Making Sense of a Health Threat: Illness Representations, Coping, and Psychological Distress among BRCA1/2 Mutation Carriers
Abstract
1. Introduction
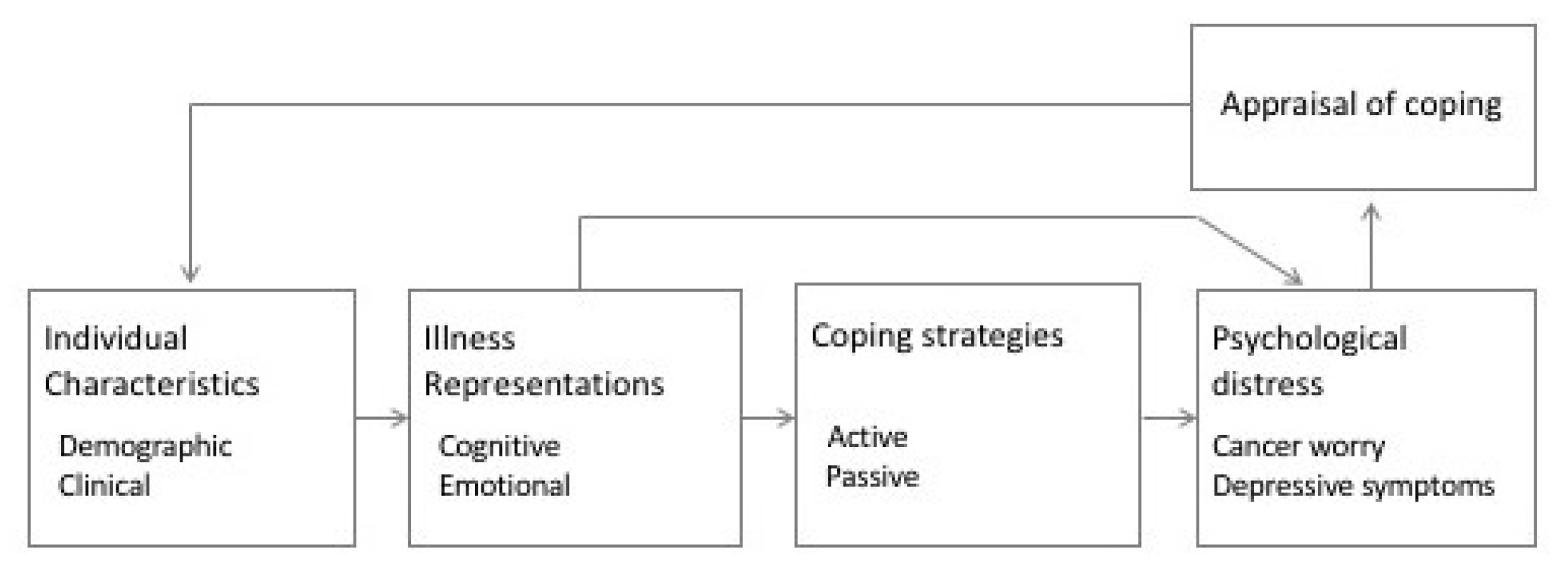
Common Sense Model of Self-Regulation of Health and Illness
2. Materials and Methods
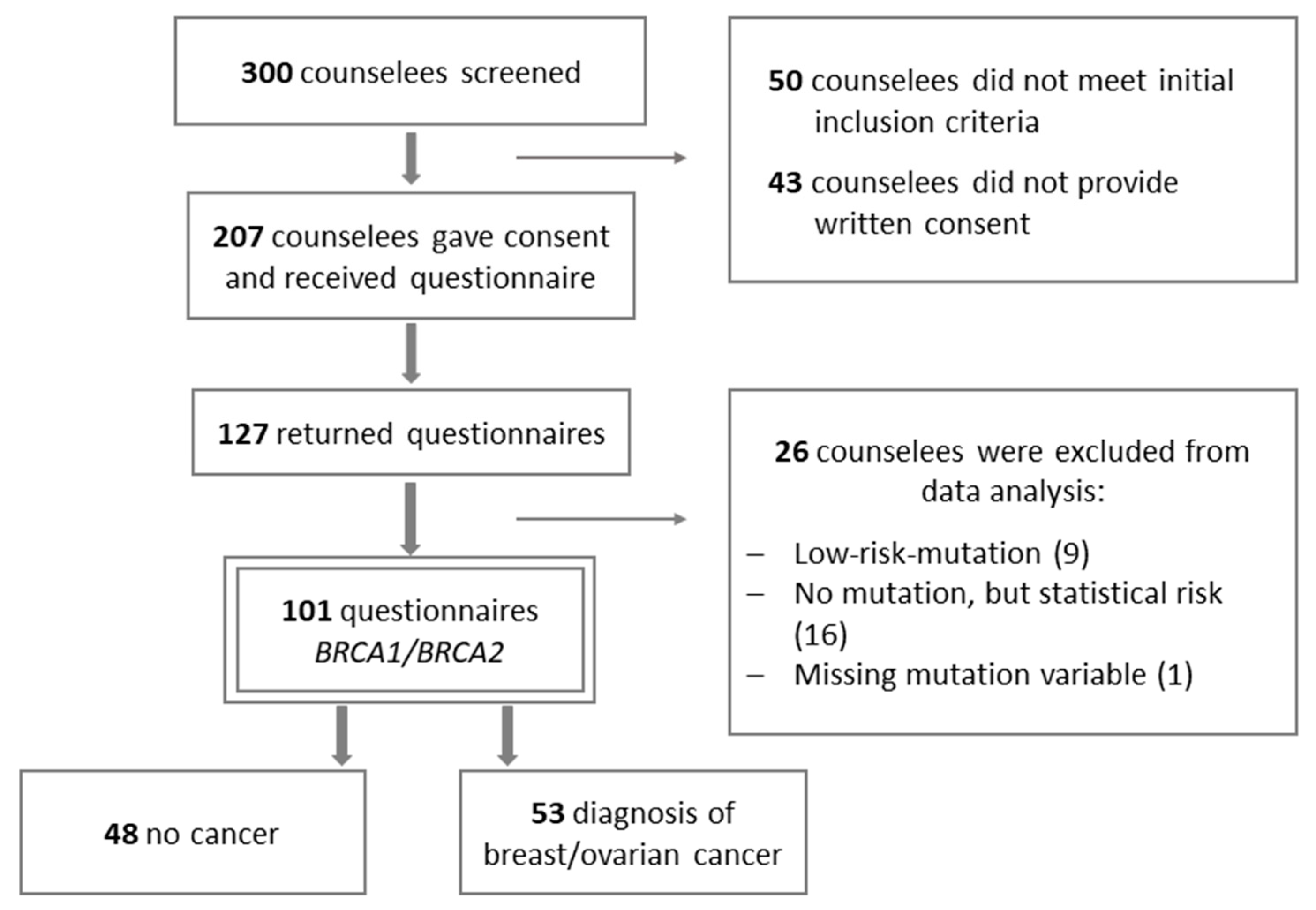
2.1. Procedures and Participants
2.2. Instrumentation
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Illness Perceptions, Coping Strategies, and Psychological Distress
3.3. Hierarchical Regression Analyses
3.3.1. Cancer Worry
3.3.2. Depressive Symptoms
4. Discussion
4.1. Study Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kuchenbaecker, K.B.; Hopper, J.L.; Barnes, D.R.; Phillips, K.A.; Mooij, T.M.; Roos-Blom, M.J.; Jervis, S.; Van Leeuwen, F.E.; Milne, R.L.; Andrieu, N.; et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. J. Am. Med. Assoc. 2017, 317, 2402–2416. [Google Scholar] [CrossRef]
- Bick, U.; Engel, C.; Krug, B.; Heindel, W.; Fallenberg, E.M.; Rhiem, K.; Maintz, D.; Golatta, M.; Speiser, D.; Rjosk-Dendorfer, D.; et al. High-risk breast cancer surveillance with MRI: 10-year experience from the German consortium for hereditary breast and ovarian cancer. Breast Cancer Res. Treat. 2019, 175, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Sigal, B.M.; Munoz, D.F.; Kurian, A.W.; Plevritis, S.K. A simulation model to predict the impact of prophylactic surgery and screening on the life expectancy of BRCA1 and BRCA2 mutation carriers. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1066–1077. [Google Scholar] [CrossRef] [PubMed]
- Butow, P.N.; Lobb, E.A.; Meiser, B.; Barratt, A.; Tucker, K.M. Psychological outcomes and risk perception after genetic testing and counselling in breast cancer: A systematic review. Med. J. Aust. 2003, 178, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, J.G.; Lobel, M.; Moyer, A. Emotional Distress Following Genetic Testing for Hereditary Breast and Ovarian Cancer: A Meta-Analytic Review. Health Psychol. 2010, 28, 510–518. [Google Scholar] [CrossRef]
- Harmsen, M.G.; Hermens, R.P.M.G.; Prins, J.B.; Hoogerbrugge, N.; de Hullu, J.A. How medical choices influence quality of life of women carrying a BRCA mutation. Crit. Rev. Oncol. Hematol. 2015, 96, 555–568. [Google Scholar] [CrossRef] [PubMed]
- Werner-Lin, A. Building the Cancer Family: Family Planning in the Context of Inherited Breast and Ovarian Cancer Risk. J. Soc. Soc. Work Res. 2010, 1, 14–27. [Google Scholar] [CrossRef]
- Ringwald, J.; Wochnowski, C.; Bosse, K.; Giel, K.E.; Schäffeler, N.; Zipfel, S.; Teufel, M. Psychological Distress, Anxiety, and Depression of Cancer-Affected BRCA1/2 Mutation Carriers: A Systematic Review. J. Genet. Couns. 2016, 25, 880–891. [Google Scholar] [CrossRef] [PubMed]
- Nelson, H.D.; Pappas, M.; Cantor, A.; Haney, E.; Holmes, R. Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA- Related Cancer in Women: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. J. Am. Med. Assoc. 2019, 322, 666–685. [Google Scholar] [CrossRef]
- Lombardi, L.; Bramanti, S.M.; Babore, A.; Stuppia, L.; Trumello, C.; Antonucci, I.; Cavallo, A. Psychological aspects, risk and protective factors related to BRCA genetic testing: A review of the literature. Support. Care Cancer 2019, 27, 3647–3656. [Google Scholar] [CrossRef] [PubMed]
- Graves, K.D.; Vegella, P.; Poggi, E.A.; Peshkin, B.N.; Tong, A.; Isaacs, C.; Finch, C.; Kelly, S.; Taylor, K.L.; Luta, G.; et al. Long-term psychosocial outcomes of BRCA1/BRCA2 testing: Differences across affected status and risk-reducing surgery choice. Cancer Epidemiol. Biomark. Prev. 2012, 21, 445–455. [Google Scholar] [CrossRef]
- Pasacreta, J.V. Psychosocial issues associated with genetic testing for breast and ovarian cancer risk: An integrative review. Cancer Investig. 2003, 21, 588–623. [Google Scholar] [CrossRef]
- Leventhal, H.; Leventhal, E.; Contrada, R. Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychol. Health 1998, 13, 717–733. [Google Scholar] [CrossRef]
- Leventhal, H.; Benyamini, Y.; Brownlee, S.; Diefenbach, M.; Leventhal, E.A.; Patrick-Miller, L.; Robitaille, C. Illness Representations: Theoretical Foundations. In Perception of Health and Illness; Petrie, K., Weinman, J.A., Eds.; Harewood Academic Publishers: Amsterdam, The Netherland, 1997; pp. 19–45. [Google Scholar]
- Decruyenaere, M.; Evers-Kiebooms, G.; Welkenhuysen, M.; Denayer, L.; Claes, E. Cognitive representations of breast cancer, emotional distress and preventive health behaviour: A theoretical perspective. Psychooncology 2000, 9, 528–536. [Google Scholar] [CrossRef]
- Moss-Morris, R.; Weinman, J.; Petrie, K.; Horne, R.; Cameron, L.; Buick, D. The Revised Illness Perception Questionnaire (IPQ-R). Psychol. Health 2002, 17, 1–16. [Google Scholar] [CrossRef]
- Richardson, E.M.; Schüz, N.; Sanderson, K.; Scott, J.L.; Schüz, B. Illness representations, coping, and illness outcomes in people with cancer: A systematic review and meta-analysis. Psychooncology 2017, 26, 724–737. [Google Scholar] [CrossRef] [PubMed]
- van Oostrom, I.; Meijers-Heijboer, H.; Duivenvoorden, H.J.; Bröcker-Vriends, A.H.J.T.; van Asperen, C.J.; Sijmons, R.H.; Seynaeve, C.; Van Gool, A.R.; Klijn, J.G.M.; Tibben, A. The common sense model of self-regulation and psychological adjustment to predictive genetic testing: A prospective study. Psychooncology 2007, 16, 1121–1129. [Google Scholar] [CrossRef]
- Rees, G.; Fry, A.; Cull, A.; Sutton, S. Illness perceptions and distress in women at increased risk of breast cancer. Psychol. Health 2004, 19, 749–765. [Google Scholar] [CrossRef]
- Claes, E.; Evers-Kiebooms, G.; Denayer, L.; Decruyenaere, M.; Boogaerts, A.; Philippe, K.; Legius, E. Predictive genetic testing for hereditary breast and ovarian cancer: Psychological distress and illness representations 1 year following disclosure. J. Genet. Couns. 2005, 14, 349–363. [Google Scholar] [CrossRef] [PubMed]
- Freeman-Gibb, L.A.; Janz, N.K.; Katapodi, M.C.; Zikmund-Fisher, B.J.; Northouse, L. The relationship between illness representations, risk perception and fear of cancer recurrence in breast cancer survivors. Psychooncology 2017, 26, 1270–1277. [Google Scholar] [CrossRef]
- Hagger, M.S.; Orbell, S. A Meta-Analytic Review of the Common-Sense Model of Illness Representations. Psychol. Health 2003, 18, 141–184. [Google Scholar] [CrossRef]
- Speiser, D.; Rebitschek, F.G.; Feufel, M.A.; Brand, H.; Besch, L.; Kendel, F. Accuracy in risk understanding among BRCA1/2-mutation carriers. Patient Educ. Couns. 2019, 102, 1925–1931. [Google Scholar] [CrossRef]
- Glattacker, M.; Bengel, J.; Jäckel, W.H. Die deutschsprachige Version des Illness Perception Questionnaire-Revised. Z. Gesundh. 2009, 17, 158–169. [Google Scholar] [CrossRef]
- Knoll, N.; Rieckmann, N.; Schwarzer, R. Coping as a mediator between personality and stress outcomes: A longitudinal study with cataract surgery patients. Eur. J. Pers. 2005, 19, 229–247. [Google Scholar] [CrossRef]
- Lerman, C.; Trock, B.; Rimer, B.K.; Jepson, C.; Brody, D.; Boyce, A. Psychological side effects of breast cancer screening. Health Psychol. 1991, 10, 259–267. [Google Scholar] [CrossRef]
- Vodermaier, A. Prophylaktische Chirurgie bei Brust- und Eierstockkrebsrisiko aus psychologischer Perspektive; Ludwig-Maximilians-Universität München: Munich, Germany, 2005. [Google Scholar]
- Löwe, B.; Spitzer, R.L.; Zipfel, S.; Herzog, W. Patient Health Questionnaire (PHQ), German Version, Manual and Materials, 2nd ed.; Pfizer: Karlsruhe, Germany, 2002. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics New International Edition; Pearson Education: Harlow, UK, 2014. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage Publications: London, UK, 2013. [Google Scholar]
- Krohne, H.W. Vigilance and cognitive avoidance as concepts in coping research. In Attention and Avoidance: Strategies in Coping with Aversiveness; Hogrefe & Huber: Toronto, ON, Canada, 1993; ISBN 3-8017-0664-8. [Google Scholar]
- Pilevarzadeh, M.; Amirshahi, M.; Afsargharehbagh, R.; Rafiemanesh, H.; Hashemi, S.-M.; Balouchi, A. Global prevalence of depression among breast cancer patients: A systematic review and meta-analysis. Breast Cancer Res. Treat. 2019, 176, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Watts, S.; Prescott, P.; Mason, J.; McLeod, N.; Lewith, G. Depression and anxiety in ovarian cancer: A systematic review and meta-analysis of prevalence rates. BMJ Open 2015, 5, e007618. [Google Scholar] [CrossRef]
- Evans, D.G.R.; Barwell, J.; Eccles, D.M.; Collins, A.; Izatt, L.; Jacobs, C.; Donaldson, A.; Brady, A.F.; Cuthbert, A.; Harrison, R.; et al. The Angelina Jolie effect: How high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res. 2014, 16, 1–6. [Google Scholar] [CrossRef]
- Kessler, S. Invited essay on the psychological aspects of genetic counseling. V. Preselection: A family coping strategy in Huntington disease. Am. J. Med. Genet. 1988, 31, 617–621. [Google Scholar] [CrossRef] [PubMed]
- Gooding, H.C.; Organista, K.; Burack, J.; Biesecker, B.B. Genetic susceptibility testing from a stress and coping perspective. Soc. Sci. Med. 2006, 62, 1880–1890. [Google Scholar] [CrossRef]
- Siemonsma, P.C.; Stuive, I.; Roorda, L.D.; Vollebregt, J.A.; Walker, M.F.; Lankhorst, G.J.; Lettinga, A.T. Cognitive Treatment of Illness Perceptions in Patients With Chronic Low Back Pain: A Randomized Controlled Trial. Phys. Ther. 2013, 93, 435–448. [Google Scholar] [CrossRef]
- Vos, J.; Gómez-García, E.; Oosterwijk, J.C.; Menko, F.H.; Stoel, R.D.; Van Asperen, C.J.; Jansen, A.M.; Stiggelbout, A.M.; Tibben, A. Opening the psychological black box in genetic counseling. The psychological impact of DNA testing is predicted by the counselees’ perception, the medical impact by the pathogenic or uninformative BRCA1/2-result. Psychooncology 2012, 21, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Schmutzler, R.; Rhiem, K. Beratung junger Frauen mit hereditärer Belastung für Brust- und EierstockkrebsCounselling of young women with hereditary risks for breast and ovarian cancer. Forum Fam. Plan. West. Hemisph. 2017, 32, 37–41. [Google Scholar] [CrossRef]
- Esplen, M.J.; Hunter, J.; Leszcz, M.; Warner, E.; Narod, S.; Metcalfe, K.; Glendon, G.; Butler, K.; Liede, A.; Young, M.A.; et al. A multicenter study of supportive-expressive group therapy for women with BRCA1/BRCA2 mutations. Cancer 2004, 101, 2327–2340. [Google Scholar] [CrossRef] [PubMed]
- Hirschberg, A.M.; Chan-Smutko, G.; Pirl, W.F. Psychiatric implications of cancer genetic testing. Cancer 2014, 121, 341–360. [Google Scholar] [CrossRef] [PubMed]
| Entire Sample (N = 101) | Diagnosis of Breast/Ovarian Cancer (n = 53) | No Breast/Ovarian Cancer (n = 48) | |
|---|---|---|---|
| Demographic characteristics | |||
| Age (years), M (SD) | 43.4 (10.9) | 46.7 (9.6) | 40.0 (11.2) |
| Partnership, n (%) | |||
| Living with a partner | 80 (79.2%) | 40 (75.5%) | 40 (83.3%) |
| Living without a partner | 21 (20.8%) | 13 (24.5%) | 8 (16.7%) |
| Presence of children, n (%) | 70 (69.3%) | 38 (71.7%) | 32 (66.7%) |
| Level of education, n (%) | |||
| High school degree | 61 (60.4%) | 28 (52.8%) | 33 (68.8%) |
| Secondary school | 40 (39.6%) | 25 (47.2%) | 15 (31.3%) |
| Occupation status, n (%) | |||
| Employed | 73 (72.3%) | 35 (66.0%) | 38 (80.9%) |
| Unemployed | 13 (12.9%) | 7 (13.2%) | 6 (12.5%) |
| Retired | 14 (13.9%) | 11 (20.8%) | 3 (6.3%) |
| Clinical Characteristics | |||
| Prophylactic surgery, n (%) | |||
| No prophylactic surgery | 46 (45.5%) | 17 (32.1%) | 29 (60.4%) |
| Prophylactic mastectomy | 13 (12.9%) | 9 (17%) | 4 (8.3%) |
| Prophylactic salpingo-oophorectomy | 27 (26.7%) | 13 (24.5%) | 14 (29.2%) |
| Mastectomy and salpingo- oophorectomy | 11 (10.9%) | 10 (18.9%) | 1 (2.1%) |
| History of cancer, n (%) | |||
| Breast cancer | - | 44 (83.3%) | - |
| Ovarian cancer | - | 5 (9.4%) | - |
| Months since diagnosis, M (SD) | - | 62.1 (62.5) | - |
| Pathogenic germline variant, n (%) | |||
| BRCA1 mutation | 62 (61.4%) | 35 (66%) | 27 (56.3%) |
| BRCA2 mutation | 39 (38.6%) | 18 (34.0%) | 21 (43.8%) |
| Months since mutation analysis, M (SD) | 14.2 (12.6) | 14.3 (11.7) | 14.1 (13.6) |
| Entire Sample (N = 101) | Diagnosis of Breast/Ovarian Cancer (n = 53) | No Breast/Ovarian Cancer (n = 48) | 95% CI | p | |
|---|---|---|---|---|---|
| Illness representations M (SD) | |||||
| Consequences | 4.8 (2.6) | 6.3 (2.5) | 5.5 (2.6) | −2.50 to −0.49 | 0.004 |
| Illness coherence | 7.3 (2.0) | 7.0 (2.4) | 7.2 (2.2) | −0.59 to 1.13 | 0.532 |
| Concern | 5.9 (2.6) | 6.5 (2.3) | 5.3 (2.9) | −2.21 to −0.16 | 0.023 |
| Emotional representations | 4.8 (2.9) | 6.3 (2.6) | 5.6 (2.9) | −2.68 to −0.50 | 0.005 |
| Personal control | 5.4 (2.4) | 5.8 (2.3) | 5.6 (2.4) | −1.29 to 0.58 | 0.453 |
| Treatment control | 6.8 (2.0) | 6.3 (2.1) | 6.5 (2.1) | −0.32 to 1.30 | 0.231 |
| Coping strategies M (SD) | |||||
| Active coping | 1.5 (1.1) | 1.9 (1.1) | 1.2 (1.0) | −1.06 to −0.23 | 0.003 |
| Social support seeking (instrumental) | 1.3 (0.9) | 1.3 (1.0) | 1.3 (0.9) | −0.45 to 0.28 | 0.645 |
| Denial | 0.4 (0.7) | 0.4 (0.7) | 0.4 (0.7) | −0.33 to 0.23 | 0.726 |
| Positive reframing | 1.5 (0.9) | 1.6 (0.9) | 1.3 (1.0) | −0.58 to 0.16 | 0.254 |
| Psychological distress M (SD) | |||||
| Cancer worry | 1.7 (0.8) | 1.9 (0.7) | 1.5 (0.9) | −0.78 to −0.15 | 0.005 |
| Depressive symptoms | 0.7 (0.5) | 0.8 (0.5) | 0.5 (0.4) | −0.45 to −0.08 | 0.006 |
| Active Coping | Social Support Seeking | Denial | Positive Reframing | |
|---|---|---|---|---|
| 1. Consequences | 0.37 * | 0.16 | 0.23 * | 0.06 |
| 2. Illness coherence | −0.09 | 0.13 | −0.06 | −0.09 |
| 3. Concern | 0.29 * | 0.07 | 0.26 * | −0.18 |
| 4. Emotional representations | 0.28 * | 0.17 | 0.30 * | −0.09 |
| 5. Personal control | 0.26 * | 0.15 | 0.15 | 0.21 * |
| 6. Treatment control | 0.23 * | 0.28 * | 0.06 | 0.27 * |
| Cancer Worry | Depressive Symptoms b | |
|---|---|---|
| Demographic Characteristics | ||
| Age | 0.05 | 0.16 |
| Marital status a | 0.06 | 0.15 |
| Presence of children a | 0.20 * | 0.08 |
| Level of education a | 0.17 | 0.19 |
| Occupation status a | 0.30 * | 0.19 |
| Clinical characteristics | ||
| Subgroups operations a | 0.21 | 0.29 * |
| History of cancer a | 0.28 | 0.29 ** |
| Months since cancer diagnosis | 0.09 | 0.33 * |
| Mutation diagnosis a | 0.14 | 0.11 |
| Months since mutation analysis | −0.16 | 0.08 |
| Illness representations | ||
| Consequences | 0.68 ** | 0.46 ** |
| Illness coherence | −0.23 * | −0.30 ** |
| Concern | 0.70 ** | 0.47 ** |
| Emotional representations | 0.64 ** | 0.67 ** |
| Personal control | 0.05 | 0.10 |
| Treatment control | −0.05 | −0.16 |
| Coping strategies | ||
| Active coping | 0.31 ** | 0.29 ** |
| Social support seeking | 0.08 | 0.14 |
| Denial | 0.14 | 0.24 * |
| Positive reframing | 0.08 | 0.05 |
| Cancer Worry | B | SE B | β |
|---|---|---|---|
| Step 1 | |||
| Presence of children | 0.27 | 0.12 | 0.15 |
| Occupation | 0.28 | 0.18 | 0.24 * |
| Step 2 | |||
| Presence of children | 0.11 | 0.13 | 0.06 |
| Occupation | 0.09 | 0.09 | 0.08 |
| Consequences | 0.09 | 0.03 | 0.30 * |
| Coherence | −0.05 | 0.03 | −0.12 |
| Concern | 0.12 | 0.03 | 0.37 ** |
| Emotional representation | 0.03 | 0.03 | 0.12 |
| Step 3 | |||
| Presence of children | 0.11 | 0.13 | 0.81 |
| Occupation | 0.09 | 0.09 | 1.03 |
| Consequences | 0.09 | 0.03 | 0.29 ** |
| Coherence | −0.05 | 0.03 | −0.12 |
| Concern | 0.12 | 0.03 | 0.37 ** |
| Emotional representation | 0.03 | 0.03 | 0.12 |
| Active coping | 0.04 | 0.05 | 0.05 |
| R2 = 0.10 for block 1; ΔR2 = 0.50 for block 2; ΔR2 = 0.00 for block 3. * p < 0.05; ** p < 0.01 | |||
| Depressive Symptoms | B | SE B | β |
| Step 1 | |||
| Prophylactic operations | 0.04 | 0.05 | 0.26 * |
| Step 2 | |||
| Prophylactic operations | 0.02 | 0.01 | 0.16 * |
| Consequences | −0.01 | 0.02 | −0.04 |
| Coherence | −0.03 | 0.01 | −0.18 * |
| Concern | 0.01 | 0.02 | 0.08 |
| Emotional representation | 0.07 | 0.01 | 0.59 ** |
| Step 3 | |||
| Prophylactic operations | 0.02 | 0.01 | 1.13 |
| Consequences | −0.01 | 0.02 | −0.06 |
| Coherence | −0.03 | 0.01 | −0.17 * |
| Concern | 0.01 | 0.02 | 0.08 |
| Emotional representation | 0.07 | 0.02 | 0.60 ** |
| Active coping | 0.02 | 0.03 | 0.07 |
| Denial coping | −0.01 | 0.04 | −0.01 |
| R2 = 0.07 for block 1; ΔR2 = 0.45 for block 2, ΔR2 = 0.00 for block 3. * p < 0.05; ** p < 0.01 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brand, H.; Speiser, D.; Besch, L.; Roseman, J.; Kendel, F. Making Sense of a Health Threat: Illness Representations, Coping, and Psychological Distress among BRCA1/2 Mutation Carriers. Genes 2021, 12, 741. https://doi.org/10.3390/genes12050741
Brand H, Speiser D, Besch L, Roseman J, Kendel F. Making Sense of a Health Threat: Illness Representations, Coping, and Psychological Distress among BRCA1/2 Mutation Carriers. Genes. 2021; 12(5):741. https://doi.org/10.3390/genes12050741
Chicago/Turabian StyleBrand, Hannah, Dorothee Speiser, Laura Besch, Julia Roseman, and Friederike Kendel. 2021. "Making Sense of a Health Threat: Illness Representations, Coping, and Psychological Distress among BRCA1/2 Mutation Carriers" Genes 12, no. 5: 741. https://doi.org/10.3390/genes12050741
APA StyleBrand, H., Speiser, D., Besch, L., Roseman, J., & Kendel, F. (2021). Making Sense of a Health Threat: Illness Representations, Coping, and Psychological Distress among BRCA1/2 Mutation Carriers. Genes, 12(5), 741. https://doi.org/10.3390/genes12050741





