SARS-CoV-2 Infection and Emery-Dreifuss Syndrome in a Young Patient with a Family History of Dilated Cardiomyopathy
Abstract
:1. Introduction
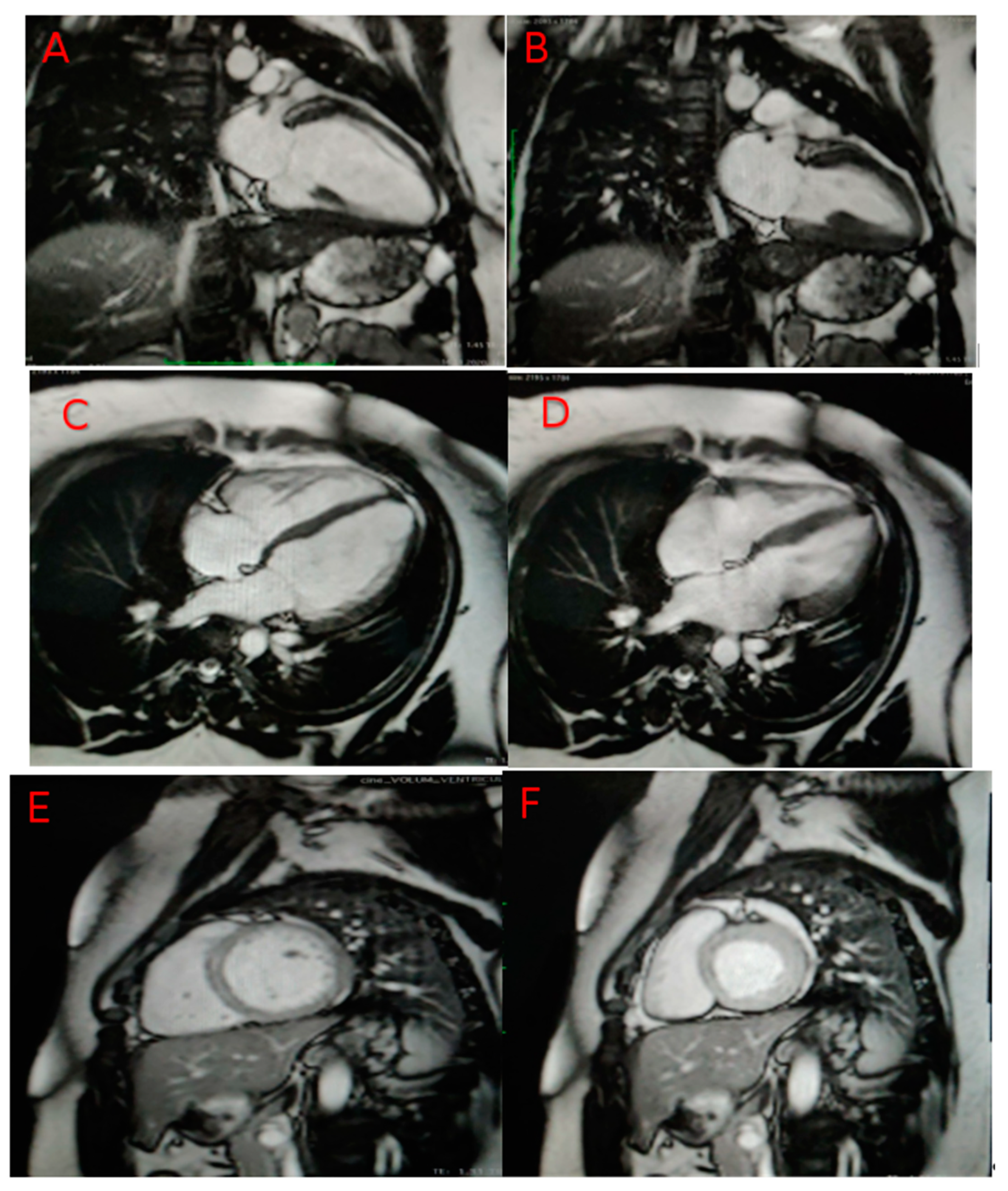
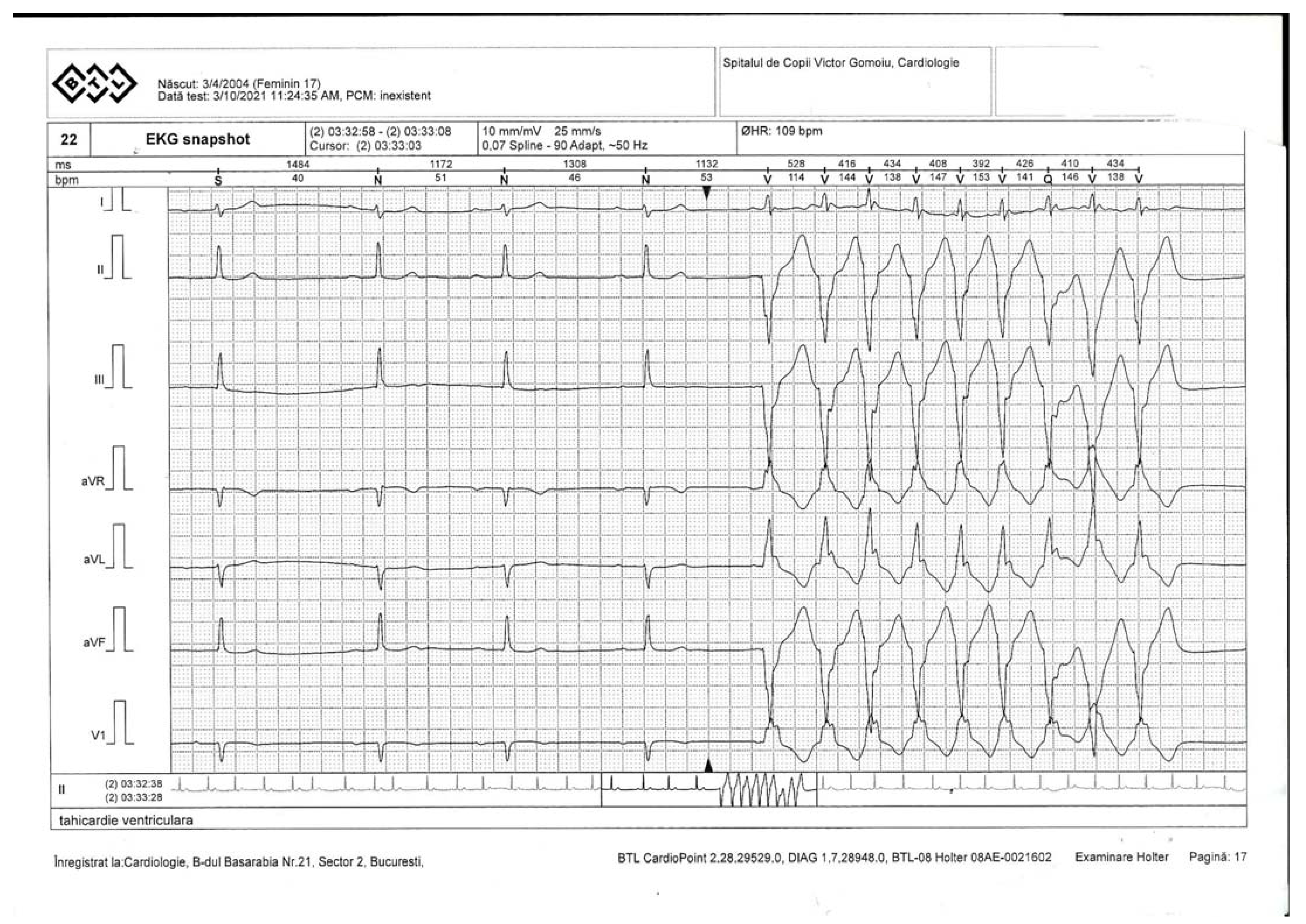
2. Case Presentation
- -
- Elevated values: high-sensitive cardiac troponin I (hs-cTnI 40.8 ng/L, normal < 6 ng/L); creatine kinase (CK 590 U/L, normal values < 192 U/L); N-terminal probrain natriuretic peptide (NT-proBNP 154 pg/mL, normal values < 125 pg/mL); D-dimers (580 ng/mL, normal values < 500 ng/mL); C-reactive protein (PCR 2 mg/dL, normal values 0.5 mg/dL); aspartate aminotransferase (AST 35 U/L, normal values < 25 U/L); alanine transaminase (ALT 50 U/L, normal values < 25 U/L), lactate dehydrogenase (LDH 248 U/L, normal values < 220 U/L);
- -
- Normal values: leukocytes (6.37 × 109 cells/L), lymphocytes (2.37 × 109 cells/L), neutrophils 6.2 × 109 cells/L, platelets 360 × 109 cells/L, creatinine 0.56 mg/dL, sodium 135 mmol/L, potassium 4.2 mmol/L.
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dai, X.; Luo, R.; Chen, Y.; Zheng, C.; Tang, Y.; Zhang, H.; Su, Y.; He, T.; Li, X. A Novel EMD Mutation Identified by Whole-Exome Sequencing in Twins with Emery–Dreifuss Muscular Dystrophy. Case Rep. Genet. 2020, 2020, 2071738. [Google Scholar] [CrossRef] [PubMed]
- Heller, S.A.; Shih, R.; Kalra, R.; Kang, P.B. Emery-Dreifuss muscular dystrophy. Muscle Nerve 2020, 61, 436–448. [Google Scholar] [CrossRef] [PubMed]
- Gueneau, L.; Bertrand, A.; Jais, J.-P.; Salih, M.; Stojkovic, T.; Wehnert, M.; Hoeltzenbein, M.; Spuler, S.; Saitoh, S.; Verschueren, A.; et al. Mutations of the FHL1 gene cause Emery-Dreifuss muscular dystrophy. Am. J. Hum. Genet. 2009, 85, 338–353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madej-Pilarczyk, A. Clinical aspects of Emery-Dreifuss muscular dystrophy. Nucleus 2018, 9, 314–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Available online: https://www.genecards.org/cgi-bin/carddisp.pl?gene=LMNA (accessed on 10 June 2021).
- Cenni, V.; Sabatelli, P.; Mattioli, E.; Marmiroli, S.; Capanni, C.; Ognibene, A.; Squarzoni, S.; Maraldi, N.M.; Bonne, G.; Columbaro, M.; et al. Lamin A N-terminal phosphorylation is associated with myoblast activation: Impairment in Emery—Dreifuss muscular dystrophy. J. Med. Genet. 2005, 42, 214–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barriales-Villa, R.; Ochoa, J.P.; Larrañaga-Moreira, J.M.; Salazar-Mendiguchía, J.; Díez-López, C.; Restrepo-Córdoba, M.A.; Álvarez-Rubio, J.; Robles-Mezcua, A.; Olmo-Conesa, M.C.; Nicolás-Rocamora, E.; et al. Risk predictors in a Spanish cohort with cardiac laminopathies. The REDLAMINA registry. Rev. Esp. Cardiol. (Engl. Ed.) 2021, 74, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Pinto, Y.M.; Reckman, Y.J. Formins Emerge as a Cause of Hypertrophic Cardiomyopathy: New Genes for Thick Hearts. J. Am. Coll. Cardiol. 2018, 72, 2468–2470. [Google Scholar] [CrossRef] [PubMed]
- Hershberger, R.E.; Morales, A. LMNA-Related Dilated Cardiomyopathy. In GeneReviews® [Internet]; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Mirzaa, G., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2008. [Google Scholar] [PubMed]
- Bonne, G.; Leturcq, F.; Yaou, R.B. Emery-Dreifuss Muscular Dystrophy. In GeneReviews® [Internet]; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Mirzaa, G., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2004. [Google Scholar] [PubMed]
- Available online: https://musculardystrophynews.com/information-about-covid-19-for-muscular-dystrophy-patients (accessed on 15 June 2021).
- Gujar, H.; Weisenberger, D.J.; Liang, G. The Roles of Human DNA Methyltransferases and Their Isoforms in Shaping the Epigenome. Genes 2019, 10, 172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Motorin, Y.; Helm, M. Methods for RNA Modification Mapping Using Deep Sequencing: Established and New Emerging Technologies. Genes 2019, 10, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dumitru, I.M.; Vlad, N.D.; Rugina, S.; Onofrei, N.; Gherca, S.; Raduna, M.; Trana, A.; Dumitrascu, M.; Popovici, E.; Bajdechi, M.; et al. SARS-CoV-2 Infection and Emery-Dreifuss Syndrome in a Young Patient with a Family History of Dilated Cardiomyopathy. Genes 2021, 12, 1070. https://doi.org/10.3390/genes12071070
Dumitru IM, Vlad ND, Rugina S, Onofrei N, Gherca S, Raduna M, Trana A, Dumitrascu M, Popovici E, Bajdechi M, et al. SARS-CoV-2 Infection and Emery-Dreifuss Syndrome in a Young Patient with a Family History of Dilated Cardiomyopathy. Genes. 2021; 12(7):1070. https://doi.org/10.3390/genes12071070
Chicago/Turabian StyleDumitru, Irina Magdalena, Nicoleta Dorina Vlad, Sorin Rugina, Nicoleta Onofrei, Sabina Gherca, Marian Raduna, Aurel Trana, Mirela Dumitrascu, Elena Popovici, Mircea Bajdechi, and et al. 2021. "SARS-CoV-2 Infection and Emery-Dreifuss Syndrome in a Young Patient with a Family History of Dilated Cardiomyopathy" Genes 12, no. 7: 1070. https://doi.org/10.3390/genes12071070
APA StyleDumitru, I. M., Vlad, N. D., Rugina, S., Onofrei, N., Gherca, S., Raduna, M., Trana, A., Dumitrascu, M., Popovici, E., Bajdechi, M., Zekra, L., & Cernat, R. C. (2021). SARS-CoV-2 Infection and Emery-Dreifuss Syndrome in a Young Patient with a Family History of Dilated Cardiomyopathy. Genes, 12(7), 1070. https://doi.org/10.3390/genes12071070






