The Effect of Chemical Surface Modification on the Repair Bond Strength of Resin Composite: An In Vitro Study
Abstract
1. Introduction
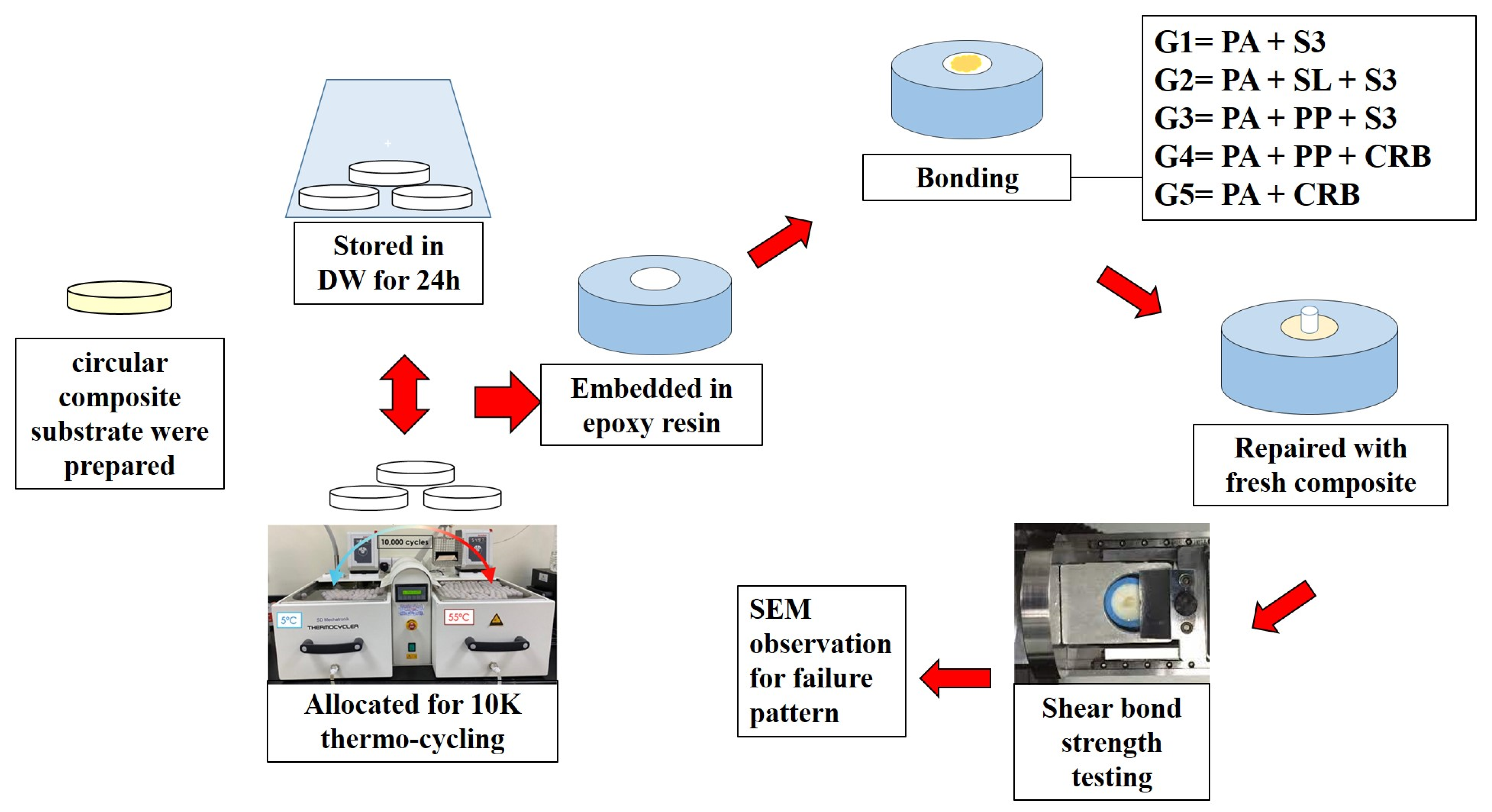
2. Materials and Methods
2.1. Study Design
2.2. Preparation of Resin Composite Substrate
2.3. Sample Size Calculation
2.4. Aging of Resin Composite Disk
2.5. Embedding of Resin Composite Disks
2.6. Bonding Protocols
2.7. Repair of the Substrate
2.8. Shear Bond Strength Testing
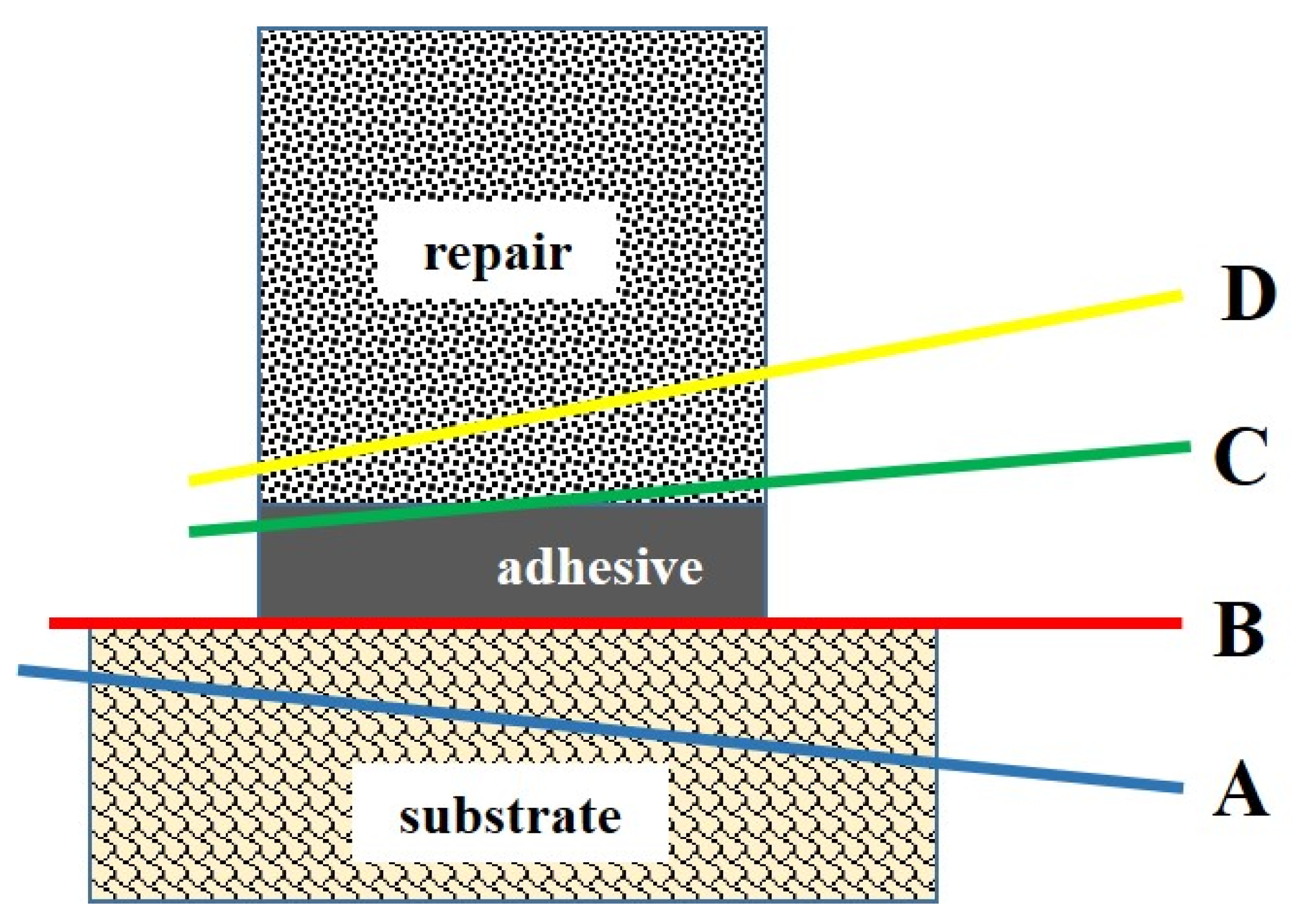
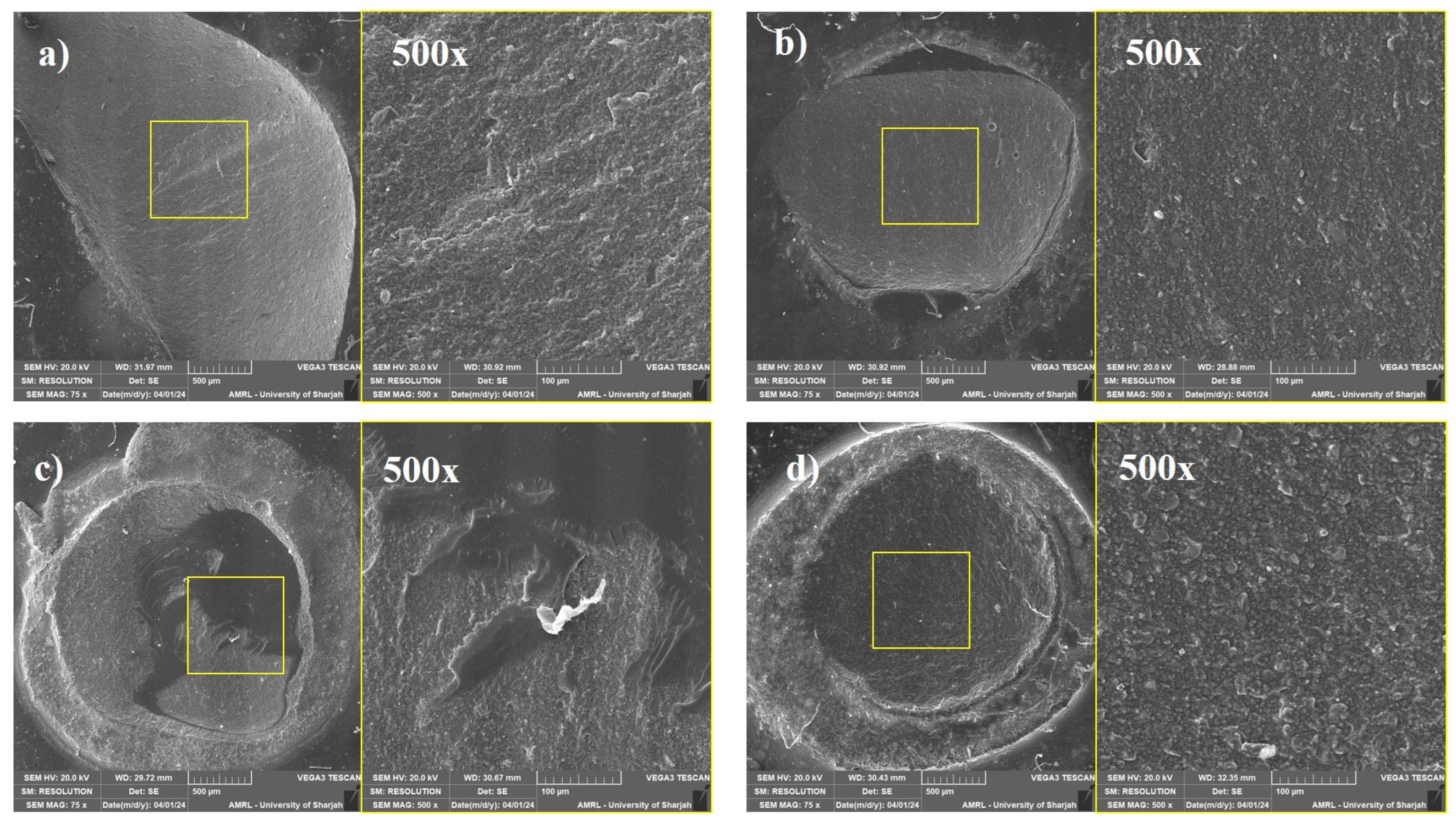
2.9. Failure Mode Analysis
2.10. Data Analysis
3. Results
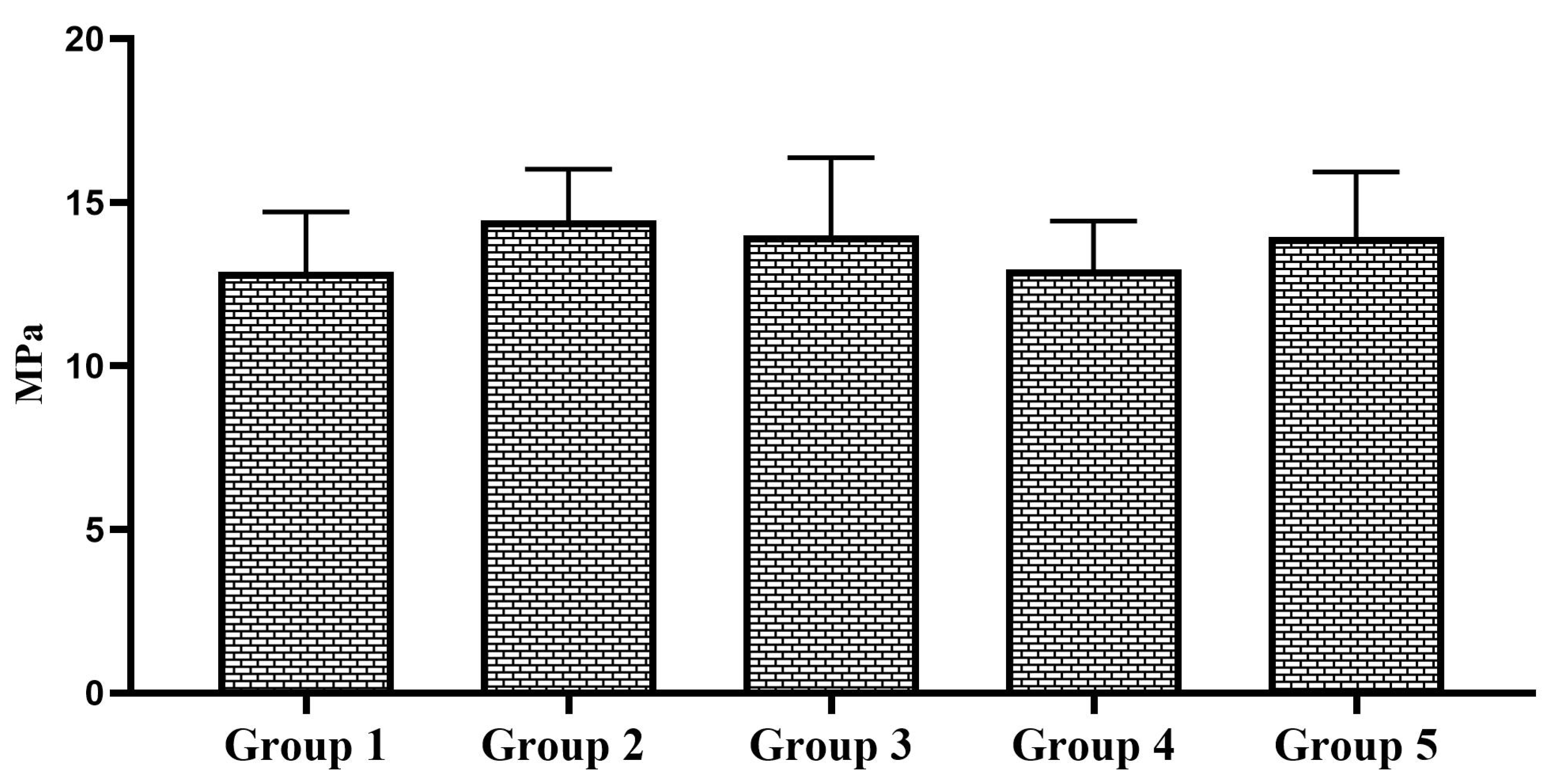
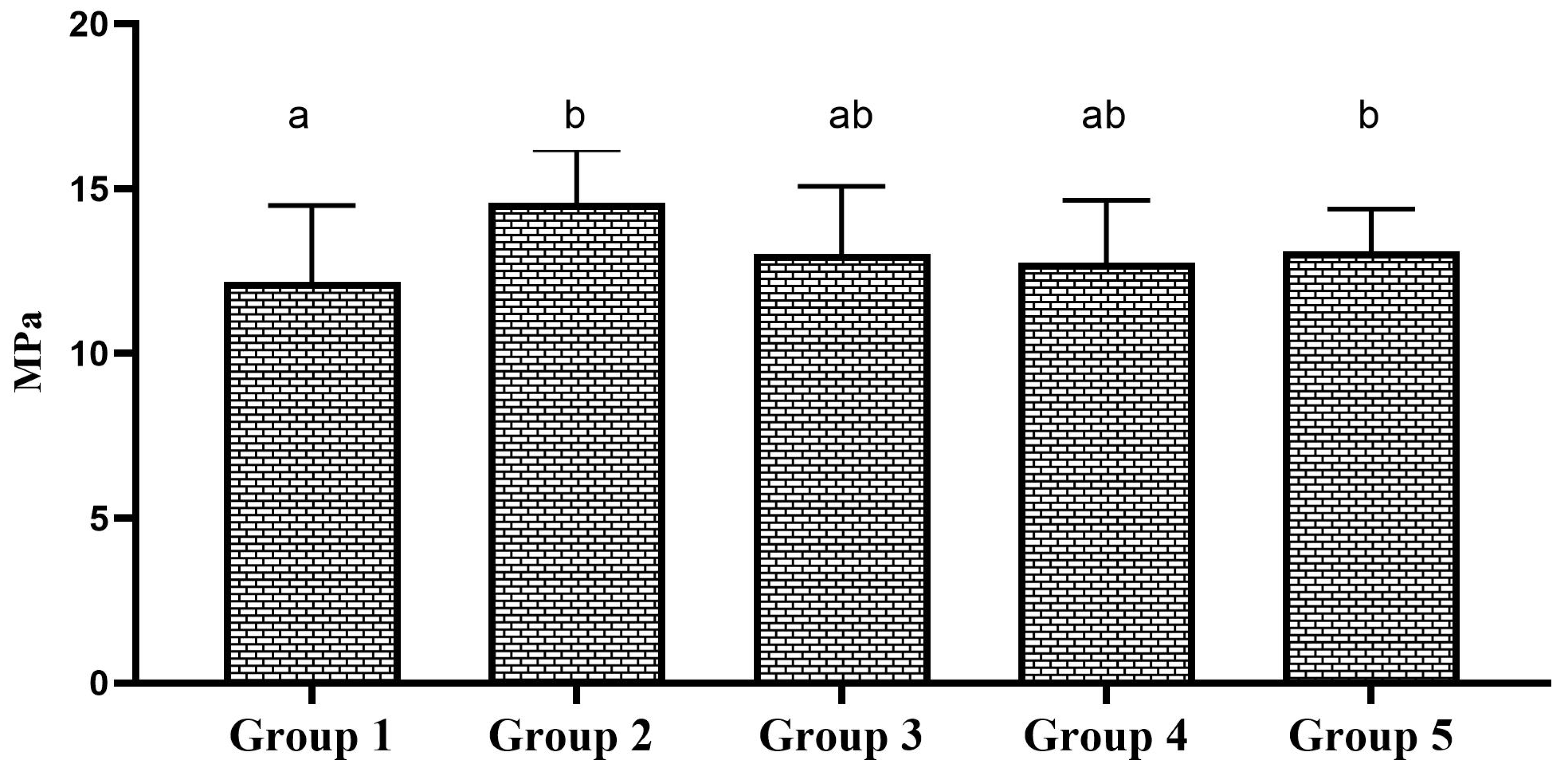
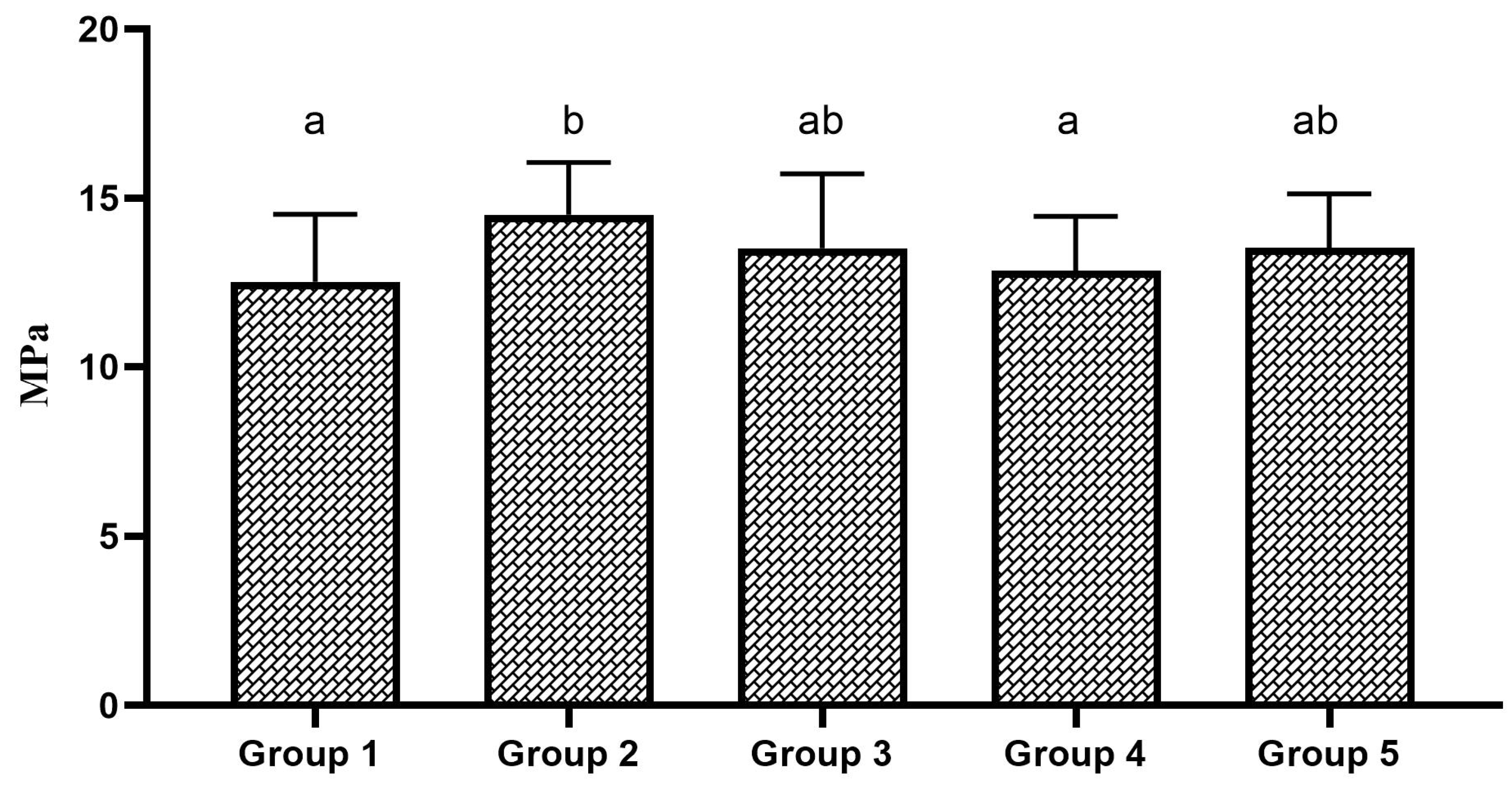
3.1. Shear Bond Strength
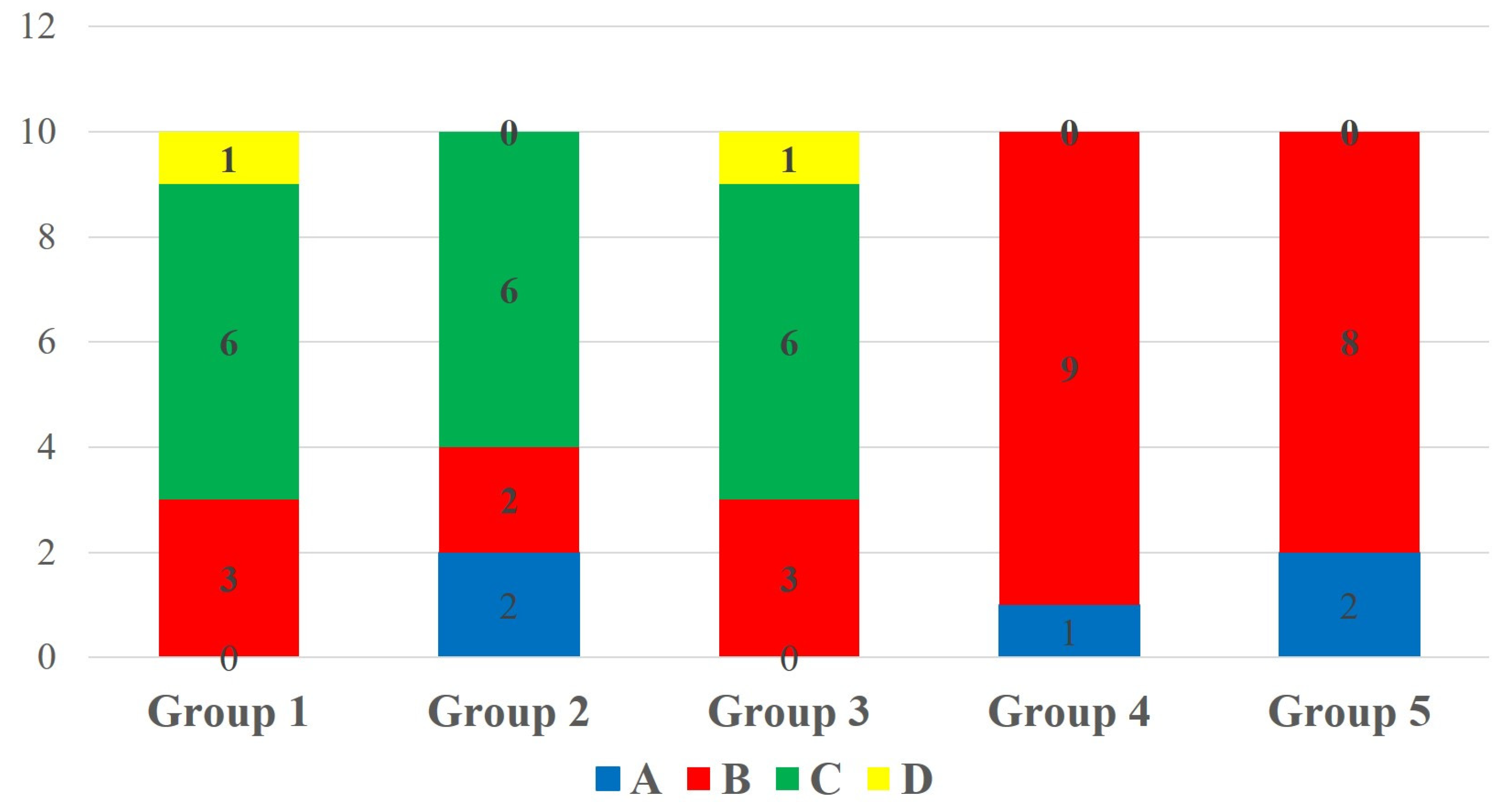
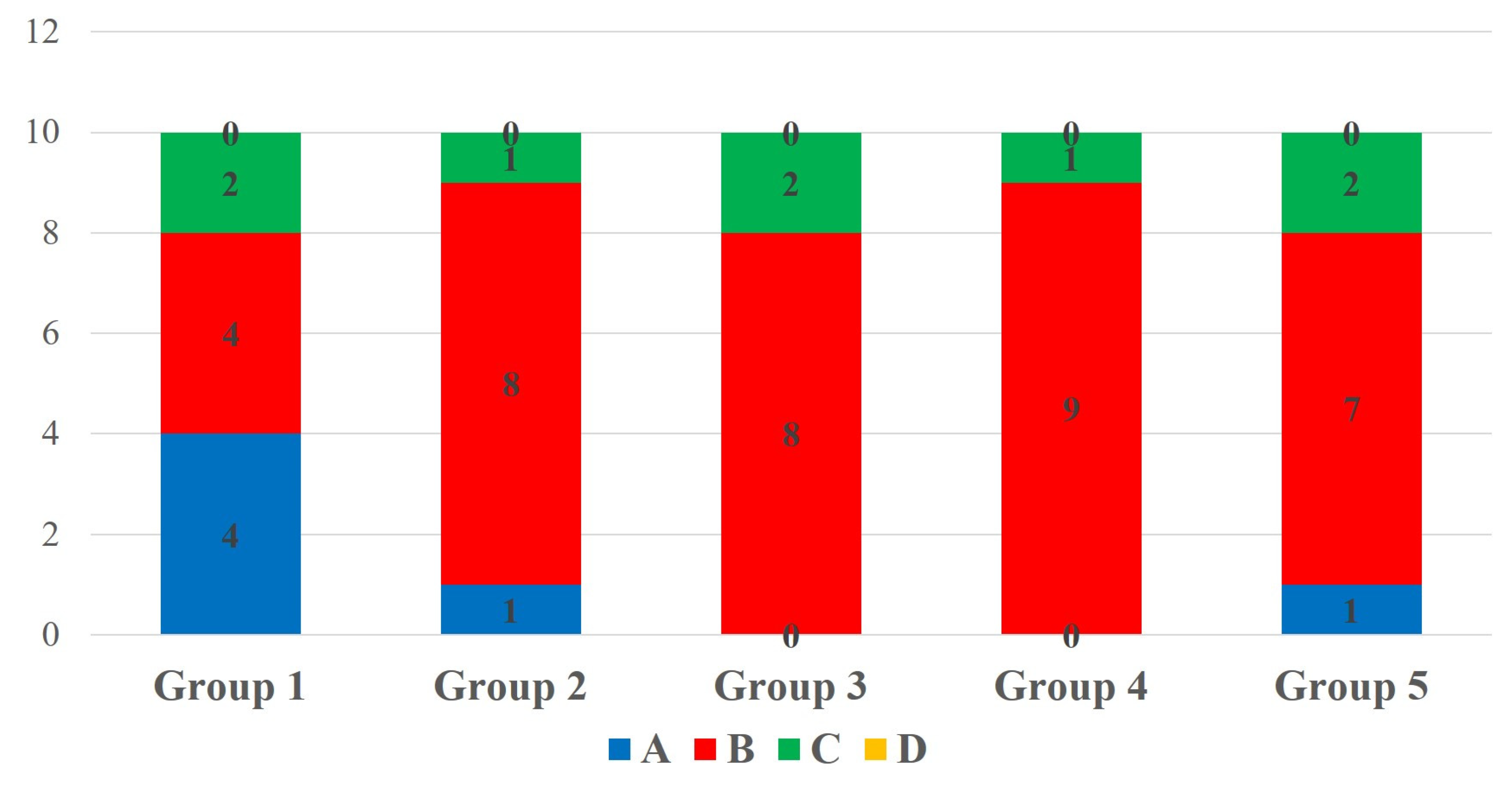
3.2. Failure Pattern
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Profeta, A.C. Preparation and Properties of Calcium-Silicate Filled Resins for Dental Restoration. Part II: Micro-Mechanical Behaviour to Primed Mineral-Depleted Dentine. Acta Odontol. Scand. 2014, 72, 607–617. [Google Scholar] [CrossRef]
- Islam, M.S.; Huda, N.; Mahendran, S.; Aryal, A.C.S.; Nassar, M.; Rahman, M.M. The Blending Effect of Single-Shade Composite with Different Shades of Conventional Resin Composites-An In Vitro Study. Eur. J. Dent. 2022, 17, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Cadenaro, M.; Josic, U.; Maravić, T.; Mazzitelli, C.; Marchesi, G.; Mancuso, E.; Breschi, L.; Mazzoni, A. Progress in Dental Adhesive Materials. J. Dent. Res. 2023, 102, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P.; Van Landuyt, K.; Lambrechts, P.; Vanherle, G. Buonocore Memorial Lecture. Adhesion to Enamel and Dentin: Current Status and Future Challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar] [PubMed]
- Islam, S.; Hiraishi, N.; Nassar, M.; Yiu, C.; Otsuki, M.; Tagami, J. Effect of Natural Cross-Linkers Incorporation in a Self-Etching Primer on Dentine Bond Strength. J. Dent. 2012, 40, 1052–1059. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Hiraishi, N.; Nassar, M.; Yiu, C.; Otsuki, M.; Tagami, J. Effect of Hesperidin Incorporation into a Self-Etching Primer on Durability of Dentin Bond. Dent. Mater. 2014, 30, 1205–1212. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Nassar, M.; Elsayed, M.A.; Jameel, D.B.; Ahmad, T.T.; Rahman, M.M. In Vitro Optical and Physical Stability of Resin Composite Materials with Different Filler Characteristics. Polymers 2023, 15, 2121. [Google Scholar] [CrossRef]
- Aziz, I.M.; Locke, M. Success and Survival of Composite Resin Restorations for the Management of Localized Anterior Tooth Wear: A Systematic Review and Meta-Analysis. Eur. J. Prosthodont. Restor. Dent. 2024, 32, 403–414. [Google Scholar] [CrossRef]
- Hatipoğlu, Ö.; Martins, J.F.B.; Karobari, M.I.; Taha, N.; Aldhelai, T.A.; Ayyad, D.M.; Madfa, A.A.; Martin-Biedma, B.; Fernández-Grisales, R.; Omarova, B.A.; et al. Clinical Decision-Making of Repair vs. Replacement of Defective Direct Dental Restorations: A Multinational Cross-Sectional Study with Meta-Analysis. J. Esthet. Restor. Dent. 2024. [Google Scholar] [CrossRef] [PubMed]
- Khanna, R.; Han, J.; Liang, E.; Lee, C.Y.; Manakil, J. The Current Attitudes and Practices of Dentists in Australia towards Composite Repair: A Cross-Sectional Survey Study. Aust. Dent. J. 2024. [Google Scholar] [CrossRef] [PubMed]
- Nassar, M.; Al-Fakhri, O.; Shabbir, N.; Islam, M.S.; Gordan, V.V.; Lynch, C.D.; Wilson, N.H.; Blum, I.R. Teaching of the Repair of Defective Composite Restorations in Middle Eastern and North African Dental Schools. J. Dent. 2021, 112, 103753. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Aryal, A.C.S.; El Bahra, S.; Abuhajjeh, A.J.; Al Mofleh, A.M.; Padmanabhan, V.; Rahman, M.M. The Effect of Mechanical Alteration on Repair Bond Strength of S-PRG-Filler-Based Resin Composite Materials. Polymers 2024, 16, 1488. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Aal-Fatlah, A.A.; Alkhan, N.S.; Aryal Ac, S.; Sadr, A.; Rehman, M.M. The Effect of Different Finishing Polishing Protocols on Stain Absorption and Color Stability of Resin Composite Restorations. Am. J. Dent. 2022, 35, 141–145. [Google Scholar] [PubMed]
- Perdigão, J. Current Perspectives on Dental Adhesion: (1) Dentin Adhesion—Not There Yet. Jpn. Dent. Sci. Rev. 2020, 56, 190–207. [Google Scholar] [CrossRef] [PubMed]
- Neto, H.N.M.; Leite, J.V.C.; de Medeiros, J.M.; e Silva Campos, D.; de Araújo Ferreira Muniz, I.; De Andrade, A.K.M.; Duarte, R.M.; De Souza, G.M.; Lima, R.B.W. Scoping Review: Effect of Surface Treatments on Bond Strength of Resin Composite Repair. J. Dent. 2024, 140, 104737. [Google Scholar] [CrossRef]
- Guo, X.; Yu, Y.; Gao, S.; Zhang, Z.; Zhao, H. Biodegradation of Dental Resin-Based Composite-A Potential Factor Affecting the Bonding Effect: A Narrative Review. Biomedicines 2022, 10, 2313. [Google Scholar] [CrossRef] [PubMed]
- Hosaka, K.; Tichy, A.; Araoka, D.; Wurihan, W.; Shibata, Y.; Ikeda, M.; Klein, C.A.; Tagami, J.; Nakajima, M. Eight-Year Microtensile Bond Strength to Dentin and Interfacial Nanomechanical Properties of a One-Step Adhesive. J. Adhes. Dent. 2021, 23, 461–467. [Google Scholar] [CrossRef]
- Iftikhar, N.; Devashish; Srivastava, B.; Gupta, N.; Ghambir, N.; Rashi-Singh, A. Comparative Evaluation of Mechanical Properties of Four Different Restorative Materials: An In Vitro Study. Int. J. Clin. Pediatr. Dent. 2019, 12, 47–49. [Google Scholar] [CrossRef]
- Hofsteenge, J.W.; Carvalho, M.A.; Botenga, E.L.F.; Cune, M.S.; Özcan, M.; Magne, P.; Gresnigt, M.M.M. Effect of Preparation Design on Fracture Strength of Compromised Molars Restored with Direct Composite Resin Restorations: An In Vitro and Finite Element Analysis Study. J. Prosthet. Dent. 2024, 131, 1150–1158. [Google Scholar] [CrossRef]
- Dall’Oca, S.; Papacchini, F.; Goracci, C.; Cury, A.H.; Suh, B.I.; Tay, F.R.; Polimeni, A.; Ferrari, M. Effect of Oxygen Inhibition on Composite Repair Strength over Time. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 81, 493–498. [Google Scholar] [CrossRef]
- Ferracane, J.L. Hygroscopic and Hydrolytic Effects in Dental Polymer Networks. Dent. Mater. 2006, 22, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Kuno, Y.; Hosaka, K.; Nakajima, M.; Ikeda, M.; Klein Junior, C.A.; Foxton, R.M.; Tagami, J. Incorporation of a Hydrophilic Amide Monomer into a One-Step Self-Etch Adhesive to Increase Dentin Bond Strength: Effect of Application Time. Dent. Mater. J. 2019, 38, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.H.; De Munck, J.; Van Landuyt, K.; Peumans, M.; Yoshihara, K.; Van Meerbeek, B. Do Universal Adhesives Benefit from an Extra Bonding Layer? J. Adhes. Dent. 2019, 21, 117–132. [Google Scholar] [CrossRef] [PubMed]
- Tichy, A.; Hosaka, K.; Abdou, A.; Nakajima, M.; Tagami, J. Degree of Conversion Contributes to Dentin Bonding Durability of Contemporary Universal Adhesives. Oper. Dent. 2020, 45, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Ramos, R.Q.; Mercelis, B.; Ahmed, M.H.; Peumans, M.; Lopes, G.C.; Van Meerbeek, B. Bonding of Composite Cements Containing 10-MDP to Zirconia Ceramics Without Dedicated Ceramic Primer. J. Adhes. Dent. 2024, 26, 135–145. [Google Scholar] [CrossRef] [PubMed]
- Martos, R.; Szalóki, M.; Gáll, J.; Csík, A.; Hegedűs, C. Comparative Analysis of Bond Strength Durability of 10-Methacryloyloxydecyl Dihydrogen Phosphate-Containing Adhesives on a Low-Viscosity Bulk-Fill Composite Surface. J. Adhes. Dent. 2022, 24, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Samran, A.; Al-Ammari, A.; El Bahra, S.; Halboub, E.; Wille, S.; Kern, M. Bond Strength Durability of Self-Adhesive Resin Cements to Zirconia Ceramic: An In Vitro Study. J. Prosthet. Dent. 2019, 121, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Staxrud, F.; Dahl, J.E. Silanising Agents Promote Resin-Composite Repair. Int. Dent. J. 2015, 65, 311–315. [Google Scholar] [CrossRef]
- Mendes, L.T.; Loomans, B.A.C.; Opdam, N.J.M.; da Silva, C.L.; Casagrande, L.; Lenzi, T.L. Silane Coupling Agents Are Beneficial for Resin Composite Repair: A Systematic Review and Meta-Analysis of In Vitro Studies. J. Adhes. Dent. 2020, 22, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Lung, C.Y.K.; Matinlinna, J.P. Aspects of Silane Coupling Agents and Surface Conditioning in Dentistry: An Overview. Dent. Mater. 2012, 28, 467–477. [Google Scholar] [CrossRef] [PubMed]
- Dimitriadi, M.; Panagiotopoulou, A.; Pelecanou, M.; Yannakopoulou, K.; Eliades, G. Stability and Reactivity of γ-ΜPTMS Silane in Some Commercial Primer and Adhesive Formulations. Dent. Mater. 2018, 34, 1089–1101. [Google Scholar] [CrossRef]
- Yao, C.; Yu, J.; Wang, Y.; Tang, C.; Huang, C. Acidic PH Weakens the Bonding Effectiveness of Silane Contained in Universal Adhesives. Dent. Mater. 2018, 34, 809–818. [Google Scholar] [CrossRef]
- Çakir, N.N.; Demirbuga, S.; Balkaya, H.; Karadaş, M. Bonding Performance of Universal Adhesives on Composite Repairs, with or Without Silane Application. J. Conserv. Dent. 2018, 21, 263–268. [Google Scholar] [CrossRef] [PubMed]
- da Silva, C.L.; Scherer, M.M.; Mendes, L.T.; Casagrande, L.; Leitune, V.C.B.; Lenzi, T.L. Does Use of Silane-Containing Universal Adhesive Eliminate the Need for Silane Application in Direct Composite Repair? Braz. Oral Res. 2020, 34, e045. [Google Scholar] [CrossRef] [PubMed]
- Ugurlu, M.; Al-Haj Husain, N.; Özcan, M. Immediate and Late Repair of Microhybrid Resin Composites: Effect of Silane Coupling Agent, Universal Adhesives and Photo Polymerization. Eur. J. Prosthodont. Restor. Dent. 2023, 31, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Michelotti, G.; Niedzwiecki, M.; Bidjan, D.; Dieckmann, P.; Deari, S.; Attin, T.; Tauböck, T.T. Silane Effect of Universal Adhesive on the Composite-Composite Repair Bond Strength After Different Surface Pretreatments. Polymers 2020, 12, 950. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Fu, J.; Liao, S.; Su, N.; Wang, H.; Liao, Y. Effects of Different Surface Conditioning Agents on the Bond Strength of Resin-Opaque Porcelain Composite. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 2014, 31, 361–364. [Google Scholar]
- Matinlinna, J.P.; Lung, C.Y.K.; Tsoi, J.K.H. Silane Adhesion Mechanism in Dental Applications and Surface Treatments: A Review. Dent. Mater. 2018, 34, 13–28. [Google Scholar] [CrossRef]
- de Oliveira Lino, L.F.; Machado, C.M.; de Paula, V.G.; Vidotti, H.A.; Coelho, P.G.; Benalcázar Jalkh, E.B.; Pegoraro, T.A.; Bonfante, E.A. Effect of Aging and Testing Method on Bond Strength of CAD/CAM Fiber-Reinforced Composite to Dentin. Dent. Mater. 2018, 34, 1690–1701. [Google Scholar] [CrossRef] [PubMed]
- Hagino, R.; Mine, A.; Kawaguchi-Uemura, A.; Tajiri-Yamada, Y.; Yumitate, M.; Ban, S.; Miura, J.; Matsumoto, M.; Yatani, H.; Nakatani, H. Adhesion Procedures for CAD/CAM Indirect Resin Composite Block: A New Resin Primer Versus a Conventional Silanizing Agent. J. Prosthodont. Res. 2020, 64, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Hosaka, K.; Tichy, A.; Ikeda, M.; Nakagawa, K.; Sadr, A.; Tagami, J.; Takahashi, M.; Sato, K.; Nishitani, Y.; Klein-Junior, C.A.; et al. Ultra-High-Speed Videography of Resin-Dentin Interface Failure Dynamics Under Tensile Load. Dent. Mater. 2019, 35, e153–e161. [Google Scholar] [CrossRef] [PubMed]
- Elsayed, M.A.; Islam, M.S.; Elbeltagy, K.; Nassar, M. Effect of Different Chelating Agents on the Shear Bond Strength of Calcium Silicate-Based Cements to Coronal Dentin. Aust. Endod. J. 2023, 49 (Suppl S1), 426–432. [Google Scholar] [CrossRef] [PubMed]
- Nassar, M.; Hiraishi, N.; Islam, M.S.; Romero, M.J.; Otsuki, M.; Tagami, J. Effect of Phytic Acid as an Endodontic Chelator on Resin Adhesion to Sodium Hypochlorite-Treated Dentin. Restor. Dent. Endod. 2020, 45, e44. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Islam, M.S.; El Bahra, S.; Aryal A C, S.; Padmanabhan, V.; Al Tawil, A.; Saleh, I.; Rahman, M.M.; Guha, U. The Effect of Chemical Surface Modification on the Repair Bond Strength of Resin Composite: An In Vitro Study. Polymers 2025, 17, 513. https://doi.org/10.3390/polym17040513
Islam MS, El Bahra S, Aryal A C S, Padmanabhan V, Al Tawil A, Saleh I, Rahman MM, Guha U. The Effect of Chemical Surface Modification on the Repair Bond Strength of Resin Composite: An In Vitro Study. Polymers. 2025; 17(4):513. https://doi.org/10.3390/polym17040513
Chicago/Turabian StyleIslam, Md Sofiqul, Shadi El Bahra, Smriti Aryal A C, Vivek Padmanabhan, Abdulaziz Al Tawil, Ihab Saleh, Muhammed Mustahsen Rahman, and Upoma Guha. 2025. "The Effect of Chemical Surface Modification on the Repair Bond Strength of Resin Composite: An In Vitro Study" Polymers 17, no. 4: 513. https://doi.org/10.3390/polym17040513
APA StyleIslam, M. S., El Bahra, S., Aryal A C, S., Padmanabhan, V., Al Tawil, A., Saleh, I., Rahman, M. M., & Guha, U. (2025). The Effect of Chemical Surface Modification on the Repair Bond Strength of Resin Composite: An In Vitro Study. Polymers, 17(4), 513. https://doi.org/10.3390/polym17040513






