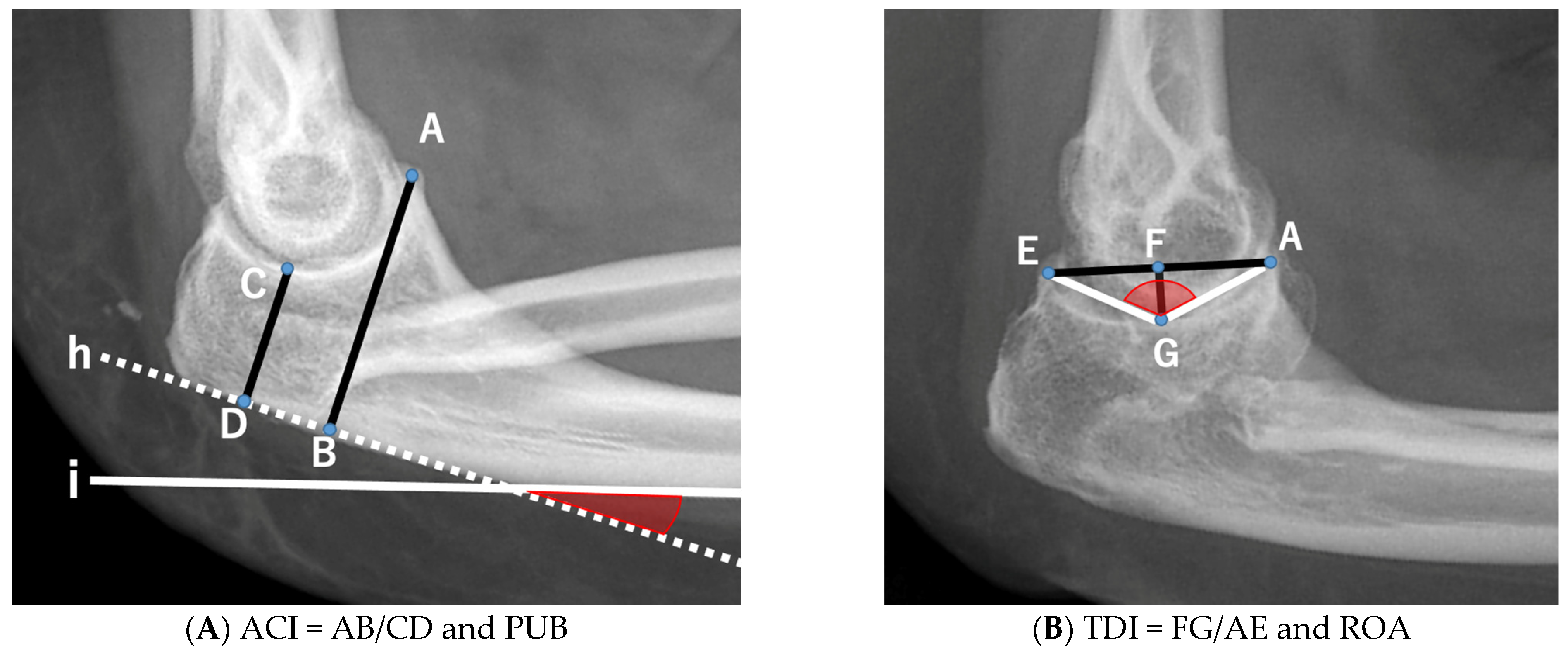
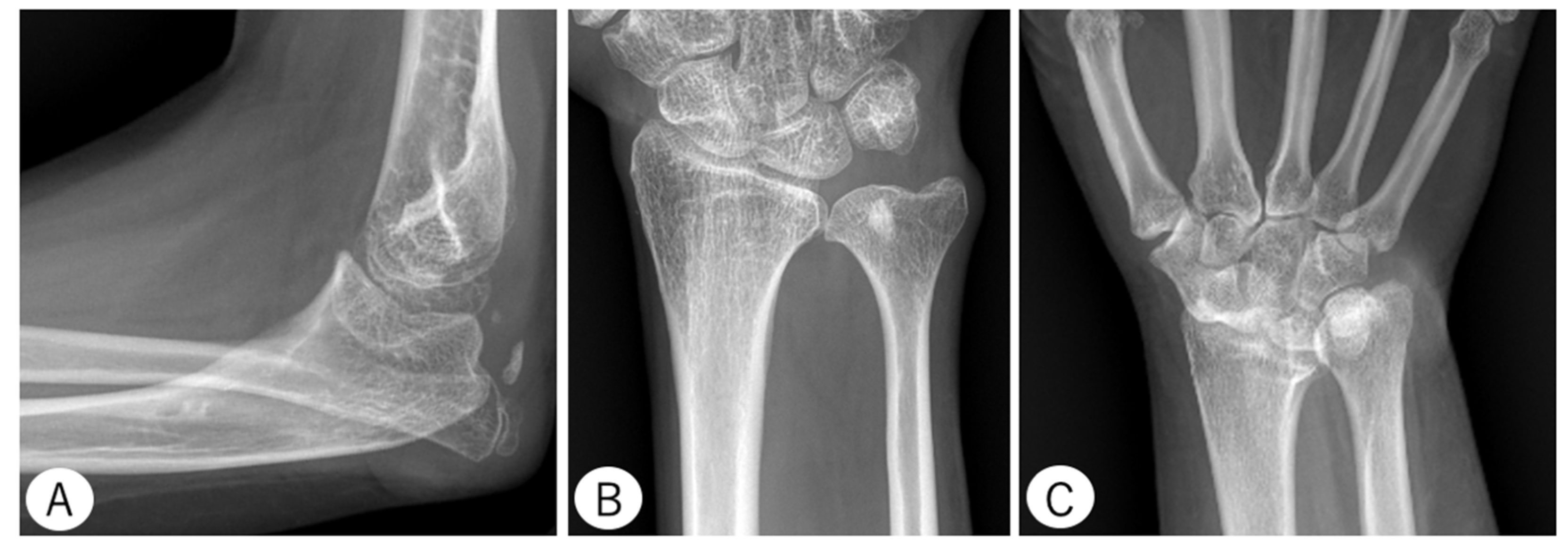
2.3.1. Elbow
- Anterior Coverage Index (ACI): defined as the ratio between the coronoid height (point A to B) and the minimal proximal ulna trochlear height (C to D).
- Trochlear Depth Index (TDI): defined as the ratio between the proximal ulna trochlear notch depth (F to G) and olecranon–coronoid distance (A to E).
- Proximal Ulnar Bow (PUB): defined as the angle between the ulnar diaphysis and olecranon.
- Radiographic Opening Angle (ROA): defined as the angle between lines from the deepest point of the trochlear notch to coronoid (A to G) and olecranon (G to E).
2.3.2. Wrist
2.3.3. Hand
3. Results
3.1. Medical Examination and Consultation
3.2. Radiological Examination
3.3. QuickDASH Patient-Reported Outcome Measure for Assessing the Upper Extremity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 8–26. [Google Scholar] [CrossRef]
- Kosho, T.; Miyake, N.; Mizumoto, S.; Hatamochi, A.; Fukushima, Y.; Yamada, S.; Sugahara, K.; Matsumoto, N. A response to: Loss of dermatan-4-sulfotransferase 1 (D4ST1/CHST14) function represents the first dermatan sulfate biosynthesis defect, “dermatan sulfate-deficient Adducted Thumb-Clubfoot Syndrome”. Which name is appropriate, “Adducted Thumb-Clubfoot Syndrome” or “Ehlers-Danlos syndrome”? Hum. Mutat. 2011, 32, 1507–1509. [Google Scholar]
- Kosho, T. CHST14/D4ST1 deficiency: New form of Ehlers-Danlos syndrome. Pediatr. Int. 2016, 58, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Brady, A.F.; Demirdas, S.; Fournel-Gigleux, S.; Ghali, N.; Giunta, C.; Kapferer-Seebacher, I.; Kosho, T.; Mendoza-Londono, R.; Pope, M.F.; Rohrbach, M.; et al. The Ehlers-Danlos syndromes, rare types. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 70–115. [Google Scholar] [CrossRef]
- Minatogawa, M.; Hirose, T.; Mizumoto, S.; Yamaguchi, T.; Nagae, C.; Taki, M.; Yamada, S.; Watanabe, T.; Kosho, T. Clinical and pathophysiological delineation of musculocontractural Ehlers-Danlos syndrome caused by dermatan sulfate epimerase deficiency (mcEDS-DSE): A detailed and comprehensive glycobiological and pathological investigation in a novel patient. Hum. Mutat. 2022. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mathiowetz, V.; Kashman, N.; Volland, G.; Weber, K.; Dowe, M.; Rogers, S. Grip and pinch strength: Normative data for adults. Arch. Phys. Med. Rehabil. 1985, 66, 69–74. [Google Scholar] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand). The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Beaton, D.E.; Wright, J.G.; Katz, J.N.; Group, U.E.C. Development of the QuickDASH: Comparison of three item-reduction approaches. J. Bone Jt. Surg. Am. 2005, 87, 1038–1046. [Google Scholar]
- Imaeda, T.; Toh, S.; Wada, T.; Uchiyama, S.; Okinaga, S.; Kusunose, K.; Sawaizumi, T. Validation of the Japanese Society for Surgery of the Hand Version of the Quick Disability of the Arm, Shoulder, and Hand (QuickDASH-JSSH) questionnaire. J. Orthop. Sci. 2006, 11, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Luceri, F.; Cucchi, D.; Rosagrata, E.; Zaolino, E.C.; Viganò, M.; Girolamo, L.; Zagarella, A.; Catapano, M.; Gallazzi, M.B.; Arrigoni, P.A.; et al. Novel Radiographic Indexes for Elbow Stability Assessment: Part A—Cadaveric Validation. Indian J. Orthop. 2021, 55, 336–346. [Google Scholar] [CrossRef]
- Kilgus, S.; Eder, C.; Siegert, P.; Moroder, P.; Zimmermann, E.; Thiele, K. The inter--individual anatomical variation of the trochlear notch as a predisposition for simple elbow dislocation. Arch. Orthop. Trauma Surg. 2021. Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Gartland, J.J.; Werley, C.W. Evaluation of healed Colles’ fractures. J. Bone Jt. Surg. Am. 1951, 33, 895–907. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Langer, M.F.; Wieskötter, B.; Hartensuer, R.; Kösters, C.; Oeckenpöhler, S. Ligament reconstruction in extensor tendon dislocation. Oper. Orthop. Traumatol. 2015, 27, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Niu, K.; Momma, H.; Kobayashi, Y. Breakfast consumption frequency is associated with grip strength in a population of healthy Japanese adults. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Isobe, F.; Nakamura, K.; Yamazaki, H.; Hayashi, M.; Itsubo, T.; Komatsu, M.; Uchiyama, S.; Takahashi, J. Difficult closed reduction of elbow dislocations: Two case reports from a multicenter retrospective chart review. JSES Rev. Rep. Tech. 2022, 2, 113–116. [Google Scholar] [CrossRef]
- King, T. Recurrent dislocation of the elbow. J. Bone Jt. Surg. Br. 1953, 35, 50–54. [Google Scholar] [CrossRef]
- Shanwen, Z.; Canjun, Z.; Song, Y. Reconstruction of coronoid process of the ulna: A literature review. J. Int. Med. Res. 2021, 49, 3000605211008323. [Google Scholar]
- Seki, A.; Olsen, B.S.; Jensen, S.L.; Eygendaal, D.; Sojbjerg, J.O. Functional anatomy of the lateral collateral ligament complex of the elbow: Configuration of Y and its role. J. Shoulder Elb. Surg. 2002, 11, 53–59. [Google Scholar] [CrossRef]
- Hull, J.R.; Owen, J.R.; Fern, S.E.; Wayne, J.S.; Boardman, N.D., III. Role of the coronoid process in varus osteoarticular stability of the elbow. J. Shoulder Elbow Surg. 2005, 14, 441–446. [Google Scholar] [CrossRef]
- Liu, R.; Miao, W.; Mu, M.; Wu, G.; Qu, J.; Wu, Y. Ulnar Rotation Osteotomy for Congenital Radial Head Dislocation. J. Hand Surg Am. 2015, 40, 1769–1775. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, K.; Kato, H.; Ikegami, S.; Hayashi, M.; Hashimoto, S.; Sakai, N.; Takahashi, J.; Taneichi, H. Prevalence and associated factors of primary elbow osteoarthritis in the Japanese general elderly population: A Japanese cohort survey randomly sampled from a basic resident registry. J. Shoulder Elbow Surg. 2022, 31, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Carlson, D.H. Coalition of the carpal bones. Skelet. Radiol. 1981, 7, 125–127. [Google Scholar] [CrossRef]
- O’Rahilly, R. A survey of carpal and tarsal anomalies. J. Bone Jt. Surg. Am. 1953, 35, 626–642. [Google Scholar] [CrossRef]
- Kimura, K. Radiological Studies on Three Finger Formulae. J. Anthrop. Soc. Nippon. 1965, 72, 146–162. [Google Scholar] [CrossRef][Green Version]
- Kosho, T.; Miyake, N.; Hatamochi, A.; Takahashi, J.; Kato, H.; Miyahara, T.; Igawa, Y.; Yasui, H.; Ishida, T.; Ono, K.; et al. A new Ehlers-Danlos syndrome with craniofacial characteristics, multiple congenital contractures, progressive joint and skin laxity, and multisystem fragility-related manifestations. Am. J. Med. Genet. Part A 2010, 152, 1333–1346. [Google Scholar] [CrossRef]
- Kosho, T.; Takahashi, J.; Ohashi, H.; Nishimura, G.; Kato, H.; Fukushima, Y. Ehlers-Danlos syndrome type VIB with characteristic facies, decreased curvatures of the spinal column, and joint contractures in two unrelated girls. Am. J. Med. Genet. Part A 2005, 138, 282–287. [Google Scholar] [CrossRef] [PubMed]


| Average Age (Years) | 21 (4–45) |
|---|---|
| Sex | |
| Female | 7 |
| Male | 6 |
| History of fracture | |
| Yes | 1 |
| No | 12 |
| History of dislocation | |
| Yes | 12 |
| No | 1 |
| Dislocation site | |
| Shoulder | 11 |
| Elbow | 2 |
| Hip | 0 |
| Patella | 7 |
| Question No. | Item |
|---|---|
| 1 | Open a tight or new jar |
| 2 | Do heavy household tasks (e.g., wash walls, wash floors) |
| 3 | Carry a shopping bag or briefcase |
| 4 | Wash your back |
| 5 | Use a knife to cut food |
| 6 | Recreational activities which require little effort (e.g., golf, hammering, tennis, etc.) |
| 7 | During the past week, to what extent has your arm, shoulder, or hand problem interfered with your normal social activities with family, friends, neighbors, or groups? |
| 8 | During the past week, were you limited in your work or other daily activities as a result of your arm, shoulder, or hand problem? |
| 9 | Arm, shoulder, or hand pain |
| 10 | Tingling (pins and needles) in your arm, shoulder, or hand |
| 11 | During the past week, how much difficulty have you had sleeping because of the pain in your arm, shoulder, or hand? |
| Patient | Age | Sex | Elbow | Wrist | |||||
|---|---|---|---|---|---|---|---|---|---|
| ACI | TDI | PUB | ROA | RD | VT | UV | |||
| 1 | 4 | F | 1.36 | - | 19.4 | - | - | - | - |
| 2 | 6 | M | 1.58 | - | 2.5 | - | - | - | - |
| 3 | 11 | M | 2.01 | - | 18.4 | - | 20.2 | 13.9 | −0.1 |
| 4 | 12 | F | 1.48 | 0.38 | 2.0 | 106 | 20.2 | 13.9 | 0.9 |
| 5 | 14 | M | 1.80 | 0.39 | 9.0 | 101 | 20.3 | 9.0 | −1.9 |
| 6 | 16 | F | 1.40 | 0.32 | 10.0 | 113 | 27.0 | 15.5 | 0 |
| 7 | 18 | M | 1.96 | 0.40 | 0 | 104 | 27.7 | 18.3 | −1.2 |
| 8 | 22 | M | 2.18 | 0.46 | 10.7 | 92 | 27.8 | 24.8 | 0 |
| 9 | 24 | F | 1.83 | 0.46 | 16.8 | 85 | 22.9 | 23.6 | 0.8 |
| 10 | 28 | F | 1.60 | 0.33 | 19.9 | 110 | 31.1 | 27.9 | 2.8 |
| 11 | 31 | F | 1.72 | 0.33 | 21.4 | 113 | 28.0 | 23.7 | 7.7 |
| 12 | 39 | M | 1.78 | 0.51 | 4.5 | 86 | 23.0 | 12.9 | 1.0 |
| 13 | 45 | F | 1.38 | 0.30 | 14.5 | 116 | 22.3 | 17.4 | 3.2 |
| Males (n = 3) | Females (n = 4) | |||||
|---|---|---|---|---|---|---|
| Length | Width | Length | Width | |||
| I | Metacarpal | 47.3 | 7.8 | 43.5 | 7.4 | |
| Phalanx | proximal | 27.3 | 5.5 | 27.4 | 5.5 | |
| distal | 20.4 | 3.7 | 18.7 | 3.1 | ||
| II | Metacarpal | 64.4 | 7.7 | 59.8 | 6.8 | |
| Phalanx | proximal | 37.3 | 6.8 | 36.4 | 6.6 | |
| middle | 21.2 | 4.9 | 21.1 | 4.6 | ||
| distal | 14.4 | 3.1 | 14.7 | 2.8 | ||
| III | Metacarpal | 63.0 | 6.6 | 56.1 | 6.1 | |
| Phalanx | proximal | 43.5 | 7.2 | 39.8 | 6.0 | |
| middle | 24.5 | 5.4 | 24.0 | 4.7 | ||
| distal | 16.0 | 3.4 | 15.9 | 3.1 | ||
| IV | Metacarpal | 56.4 | 5.6 | 51.8 | 5.5 | |
| Phalanx | proximal | 40.4 | 6.0 | 37.7 | 5.4 | |
| middle | 23.7 | 4.7 | 23.3 | 4.4 | ||
| distal | 16.6 | 3.0 | 16.0 | 3.3 | ||
| V | Metacarpal | 51.5 | 6.1 | 49.0 | 5.7 | |
| Phalanx | proximal | 31.4 | 5.3 | 29.9 | 4.8 | |
| middle | 16.3 | 3.7 | 16.4 | 3.6 | ||
| distal | 13.8 | 2.2 | 13.1 | 2.3 | ||
| Year | Number of Patients | Width of Medullary Cavity (mm) | Ratio of Medullary Cavity of the Metacarpal Bone |
|---|---|---|---|
| Under 12 | 3 | 2.5 | 0.52 |
| 12 | 1 | 3.1 | 0.44 |
| 14 | 1 | 3.6 | 0.55 |
| 16 | 1 | 1.0 | 0.15 |
| 18 | 1 | 1.1 | 0.21 |
| 20–29 | 3 | 2.1 | 0.33 |
| 30–39 | 2 | 2.4 | 0.31 |
| 40–49 | 1 | 1.8 | 0.29 |
| Patient | QuickDASH Score | Component of QuickDASH | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
| 1 | 37.5 | 5 | - | 3 | 5 | 2 | 5 | 1 | 1 | 1 | 1 | 1 |
| 2 | 47.7 | 4 | 4 | 3 | 4 | 4 | 3 | 3 | 4 | 1 | 1 | 1 |
| 3 | 34.1 | 5 | 4 | 3 | 4 | 2 | 1 | 2 | 2 | 1 | 1 | 1 |
| 4 | 36.4 | 5 | 4 | 4 | 4 | 2 | 1 | 2 | 2 | 1 | 1 | 1 |
| 5 | 54.5 | 5 | 4 | 4 | 5 | 2 | 2 | 4 | 5 | 2 | 1 | 1 |
| 6 | 52.3 | 5 | 5 | 5 | 4 | 1 | 1 | 5 | 2 | 1 | 4 | 1 |
| 7 | 18.2 | 3 | 2 | 2 | 1 | 3 | 1 | 2 | 2 | 1 | 1 | 1 |
| 8 | 4.5 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| 9 | 31.8 | 5 | 3 | 3 | 1 | 3 | 1 | 2 | 1 | 3 | 2 | 1 |
| 10 | 50 | 5 | 4 | 4 | 4 | 3 | 2 | 3 | 3 | 2 | 1 | 2 |
| 11 | 31.8 | 5 | 3 | 3 | 2 | 3 | 1 | 2 | 2 | 2 | 1 | 1 |
| 12 | 15.9 | 2 | 1 | 2 | 5 | 1 | 1 | 1 | 1 | 2 | 1 | 1 |
| 13 | 34.1 | 5 | 4 | 3 | 1 | 2 | 1 | 4 | 3 | 1 | 1 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Isobe, F.; Hayashi, M.; Kobayashi, R.; Nakamura, M.; Kosho, T.; Takahashi, J. Clinical Presentation and Characteristics of the Upper Extremity in Patients with Musculocontractural Ehlers–Danlos Syndrome. Genes 2022, 13, 1978. https://doi.org/10.3390/genes13111978
Isobe F, Hayashi M, Kobayashi R, Nakamura M, Kosho T, Takahashi J. Clinical Presentation and Characteristics of the Upper Extremity in Patients with Musculocontractural Ehlers–Danlos Syndrome. Genes. 2022; 13(11):1978. https://doi.org/10.3390/genes13111978
Chicago/Turabian StyleIsobe, Fumihiro, Masanori Hayashi, Rena Kobayashi, Manami Nakamura, Tomoki Kosho, and Jun Takahashi. 2022. "Clinical Presentation and Characteristics of the Upper Extremity in Patients with Musculocontractural Ehlers–Danlos Syndrome" Genes 13, no. 11: 1978. https://doi.org/10.3390/genes13111978
APA StyleIsobe, F., Hayashi, M., Kobayashi, R., Nakamura, M., Kosho, T., & Takahashi, J. (2022). Clinical Presentation and Characteristics of the Upper Extremity in Patients with Musculocontractural Ehlers–Danlos Syndrome. Genes, 13(11), 1978. https://doi.org/10.3390/genes13111978








