Atypical NF1 Microdeletions: Challenges and Opportunities for Genotype/Phenotype Correlations in Patients with Large NF1 Deletions
Abstract
1. Introduction
2. Patient and Methods
2.1. Genetic Analysis
2.2. Investigation of the Cognitive Abilities of Patient 310221
3. Results
3.1. Clinical Investigation of Patient 310221
3.2. Development and Cognitive Abilities
3.3. Characterisation of the Deletion in Patient 310221
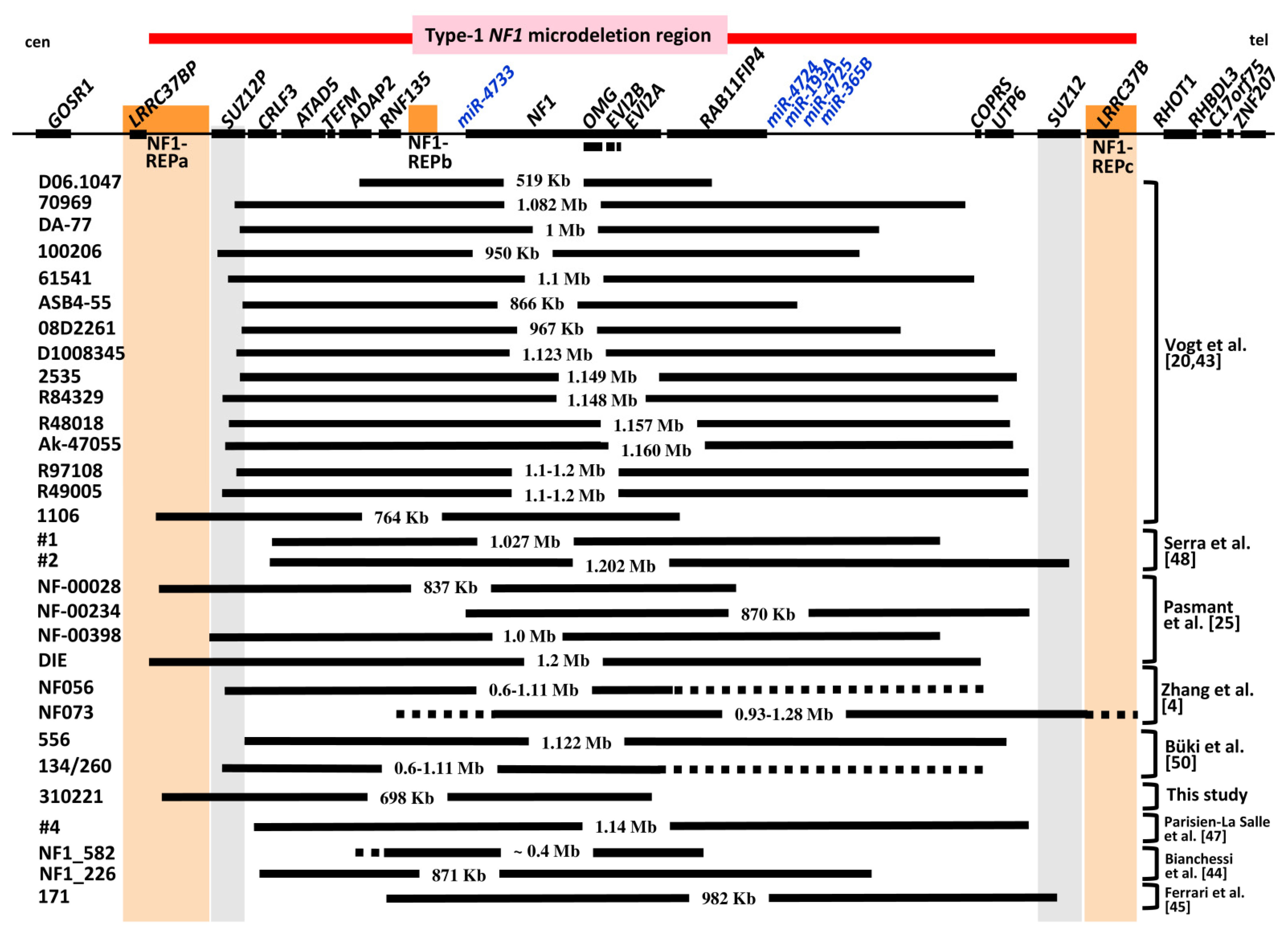
3.4. Comparison of the Deletion in Patient 310221 with Previously Reported Atypical NF1 Deletions
| Official HGNC Gene Symbol | MIM# | Official Gene Name | pLI Score |
|---|---|---|---|
| CRLF3 | 614853 | cytokine receptor like factor 3 | 0 |
| ATAD5 | 609534 | ATPase family, AAA domain containing 5 | 1.00 |
| TEFM | 616422 | transcription elongation factor, mitochondrial | 0.51 |
| ADAP2 | 608635 | ArfGAP with dual PH domains 2 | 0.00 |
| RNF135 | 611358 | ring finger protein 135 | 0.00 |
| NF1 | 162200 | neurofibromin | 1.00 |
| OMG | 164345 | oligodendrocyte myelin glycoprotein | 0.97 |
| EVI2B | 158381 | ecotropic viral integration site 2B | 0.06 |
| EVI2A | 158380 | ecotropic viral integration site 2A | 0.00 |
| RAB11FIP4 | 611999 | RAB11 family interacting protein 4 | 0.99 |
| COPRS | 616477 | coordinator of PRMT5 and differentiation stimulator | 0.25 |
| UTP6 | - | UTP6 small subunit processome component | 0 |
| SUZ12 | 613675 | SUZ12 polycomb repressive complex 2 subunit | 1.00 |
| LRRC37B | 616558 | leucine rich repeat containing 37B | 0.01 |
| Patient ID | Deletion Size in Mb | References |
|---|---|---|
| UWA 106-3 | 3.2–3.7 | [6,27,28,31] |
| UWA 155-1 | 2.1–2.7 | [6,31] |
| ID806 | ~7 | [29,37] |
| 3724A | 2.0–3.1 | [1,31] |
| UWA 113-1 | ~1 | [6] |
| BUD | 4.7 | [7,31,50] |
| BL | 3 | [30] |
| 6 | 3 | [32] |
| 118 | 1–2 | [33] |
| 442 | 2 | [35,50] |
| 806 | 5.5 | [25,36] |
| T165 | >2.2 | [36,37] |
| 282775 | >1.33 | [36,37] |
| T145 | 1.61–1.75 | [36,37] |
| SNF1-2 | ~1.3 | [38] |
| SNF1-3 | 1.84–2.8 | [38] |
| 552 | 2.7 | [39] |
| DUB | 7.6 | [40] |
| NF00358 | 1.2 | [41] |
| D05.2678 | 5.9 | [43] |
| D0801587 | 2 | [43] |
| 619 | 3 | [43,51] |
| ID not specified | 2.8 | [42] |
| NF040 | 1.27–1.46 | [5] |
| NF076 | 1.26–1.63 | [5] |
| NF1_31 | 1.8 | [44] |
| NF1_505 | 1.1 | [44] |
| NF1_724 | >1.6 | [44] |
| ID not specified | 1.695 | [46] |
| 2019 | 1.26–1.63 | [49] |
| 125 | 1.6 | [50] |
| Patient ID | Centromeric Breakpoint | Telomeric Breakpoint | Method of Analysis | SUZ12 Copies | Deletion Size | Mosaic | Reference |
|---|---|---|---|---|---|---|---|
| D06.1047 | ADAP2 | RAB11FIP4 | BS-PCR, MLPA | 2 | 519,291 bp | yes | [43] |
| 70969 | SUZ12P | RAB11FIP4 and COPRS | BS-PCR, MLPA | 2 | 1,082,491 bp | no | [43] |
| DA-77 | SUZ12P | between RAB11FIP4 and COPRS | BS-PCR, MLPA | 2 | 1,001,546 bp | yes | [43] |
| 100206 | SUZ12P | between RAB11FIP4 and COPRS | BS-PCR, MLPA | 2 | 950,940 bp | yes | [43] |
| 61541 | SUZ12P | between COPRS and UTP6 | BS-PCR, MLPA | 2 | 1,105,242 bp | yes | [43] |
| ASB4-55 | SUZ12P | between RAB11FIP4 and COPRS | BS-PCR, MLPA | 2 | 866,769 bp | yes | [43] |
| 08D2261 | SUZ12P | between RAB11FIP4 and COPRS | BS-PCR, MLPA | 2 | 976,455 bp | yes | [43] |
| D1008345 | SUZ12P | UTP6 | BS-PCR, MLPA | 2 | 1,123,78 bp | no | [43] |
| 2535 | SUZ12P | between UTP6 and SUZ12 | BS-PCR, MLPA | 2 | 1149,077 bp | no | [43] |
| R84329 | SUZ12P | UTP6 | BS-PCR, MLPA | 2 | 1,148,828 bp | yes | [43] |
| R48018 | SUZ12P | between UTP6 and SUZ12 | BS-PCR, MLPA | 2 | 1,157,378 bp | no | [43] |
| Ak-47055 | SUZ12P | between UTP6 and SUZ12 | BS-PCR, MLPA | 2 | 1,160,989 bp | yes | [43] |
| R97108 | SUZ12P | between UTP6 and SUZ12 | MLPA | 2 | 1.1–1.2 Mb | nd | [20] |
| R49005 | SUZ12P | between UTP6 and SUZ12 | MLPA | 2 | 1.1–1.2 Mb | nd | [20] |
| 1106 | NF1REPa | RAB11FIP4 | BS-PCR, MLPA | 2 | 764,080 bp | no | [43] |
| #1 | CRLF3 | 28 kb centromeric to COPRS | microarray | 2 | 1,027,355 bp | no | [48] |
| #2 | CRLF3 | SUZ12 | microarray | 1 | 1,202,659 bp | no | [48] |
| NF00028 | LRRC37BP | RAB11FIP4 | microarray | 2 | 837 Kb | nd | [25] |
| NF00234 | RNF135 | between UTP6 and SUZ12 | microarray | 2 | 870 Kb | nd | [25] |
| NF00398 | LRRC37BP | between RAB11FIP4 and COPRS | microarray | 2 | 1.0 Mb | nd | [25] |
| DIE | NF1-REPa | between COPRS and UTP6 | microarray | 2 | 1.2 Mb | nd | [25] |
| NF056 | SUZ12P | between NF1 exon 57 and UTP6 | MLPA | 2 | 0.6–1.11 Mb | nd | [4] |
| NF073 | between RNF135 and NF1 exon 1 | between LRRC37B and ZNF207 | MLPA | 1 | 0.93–1.28 Mb | nd | [4] |
| 556 | between SUZ12P and CRLF3 | UTP6 | microarray, MLPA | 2 | 1,122,447 bp | yes | [50] |
| 134/260 | SUZ12P | between NF1 exon 58 and UTP6 | MLPA | 2 | 0.6–1.11 Mb | no | [50] |
| 310221 | NF1-REPa | intron 57 of NF1 | microarray, MLPA | 2 | 698 Kb | no | this study |
| #4 | CRLF3 | between UTP6 and SUZ12 | microarray | 2 | 1,144,007 bp | nd | [47] |
| NF_582 | between ADAP2 and RNF135 | between NF1 exons 57 and 58 | MLPA | 2 | ~0.4 Mb | nd | [44] |
| NF_226 | CRLF3 | between RAB11FIP4 and COPRS | microarray | 2 | 871 Kb | nd | [44] |
| 171 | RNF135 | SUZ12 | microarray | 1 | 981,763 bp | nd | [45] |
3.5. Genotype/Phenotype Correlations in Patients with Atypical NF1 Deletions of Group #2
| Clinical Features | Patients | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 556 | 134 | 260 | 310221 | #1 | #2 | NF056 | NF073 | 171 | |
| m, 10y | f, 40y | m, 8y | m, 7y | f, 4y | f, 3y | f, 60y | f, 25y | m, 3y | |
| Broad nasal bridge | nd | nd | nd | − | − | + | nd | nd | nd |
| Downward slanting palpebral fissures | nd | nd | nd | − | − | nd | nd | nd | nd |
| Hypertelorism | − | + | + | +, mild | − | + | nd | nd | nd |
| Facial asymmetry | − | − | − | − | − | nd | nd | nd | nd |
| Coarse face | − | − | − | − | − | nd | nd | nd | nd |
| Micrognathia | nd | nd | nd | − | − | nd | nd | nd | nd |
| Broad neck | − | − | − | − | − | + | nd | nd | nd |
| Large hand and feet | − | − | − | − | − | nd | nd | nd | nd |
| Excess soft tissue on hands | − | − | − | − | − | nd | nd | nd | nd |
| Café-au-lait spots | + | + | + | + | + | + | + | + | + |
| Freckling | + | + | + | + | + | + | + | + | + |
| Lisch nodules | − | − | − | − | + | nd | nd | nd | − |
| Tall stature/overgrowth | − | − | − | − | − | − | nd | nd | + |
| Subcutaneous neurofibromas | − | + | − | − | − | − | nd | nd | nd |
| Cutaneous neurofibromas | − | − | − | − | − | − | + | + | nd |
| Externally visible plexiform neurofibromas | − | − | − | − | − | − | nd | nd | nd |
| Spinal neurofibromas | − | nd | nd | − | nd | nd | nd | nd | nd |
| Delay in development | − | − | + | + | + | global, + | nd | nd | + |
| Learning difficulties | − | − | − | + | + | + | nd | nd | nd |
| Speech difficulties | − | − | − | + | + | nd | nd | nd | nd |
| IQ | 89 | nd | nd | 93 | 88 | 55 | nd | nd | nd |
| Attention deficit and hyperactivity | − | − | − | + | + | nd | nd | nd | nd |
| Autism spectrum disorder | nd | nd | nd | + | nd | nd | nd | nd | nd |
| Scoliosis | − | + | − | +, mild | +, severe | nd | − | − | nd |
| Pectus excavatum | − | − | + | + | − | nd | − | − | nd |
| Bone cysts | − | − | − | − | − | nd | − | − | nd |
| Other bone abnormalities | − | − | − | pes planus | bilateral calcaneovalgus | genu valgum, pes planus | − | − | nd |
| Joint hyperflexibility | − | − | − | nd | nd | nd | nd | nd | nd |
| Macrocephaly | − | − | + | + | nd | + | nd | nd | − |
| Muscular hypotonia | − | − | − | + | + | − | nd | nd | + |
| MPNSTs | − | − | − | − | − | − | − | − | nd |
| T2 hyperintensities | − | nd | + | − | − | + | nd | nd | + |
| Optic gliomas | + | − | + | − | − | − | nd | nd | nd |
| SUZ12copy number | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cnossen, M.H.; van der Est, M.N.; Breuning, M.H.; van Asperen, C.J.; Breslau-Siderius, E.J.; van der Ploeg, A.T.; de Goede-Bolder, A.; van den Ouweland, A.M.; Halley, D.J.; Niermeijer, M.F. Deletions spanning the neurofibromatosis type 1 gene: Implications for genotype-phenotype correlations in neurofibromatosis type 1? Hum. Mutat. 1997, 9, 458–464. [Google Scholar] [CrossRef]
- Rasmussen, S.A.; Colman, S.D.; Ho, V.T.; Abernathy, C.R.; Arn, P.H.; Weiss, L.; Schwartz, C.; Saul, R.A.; Wallace, M.R. Constitutional and mosaic large NF1 gene deletions in neurofibromatosis type 1. J. Med. Genet. 1998, 35, 468–471. [Google Scholar] [CrossRef][Green Version]
- Kluwe, L.; Siebert, R.; Gesk, S.; Friedrich, R.E.; Tinschert, S.; Kehrer-Sawatzki, H.; Mautner, V.-F. Screening 500 unselected neurofibromatosis 1 patients for deletions of the NF1 gene. Hum. Mutat. 2004, 23, 111–116. [Google Scholar] [CrossRef]
- Zhang, J.; Tong, H.; Fu, X.; Zhang, Y.; Liu, J.; Cheng, R.; Liang, J.; Peng, J.; Sun, Z.; Liu, H.; et al. Molecular characterization of NF1 and neurofibromatosis type 1 genotype-phenotype correlations in a Chinese population. Sci. Rep. 2015, 5, 11291. [Google Scholar] [CrossRef] [PubMed]
- Kehrer-Sawatzki, H.; Mautner, V.-F.; Cooper, D.N. Emerging genotype–phenotype relationships in patients with large NF1 deletions. Hum. Genet. 2017, 136, 349–376. [Google Scholar] [CrossRef] [PubMed]
- Dorschner, M.O.; Sybert, V.P.; Weaver, M.; Pletcher, B.A.; Stephens, K. NF1 microdeletion breakpoints are clustered at flanking repetitive sequences. Hum. Mol. Genet. 2000, 9, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Jenne, D.E.; Tinschert, S.; Reimann, H.; Lasinger, W.; Thiel, G.; Hameister, H.; Kehrer-Sawatzki, H. Molecular characterization and gene content of breakpoint boundaries in patients with neurofibromatosis type 1 with 17q11.2 microdeletions. Am. J. Hum. Genet. 2001, 69, 516–527. [Google Scholar] [CrossRef] [PubMed][Green Version]
- López-Correa, C.; Dorschner, M.; Brems, H.; Lázaro, C.; Clementi, M.; Upadhyaya, M.; Dooijes, D.; Moog, U.; Kehrer-Sawatzki, H.; Rutkowski, J.L.; et al. Recombination hotspot in NF1 microdeletion patients. Hum. Mol. Genet. 2001, 10, 1387–1392. [Google Scholar] [CrossRef]
- Messiaen, L.; Vogt, J.; Bengesser, K.; Fu, C.; Mikhail, F.; Serra, E.; Garcia, C.L.; Cooper, D.N.; Lazaro, C.; Kehrer-Sawatzki, H. Mosaic type-1 NF1 microdeletions as a cause of both generalized and segmental neurofibromatosis type-1 (NF1). Hum. Mutat. 2011, 32, 213–219. [Google Scholar] [CrossRef]
- Summerer, A.; Schäfer, E.; Mautner, V.-F.; Messiaen, L.; Cooper, D.N.; Kehrer-Sawatzki, H. Ultra-deep amplicon sequencing indicates absence of low-grade mosaicism with normal cells in patients with type-1 NF1 deletions. Hum. Genet. 2018, 138, 73–81. [Google Scholar] [CrossRef]
- Correa, C.L.; Brems, H.; Lázaro, C.; Marynen, P.; Legius, E. Unequal meiotic crossover: A frequent cause of NF1 microdeletions. Am. J. Hum. Genet. 2000, 66, 1969–1974. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Neuhäusler, L.; Summerer, A.; Cooper, D.N.; Mautner, V.-F.; Kehrer-Sawatzki, H. Pronounced maternal parent-of-origin bias for type-1 NF1 microdeletions. Hum. Genet. 2018, 137, 365–373. [Google Scholar] [CrossRef]
- Forbes, S.H.; Dorschner, M.O.; Le, R.; Stephens, K. Genomic context of paralogous recombination hotspots mediating recurrent NF1 region microdeletion. Genes Chromosom. Cancer 2004, 41, 12–25. [Google Scholar] [CrossRef]
- De Raedt, T.; Stephens, M.; Heyns, I.; Brems, H.; Thijs, D.; Messiaen, L.; Stephens, K.; Lazaro, C.; Wimmer, K.; Kehrer-Sawatzki, H.; et al. Conservation of hotspots for recombination in low-copy repeats associated with the NF1 microdeletion. Nat. Genet. 2006, 38, 1419–1423. [Google Scholar] [CrossRef]
- Bengesser, K.; Vogt, J.; Mussotter, T.; Mautner, V.-F.; Messiaen, L.; Cooper, D.N.; Kehrer-Sawatzki, H. Analysis of crossover breakpoints yields new insights into the nature of the gene conversion events associated with large NF1 deletions mediated by nonallelic homologous recombination. Hum. Mutat. 2013, 35, 215–226. [Google Scholar] [CrossRef]
- Hillmer, M.; Wagner, D.; Summerer, A.; Daiber, M.; Mautner, V.-F.; Messiaen, L.; Cooper, D.N.; Kehrer-Sawatzki, H. Fine mapping of meiotic NAHR-associated crossovers causing large NF1 deletions. Hum. Mol. Genet. 2015, 25, 484–496. [Google Scholar] [CrossRef]
- Hillmer, M.; Summerer, A.; Mautner, V.-F.; Högel, J.; Cooper, D.N.; Kehrer-Sawatzki, H. Consideration of the haplotype diversity at nonallelic homologous recombination hotspots improves the precision of rearrangement breakpoint identification. Hum. Mutat. 2017, 38, 1711–1722. [Google Scholar] [CrossRef]
- Summerer, A.; Mautner, V.-F.; Upadhyaya, M.; Claes, K.; Högel, J.; Cooper, D.N.; Messiaen, L.; Kehrer-Sawatzki, H. Extreme clustering of type-1 NF1 deletion breakpoints co-locating with G-quadruplex forming sequences. Hum. Genet. 2018, 137, 511–520. [Google Scholar] [CrossRef]
- Steinmann, K.; Cooper, D.N.; Kluwe, L.; Chuzhanova, N.A.; Senger, C.; Serra, E.; Lazaro, C.; Gilaberte, M.; Wimmer, K.; Mautner, V.-F.; et al. Type 2 NF1 deletions are highly unusual by virtue of the absence of nonallelic homologous recombination hotspots and an apparent preference for female mitotic recombination. Am. J. Hum. Genet. 2007, 81, 1201–1220. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.; Mussotter, T.; Bengesser, K.; Claes, K.; Högel, J.; Chuzhanova, N.; Fu, C.; van den Ende, J.; Mautner, V.-F.; Cooper, D.N.; et al. Identification of recurrent type-2 NF1 microdeletions reveals a mitotic nonallelic homologous recombination hotspot underlying a human genomic disorder. Hum. Mutat. 2012, 33, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Kehrer-Sawatzki, H.; Kluwe, L.; Sandig, C.; Kohn, M.; Wimmer, K.; Krammer, U.; Peyrl, A.; Jenne, D.; Hansmann, I.; Mautner, V.-F. High frequency of mosaicism among patients with neurofibromatosis type 1 (NF1) with microdeletions caused by somatic recombination of the JJAZ1 gene. Am. J. Hum. Genet. 2004, 75, 410–423. [Google Scholar] [CrossRef] [PubMed]
- Roehl, A.C.; Vogt, J.; Mussotter, T.; Zickler, A.N.; Spöti, H.; Högel, J.; Chuzhanova, N.; Wimmer, K.; Kluwe, L.; Mautner, V.-F.; et al. Intrachromosomal mitotic nonallelic homologous recombination is the major molecular mechanism underlying type-2 NF1 deletions. Hum. Mutat. 2010, 31, 1163–1173. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Roehl, A.C.; Mussotter, T.; Cooper, D.N.; Kluwe, L.; Wimmer, K.; Högel, J.; Zetzmann, M.; Vogt, J.; Mautner, V.F.; Kehrer-Sawatzki, H. Tissue-specific differences in the proportion of mosaic large NF1 deletions are suggestive of a selective growth advantage of hematopoietic del(+/−) stem cells. Hum. Mutat. 2012, 33, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Bengesser, K.; Cooper, D.N.; Steinmann, K.; Kluwe, L.; Chuzhanova, N.; Wimmer, K.; Tatagiba, M.; Tinschert, S.; Mautner, V.-F.; Kehrer-Sawatzki, H. A novel third type of recurrent NF1 microdeletion mediated by nonallelic homologous recombination between LRRC37B-containing low-copy repeats in 17q11.2. Hum. Mutat. 2010, 31, 742–751. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pasmant, E.; Sabbagh, A.; Spurlock, G.; Laurendeau, I.; Grillo, E.; Hamel, M.J.; Martin, L.; Barbarot, S.; Leheup, B.; Rodriguez, D.; et al. NF1 microdeletions in neurofibromatosis type 1: From genotype to phenotype. Hum. Mutat. 2010, 31, 1506–1518. [Google Scholar] [CrossRef]
- Zickler, A.M.; Hampp, S.; Messiaen, L.; Bengesser, K.; Mussotter, T.; Roehl, A.C.; Wimmer, K.; Mautner, V.-F.; Kluwe, L.; Upadhyaya, M.; et al. Characterization of the nonallelic homologous recombination hotspot PRS3 associated with type-3 NF1 deletions. Hum. Mutat. 2012, 33, 372–383. [Google Scholar] [CrossRef] [PubMed]
- Kayes, L.M.; Riccardi, V.M.; Burke, W.; Bennett, R.L.; Stephens, K. Large de novo DNA deletion in a patient with sporadic neurofibromatosis 1, mental retardation, and dysmorphism. J. Med. Genet. 1992, 29, 686–690. [Google Scholar] [CrossRef]
- Kayes, L.M.; Burke, W.; Riccardi, V.M.; Bennett, R.; Ehrlich, P.; Rubenstein, A.; Stephens, K. Deletions spanning the neurofibromatosis 1 gene: Identification and phenotype of five patients. Am. J. Hum. Genet. 1994, 54, 424–436. [Google Scholar]
- Upadhyaya, M.; Roberts, S.H.; Maynard, J.; Sorour, E.; Thompson, P.W.; Vaughan, M.; Wilkie, A.; Hughes, H.E. A cytogenetic deletion, del(17)(q11.22q21.1), in a patient with sporadic neurofibromatosis type 1 (NF1) associated with dysmorphism and developmental delay. J. Med. Genet. 1996, 33, 148–152. [Google Scholar] [CrossRef]
- Riva, P.; Corrado, L.; Natacci, F.; Castorina, P.; Wu, B.-L.; Schneider, G.H.; Clementi, M.; Tenconi, R.; Korf, B.R.; Larizza, L. NF1 microdeletion syndrome: Refined FISH characterization of sporadic and familial deletions with locus-specific probes. Am. J. Hum. Genet. 2000, 66, 100–109. [Google Scholar] [CrossRef][Green Version]
- Kehrer-Sawatzki, H.; Tinschert, S.; Jenne, D.E. Heterogeneity of breakpoints in non-LCR-mediated large constitutional deletions of the 17q11.2 NF1 tumor suppressor region. J. Med. Genet. 2003, 40, E116. [Google Scholar] [CrossRef] [PubMed]
- Gervasini, C.; Orzan, F.N.; Bentivegna, A.; Colapietro, P.; Friso, A.; Tenconi, R.; Upadhyaya, M.; Larizza, L.; Corrado, L.; Venturin, M.; et al. Evidence for non-homologous end joining and non-allelic homologous recombination in atypical NF1 microdeletions. Hum. Genet. 2004, 115, 69–80. [Google Scholar] [CrossRef]
- Venturin, M.; Guarnieri, P.; Natacci, F.; Stabile, M.; Tenconi, R.; Clementi, M.; Hernandez, C.; Thompson, P.; Upadhyaya, M.; Larizza, L.; et al. Mental retardation and cardiovascular malformations in NF1 microdeleted patients point to candidate genes in 17q11.2. J. Med. Genet. 2004, 41, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Gervasini, C.; Venturin, M.; Orzan, F.N.; Friso, A.; Clementi, M.; Tenconi, R.; Larizza, L.; Riva, P. Uncommon Alu-mediated NF1 microdeletion with a breakpoint inside the NF1 gene. Genomics 2005, 85, 273–279. [Google Scholar] [CrossRef]
- Kehrer-Sawatzki, H.; Kluwe, L.; Mautner, V.-F. Extensively high load of internal tumors determined by whole body MRI scanning in a patient with neurofibromatosis type 1 and a non-LCR-mediated 2-Mb deletion in 17q11.2. Hum. Genet. 2005, 116, 466–475. [Google Scholar] [CrossRef]
- Mantripragada, K.K.; Thuresson, A.-C.; Piotrowski, A.; De Ståhl, T.D.; Menzel, U.; Grigelionis, G.; Ferner, R.E.; Griffiths, S.; Bolund, L.; Mautner, V.; et al. Identification of novel deletion breakpoints bordered by segmental duplications in the NF1 locus using high resolution array-CGH. J. Med. Genet. 2005, 43, 28–38. [Google Scholar] [CrossRef][Green Version]
- Wimmer, K.; Yao, S.; Claes, K.; Kehrer-Sawatzki, H.; Tinschert, S.; De Raedt, T.; Legius, E.; Callens, T.; Beiglböck, H.; Maertens, O.; et al. Spectrum of single- and multiexon NF1 copy number changes in a cohort of 1,100 unselected NF1 patients. Genes Chromosom. Cancer 2006, 45, 265–276. [Google Scholar] [CrossRef]
- Maertens, O.; De Schepper, S.; Vandesompele, J.; Brems, H.; Heyns, I.; Janssens, S.; Speleman, F.; Legius, E.; Messiaen, L. Molecular dissection of isolated disease features in mosaic neurofibromatosis type 1. Am. J. Hum. Genet. 2007, 81, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Kehrer-Sawatzki, H.; Schmid, E.; Fünsterer, C.; Kluwe, L.; Mautner, V.-F. Absence of cutaneous neurofibromas in an NF1 patient with an atypical deletion partially overlapping the common 1.4 Mb microdeleted region. Am. J. Med. Genet. Part A 2008, 146, 691–699. [Google Scholar] [CrossRef]
- Pasmant, E.; De Saint-Trivier, A.; Laurendeau, I.; Dieux-Coeslier, A.; Parfait, B.; Vidaud, M.; Vidaud, M.; Bieche, I. Characterization of a 7.6-Mb germline deletion encompassing the NF1 locus and about a hundred genes in an NF1 contiguous gene syndrome patient. Eur. J. Hum. Genet. 2008, 16, 1459–1466. [Google Scholar] [CrossRef]
- Pasmant, E.; Sabbagh, A.; Masliah-Planchon, J.; Haddad, V.; Hamel, M.-J.; Laurendeau, I.; Soulier, J.; Parfait, B.; Wolkenstein, P.; Bièche, I.; et al. Detection and characterization of NF1 microdeletions by custom high resolution array CGH. J. Mol. Diagn. 2009, 11, 524–529. [Google Scholar] [CrossRef][Green Version]
- Taylor Tavares, A.L.; Willatt, L.; Armstrong, R.; Simonic, I.; Park, S.-M. Mosaic deletion of the NF1 gene in a patient with cognitive disability and dysmorphic features but without diagnostic features of NF1. Am. J. Med. Genet. Part A 2013, 161, 1185–1188. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.; Bengesser, K.; Claes, K.; Wimmer, K.; Mautner, V.-F.; Van Minkelen, R.; Legius, E.; Brems, H.; Upadhyaya, M.; Högel, J.; et al. SVA retrotransposon insertion-associated deletion represents a novel mutational mechanism underlying large genomic copy number changes with non-recurrent breakpoints. Genome Biol. 2014, 15, R80. [Google Scholar] [CrossRef]
- Bianchessi, D.; Morosini, S.; Saletti, V.; Ibba, M.C.; Natacci, F.; Esposito, S.; Cesaretti, C.; Riva, D.; Finocchiaro, G.; Eoli, M. 126 novel mutations in Italian patients with neurofibromatosis type 1. Mol. Genet. Genom. Med. 2015, 3, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, L.; Scuvera, G.; Tucci, A.; Bianchessi, D.; Rusconi, F.; Menni, F.; Battaglioli, E.; Milani, D.; Riva, P. Identification of an atypical microdeletion generating the RNF135-SUZ12 chimeric gene and causing a position effect in an NF1 patient with overgrowth. Hum. Genet. 2017, 136, 1329–1339. [Google Scholar] [CrossRef]
- Al-Araimi, M.; Hamza, N.; Al Yahmadi, A.; Al Mazrooey, H.; Elsheikh, A.; Al Amri, A.; Al Harrasi, S.; Hausdorf, L.; Mula-Abed, W. Rare NF1 microdeletion syndrome in an Omani patient. Clin. Case Rep. 2018, 6, 2424–2426. [Google Scholar] [CrossRef]
- Parisien-La Salle, S.; Dumas, N.; Rondeau, G.; Latour, M.; Bourdeau, I. Isolated pheochromocytoma in a 73-year-old man with no clinical manifestations of type 1 neurofibromatosis carrying an unsuspected deletion of the entire NF1 gene. Front Endocrinol 2019, 10, 546. [Google Scholar] [CrossRef]
- Serra, G.; Antona, V.; Corsello, G.; Zara, F.; Piro, E.; Falsaperla, R. NF1 microdeletion syndrome: Case report of two new patients. Ital. J. Pediatr. 2019, 45, 1–7. [Google Scholar] [CrossRef]
- Kluwe, L.; Friedrich, R.E.; Farschtschi, S.C.; Hagel, C.; Kehrer-Sawatzki, H.; Mautner, V. Null phenotype of neurofibromatosis type 1 in a carrier of a heterozygous atypical NF1 deletion due to mosaicism. Hum. Mutat. 2020, 41, 1226–1231. [Google Scholar] [CrossRef] [PubMed]
- Büki, G.; Zsigmond, A.; Czakó, M.; Szalai, R.; Antal, G.; Farkas, V.; Fekete, G.; Nagy, D.; Széll, M.; Tihanyi, M.; et al. Genotype-phenotype associations in patients with type-1, type-2, and atypical NF1 microdeletions. Front. Genet. 2021, 12, 673025. [Google Scholar] [CrossRef]
- Kehrer-Sawatzki, H.; Kluwe, L.; Salamon, J.; Well, L.; Farschtschi, S.; Rosenbaum, T.; Mautner, V.-F. Clinical characterization of children and adolescents with NF1 microdeletions. Child’s Nerv. Syst. 2020, 36, 2297–2310. [Google Scholar] [CrossRef] [PubMed]
- Ottenhoff, M.M.J.; Msc, A.B.R.; Mous, S.E.; Plasschaert, E.; Msc, D.G.; Brems, H.; Oostenbrink, R.; Van Minkelen, R.; Nellist, M.; Schorry, E.; et al. Examination of the genetic factors underlying the cognitive variability associated with neurofibromatosis type 1. Genet. Med. 2020, 22, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Pacot, L.; Vidaud, D.; Sabbagh, A.; Laurendeau, I.; Briand-Suleau, A.; Coustier, A.; Maillard, T.; Barbance, C.; Morice-Picard, F.; Sigaudy, S.; et al. Severe phenotype in patients with large deletions of NF1. Cancers 2021, 13, 2963. [Google Scholar] [CrossRef] [PubMed]
- Well, L.; Döbel, K.; Kluwe, L.; Bannas, P.; Farschtschi, S.; Adam, G.; Mautner, V.F.; Salamon, J. Genotype-phenotype correlation in neurofibromatosis type-1: NF1 whole gene deletions lead to high tumor-burden and increased tumor-growth. PLoS Genet 2021, 17, e1009517. [Google Scholar] [CrossRef]
- Hellbrügge, T. Münchener Funktionelle Entwicklungsdiagnostik, Zweites und Drittes Lebensjahr. Durchführungs-, Beurteilungs- und Interpretationshinweise; 4. korrigierte und Erweiterte Auflage; Deutsche Akademie für Entwicklungsrehabilitation: München, Germany, 1994. [Google Scholar]
- Köhler, G.; Egelkraut, H. Münchener Funktionelle Entwicklungsdiagnostik für das Zweite und Dritte Lebensjahr, Handanweisung; Universität München, Institut für Soziale Pädiatrie und Jugendmedizin: München, Germany, 1984. [Google Scholar]
- Wechsler, D. The Wechsler Preschool and Primary Scale of Intelligence, 4rd ed.; The Psychological Corporation: San Antonio, TX, USA, 2012. [Google Scholar]
- Kaufman, A.S.; Kaufman, N.L. Kaufman Assessment Battery for Children: Second Edition (KABC-II); AGS Publishing: Circle Pines, MN, USA, 2004. [Google Scholar]
- Edwards, S.; Fletcher, P.; Garman, M.; Hughes, A.; Letts, C.; Sinka, I. Reynell Developmental Language Scales III—The University of Reading Edition; GL Assessments: London, UK, 1997. [Google Scholar]
- Grimm, H. Sprachentwicklungstest für Zweijährige Kinder. SETK-2; Hogrefe: Göttingen, Germany, 2000. [Google Scholar]
- Grimm, H. Sprachentwicklungstest für drei- bis Fünfjährige Kinder—SETK 3-5; Hogrefe: Göttingen, Germany, 2001. [Google Scholar]
- Kiese-Himmel, C. AWST-R—Aktiver Wortschatztest für 3- bis 5-Jährige Kinder: Manual, Neuaufl. ed.; Hogrefe Verlag: Göttingen, Germany, 2005; ISBN 13-978-3801719777. [Google Scholar]
- Beery, K.; Buktenica, N.; Beery, N. Beery-Buktenica Developmental Test of Visual-Motor Integration Sixth Edition (Beery VMI) Visual Perception Forms; Psychological Corporation Ltd.: Tokyo, Japan, 2010; Volume 25, p. 46246. ISBN 978-0-7491-6028-9. [Google Scholar]
- Lek, M.; Karczewski, K.J.; Minikel, E.V.; Samocha, K.E.; Banks, E.; Fennell, T.; O’Donnell-Luria, A.H.; Ware, J.S.; Hill, A.J.; Cummings, B.B.; et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 2016, 536, 285–291. [Google Scholar] [CrossRef]
- Soucy, E.A.; Gao, F.; Gutmann, D.H.; Dunn, C.M. Developmental delays in children with neurofibromatosis type 1. J. Child Neurol. 2012, 27, 641–644. [Google Scholar] [CrossRef]
- Wessel, L.; Gao, F.; Gutmann, D.H.; Dunn, C.M. Longitudinal analysis of developmental delays in children with neurofibromatosis type 1. J. Child Neurol. 2013, 28, 1689–1693. [Google Scholar] [CrossRef]
- Kolesnik, A.M.; Jones, E.J.H.; Garg, S.; Green, J.; Charman, T.; Johnson, M.H.; EDEN-BASIS Team. Early development of infants with neurofibromatosis type 1: A case series. Mol. Autism 2017, 8, 62. [Google Scholar] [CrossRef]
- Arnold, S.S.; Payne, J.M.; Lorenzo, J.; North, K.N.; Barton, B. Preliteracy impairments in children with neurofibromatosis type 1. Dev. Med. Child Neurol. 2018, 60, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Thompson, H.L. Evaluation of phonological processing skills of young children with neurofibromatosis type 1. Dev. Med. Child Neurol. 2018, 60, 642. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.A.; MacWilliams, B.; Carey, J.C.; Viskochil, D.H.; D’Astous, J.L.; Stevenson, D.A. Motor proficiency in children with neurofibromatosis type 1. Pediatr. Phys. Ther. 2010, 22, 344–348. [Google Scholar] [CrossRef]
- Lorenzo, J.; Barton, B.; Acosta, M.T.; North, K. Mental, motor, and language development of toddlers with neurofibromatosis Type 1. J. Pediatr. 2011, 158, 660–665. [Google Scholar] [CrossRef]
- Lehtonen, A.; Howie, E.; Trump, D.; Huson, S.M. Behaviour in children with neurofibromatosis type 1: Cognition, executive function, attention, emotion, and social competence. Dev. Med. Child Neurol. 2012, 55, 111–125. [Google Scholar] [CrossRef]
- Krab, L.C.; De Goede-Bolder, A.; Aarsen, F.K.; Moll, H.A.; De Zeeuw, C.I.; Elgersma, Y.; Van Der Geest, J.N. Motor learning in children with neurofibromatosis type I. Cerebellum 2010, 10, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Debrabant, J.; Plasschaert, E.; Caeyenberghs, K.; Vingerhoets, G.; Legius, E.; Janssens, S.; Van Waelvelde, H. Deficient motor timing in children with neurofibromatosis type 1. Res. Dev. Disabil. 2014, 35, 3131–3138. [Google Scholar] [CrossRef] [PubMed]
- Plasschaert, E.; Van Eylen, L.; Descheemaeker, M.; Noens, I.; Legius, E.; Steyaert, J. Executive functioning deficits in children with neurofibromatosis type 1: The influence of intellectual and social functioning. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2016, 171, 348–362. [Google Scholar] [CrossRef] [PubMed]
- Descheemaeker, M.; Roelandts, K.; De Raedt, T.; Brems, H.; Fryns, J.; Legius, E. Intelligence in individuals with a neurofibromatosis type 1 microdeletion. Am. J. Med. Genet. 2004, 131, 325–326. [Google Scholar] [CrossRef]
- Mautner, V.-F.; Kluwe, L.; Friedrich, R.E.; Roehl, A.C.; Bammert, S.; Hogel, J.; Spori, H.; Cooper, D.N.; Kehrer-Sawatzki, H. Clinical characterisation of 29 neurofibromatosis type-1 patients with molecularly ascertained 1.4 Mb type-1 NF1 deletions. J. Med. Genet. 2010, 47, 623–630. [Google Scholar] [CrossRef]
- Uechi, L.; Jalali, M.; Wilbur, J.D.; French, J.L.; Jumbe, N.L.; Meaney, M.J.; Gluckman, P.D.; Karnani, N.; Sakhanenko, N.A.; Galas, D.J.; et al. Complex genetic dependencies among growth and neurological phenotypes in healthy children: Towards deciphering developmental mechanisms. PLoS ONE 2020, 15, e0242684. [Google Scholar] [CrossRef]
- De Raedt, T.; Beert, E.; Pasmant, E.; Luscan, A.; Brems, H.; Ortonne, N.; Helin, K.; Hornick, J.L.; Mautner, V.; Kehrer-Sawatzki, H.; et al. PRC2 loss amplifies Ras-driven transcription and confers sensitivity to BRD4-based therapies. Nature 2014, 514, 247–251. [Google Scholar] [CrossRef]
- Lee, W.; Teckie, S.; Wiesner, T.; Ran, L.; Granada, C.N.P.; Lin, M.; Zhu, S.; Cao, Z.; Liang, Y.; Sboner, A.; et al. PRC2 is recurrently inactivated through EED or SUZ12 loss in malignant peripheral nerve sheath tumors. Nat. Genet. 2014, 46, 1227–1232. [Google Scholar] [CrossRef]
- Zhang, M.; Wang, Y.; Jones, S.; Sausen, M.; McMahon, K.; Sharma, R.; Wang, Q.; Belzberg, A.J.; Chaichana, K.; Gallia, G.L.; et al. Somatic mutations of SUZ12 in malignant peripheral nerve sheath tumors. Nat. Genet. 2014, 46, 1170–1172. [Google Scholar] [CrossRef]
- Imagawa, E.; Albuquerque, E.V.; Isidor, B.; Mitsuhashi, S.; Mizuguchi, T.; Miyatake, S.; Takata, A.; Miyake, N.; Boguszewski, M.C.; Boguszewski, C.; et al. Novel SUZ12 mutations in Weaver-like syndrome. Clin. Genet. 2018, 94, 461–466. [Google Scholar] [CrossRef]
- Cyrus, S.S.; Cohen, A.S.A.; Agbahovbe, R.; Avela, K.; Yeung, K.S.; Chung, B.H.Y.; Luk, H.; Tkachenko, N.; Choufani, S.; Weksberg, R.; et al. Rare SUZ12 variants commonly cause an overgrowth phenotype. Am. J. Med. Genet. Part C Semin. Med. Genet. 2019, 181, 532–547. [Google Scholar] [CrossRef]
- Cyrus, S.; Burkardt, D.; Weaver, D.D.; Gibson, W. PRC2-complex related dysfunction in overgrowth syndromes: A review of EZH2, EED, and SUZ12 and their syndromic phenotypes. Am. J. Med. Genet. Part C Semin. Med. Genet. 2019, 181, 519–531. [Google Scholar] [CrossRef]
- van Asperen, C.J.; Overweg-Plandsoen, W.C.; Cnossen, M.H.; van Tijn, D.A.; Hennekam, R.C. Familial neurofibromatosis type 1 associated with an overgrowth syndrome resembling Weaver syndrome. J. Med. Genet. 1998, 35, 323–327. [Google Scholar] [CrossRef][Green Version]
- Spiegel, M.; Oexle, K.; Horn, D.; Windt, E.; Buske, A.; Albrecht, B.; Prott, E.-C.; Seemanová, E.; Seidel, J.; Rosenbaum, T.; et al. Childhood overgrowth in patients with common NF1 microdeletions. Eur. J. Hum. Genet. 2005, 13, 883–888. [Google Scholar] [CrossRef] [PubMed]
- Mensink, K.A.; Ketterling, R.; Flynn, H.C.; Knudson, R.A.; Lindor, N.M.; Heese, B.A.; Spinner, R.J.; Babovic-Vuksanovic, D. Connective tissue dysplasia in five new patients with NF1 microdeletions: Further expansion of phenotype and review of the literature. J. Med. Genet. 2005, 43, e08. [Google Scholar] [CrossRef] [PubMed]
- Ning, X.; Farschtschi, S.; Jones, A.; Kehrer-Sawatzki, H.; Mautner, V.-F.; Friedman, J.M. Growth in neurofibromatosis 1 microdeletion patients. Clin. Genet. 2015, 89, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Douglas, J.; Cilliers, D.; Coleman, K.; Tatton-Brown, K.; Barker, K.; Bernhard, B.; Burn, J.; Huson, S.; Josifova, D.; Lacombe, D.; et al. Mutations in RNF135, a gene within the NF1 microdeletion region, cause phenotypic abnormalities including overgrowth. Nat. Genet. 2007, 39, 963–965. [Google Scholar] [CrossRef] [PubMed]
- Pobric, G.; Taylor, J.R.; Ramalingam, H.M.; Pye, E.; Robinson, L.; Vassallo, G.; Jung, J.; Bhandary, M.; Szumanska-Ryt, K.; Theodosiou, L.; et al. Cognitive and electrophysiological correlates of working memory impairments in neurofibromatosis type 1. J. Autism Dev. Disord. 2021, 8, 1–17. [Google Scholar] [CrossRef]
- Mautner, V.F.; Kluwe, L.; Thakker, S.D.; Leark, R.A. Treatment of ADHD in neurofibromatosis type 1. Dev. Med. Child Neurol. 2002, 44, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Lehtonen, A.; Huson, S.M.; Emsley, R.; Trump, D.; Evans, D.G.; Green, J. Autism and other psychiatric comorbidity in neurofibromatosis type 1: Evidence from a population-based study. Dev. Med. Child Neurol. 2013, 55, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Isenberg, J.C.; Templer, A.; Gao, F.; Titus, J.B.; Gutmann, D.H. Attention skills in children with neurofibromatosis type 1. J. Child Neurol. 2012, 28, 45–49. [Google Scholar] [CrossRef]
- Heimgärtner, M.; Granström, S.; Haas-Lude, K.; Leark, R.A.; Mautner, V.F.; Lidzba, K. Attention deficit predicts intellectual functioning in children with neurofibromatosis type 1. Int. J. Pediatr. 2019, 10, 9493837. [Google Scholar] [CrossRef]
- Lion-François, L.; Herbillon, V.; Peyric, E.; Mercier, C.; Gérard, D.; Ginhoux, T.; Coutinho, V.; Kemlin, I.; Kassai, B.; Desportes, V.; et al. Attention and executive disorders in neurofibromatosis 1: Comparison between NF1 with ADHD symptomatology (NF1 + ADHD) and ADHD per se. J. Atten. Disord. 2017, 24, 1807–1823. [Google Scholar] [CrossRef]
- Payne, J.M.; Haebich, K.M.; MacKenzie, R.; Walsh, K.; Hearps, S.J.C.; Coghill, D.; Barton, B.; Pride, N.A.; Ullrich, N.J.; Tonsgard, J.H.; et al. Cognition, ADHD symptoms, and functional impairment in children and adolescents with neurofibromatosis type 1. J. Atten. Disord. 2021, 25, 1177–1186. [Google Scholar] [CrossRef]
- Garg, S.; Heuvelman, H.; Huson, S.; Tobin, H.; Green, J. Northern UK NF1 Research Network. Sex bias in autism spectrum disorder in neurofibromatosis type 1. J. Neurodev. Disord. 2016, 8, 26. [Google Scholar] [CrossRef]
- Eijk, S.; Mous, S.E.; Dieleman, G.C.; Dierckx, B.; Rietman, A.B.; De Nijs, P.F.A.; Hoopen, L.W.T.; Van Minkelen, R.; Elgersma, Y.; Catsman-Berrevoets, C.E.; et al. Autism spectrum disorder in an unselected cohort of children with neurofibromatosis type 1 (NF1). J. Autism Dev. Disord. 2018, 48, 2278–2285. [Google Scholar] [CrossRef]
- Morris, S.M.; Gutmann, D.H. A genotype—phenotype correlation for quantitative autistic trait burden in neurofibromatosis 1. Neurol. 2018, 90, 377–379. [Google Scholar] [CrossRef]
- Haebich, K.M.; Pride, N.A.; Walsh, K.; Chisholm, A.; Rouel, M.; Maier, A.; Anderson, V.; Barton, B.; Silk, T.; Korgaonkar, M.; et al. Understanding autism spectrum disorder and social functioning in children with neurofibromatosis type 1: Protocol for a cross-sectional multimodal study. BMJ Open 2019, 9, e030601. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.M.; Acosta, M.T.; Garg, S.; Green, J.; Huson, S.; Legius, E.; North, K.N.; Payne, J.M.; Plasschaert, E.; Frazier, T.W.; et al. Disease burden and symptom structure of autism in neurofibromatosis type 1: A study of the International NF1-ASD Consortium Team (INFACT). JAMA Psychiatry 2016, 73, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Wegscheid, M.L.; Anastasaki, C.; Hartigan, K.A.; Cobb, O.M.; Papke, J.B.; Traber, J.N.; Morris, S.M.; Gutmann, D.H. Patient-derived iPSC-cerebral organoid modeling of the 17q11.2 microdeletion syndrome establishes CRLF3 as a critical regulator of neurogenesis. Cell Rep. 2021, 36, 109315. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kehrer-Sawatzki, H.; Wahlländer, U.; Cooper, D.N.; Mautner, V.-F. Atypical NF1 Microdeletions: Challenges and Opportunities for Genotype/Phenotype Correlations in Patients with Large NF1 Deletions. Genes 2021, 12, 1639. https://doi.org/10.3390/genes12101639
Kehrer-Sawatzki H, Wahlländer U, Cooper DN, Mautner V-F. Atypical NF1 Microdeletions: Challenges and Opportunities for Genotype/Phenotype Correlations in Patients with Large NF1 Deletions. Genes. 2021; 12(10):1639. https://doi.org/10.3390/genes12101639
Chicago/Turabian StyleKehrer-Sawatzki, Hildegard, Ute Wahlländer, David N. Cooper, and Victor-Felix Mautner. 2021. "Atypical NF1 Microdeletions: Challenges and Opportunities for Genotype/Phenotype Correlations in Patients with Large NF1 Deletions" Genes 12, no. 10: 1639. https://doi.org/10.3390/genes12101639
APA StyleKehrer-Sawatzki, H., Wahlländer, U., Cooper, D. N., & Mautner, V.-F. (2021). Atypical NF1 Microdeletions: Challenges and Opportunities for Genotype/Phenotype Correlations in Patients with Large NF1 Deletions. Genes, 12(10), 1639. https://doi.org/10.3390/genes12101639







