Quality of Life Scores Remained Different among the Genotypic Groups of Patients with Suspected Hemochromatosis, Even after Treatment Period
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. SF-36 Health Survey
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Brissot, P.; Pietrangelo, A.; Adams, P.C.; Graaff, B.; De McLaren, C.E.; Loreál, O. Haemochromatosis. Nat. Rev. Dis. Prim. 2018, 4, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Radford-Smith, D.E.; Powell, E.E.; Powell, L.W. Haemochromatosis: A clinical update for the practising physician. Intern. Med. J. 2018, 48, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Brissot, P.; Troadec, M.-B.; Loréal, O.; Brissot, E. Pathophysiology and classification of iron overload diseases; update 2018. Transfus. Clin. Biol. 2019, 26, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.C.J.L.; Krieger, J.E.; Pereira, A.C. Molecular Diagnostic and Pathogenesis of Hereditary Hemochromatosis. Int. J. Mol. Sci. 2012, 13, 1497–1511. [Google Scholar] [CrossRef]
- Pilling, L.C.; Tamosauskaite, J.; Jones, G.; Wood, A.R.; Jones, L.; Kuo, C.L.; Kuchel, G.A.; Ferrucci, L.; Melzer, D. Common conditions associated with hereditary haemochromatosis genetic variants: Cohort study in UK Biobank. BMJ 2019, 364, 5222. [Google Scholar] [CrossRef]
- Brissot, P.; Loréal, O. Iron metabolism and related genetic diseases: A cleared land, keeping mysteries. J. Hepatol. 2016, 64, 505–515. [Google Scholar] [CrossRef]
- Pietrangelo, A. Non-HFE hemochromatosis. Semin. Liver Dis. 2005, 25, 450–460. [Google Scholar] [CrossRef]
- Adams, P.; Altes, A.; Brissot, P.; Butzeck, B.; Cabantchik, I.; Cançado, R.; Distante, S.; Evans, P.; Evans, R.; Ganz, T.; et al. Therapeutic recommendations in HFE hemochromatosis for p.Cys282Tyr (C282Y/C282Y) homozygous genotype. Hepatol. Int. 2018, 12, 83–86. [Google Scholar] [CrossRef]
- WHO. The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]
- Rogerson, R.J. Environmental and health-related quality of life: Conceptual and methodological similarities. Soc. Sci. Med. 1995, 41, 1373–1382. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 205031211667172. [Google Scholar] [CrossRef]
- Ciconelli, R.M.; Ferraz, M.B.; Santos, W.; Meinão, I.; Quaresma, M.R. Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36). Rev. Bras Reum. 1999, 39, 143–150. [Google Scholar]
- Fonseca, P.F.; Cançado, R.D.; Naoum, F.A.; Dinardo, C.L.; Fonseca, G.H.; Gualandro, S.F.; Krieger, J.E.; Pereira, A.C.; Brissot, P.; Santos, P.C. Quality of life scores differs between genotypic groups of patients with suspected hereditary hemochromatosis. BMC Med. Genet. 2018, 19, 3. [Google Scholar] [CrossRef]
- Fonseca, P.F.S.; Cançado, R.D.; Uellendahl Lopes, M.M.; Correia, E.; Lescano, M.A.; Santos, P.C.J.L. HAMP Gene Mutation Associated with Juvenile Hemochromatosis in Brazilian Patients. Acta Haematol. 2016, 135, 228–231. [Google Scholar] [CrossRef]
- De Lima Santos, P.C.; Pereira, A.C.; Cançado, R.D.; Schettert, I.T.; Hirata, R.D.; Hirata, M.H.; Figueiredo, M.S.; Chiattone, C.S.; Krieger, J.E.; Guerra-Shinohara, E.M. Hemojuvelin and Hepcidin Genes Sequencing in Brazilian Patients with Primary Iron Overload. Genet. Test. Mol. Biomark. 2010, 14, 803–806. [Google Scholar] [CrossRef]
- Martinez-Martin, P. What is quality of life and how do we measure it? Relevance to Parkinson’s disease and movement disorders. Mov. Disord. 2017, 32, 382–392. [Google Scholar] [CrossRef]
- Pan, Y.; Barnhart, H.X. Methods for assessing the reliability of quality of life based on SF-36. Stat. Med. 2016, 35, 5656–5665. [Google Scholar] [CrossRef]
- Ware, J.E.; Snow, K.K.; Kosinski, M.; Gandek, B. SF-36 Health Survey: Manual and Interpretation Guide; Health Institute, New England Medical Center: Boston, MA, USA, 1993. [Google Scholar]
- De Graaff, B.; Neil, A.; Sanderson, K.; Yee, K.C.; Palmer, A.J. Quality of life utility values for hereditary haemochromatosis in Australia. Health Qual. Life Outcomes 2016, 14, 31. [Google Scholar] [CrossRef]
- Van der Plas, S.M.; Hansen, B.E.; de Boer, J.B.; Stijnen, T.; Passchier, J.; Rob, A.; Schalm, S.W. Generic and disease-specific health related quality of life of liver patients with various aetiologies: A survey. Qual. Life Res. 2007, 16, 375–388. [Google Scholar] [CrossRef]
- Shaheen, N.J.; Lawrence, L.B.; Bacon, B.R.; Barton, J.C.; Barton, N.H.; Galanko, J.; Martin, C.F.; Burnett, C.K.; Sandler, R.S. Insurance, employment, and psychosocial consequences of a diagnosis of hereditary hemochromatosis in subjects without end organ damage. Am. J. Gastroenterol. 2003, 98, 1175–1180. [Google Scholar] [CrossRef]
- Meiser, B.; Dunn, S.; Dixon, J.; Powell, L.W. Psychological Adjustment and Knowledge about Hereditary Hemochromatosis in a Clinic-Based Sample: A Prospective Study. J. Genet. Couns. 2005, 14, 453–463. [Google Scholar] [CrossRef]
- Rombout-Sestrienkova, E.; Winkens, B.; Essers, B.A.; Nieman, F.H.; Noord, P.A.; Janssen, M.C.; van Deursen, C.T.; Boonen, A.; Reuser-Kaasenbrood, E.P.; Heeremans, J.; et al. Erythrocytapheresis versus phlebotomy in the maintenance treatment of HFE hemochromatosis patients: Results from a randomized crossover trial. Transfusion 2016, 56, 261–270. [Google Scholar] [CrossRef]
- Ong, S.Y.; Gurrin, L.C.; Dolling, L.; Dixon, J.; Nicoll, A.J.; Wolthuizen, M.; Wood, E.M.; Anderson, G.J.; Ramm, G.A.; Allen, K.J.; et al. Reduction of body iron in HFE-related haemochromatosis and moderate iron overload (Mi-Iron): A multicentre, participant-blinded, randomised controlled trial. Lancet Haematol. 2017, 4, e607–e614. [Google Scholar] [CrossRef]
- Milet, J.; Déhais, V.; Bourgain, C.; Jouanolle, A.M.; Mosser, A.; Perrin, M.; Morcet, J.; Brissot, P.; David, V.; Deugnier, Y.; et al. Common variants in the BMP2, BMP4, and HJV genes of the hepcidin regulation pathway modulate HFE hemochromatosis penetrance. Am. J. Hum. Genet. 2007, 81, 799–807. [Google Scholar] [CrossRef]
- Rombout-Sestrienkova, E.; Koek, G.H.; Neslo, R.; van Kraaij, M.; Menheere, P.P.; Masclee, A.; Swinkels, D.W. Course of iron parameters in HFE-hemochromatosis patients during initial treatment with erythrocytapheresis compared to phlebotomy. J. Clin. Apher. 2016, 31, 564–570. [Google Scholar] [CrossRef]
- Brissot, P.; Ball, S.; Rofail, D.; Cannon, H.; Jin, V.W. Hereditary hemochromatosis: Patient experiences of the disease and phlebotomy treatment. Transfusion 2011, 51, 1331–1338. [Google Scholar] [CrossRef]
- Bacon, B.R.; Adams, P.C.; Kowdley, K.V.; Powell, L.W.; Tavill, A.S. Diagnosis and management of hemochromatosis: 2011 Practice Guideline by the American Association for the Study of Liver Diseases. Hepatology 2011, 54, 328–343. [Google Scholar] [CrossRef]
- Kowdley, K.V.; Brown, K.E.; Ahn, J.; Sundaram, V. ACG Clinical Guideline. Am. J. Gastroenterol. 2019, 114, 1202–1218. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL clinical practice guidelines for HFE hemochromatosis. J. Hepatol. 2010, 53, 3–22. [Google Scholar] [CrossRef]
- Porto, G.; Brissot, P.; Swinkels, D.W.; Zoller, H.; Kamarainen, O.; Patton, S.; Alonso, I.; Morris, M.; Keeney, S. EMQN best practice guidelines for the molecular genetic diagnosis of hereditary hemochromatosis (HH). Eur. J. Hum. Genet. 2016, 24, 479–495. [Google Scholar] [CrossRef]
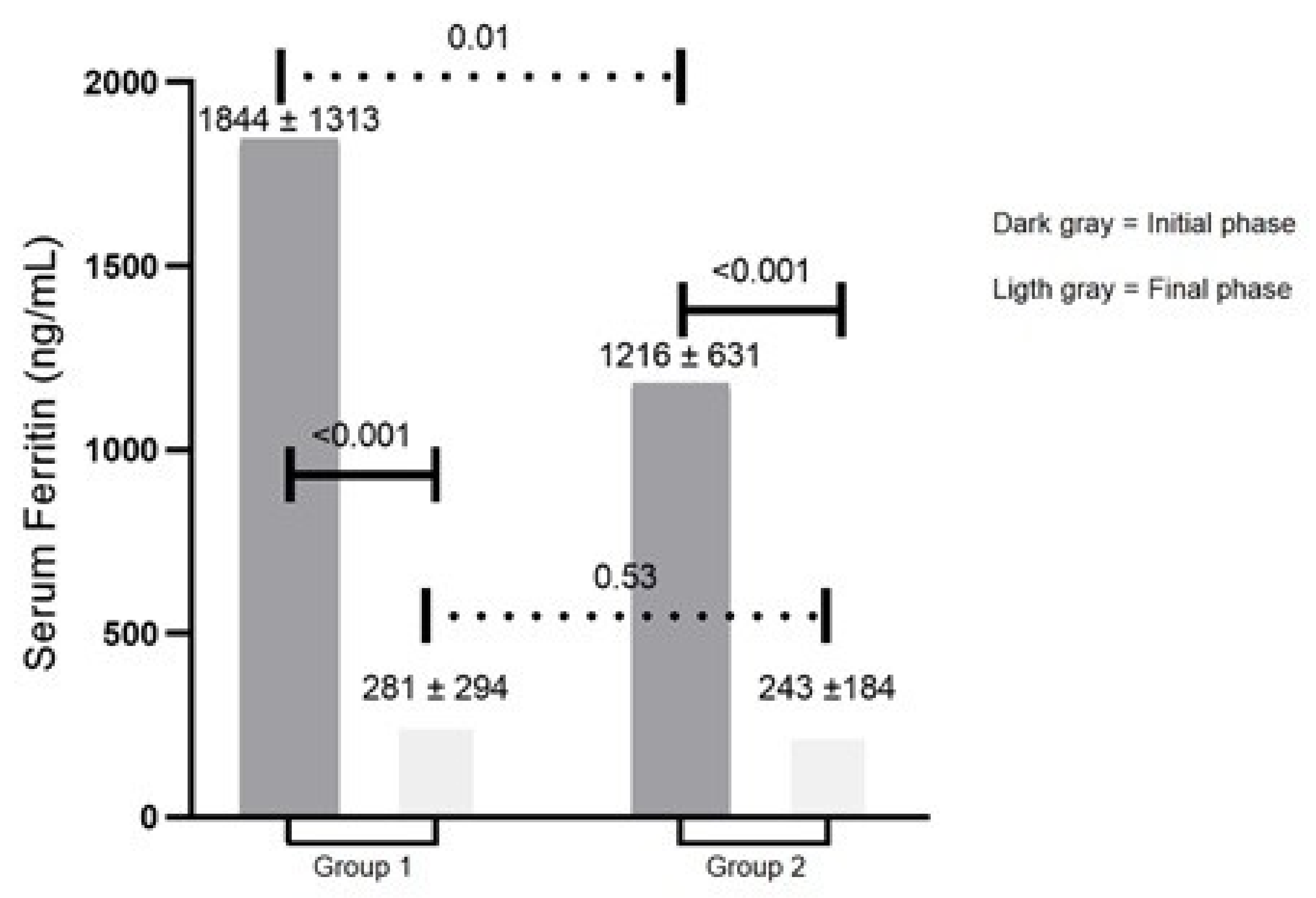
| Group 1 a n = 23 | Group 2 b n = 42 | p-Value | |
|---|---|---|---|
| Gender (male), % | 34.8 | 85.7 | 0.001 |
| Age (years), mean ± SD | 50 ± 13 | 54 ± 12 | 0.21 |
| Serum ferritin (ng/mL), mean ± SD | 281 ± 294 | 236 ± 174 | 0.53 |
| Number of phlebotomies | 8.8 ± 6.3 | 5.3 ± 5.8 | 0.72 |
| Self-declared race/color, % | |||
| White | 78.3 | 92.9 | 0.15 |
| Intermediate | 17.4 | 4.8 | |
| Asian and Amerindian | 4.3 | 2.3 | |
| Level of education, % | |||
| University | 65.2 | 73.8 | 0.89 |
| Others | 34.8 | 26.2 | |
| Consumption of alcoholic beverages, % | |||
| Never | 52.2 | 31.0 | 0.20 |
| Occasionally | 43.5 | 57.1 | |
| Frequently | 4.3 | 11.9 |
| SF-36 Domains Group 1a | Group 1 a n = 23 | Group 2 b n = 42 | p-Value |
|---|---|---|---|
| Physical functions | 84 ± 24 | 82 ± 22 | 0.34 |
| Role physical | 74 ± 43 | 73 ± 36 | 0.13 |
| Bodily pain | 64 ± 30 | 74 ± 24 | 0.03 |
| General health perception | 58 ± 21 | 69 ± 21 | 0.03 |
| Vitality | 56 ± 24 | 67 ± 21 | 0.01 |
| Social functioning | 68 ± 31 | 87 ± 22 | 0.01 |
| Role emotional | 57 ± 45 | 83 ± 30 | 0.01 |
| Mental health | 69 ± 22 | 77 ± 20 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acevedo, L.A.U.; Alvarenga, A.M.; Fonseca, P.F.S.; da Silva, N.K.; Cançado, R.D.; Naoum, F.A.; Dinardo, C.L.; Pereira, A.C.; Brissot, P.; Santos, P.C.J.L. Quality of Life Scores Remained Different among the Genotypic Groups of Patients with Suspected Hemochromatosis, Even after Treatment Period. Genes 2022, 13, 118. https://doi.org/10.3390/genes13010118
Acevedo LAU, Alvarenga AM, Fonseca PFS, da Silva NK, Cançado RD, Naoum FA, Dinardo CL, Pereira AC, Brissot P, Santos PCJL. Quality of Life Scores Remained Different among the Genotypic Groups of Patients with Suspected Hemochromatosis, Even after Treatment Period. Genes. 2022; 13(1):118. https://doi.org/10.3390/genes13010118
Chicago/Turabian StyleAcevedo, Luis Alfredo Utria, Aline Morgan Alvarenga, Paula Fernanda Silva Fonseca, Nathália Kozikas da Silva, Rodolfo Delfini Cançado, Flavio Augusto Naoum, Carla Luana Dinardo, Alexandre Costa Pereira, Pierre Brissot, and Paulo Caleb Junior Lima Santos. 2022. "Quality of Life Scores Remained Different among the Genotypic Groups of Patients with Suspected Hemochromatosis, Even after Treatment Period" Genes 13, no. 1: 118. https://doi.org/10.3390/genes13010118
APA StyleAcevedo, L. A. U., Alvarenga, A. M., Fonseca, P. F. S., da Silva, N. K., Cançado, R. D., Naoum, F. A., Dinardo, C. L., Pereira, A. C., Brissot, P., & Santos, P. C. J. L. (2022). Quality of Life Scores Remained Different among the Genotypic Groups of Patients with Suspected Hemochromatosis, Even after Treatment Period. Genes, 13(1), 118. https://doi.org/10.3390/genes13010118







