Rheology of Dental Photopolymers for SLA/DLP/MSLA 3D Printing
Abstract
1. Introduction
- (i)
- Technology-specific printability windows that define the viscosity ranges, shear-thinning requirements, and thixotropic behavior for SLA, DLP, and mSLA;
- (ii)
- Formulation strategies that shift η(γ̇,T) while preserving optical and mechanical performance; and
- (iii)
- Opto-rheological coupling (e.g., penetration depth Dp, scattering behavior) and its implications for processing. By bridging the fundamentals of material science with dental applications, this review provides a comprehensive framework to guide resin formulation, printer operation, and clinical translation.
2. Printability Window
Technology-Specific Windows
3. Methodology of Measurement
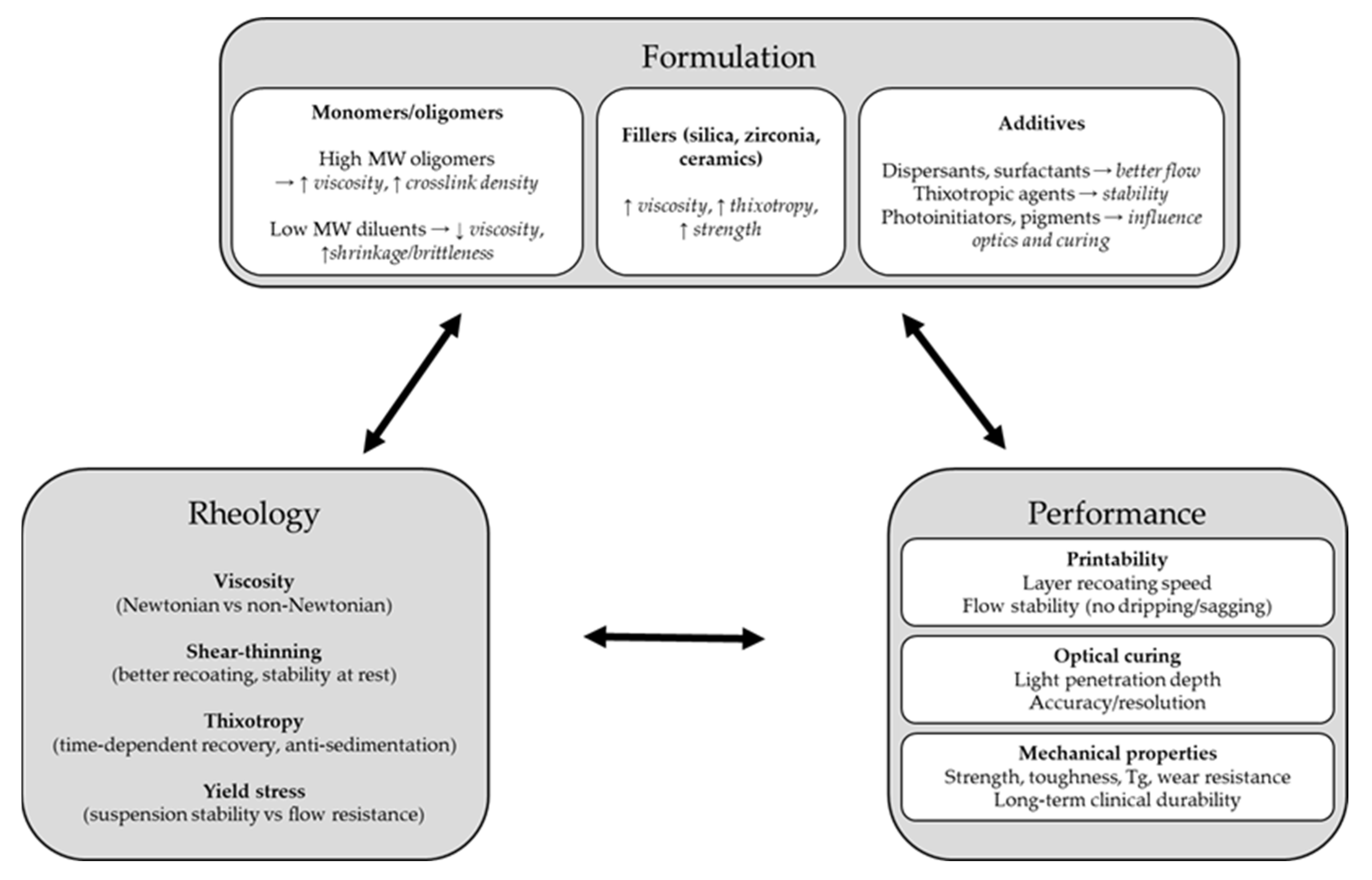
4. Formulation–Rheology
5. Rheology–Optics
Quantitative Coupling Between Particle Size, Scattering, and Cure Depth
6. Rheology–Mechanical Properties
6.1. Monomer Functionality and Crosslink Density
6.2. Filler Content
6.3. Degree of Cure and Network Formation
7. Discussion
8. Conclusions
- Design for viscosity: η (25–30 °C, γ̇ = 10–50 s−1) ≈ 0.1–1.5 Pa·s for DLP/MSLA, and ≤3 Pa·s for SLA with a recoater, to ensure uniform gap refill and controlled peel forces.
- Standardize reporting: Always report η at defined γ̇ and T, thixotropy recovery, τy, and Ec/Dp as a minimal framework for method-to-method comparison.
- Optical tuning: Adjust the penetration depth (Dp) with absorbers to ≈1.1–1.5× the target layer height, and re-establish Ec after any formulation change.
- Filler use: Employ sub-µm, index-matched fillers with validated dispersion to increase stiffness while limiting viscosity rise and scattering.
- Temperature management: Maintain the resin temperature between 25 and 30 °C to widen the printability window without altering the formulation.
- Formulation balance: Co-optimize the oligomer–diluent ratio to preserve mechanical performance (modulus, Tg) while maintaining flow and avoiding excessive dilution that causes brittleness.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Jeong, M.; Radomski, K.; Lopez, D.; Liu, J.T.; Lee, J.D.; Lee, S.J. Materials and Applications of 3D Printing Technology in Dentistry: An Overview. Dent. J. 2023, 12, 1. [Google Scholar] [CrossRef]
- Iftekar, S.F.; Aabid, A.; Amir, A.; Baig, M. Advancements and Limitations in 3D Printing Materials and Technologies: A Critical Review. Polymers 2023, 15, 2519. [Google Scholar] [CrossRef]
- Singh, R.; Gupta, A.; Tripathi, O.; Srivastava, S.; Singh, B.; Awasthi, A.; Rajput, S.K.; Sonia, P.; Singhal, P.; Saxena, K.K. Powder Bed Fusion Process in Additive Manufacturing: An Overview. Mater. Today Proc. 2020, 26, 3058–3070. [Google Scholar] [CrossRef]
- Fiedor, P.; Ortyl, J. A New Approach to Micromachining: High-Precision and Innovative Additive Manufacturing Solutions Based on Photopolymerization Technology. Materials 2020, 13, 2951. [Google Scholar] [CrossRef] [PubMed]
- Islam, A.; Rahman, M.Z. Recent Advances in Additive Manufacturing Techniques: An In-Depth Review. In Comprehensive Materials Processing, 2nd ed.; Hashmi, S., Ed.; Elsevier: Oxford, UK, 2024; pp. 352–378. [Google Scholar] [CrossRef]
- Mukhtarkhanov, M.; Perveen, A.; Talamona, D. Application of Stereolithography Based 3D Printing Technology in Investment Casting. Micromachines 2020, 11, 946. [Google Scholar] [CrossRef] [PubMed]
- Calafel, M.I.; Criado-Gonzalez, M.; Aguirresarobe, R.; Fernández, M.; Mijangos, C. From rheological concepts to additive manufacturing assessment of hydrogel-based materials for advanced bioprinting applications. Mater. Adv. 2025, 6, 4566–4597. [Google Scholar] [CrossRef]
- Bercea, M. Rheology as a Tool for Fine-Tuning the Properties of Printable Bioinspired Gels. Molecules 2023, 28, 2766. [Google Scholar] [CrossRef]
- Komissarenko, D.A.; Sokolov, P.S.; Evstigneeva, A.D.; Shmeleva, I.A.; Dosovitsky, A.E. Rheological and Curing Behavior of Acrylate-Based Suspensions for the DLP 3D Printing of Complex Zirconia Parts. Materials 2018, 11, 2350. [Google Scholar] [CrossRef]
- Paxton, N.; Smolan, W.; Böck, T.; Melchels, F.; Groll, J.; Jungst, T. Proposal to Assess Printability of Bioinks for Extrusion-Based Bioprinting and Evaluation of Rheological Properties Governing Bioprintability. Biofabrication 2017, 9, 044107. [Google Scholar] [CrossRef]
- Blaeser, A.; Duarte Campos, D.F.; Puster, U.; Richtering, W.; Stevens, M.M.; Fischer, H. Controlling Shear Stress in 3D Bioprinting Is a Key Factor to Balance Printing Resolution and Stem Cell Integrity. Adv. Healthc. Mater. 2016, 5, 326–333. [Google Scholar] [CrossRef]
- Zhao, Y.; Li, Y.; Mao, S.; Sun, W.; Yao, R. The Influence of Printing Parameters on Cell Survival Rate and Printability in Microextrusion-Based 3D Cell Printing Technology. Biofabrication 2015, 7, 045002. [Google Scholar] [CrossRef]
- Ning, L.; Guillemot, A.; Zhao, J.; Kipouros, G.; Chen, X. Influence of Flow Behavior of Alginate-Cell Suspensions on Cell Viability and Proliferation. Tissue Eng. Part C 2016, 22, 652–662. [Google Scholar] [CrossRef] [PubMed]
- Kesti, M.; Fisch, P.; Pensalfini, M.; Mazza, E.; Zenobi-Wong, M. Guidelines for Standardization of Bioprinting: A Systematic Study of Process Parameters and Their Effect on Bioprinted Structures. BioNanoMaterials 2016, 17, 193–204. [Google Scholar] [CrossRef]
- Li, M.; Tian, X.; Schreyer, D.J.; Chen, X. Effect of Needle Geometry on Flow Rate and Cell Damage in the Dispensing-Based Biofabrication Process. Biotechnol. Prog. 2011, 27, 1777–1784. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, J.; Duan, Y.; Liu, N.; Jiang, J.; Ma, R.; Xi, H.; Li, X. Rheology and Curability Characterization of Photosensitive Slurries for 3D Printing of Si₃N₄ Ceramics. Appl. Sci. 2020, 10, 6438. [Google Scholar] [CrossRef]
- Tumbleston, J.R.; Shirvanyants, D.; Ermoshkin, N.; Janusziewicz, R.; Johnson, A.R.; Kelly, D.; Chen, K.; Pinschmidt, R.; Rolland, J.P.; Ermoshkin, A.; et al. Additive Manufacturing. Continuous Liquid Interface Production of 3D Objects. Science 2015, 347, 1349–1352. [Google Scholar] [CrossRef]
- Calignano, F.; Manfredi, D.; Ambrosio, E.P.; Biamino, S.; Lombardi, M.; Atzeni, E.; Salmi, A.; Minetola, P.; Iuliano, L.; Fino, P. Overview on Additive Manufacturing Technologies. Proc. IEEE 2017, 105, 593–612. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef]
- Muth, J.T.; Vogt, D.M.; Truby, R.L.; Menguc, Y.; Kolesky, D.B.; Wood, R.J.; Lewis, J.A. Embedded 3D Printing of Strain Sensors within Highly Stretchable Elastomers. Adv. Mater. 2014, 26, 6307–6312. [Google Scholar] [CrossRef]
- Weng, Z.; Huang, X.; Peng, S.; Zhang, J.; Yan, Q.; Zhang, Y.; Xu, S.; Li, L.; Lin, Z. 3D Printing of Ultra-High Viscosity Resin by a Linear Scan-Based Vat Photopolymerization System. Nat. Commun. 2023, 14, 4303. [Google Scholar] [CrossRef]
- Garcia, G.E.S.; de Sousa Junior, R.R.; Gouveia, J.R.; dos Santos, D.J. Graphene Oxide-Based Nanocomposites for Stereolithography (SLA) 3D Printing: Comprehensive Mechanical Characterization under Combined Loading Modes. Polymers 2024, 16, 1261. [Google Scholar] [CrossRef]
- Cramer, C.L.; Hmeidat, N.S.; Mitchell, D.J.; Layani, M.; Liao, H.; Tarat, A.; Drzal, L.T.; Bandyopadhyay, A. Rheology Improvement for Silicon Nitride and Resin Slurries for Vat Photopolymerization Printing and Sintering. npj Adv. Manuf. 2025, 2, 36. [Google Scholar] [CrossRef]
- Herrada-Manchón, H.; Fernández, M.A.; Aguilar, E. Essential Guide to Hydrogel Rheology in Extrusion 3D Printing: How to Measure It and Why It Matters? Gels 2023, 9, 517. [Google Scholar] [CrossRef] [PubMed]
- Cooke, M.E.; Rosenzweig, D.H. The Rheology of Direct and Suspended Extrusion Bioprinting. APL Bioeng. 2021, 5, 011502. [Google Scholar] [CrossRef] [PubMed]
- Panda, B.; Noor Mohamed, N.A.; Paul, S.C.; Bhagath Singh, G.; Tan, M.J.; Šavija, B. The Effect of Material Fresh Properties and Process Parameters on Buildability and Interlayer Adhesion of 3D Printed Concrete. Materials 2019, 12, 2149. [Google Scholar] [CrossRef] [PubMed]
- Barrulas, R.V.; Corvo, M.C. Rheology in Product Development: An Insight into 3D Printing of Hydrogels and Aerogels. Gels 2023, 9, 986. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, G.J.; Hong, S.; An, J.H.; Kim, B.J.; Ha, C.W. Sequential Process Optimization for a Digital Light Processing System to Minimize Trial and Error. Sci. Rep. 2022, 12, 13553. [Google Scholar] [CrossRef]
- Pagac, M.; Hajnys, J.; Ma, Q.P.; Jancar, L.; Jansa, J.; Stefek, P.; Mesicek, J. A Review of Vat Photopolymerization Technology: Materials, Applications, Challenges, and Future Trends of 3D Printing. Polymers 2021, 13, 598. [Google Scholar] [CrossRef]
- Lee, J.H.; Um, C.M.; Lee, I.B. Rheological Properties of Resin Composites According to Variations in Monomer and Filler Composition. Dent. Mater. 2006, 22, 515–526. [Google Scholar] [CrossRef]
- Steyrer, B.; Liska, R.; Stampfl, J. Hot Lithography: Concepts, Materials, and Applications. Adv. Mater. Technol. 2018, 3, 1700327. [Google Scholar] [CrossRef]
- Jacobs, P.F. Rapid Prototyping & Manufacturing: Fundamentals of Stereolithography; SME: Dearborn, MI, USA, 1992. [Google Scholar]
- Kolibaba, T.J.; Killgore, J.P.; Caplins, B.W.; Higgins, C.I.; Arp, U.; Miller, C.C.; Poster, D.L.; Zong, Y.; Broce, S.; Wang, T.; et al. Results of an interlaboratory study on the working curve in vat photopolymerization. Addit. Manuf. 2024, 84, 104082. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Miyamoto, N.; Liu, H.; Iwaki, M.; Komagamine, Y.; Minakuchi, S. Effect of Different Filler Contents and Printing Directions on the Mechanical Properties for Photopolymer Resins. Int. J. Mol. Sci. 2022, 23, 2296. [Google Scholar] [CrossRef]
- Oivanen, M.; Keulemans, F.; Garoushi, S.; Vallittu, P.K.; Lassila, L. The effect of refractive index of fillers and polymer matrix on translucency and color matching of dental resin composite. Biomater. Investig. Dent. 2021, 8, 48–53. [Google Scholar] [CrossRef]
- Zakeri, S.; Vippola, M.; Levänen, E. A Comprehensive Review of the Photopolymerization of Ceramic Resins Used in Stereolithography. Addit. Manuf. 2020, 35, 101177. [Google Scholar] [CrossRef]
- ApplyLabWork. Design Concept Series: MSLA Modeling Clear, for LED/LCD Printers. ApplyLabWork (Blog/Product Page). Available online: https://applylabwork.com/design-concept-series-msla-modeling-clear-for-led-lcd-printers/ (accessed on 28 August 2025).
- ApplyLabWork. ApplyLabWork|3D Printing Resins for SLA/DLP/LED/LCD Printer Compatible. Available online: https://applylabwork.com/ (accessed on 28 August 2025).
- Afridi, A.; Al Rashid, A.; Koç, M. Recent Advances in the Development of Stereolithography-Based Additive Manufacturing Processes: A Review of Applications and Challenges. Bioprinting 2024, 43, e00360. [Google Scholar] [CrossRef]
- Lee, J.M.; Son, K.; Lee, K.B. Evaluation of Photopolymer Resins for Dental Prosthetics Fabricated via the Stereolithography Process at Different Polymerization Temperatures—Part I: Conversion Rate and Mechanical Properties. J. Prosthet. Dent. 2024, 131, 166.e1–166.e9. [Google Scholar] [CrossRef] [PubMed]
- Romberg, S.K.; Kotula, A.P. Simultaneous Rheology and Cure Kinetics Dictate Thermal Post-Curing of Thermoset Composite Resins for Material Extrusion. Addit. Manuf. 2023, 71, 103589. [Google Scholar] [CrossRef] [PubMed]
- Atta, I.; Bourauel, C.; Alkabani, Y.; Mohamed, N.; Kimbe, H.; Alhotan, A.; Ghoneima, A.; Elshazly, T. Physiochemical and Mechanical Characterisation of Orthodontic 3D Printed Aligner Material Made of Shape Memory Polymers (4D Aligner Material). J. Mech. Behav. Biomed. Mater. 2024, 150, 106337. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Kim, H.; Kim, S.H.; Kim, S.J.; Cha, J.Y.; Lee, S.Y.; Lee, J.; Min, J.; Jang, S.; Khan, T.A.; et al. Mechanical and Viscoelastic Properties of a Temperature-Responsive Photocurable Resin for 3D Printed Orthodontic Clear Aligners. Sci. Rep. 2025, 15, 23530. [Google Scholar] [CrossRef]
- Pratap, B.; Gupta, R.K.; Bhardwaj, B.; Nag, M. Resin-Based Restorative Dental Materials: Characteristics and Future Perspectives. Jpn. Dent. Sci. Rev. 2019, 55, 126–138. [Google Scholar] [CrossRef]
- Ruíz de Azúa, O.; Agulló, N.; Arbusà, J.; Borrós, S. Improving Glass Transition Temperature and Toughness of Epoxy Adhesives by a Complex Room-Temperature Curing System by Changing the Stoichiometry. Polymers 2023, 15, 252. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Domarecka, M.; Kopacz, K.; Sokolowski, J.; Bociong, K. An Evaluation of the Properties of Urethane Dimethacrylate-Based Dental Resins. Materials 2021, 14, 2727. [Google Scholar] [CrossRef]
- Yoshinaga, K.; Yoshihara, K.; Yoshida, Y. Development of New Diacrylate Monomers as Substitutes for Bis-GMA and UDMA. Dent. Mater. 2021, 37, e391–e398. [Google Scholar] [CrossRef] [PubMed]
- Borandeh, S.; van Bochove, B.; Teotia, A.; Seppälä, J. Polymeric Drug Delivery Systems by Additive Manufacturing. Adv. Drug Deliv. Rev. 2021, 173, 349–373. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Xie, C.; Wang, G.; He, R.; Ding, G.; Wang, M.; Dai, D.; Fang, D. High Solid Loading, Low Viscosity Photosensitive Al₂O₃ Slurry for Stereolithography-Based Additive Manufacturing. Ceram. Int. 2019, 45, 203–208. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D Printing with Polymers: Challenges among Expanding Options and Opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef]
- Kilambi, H.; Cramer, N.B.; Schneidewind, L.H.; Shah, P.; Stansbury, J.W.; Bowman, C.N. Evaluation of Highly Reactive Mono-Methacrylates as Reactive Diluents for BisGMA-Based Dental Composites. Dent. Mater. 2009, 25, 33–38. [Google Scholar] [CrossRef][Green Version]
- Choi, Y.; Kim, J.; Lee, C.; Lee, G.; Hyeon, J.; Jeong, S.K.; Cho, N. Enhancing the Mechanical Strength of a Photocurable 3D Printing Material Using Potassium Titanate Additives for Craniofacial Applications. Biomimetics 2024, 9, 698. [Google Scholar] [CrossRef]
- Guo, G.; Fan, Y.; Zhang, J.F.; Hagan, J.L.; Xu, X. Novel Dental Composites Reinforced with Zirconia-Silica Ceramic Nanofibers. Dent. Mater. 2012, 28, 360–368. [Google Scholar] [CrossRef]
- Kundie, F.; Azhari, C.H.; Mansa, R.F.; Ahmad, Z.A. Effects of Filler Size on the Mechanical Properties of Polymer-Filled Dental Composites: A Review of Recent Developments. J. Phys. Sci. 2018, 29, 141–165. [Google Scholar] [CrossRef]
- Mewis, J.; Wagner, N.J. Colloidal Suspension Rheology; Cambridge University Press: Cambridge, UK, 2012. [Google Scholar] [CrossRef]
- Kim, K.-M.; Kim, H.; Kim, H.-J. Enhancing Thermo-Mechanical Properties of Epoxy Composites Using Fumed Silica with Different Surface Treatment. Polymers 2021, 13, 2691. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Zhou, M.; Drummer, D. Effects of Fumed Silica on Thixotropic Behavior and Processing Window by UV-Assisted Direct Ink Writing. Polymers 2022, 14, 3107. [Google Scholar] [CrossRef] [PubMed]
- Goh, G.D.; Yap, Y.L.; Agarwala, S.; Yeong, W.Y. Recent Progress in Additive Manufacturing of Fiber-Reinforced Polymer Composite. Adv. Mater. Interfaces 2019, 6, 1800271. [Google Scholar] [CrossRef]
- Schmidleithner, C.; Kalaskar, D.M. Stereolithography. In 3D Printing; Cvetković, D., Ed.; IntechOpen: London, UK, 2018; pp. 1–22. [Google Scholar] [CrossRef]
- De Hazan, Y.; Heinecke, J.; Weber, A.; Graule, T. High Solids Loading Ceramic Colloidal Dispersions in UV Curable Media via Comb-Polyelectrolyte Surfactants. J. Colloid Interface Sci. 2009, 337, 66–74. [Google Scholar] [CrossRef]
- Ma, S.; Fu, S.; Yang, T.; Li, K.; Chen, G.; Dong, Q.; Gao, Y.; Xu, L.; Ji, H. Unveiling the Critical Role of Rheology Modifiers in Additive Manufacturing of Geopolymers and Their Mechanical Properties. Addit. Manuf. 2023, 78, 103826. [Google Scholar] [CrossRef]
- De Camargo, I.L.; Morais, M.M.; Fortulan, C.A.; Branciforti, M.C. A Review on the Rheological Behavior and Formulations of Ceramic Suspensions for Vat Photopolymerization. Ceram. Int. 2021, 47, 11906–11921. [Google Scholar] [CrossRef]
- Aloui, F.; Lecamp, L.; Lebaudy, P.; Burel, F. Relationships between Refractive Index Change and Light Scattering during Photopolymerization of Acrylic Composite Formulations. J. Eur. Ceram. Soc. 2016, 36, 1805–1809. [Google Scholar] [CrossRef]
- Shaukat, U.; Rossegger, E.; Schlögl, S. A Review of Multi-Material 3D Printing of Functional Materials via Vat Photopolymerization. Polymers 2022, 14, 2449. [Google Scholar] [CrossRef]
- Ahmad, K.H.; Mohamad, Z.; Khan, Z.I.; Habib, M. Tailoring UV Penetration Depth in Photopolymer Nanocomposites: Advancing SLA 3D Printing Performance with Nanofillers. Polymers 2025, 17, 97. [Google Scholar] [CrossRef]
- Bove, A.; Calignano, F.; Galati, M.; Iuliano, L. Photopolymerization of Ceramic Resins by Stereolithography Process: A Review. Appl. Sci. 2022, 12, 3591. [Google Scholar] [CrossRef]
- Bennett, J. Measuring UV Curing Parameters of Commercial Photopolymers used in Additive Manufacturing. Addit. Manuf. 2017, 18, 203–212. [Google Scholar] [CrossRef]
- Mitkus, R.; Scharnofske, M.; Sinapius, M. Characterization 0.1 wt.% Nanomaterial/Photopolymer Composites with Poor Nanomaterial Dispersion: Viscosity, Cure Depth and Dielectric Properties. Polymers 2021, 13, 3948. [Google Scholar] [CrossRef]
- Sun, C.; Fang, N.; Wu, D.M.; Zhang, X. Projection micro-stereolithography using digital micro-mirror dynamic mask. Sens. Actuators A Phys. 2005, 121, 113–120. [Google Scholar] [CrossRef]
- Wieckowski, H.S.; Erb, R.M. Tuning Depth of Cure in Resins with Photoabsorbing Fillers for Vat Photopolymerization. MRS Commun. 2025, 15, 308–319. [Google Scholar] [CrossRef]
| Parameter | Typical Target/Guideline | Rationale |
|---|---|---|
| Viscosity at 25–30 °C (γ̇ ≈ 10–100 s−1) | 0.1–2.0 Pa·s (100–2000 mPa·s) | Reliable self-leveling and moderate peel forces |
| Zero-shear viscosity/yield stress | Low-to-moderate; just enough to prevent sagging | Stability without impeding leveling; avoid trapped voids |
| Shear-thinning index (n in power-law) | 0.5–0.9 (pseudoplastic) | Low η during recoating; higher η at rest |
| Operating temperature | 25–30 °C (heated vat recommended) | Heating reduces viscosity; hot lithography shows improved flow and green properties |
| Layer height vs. optical Dp | Dp ≈ 1.1–1.5 × layer thickness | Ensures bond without overcure; aligns with Jacobs’ working curve model |
| Fillers (vol%) | Minimal necessary; sub-micron preferred | Balances viscosity and scattering; improves dispersion, and reduces light attenuation |
| Technique | Viscosity at 25–30 °C (γ̇ ≈ 10–100 s−1) | Shear/Thixotropy Profile | Process Notes |
|---|---|---|---|
| SLA (laser) | ~0.5–3 Pa·s typical; up to ~5 Pa·s reported for conventional SLA; >10 Pa·s only with specialized linear-scan VPP | Mild shear-thinning helpful; low-to-moderate thixotropy acceptable | Blade/wiper aids redistribution; longer settle often tolerable. Upper conventional limit ≈5000 mPa·s; ultra-high viscosity feasible only with linear-scan VPP. |
| DLP (proj.) | ~0.1–2 Pa·s typical (100–2000 mPa·s); up to ~3 Pa·s possible with heating and very slow peel; higher viscosities generally require non-standard hardware | Shear-thinning needed; keep yield stress low enough to allow complete re-wetting | Fast self-leveling and minimized peel forces; heated vats often used. Ceramic DLP slurries printable in the ~1–2 Pa·s range at relevant shear rates. |
| MSLA (LCD) | ~0.1–1.5 Pa·s typical, evidenced by multiple LCD/MSLA datasheets (≈0.36–0.52 Pa·s common; some flexible resins up to ~2.2 Pa·s) | Similar to DLP; very short cycles demand rapid shear-thinning and recovery | Keep resin warm; avoid heavy pigments that hinder leveling. Vendor TDS show LCD/MSLA resins commonly 300–520 mPa·s, with some formulations near ~2 Pa·s. |
| Item | Recommended Practice | Reported Metric |
|---|---|---|
| Geometry/gap | Cone-plate (1–2°) or parallel-plate; 25–30 °C | Geometry, gap, temperature |
| Shear sweep | γ̇ = 0.1–100 s−1 (both up and down) | η(γ̇) curve; power-law fit (K, n) |
| Thixotropy/recovery | 3-interval test: low–high–low shear (e.g., 0.1/50/0.1 s−1) | % viscosity recovery at 30–60 s; hysteresis area |
| Yield stress | Stress ramp or creep tests | τy (Pa) and method |
| Temp dependence | 20–60 °C ramp | Arrhenius fit (activation energy for flow) |
| Viscoelasticity | SAOS (G′, G′′, tan δ) in LVR | G′, G′′ vs. ω at 25–30 °C |
| Reporting | Always include temperature and shear-rate for η values | η at 10 s−1 and 50 s−1 (25 °C/30 °C) |
| Lever | Primary Effect on Flow | Secondary Effects | Practical Guidance |
|---|---|---|---|
| ↑ Oligomer (UDMA/Bis-GMA) | ↑ η; mild shear-thinning | ↑ modulus, Tg; ↓ shrinkage | Dilute with reactive monomer to keep η < 2 Pa·s. |
| Reactive diluent (TEGDMA) | ↓ η; often Newtonian | ↑ crosslink density; risk brittleness | Limit to minimum that achieves printability. |
| Nanofiller (silica, etc.) | + thixotropy; ↑ η at low shear | ↑ stiffness; ↑ scattering if mismatched | Use sub-µm; surface-treat; disperse ultrasonically. |
| Pigments/absorbers | ~η neutral (low wt%) | Tune Dp; color/opacity | Use potent dyes at low ppm; avoid large pigments. |
| Index matching | — | ↓ scattering; ↑ Dp at a given loading | Match n(resin) ≈ n(filler) to preserve cure depth. |
| Factor | Optical Impact | Mitigation |
|---|---|---|
| ↑ Filler (vol%) | ↓ Dp; ↑ lateral light spread (XY overcure) | Limit loading; index-match; finer layers |
| Smaller particles | More centers → ↑ scattering; ↓ Dp | Use sub-µm but avoid excessive nano-loadings; disperse well |
| High viscosity | Non-uniform films; trapped bubbles → cure noise | Warm to 25–30 °C; add settle time; mild agitation |
| Thixotropy (high) | Incomplete re-wetting; uneven exposure | Keep τy low; ensure rapid breakdown under shear |
| Dp vs. layer | Dp too low → poor Z-bond; too high → z-bleed | Tune absorber to Dp ≈ 1.1–1.5 × layer thickness |
| Change | Typical Mechanical Outcome | Printability Implication |
|---|---|---|
| ↑ Oligomer fraction | ↑ modulus/strength/Tg; ↓ shrinkage | ↑ η; may require heating/slower cycles |
| +Sub-µm filler (5–15 wt%) | ↑ stiffness/hardness; radiopacity | ↑ η + shear-thinning; check dispersion and Dp |
| +Excess diluent | Easier flow; risk brittleness/shrinkage | ↓ η; consider toughener; ensure full conversion |
| Higher print temp (30 °C) | ↑ conversion; ↑ strength (via lower η during cure) | Validate dimensional accuracy; recalibrate Ec |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šimunović, L.; Brenko, L.; Marić, A.J.; Meštrović, S.; Haramina, T. Rheology of Dental Photopolymers for SLA/DLP/MSLA 3D Printing. Polymers 2025, 17, 2706. https://doi.org/10.3390/polym17192706
Šimunović L, Brenko L, Marić AJ, Meštrović S, Haramina T. Rheology of Dental Photopolymers for SLA/DLP/MSLA 3D Printing. Polymers. 2025; 17(19):2706. https://doi.org/10.3390/polym17192706
Chicago/Turabian StyleŠimunović, Luka, Luka Brenko, Antun Jakob Marić, Senka Meštrović, and Tatjana Haramina. 2025. "Rheology of Dental Photopolymers for SLA/DLP/MSLA 3D Printing" Polymers 17, no. 19: 2706. https://doi.org/10.3390/polym17192706
APA StyleŠimunović, L., Brenko, L., Marić, A. J., Meštrović, S., & Haramina, T. (2025). Rheology of Dental Photopolymers for SLA/DLP/MSLA 3D Printing. Polymers, 17(19), 2706. https://doi.org/10.3390/polym17192706







