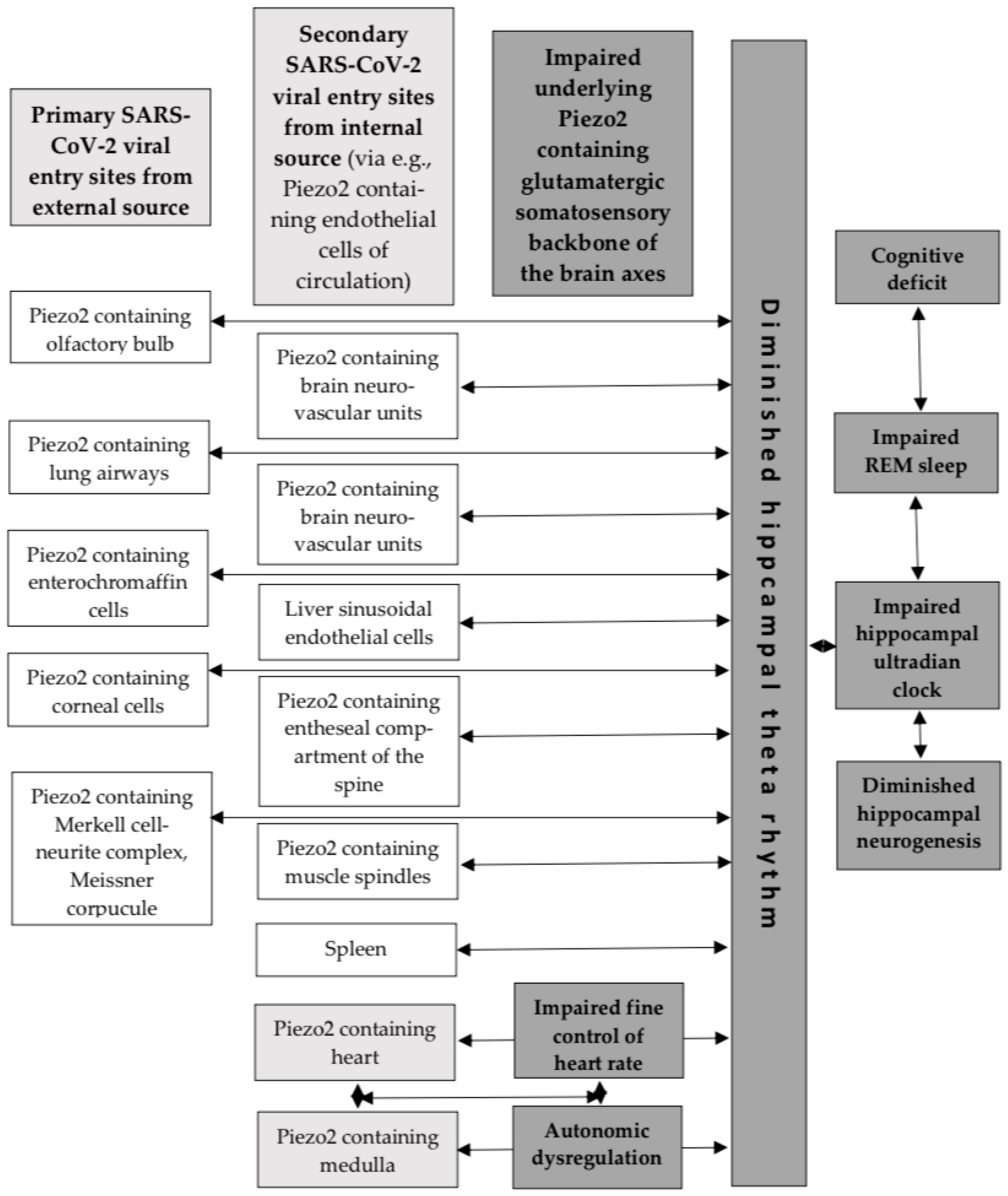
Underlying Piezo2 Channelopathy-Induced Neural Switch of COVID-19 Infection
Abstract
1. Introduction
2. Proton Affinity Switch
3. Pro-Inflammatory Switch
4. Hippocampus and the Medulla
5. Limitations
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACE2 | angiotensin-converting enzyme 2 |
| ANLS | astrocyte neurite lactate shuttle |
| ER | endoplasmic reticulum |
| HS | heparan sulfate |
| NVU | neurovascular unit |
| OXPHOS | oxidative phosphorylation |
| RBD | receptor-binding domain |
| REM | rapid eye movement |
| SERCA | sarco/endoplasmic reticulum calcium ATPases |
References
- Fekete, R.; Simats, A.; Biro, E.; Posfai, B.; Cserep, C.; Schwarcz, A.D.; Szabadits, E.; Kornyei, Z.; Toth, K.; Ficho, E.; et al. Microglia dysfunction, neurovascular inflammation and focal neuropathologies are linked to IL-1- and IL-6-related systemic inflammation in COVID-19. Nat. Neurosci. 2025, 28, 558–576. [Google Scholar] [CrossRef]
- Sonkodi, B. Delayed-Onset Muscle Soreness Begins with a Transient Neural Switch. Int. J. Mol. Sci. 2025, 26, 2319. [Google Scholar] [CrossRef] [PubMed]
- Medvedev, Z.A. An attempt at a rational classification of theories of ageing. Biol. Rev. Camb. Philos. Soc. 1990, 65, 375–398. [Google Scholar] [CrossRef]
- Sonkodi, B. Acquired Piezo2 Channelopathy is One Principal Gateway to Pathophysiology. Front. Biosci. 2025, 30, 33389. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Liu, J.; Deng, X.; Bo, L. Understanding COVID-19-associated endothelial dysfunction: Role of PIEZO1 as a potential therapeutic target. Front. Immunol. 2024, 15, 1281263. [Google Scholar] [CrossRef]
- Soung, A.L.; Vanderheiden, A.; Nordvig, A.S.; Sissoko, C.A.; Canoll, P.; Mariani, M.B.; Jiang, X.; Bricker, T.; Rosoklija, G.B.; Arango, V.; et al. COVID-19 induces CNS cytokine expression and loss of hippocampal neurogenesis. Brain 2022, 145, 4193–4201. [Google Scholar] [CrossRef]
- Sonkodi, B.; Nagy, Z.; Keller-Pintér, A.; Klivényi, P.; Széll, M. Likely pathogenic variants of SDC3, KCNA2, KCNK1, KCNK16 and HSF1 are in support of acquired irreversible PIEZO2 channelopathy in ALS onset. Res. Sq. 2025. preprint. [Google Scholar] [CrossRef]
- Kearns, F.L.; Sandoval, D.R.; Casalino, L.; Clausen, T.M.; Rosenfeld, M.A.; Spliid, C.B.; Amaro, R.E.; Esko, J.D. Spike-heparan sulfate interactions in SARS-CoV-2 infection. Curr. Opin. Struct. Biol. 2022, 76, 102439. [Google Scholar] [CrossRef]
- Kim, S.H.; Kearns, F.L.; Rosenfeld, M.A.; Votapka, L.; Casalino, L.; Papanikolas, M.; Amaro, R.E.; Freeman, R. SARS-CoV-2 evolved variants optimize binding to cellular glycocalyx. Cell Rep. Phys. Sci. 2023, 4, 101346. [Google Scholar] [CrossRef]
- Nie, C.; Sahoo, A.K.; Netz, R.R.; Herrmann, A.; Ballauff, M.; Haag, R. Charge Matters: Mutations in Omicron Variant Favor Binding to Cells. Chembiochem 2022, 23, e202100681. [Google Scholar] [CrossRef]
- Dér, A.; Kelemen, L.; Fábián, L.; Taneva, S.G.; Fodor, E.; Páli, T.; Cupane, A.; Cacace, M.G.; Ramsden, J.J. Interfacial Water Structure Controls Protein Conformation. J. Phys. Chem. B 2007, 111, 5344–5350. [Google Scholar] [CrossRef]
- Langmár, G.; Sümegi, T.; Fülöp, B.; Pozsgai, L.; Mocsai, T.; Tóth, M.; Racz, L.; Kopper, B.; Dér, A.; Búzás, A.; et al. HRV Alterations During Delayed-Onset Muscle Soreness Inducing Exercise—With Piezo2 Interpretation. Preprints 2025. [Google Scholar] [CrossRef]
- Hudak, A.; Letoha, A.; Szilak, L.; Letoha, T. Contribution of Syndecans to the Cellular Entry of SARS-CoV-2. Int. J. Mol. Sci. 2021, 22, 5336. [Google Scholar] [CrossRef]
- Hudak, A.; Morgan, G.; Bacovsky, J.; Patai, R.; Polgar, T.F.; Letoha, A.; Pettko-Szandtner, A.; Vizler, C.; Szilak, L.; Letoha, T. Biodistribution and Cellular Internalization of Inactivated SARS-CoV-2 in Wild-Type Mice. Int. J. Mol. Sci. 2022, 23, 7609. [Google Scholar] [CrossRef]
- Sonkodi, B. PIEZO2 Proton Affinity and Availability May Also Regulate Mechanical Pain Sensitivity, Drive Central Sensitization and Neurodegeneration. Int. J. Mol. Sci. 2025, 26, 1246. [Google Scholar] [CrossRef]
- Sang, P.; Chen, Y.Q.; Liu, M.T.; Wang, Y.T.; Yue, T.; Li, Y.; Yin, Y.R.; Yang, L.Q. Electrostatic Interactions Are the Primary Determinant of the Binding Affinity of SARS-CoV-2 Spike RBD to ACE2: A Computational Case Study of Omicron Variants. Int. J. Mol. Sci. 2022, 23, 4796. [Google Scholar] [CrossRef] [PubMed]
- Verkhivker, G.; Agajanian, S.; Kassab, R.; Krishnan, K. Probing Mechanisms of Binding and Allostery in the SARS-CoV-2 Spike Omicron Variant Complexes with the Host Receptor: Revealing Functional Roles of the Binding Hotspots in Mediating Epistatic Effects and Communication with Allosteric Pockets. Int. J. Mol. Sci. 2022, 23, 1542. [Google Scholar] [CrossRef] [PubMed]
- Agmon, N. The Grotthuss mechanism. Chem. Phys. Lett. 1995, 244, 456–462. [Google Scholar] [CrossRef]
- Berta, B.; Tordai, H.; Lukacs, G.L.; Papp, B.; Enyedi, A.; Padanyi, R.; Hegedus, T. SARS-CoV-2 envelope protein alters calcium signaling via SERCA interactions. Sci. Rep. 2024, 14, 21200. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; He, T.; Chen, S.; Yang, D.; Yi, W.; Cao, H.; Xiao, G. Roles of mechanosensitive channel Piezo1/2 proteins in skeleton and other tissues. Bone Res. 2021, 9, 44. [Google Scholar] [CrossRef]
- Zhang, T.; Chi, S.; Jiang, F.; Zhao, Q.; Xiao, B. A protein interaction mechanism for suppressing the mechanosensitive Piezo channels. Nat. Commun. 2017, 8, 1797. [Google Scholar] [CrossRef]
- Szczot, M.; Nickolls, A.R.; Lam, R.M.; Chesler, A.T. The Form and Function of PIEZO2. Annu. Rev. Biochem. 2021, 90, 507–534. [Google Scholar] [CrossRef]
- Shin, H.J.; Lee, W.; Ku, K.B.; Yoon, G.Y.; Moon, H.W.; Kim, C.; Kim, M.H.; Yi, Y.S.; Jun, S.; Kim, B.T.; et al. SARS-CoV-2 aberrantly elevates mitochondrial bioenergetics to induce robust virus propagation. Signal Transduct. Target. Ther. 2024, 9, 125. [Google Scholar] [CrossRef]
- Singer, D.; Camargo, S.M.; Ramadan, T.; Schafer, M.; Mariotta, L.; Herzog, B.; Huggel, K.; Wolfer, D.; Werner, S.; Penninger, J.M.; et al. Defective intestinal amino acid absorption in Ace2 null mice. Am. J. Physiol. Gastrointest. Liver Physiol. 2012, 303, G686–G695. [Google Scholar] [CrossRef]
- Greene, K.S.; Choi, A.; Yang, N.; Chen, M.; Li, R.; Qiu, Y.; Ezzatpour, S.; Rojas, K.S.; Shen, J.; Wilson, K.F.; et al. Glutamine metabolism is essential for coronavirus replication in host cells and in mice. J. Biol. Chem. 2025, 301, 108063. [Google Scholar] [CrossRef]
- Durante, W. Glutamine Deficiency Promotes Immune and Endothelial Cell Dysfunction in COVID-19. Int. J. Mol. Sci. 2023, 24, 7593. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Sriramula, S.; Lazartigues, E. Excessive Glutamate Stimulation Impairs ACE2 Activity Through ADAM17-Mediated Shedding in Cultured Cortical Neurons. Cell. Mol. Neurobiol. 2018, 38, 1235–1243. [Google Scholar] [CrossRef]
- Sonkodi, B. Proton-Mediated PIEZO2 Channelopathy: Linking Oxaliplatin Treatment to Impaired Proprioception and Cognitive Deficits. Cancers 2024, 16, 3898. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, J.W.; Haltom, J.A.; Albrecht, Y.E.S.; Lie, T.; Olali, A.Z.; Widjaja, G.A.; Ranshing, S.S.; Angelin, A.; Murdock, D.; Wallace, D.C. SARS-CoV-2 mitochondrial metabolic and epigenomic reprogramming in COVID-19. Pharmacol. Res. 2024, 204, 107170. [Google Scholar] [CrossRef] [PubMed]
- Malko, P.; Jia, X.; Wood, I.; Jiang, L.H. Piezo1 channel-mediated Ca2+ signaling inhibits lipopolysaccharide-induced activation of the NF-kappaB inflammatory signaling pathway and generation of TNF-alpha and IL-6 in microglial cells. Glia 2023, 71, 848–865. [Google Scholar] [CrossRef]
- Sonkodi, B. Delayed Onset Muscle Soreness and Critical Neural Microdamage-Derived Neuroinflammation. Biomolecules 2022, 12, 1207. [Google Scholar] [CrossRef] [PubMed]
- Sonkodi, B. Only activated macrophages excite muscle spindles with glutamate to bolster locomotion. OSF Prepr. 2025. [Google Scholar] [CrossRef]
- Chi, S.; Cui, Y.; Wang, H.; Jiang, J.; Zhang, T.; Sun, S.; Zhou, Z.; Zhong, Y.; Xiao, B. Astrocytic Piezo1-mediated mechanotransduction determines adult neurogenesis and cognitive functions. Neuron 2022, 110, 2984–2999.e8. [Google Scholar] [CrossRef]
- Pedemonte, M.; Goldstein-Daruech, N.; Velluti, R.A. Temporal correlations between heart rate, medullary units and hippocampal theta rhythm in anesthetized, sleeping and awake guinea pigs. Auton. Neurosci. 2003, 107, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Pedemonte, M.; Velluti, R.A. Sensory processing could be temporally organized by ultradian brain rhythms. Rev. Neurol. 2005, 40, 166–172. [Google Scholar] [CrossRef]
- Sonkodi, B. It Is Time to Consider the Lost Battle of Microdamaged Piezo2 in the Context of E. coli and Early-Onset Colorectal Cancer. Int. J. Mol. Sci. 2025, 26, 7160. [Google Scholar] [CrossRef]
- Tedjasukmana, R.; Budikayanti, A.; Islamiyah, W.R.; Witjaksono, A.; Hakim, M. Sleep disturbance in post COVID-19 conditions: Prevalence and quality of life. Front. Neurol. 2022, 13, 1095606. [Google Scholar] [CrossRef]
- Clemente, L.; La Rocca, M.; Quaranta, N.; Iannuzzi, L.; Vecchio, E.; Brunetti, A.; Gentile, E.; Dibattista, M.; Lobasso, S.; Bevilacqua, V.; et al. Prefrontal dysfunction in post-COVID-19 hyposmia: An EEG/fNIRS study. Front. Hum. Neurosci. 2023, 17, 1240831. [Google Scholar] [CrossRef]
- Zhang, Q.; Ma, H.; Huo, L.; Wang, S.; Yang, Q.; Ye, Z.; Cao, J.; Wu, S.; Ma, C.; Shang, C. Neural mechanism of trigeminal nerve stimulation recovering defensive arousal responses in traumatic brain injury. Theranostics 2025, 15, 2315–2337. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sonkodi, B. Underlying Piezo2 Channelopathy-Induced Neural Switch of COVID-19 Infection. Cells 2025, 14, 1182. https://doi.org/10.3390/cells14151182
Sonkodi B. Underlying Piezo2 Channelopathy-Induced Neural Switch of COVID-19 Infection. Cells. 2025; 14(15):1182. https://doi.org/10.3390/cells14151182
Chicago/Turabian StyleSonkodi, Balázs. 2025. "Underlying Piezo2 Channelopathy-Induced Neural Switch of COVID-19 Infection" Cells 14, no. 15: 1182. https://doi.org/10.3390/cells14151182
APA StyleSonkodi, B. (2025). Underlying Piezo2 Channelopathy-Induced Neural Switch of COVID-19 Infection. Cells, 14(15), 1182. https://doi.org/10.3390/cells14151182





