Next-Generation Sequencing-Based Pre-Implantation Genetic Testing for Aneuploidy (PGT-A): First Report from Saudi Arabia
Abstract
1. Introduction
2. Material and Methods
Study Approval and Consent
3. Study Subjects
3.1. Genomic DNA Extraction from Blastomere Biopsy
3.2. Pre-Amplification of Genomic DNA
3.3. Amplification of DNA Libraries
3.4. Pool, Purify, and Quantification of the DNA Libraries
3.5. Loading of DNA Libraries Pool into Ion Chef™ Equipment
3.6. Initialization and Sequencing Run into Ion S5™
3.7. Bioinformatics Analysis and Interpretation of NGS Data
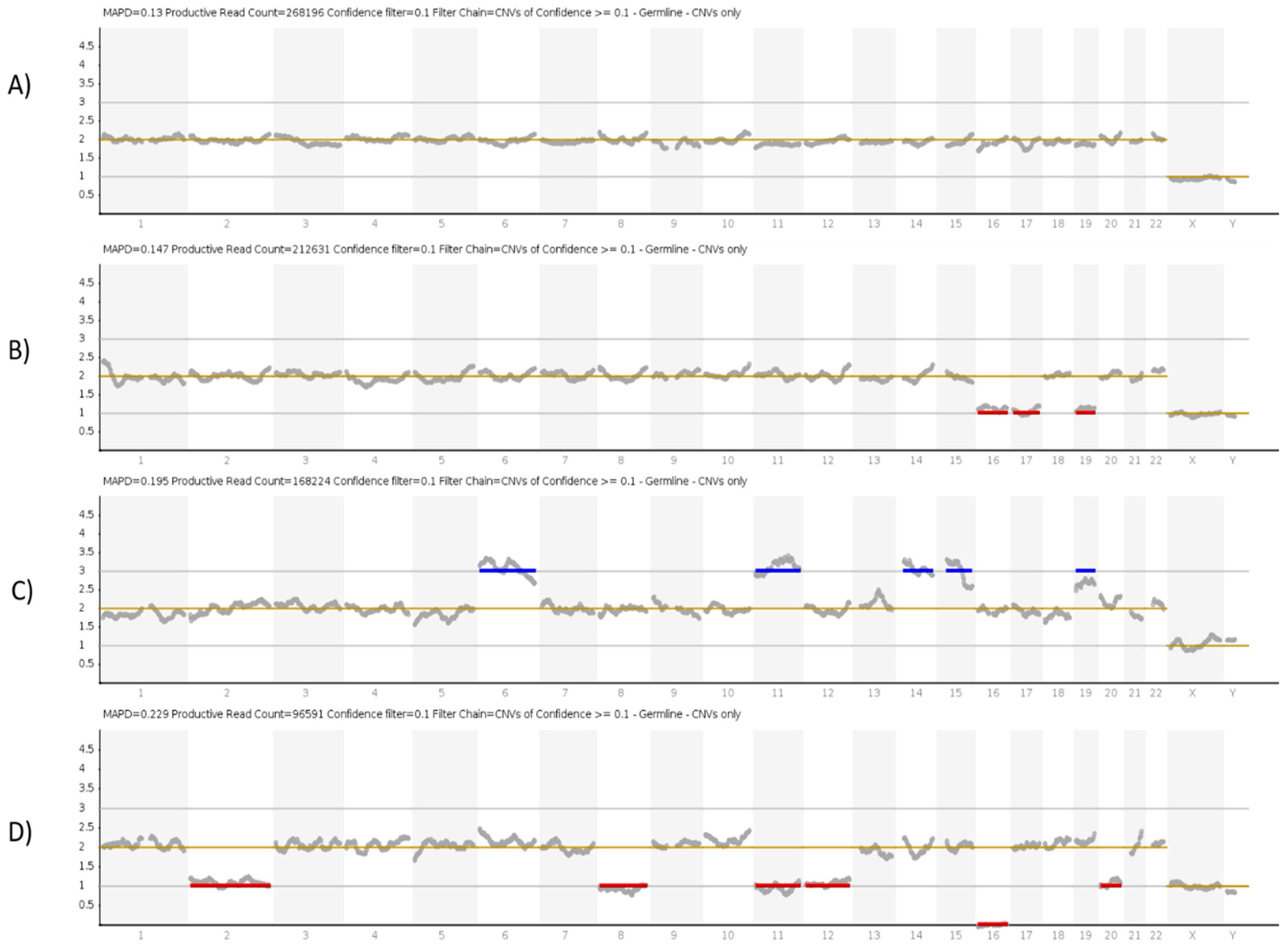
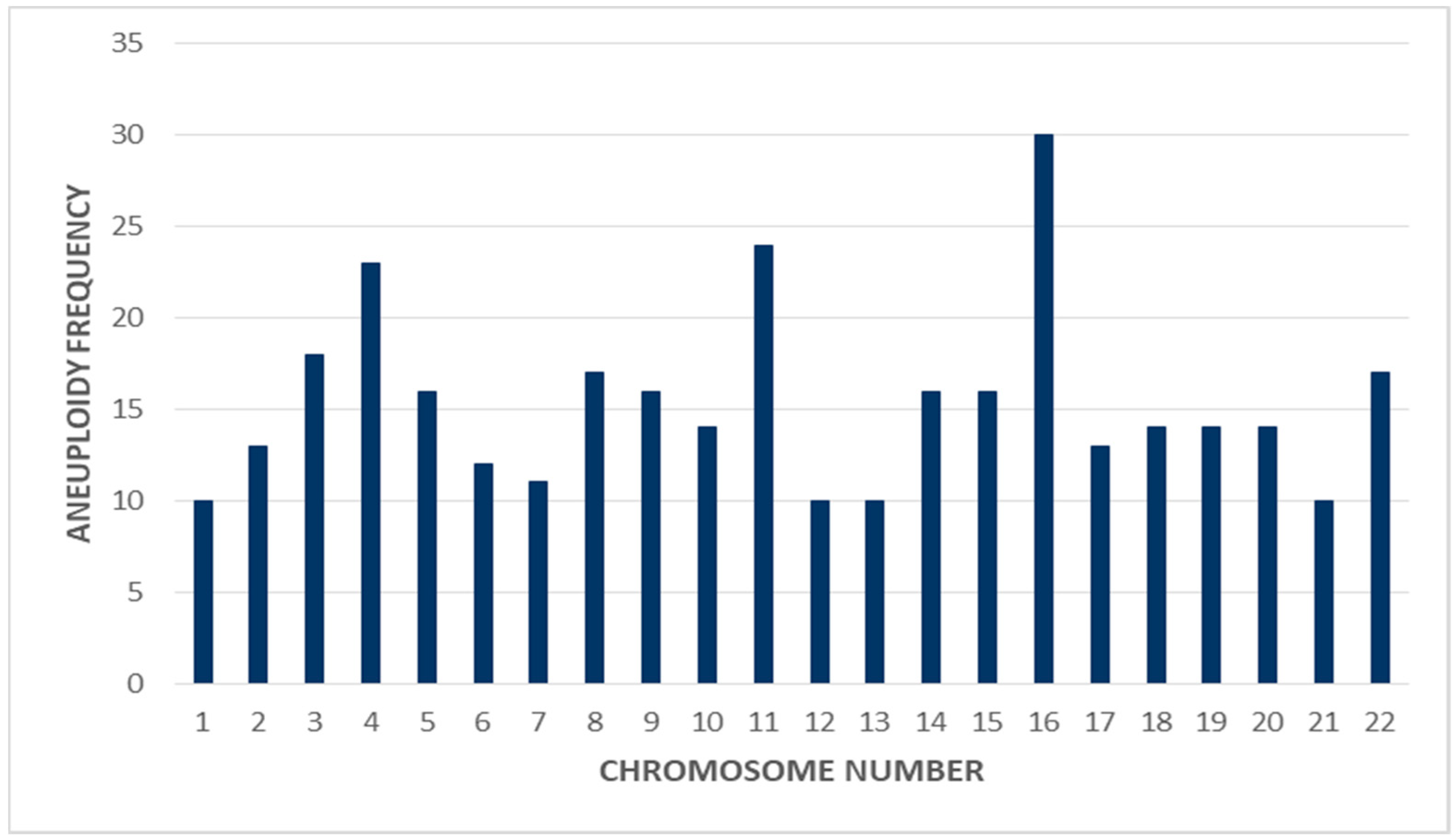
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethical Standards
Abbreviations
| PGT-A | Pre-Implantation Genetic Testing for Aneuploidy |
| PGS | Pre-Implantation Genetic Screening |
| PGD | Pre-Implantation Genetic Diagnosis |
| IVF | In vitro Fertilization |
| PCR | Polymerase Chain Reaction |
| NSG | Next-Generation sequencing |
| FISH | Fluorescence in situ hybridization |
| NFW | Nuclease Free Water |
| IRB | Institution Review Board |
| NGHA | National Guard Health Affairs |
| KAIMRC | King Abdullah International Medical Research Center |
References
- Alberti, A.; Salomon, L.J.; Le Lorc’h, M.; Couloux, A.; Bussières, L.; Goupil, S.; Malan, V.; Pelletier, E.; Hyon, C.; Vialard, F.; et al. Non-invasive prenatal testing for trisomy 21 based on analysis of cell-free fetal DNA circulating in the maternal plasma. Prenat Diagn. 2015, 35, 471–476. [Google Scholar] [CrossRef]
- Badeau, M.; Lindsay, C.; Blais, J.; Nshimyumukiza, L.; Takwoingi, Y.; Langlois, S.; Légaré, F.; Giguère, Y.; Turgeon, A.F.; Witteman, W.; et al. Genomics-based non-invasive prenatal testing for detection of fetal chromosomal aneuploidy in pregnant women. Cochrane Database Syst. Rev. 2017, 11, Cd011767. [Google Scholar] [CrossRef]
- Benachi, A.; Letourneau, A.; Kleinfinger, P.; Senat, M.V.; Gautier, E.; Favre, R.; Bidat, L.; Houfflin-Debarge, V.; Bouyer, J.; Costa, J.M. Cell-free DNA analysis in maternal plasma in cases of fetal abnormalities detected on ultrasound examination. Obstet. Gynecol. 2015, 125, 1330–1337. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhang, L.; Lv, H.; Li, Y.; Zhu, C.; Tian, W.; Zhao, L. Applying high-throughput sequencing to identify and evaluate foetal chromosomal deletion and duplication. J. Cell Mol. Med. 2020, 24, 9936–9944. [Google Scholar] [CrossRef] [PubMed]
- Cuckle, H.; Maymon, R. Development of prenatal screening--A historical overview. Semin. Perinatol. 2016, 40, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Pös, O.; Budiš, J.; Szemes, T. Recent trends in prenatal genetic screening and testing. F1000Research 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.; Wapner, R. Prenatal diagnosis by chromosomal microarray analysis. Fertil. Steril. 2018, 109, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Ambartsumyan, G.; Clark, A.T. Aneuploidy and early human embryo development. Hum. Mol. Genet. 2008, 17, R10–R15. [Google Scholar] [CrossRef]
- Rubio, C.; Mercader, A.; Mateu, E.; Buendía, P.; Pehlivan, T.; Viloria, T.; De los Santos, M.J.; Simón, C.; Remohí, J.; Pellicer, A.; et al. Impact of chromosomal abnormalities on preimplantation embryo development. Prenat. Diagn. 2007, 27, 748–756. [Google Scholar] [CrossRef]
- Handyside, A.H. 24-chromosome copy number analysis: A comparison of available technologies. Fertil. Steril. 2013, 100, 595–602. [Google Scholar] [CrossRef]
- Lukaszuk, K.; Jakiel, G.; Kuczynski, W.; Pukszta, S.; Liss, J.; Plociennik, L.; Lukaszuk, A.; Pastuszek, E. Next generation sequencing for preimplantation genetic testing of blastocysts aneuploidies in women of different ages. Ann. Agric. Environ. Med. 2016, 23, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Treff, N.R.; Forman, E.J.; Scott, R.T., Jr. Next-generation sequencing for preimplantation genetic diagnosis. Fertil. Steril. 2013, 99, e17–e18. [Google Scholar] [CrossRef]
- Gianaroli, L.; Magli, M.C.; Ferraretti, A.P.; Fortini, D.; Grieco, N. Pronuclear morphology and chromosomal abnormalities as scoring criteria for embryo selection. Fertil. Steril. 2003, 80, 341–349. [Google Scholar] [CrossRef]
- Machtinger, R.; Racowsky, C. Morphological systems of human embryo assessment and clinical evidence. Reprod. Biomed. Online 2013, 26, 210–221. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.L.; Hong, K.H.; Scott, R.T., Jr. Selecting the optimal time to perform biopsy for preimplantation genetic testing. Fertil. Steril. 2013, 100, 608–614. [Google Scholar] [CrossRef]
- Scott, R.T., Jr.; Upham, K.M.; Forman, E.J.; Hong, K.H.; Scott, K.L.; Taylor, D.; Tao, X.; Treff, N.R. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: A randomized controlled trial. Fertil. Steril. 2013, 100, 697–703. [Google Scholar] [CrossRef]
- Capalbo, A.; Ubaldi, F.M.; Rienzi, L.; Scott, R.; Treff, N. Detecting mosaicism in trophectoderm biopsies: Current challenges and future possibilities. Hum. Reprod. 2017, 32, 492–498. [Google Scholar] [CrossRef]
- Capalbo, A.; Treff, N.R.; Cimadomo, D.; Tao, X.; Upham, K.; Ubaldi, F.M.; Rienzi, L.; Scott, R.T., Jr. Comparison of array comparative genomic hybridization and quantitative real-time PCR-based aneuploidy screening of blastocyst biopsies. Eur. J. Hum. Genet. 2015, 23, 901–906. [Google Scholar] [CrossRef]
- Zhang, C.; Zhang, C.; Chen, S.; Yin, X.; Pan, X.; Lin, G.; Tan, Y.; Tan, K.; Xu, Z.; Hu, P.; et al. A single cell level based method for copy number variation analysis by low coverage massively parallel sequencing. PLoS ONE 2013, 8, e54236. [Google Scholar] [CrossRef]
- Simpson, J.L.; Rechitsky, S.; Kuliev, A. Next-generation sequencing for preimplantation genetic diagnosis. Fertil. Steril. 2013, 99, 1203–1204. [Google Scholar] [CrossRef]
- Yeung, Q.S.Y.; Zhang, Y.X.; Chung, J.P.W.; Lui, W.T.; Kwok, Y.K.Y.; Gui, B.; Kong, G.W.S.; Cao, Y.; Li, T.C.; Choy, K.W. A prospective study of non-invasive preimplantation genetic testing for aneuploidies (NiPGT-A) using next-generation sequencing (NGS) on spent culture media (SCM). J. Assist. Reprod. Genet. 2019, 36, 1609–1621. [Google Scholar] [CrossRef] [PubMed]
- Sachdeva, K.; Discutido, R.; Albuz, F.; Almekosh, R.; Peramo, B. Validation of Next-Generation Sequencer for 24-Chromosome Aneuploidy Screening in Human Embryos. Genet. Test. Mol. Biomarkers 2017, 21, 674–680. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Liu, Y.; Ma, P.; Chen, J.; Ding, T. Application of next generation sequencing for the preimplantation genetic test of 71 couples with one partner carrying a reciprocal or Robertsonian translocation. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 2020, 37, 563–566. [Google Scholar] [PubMed]
- García-Pascual, C.M.; Navarro-Sánchez, L.; Navarro, R.; Martínez, L.; Jiménez, J.; Rodrigo, L.; Simón, C.; Rubio, C. Optimized NGS Approach for Detection of Aneuploidies and Mosaicism in PGT-A and Imbalances in PGT-SR. Genes 2020, 11, 724. [Google Scholar] [CrossRef]
- Kung, A.; Bankowski, B.; Coates, A.; Wells, D. Validation of next-generation sequencing for comprehensive chromosome screening of embryos. Reprod. Biomed. Online 2015, 31, 760–769. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.; Rodrigo, L.; Garcia-Pascual, C.; Peinado, V.; Campos-Galindo, I.; Garcia-Herrero, S.; Simón, C. Clinical application of embryo aneuploidy testing by next-generation sequencing. Biol. Reprod. 2019, 101, 1083–1090. [Google Scholar] [CrossRef]
- Maxwell, S.M.; Colls, P.; Hodes-Wertz, B.; McCulloh, D.H.; McCaffrey, C.; Wells, D.; Munné, S.; Grifo, J.A. Why do euploid embryos miscarry? A case-control study comparing the rate of aneuploidy within presumed euploid embryos that resulted in miscarriage or live birth using next-generation sequencing. Fertil. Steril. 2016, 106, 1414–1419.e5. [Google Scholar] [CrossRef] [PubMed]
- Fiorentino, F.; Biricik, A.; Bono, S.; Spizzichino, L.; Cotroneo, E.; Cottone, G.; Kokocinski, F.; Michel, C.E. Development and validation of a next-generation sequencing-based protocol for 24-chromosome aneuploidy screening of embryos. Fertil. Steril. 2014, 101, 1375–1382. [Google Scholar] [CrossRef]
- Alyafee, Y.; Al Tuwaijri, A.; Alam, Q.; Umair, M.; Haddad, S.; Alharbi, M.; Ballow, M.; Al Drees, M.; AlAbdulrahman, A.; Al Khaldi, A.; et al. Next Generation Sequencing Based Non-invasive Prenatal Testing (NIPT): First Report From Saudi Arabia. Front. Genet. 2021, 12, 630787. [Google Scholar] [CrossRef] [PubMed]
- Hassold, T.; Merrill, M.; Adkins, K.; Freeman, S.; Sherman, S. Recombination and maternal age-dependent nondisjunction: Molecular studies of trisomy 16. Am. J. Hum. Genet. 1995, 57, 867–874. [Google Scholar]
- Chapuis, A.; Gala, A.; Ferrières-Hoa, A.; Mullet, T.; Bringer-Deutsch, S.; Vintejoux, E.; Torre, A.; Hamamah, S. Sperm quality and paternal age: Effect on blastocyst formation and pregnancy rates. Basic Clin. Androl. 2017, 27, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.X.; Chen, J.J.; Nabu, S.; Yeung, Q.S.Y.; Li, Y.; Tan, J.H.; Suksalak, W.; Chanchamroen, S.; Quangkananurug, W.; Wong, P.S.; et al. The Pregnancy Outcome of Mosaic Embryo Transfer: A Prospective Multicenter Study and Meta-Analysis. Genes 2020, 11, 973. [Google Scholar] [CrossRef] [PubMed]
| Results | Percentage % | Standard Deviation | |
|---|---|---|---|
| No of the embryos analyzed | 200 | 100 | |
| Mean female age | 35.15 | - | 4.64 |
| Mean male age | 44.5 | - | 8.95 |
| Informative embryos | 166 | 83 | |
| Euploid embryos | 46 | 23 | |
| Aneuploid embryos | 120 | 60 | |
| Result | Number of Embryos | Percentage of Total | Recommendation for Transfer | Pregnancy Rate | |
|---|---|---|---|---|---|
| Euoploidy | 46 | 23 | YES | 17% | |
| Aneuploidy | Complex Abnormal Embryo | 57 | 28.5 | NO | |
| Chaotic Abnormal Embryo | 33 | 16.5 | NO | ||
| Single Chromosome Aneuploidy | 20 | 10 | NO | ||
| Partial Chromosome Abnormality | 7 | 3.5 | NO | ||
| Mosaic Embryo | 3 | 1.5 | NO | ||
| Poor quality embryo | 34 | 17 | NO | ||
| Gender | Age (Years) | No. of Embryos | No. Euploidy | % of Euploidy | No. of Aneuploidy | % of Aneuploidy | No. of Poor Quality | % of Poor Quality |
|---|---|---|---|---|---|---|---|---|
| Maternal | 25–30 | 37 | 9 | 24.3 | 21 | 56.8 | 7 | 18.9 |
| 31–35 | 59 | 19 | 32.2 | 35 | 59.3 | 5 | 8.5 | |
| 36–40 | 69 | 17 | 24.6 | 42 | 60.9 | 10 | 14.5 | |
| ≥40 | 35 | 8 | 22.9 | 22 | 62.9 | 5 | 14.3 | |
| Paternal | 36–40 | 78 | 10 | 12.5 | 50 | 64.1 | 18 | 23.1 |
| 41–45 | 58 | 8 | 13.8 | 44 | 75.8 | 6 | 10.3 | |
| 46–50 | 12 | 2 | 16.6 | 8 | 66.7 | 2 | 16.6 | |
| ≥50 | 62 | 14 | 22.6 | 34 | 54.8 | 14 | 22.6 |
| Age (Years) | T | M | PD | Mo | Complex | Chaotic |
|---|---|---|---|---|---|---|
| 25–30 | 2 | 2 | 2 | 1 | 9 | 5 |
| 31–35 | 5 | 2 | 1 | - | 17 | 10 |
| 36–40 | 3 | 5 | 4 | 2 | 14 | 14 |
| ≥40 | 1 | - | - | - | 17 | 4 |
| Total | 11 | 9 | 7 | 3 | 57 | 33 |
| % of Total | 9.2 | 7.5 | 5.8 | 2.5 | 47.5 | 27.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyafee, Y.; Alam, Q.; Tuwaijri, A.A.; Umair, M.; Haddad, S.; Alharbi, M.; Alrabiah, H.; Al-Ghuraibi, M.; Al-Showaier, S.; Alfadhel, M. Next-Generation Sequencing-Based Pre-Implantation Genetic Testing for Aneuploidy (PGT-A): First Report from Saudi Arabia. Genes 2021, 12, 461. https://doi.org/10.3390/genes12040461
Alyafee Y, Alam Q, Tuwaijri AA, Umair M, Haddad S, Alharbi M, Alrabiah H, Al-Ghuraibi M, Al-Showaier S, Alfadhel M. Next-Generation Sequencing-Based Pre-Implantation Genetic Testing for Aneuploidy (PGT-A): First Report from Saudi Arabia. Genes. 2021; 12(4):461. https://doi.org/10.3390/genes12040461
Chicago/Turabian StyleAlyafee, Yusra, Qamre Alam, Abeer Al Tuwaijri, Muhammad Umair, Shahad Haddad, Meshael Alharbi, Hayat Alrabiah, Maha Al-Ghuraibi, Sahar Al-Showaier, and Majid Alfadhel. 2021. "Next-Generation Sequencing-Based Pre-Implantation Genetic Testing for Aneuploidy (PGT-A): First Report from Saudi Arabia" Genes 12, no. 4: 461. https://doi.org/10.3390/genes12040461
APA StyleAlyafee, Y., Alam, Q., Tuwaijri, A. A., Umair, M., Haddad, S., Alharbi, M., Alrabiah, H., Al-Ghuraibi, M., Al-Showaier, S., & Alfadhel, M. (2021). Next-Generation Sequencing-Based Pre-Implantation Genetic Testing for Aneuploidy (PGT-A): First Report from Saudi Arabia. Genes, 12(4), 461. https://doi.org/10.3390/genes12040461








