Abstract
This paper presents a comprehensive review of natural fiber-reinforced composites (NFRCs) for lower-limb prosthetic designs. It covers the characteristics, types, and properties of natural fiber-reinforced composites as well as their advantages and drawbacks in prosthetic designs. This review also discusses successful prosthetic designs that incorporate NFRCs and the factors that make them effective. Additionally, this study explores the use of computational biomechanical models to evaluate the effectiveness of prosthetic devices and the key factors that are considered. Overall, this document provides a valuable resource for anyone interested in using NFRCs for lower-limb prosthetic designs.
1. Introduction
Lower-limb amputation is a complex and devastating issue affecting millions of people worldwide [1,2,3,4,5,6]. Prosthetic devices are the most practical choice for restoring ambulatory motor function in individuals with lower-limb amputations [7,8,9]. However, in developing countries, most prosthetic users are compelled to use rudimentary and inefficient designs because of their low acquisition costs [10,11]. This lack of affordable and efficient prosthetic devices perpetuates the marginalization of individuals with lower-limb amputations, subsequently affecting their musculoskeletal system and mobility [12,13,14,15,16,17,18,19,20,21].
In developed countries, the sustainability of materials and manufacturing components used in prosthetic devices is usually not a primary concern in the prosthetic design process [22]. Consequently, the most functional prostheses are those with the most advanced components and naturally higher costs [7,8,10,11,23,24,25,26,27,28]. Therefore, proposing alternative, sustainable, and cost-effective materials for lower-limb prosthetic designs could provide affordable prosthetic solutions for the most vulnerable populations.
Recent advances in natural fiber-reinforced composites (NFRCs) have demonstrated good mechanical and ecological properties compared with synthetic fibers (such as carbon and glass fibers), while also being economically accessible and abundant [29,30,31,32,33,34]. To mention a few, fibers such as kenaf [8,35,36,37], jute [38], ramie [39], and hemp [40] have highlighted their mechanical performance and versatility, comparing favorably against synthetic fibers in terms of their mechanical properties and common applications.
The aim of this review is to methodically evaluate NFRCs (natural fiber-reinforced composites) as a potential substitute material for use in lower-limb prosthetics. This study establishes the groundwork for future research and development in this sector by offering a thorough examination of the characteristics, manufacturing methods, advantages, and drawbacks of NFRCs, along with evaluating the pertinent international standards and available computational biomechanical modeling techniques to validate the performance and usability of devices. This work supports the development and production of prosthetic devices that are affordable, eco-friendly, and high-performing, improving the lives of those who have lost limbs, especially in situations where resources are scarce.
2. Background
2.1. Lower-Limb Amputation and Prosthetic Options
Lower-limb amputations can be caused by trauma, illnesses, or congenital problems, having a serious negative impact on both physical and emotional health [41,42,43,44,45,46,47,48]. Prosthetic devices have been created to solve this problem, and can be customized to match the unique demands of each user [7,8,9,10,11]. Finding a suitable fit for the user and assuring the durability of the device remain challenges, despite advances in prosthetic technology [18,19,20,21].
One major challenge associated with prosthetic devices is their high acquisition costs, ranging from several thousands to tens of thousands of dollars, depending on the type and complexity of the device. This cost can limit access to prosthetic devices for many individuals, particularly those with inadequate health insurance coverage [10,11,49,50,51,52]. Programs such as Medicare (https://www.medicare.gov, accessed on 12 May 2023) and Medicaid (https://medicaid.gov, accessed on 12 May 2023) in the United States may offer some relief; however, the costs associated with prosthetic devices may not be fully covered. In addition, restrictions on the types of devices covered or the frequency with which they can be replaced may limit access. Nevertheless, it must be highlighted that these government medical programs may vary in their availability and quality from one country to another, or, in some cases, may not exist, especially in developing countries [53].
In low- and middle-income countries, the high acquisition costs of prosthetic devices present a significant barrier to their accessibility [10,49,53,54]. Although efforts have been made to develop low-cost prosthetic devices using alternative materials and manufacturing processes, these devices may not offer the same level of functionality or durability as more expensive options [8,55,56].
2.2. Transtibial Prosthetic Design Considerations
Transtibial prostheses are lower-limb prosthetic devices that replace the missing or amputated foot and ankle. The design of transtibial prostheses involves several key components, including the socket, pylon or shank, and the foot or ankle [7,8,27,28,57].
The socket component (Figure 1a) is crucial for the prosthesis to fit the residual limb securely and comfortably. The socket must be made to offer a stable attachment point for the rest of the prosthesis and fit snugly over the residual limb [8,11,27,28]. A good fit is essential to ensure that the prosthesis performs as intended and does not irritate or disturb the user.
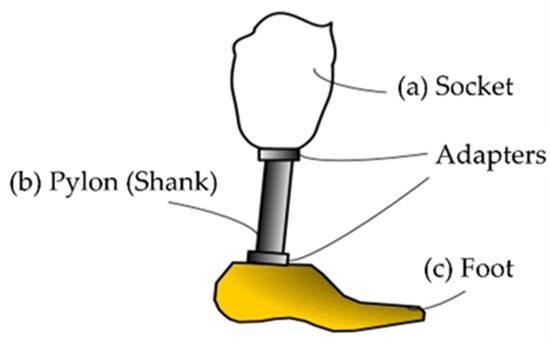
Figure 1.
Main components of a passive transtibial prosthesis: (a) the socket, the part of the prosthesis that fits over the residual limb (the remaining part of the amputated leg); (b) the shank (or pylon), a rigid component that extends from the socket down to the foot; (c) the foot, the component of the prosthesis that mimics the function of a natural foot, absorbs shock during walking, and provides stability. Reprinted from ref. [58].
Connecting the socket to the foot or ankle component is performed using the pylon or shank component (Figure 1b) of the prosthesis. For weight-bearing activities, such as walking or running [11], this component must provide sufficient support and stability [7]. The materials utilized for this component must be sufficiently sturdy to withstand continuous loading cycles without failure [10].
The foot component (Figure 1c) of the prosthesis is designed to replicate the function of the biological foot as much as possible [59,60,61,62,63,64]. This might involve incorporating features such as shock absorption, flexibility, and articulation into the design [7]. The materials used for this element must also be carefully selected to ensure that they are sufficiently durable to withstand repeated use over time [50]. Table 1 describes some details of the commercial prosthetic feet currently available on the market, as well as the different materials used to manufacture them.

Table 1.
Commercial prosthetic feet from different manufacturers.
Hydraulic systems, advanced sensors, and control systems are just a few more elements that transtibial prostheses may contemplate if necessary, increasing the cost for the user [11]. These features can provide the prosthesis with more control and allow a more fluid gait pattern.
Transtibial prostheses must be carefully designed considering characteristics such as the proper fit, support, functionality, and material selection [11]. In recent years, advances in both materials science and engineering have achieved more sophisticated prosthetic devices, but to advance the field of prosthetics and improve outcomes for those with amputated lower limbs, continued work in this area is crucial.
2.3. Materials Used in Prosthetic Manufacturing
For many years, conventional materials, such as metals and plastics, have mainly been used in the manufacture of prosthetics [7,11,65]. Although they are strong and long-lasting, metals, such as aluminum and titanium, can also be heavy and unwieldy [10,26,66]. In contrast, while plastics such as polypropylene and polyethylene are lightweight, they cannot be as strong or long-lasting as metals and usually deteriorate with time [7,10,65,67,68].
In contrast to conventional materials, synthetic composites offer several benefits. They are created by fusing a matrix substance, such as epoxy resin, with synthetic fibers such as carbon or glass fibers [29,69,70,71,72,73]. Excellent strength-to-weight ratios and customizability for particular design requirements are notable features of synthetic composites [70,74,75,76]. They also exhibit good fatigue characteristics and are corrosion-resistant [77,78,79,80]. Although they can be expensive [71,81,82,83,84,85,86,87], synthetic composites may not be biodegradable [8,27,28].
NFRCs have many advantages over synthetic and conventional materials [30,31,32]. Natural fibers, such as kenaf, flax, or jute, can be used to create these types of composites [29,73,88,89,90]. Natural fiber-reinforced composites have exceptional mechanical qualities, including a low density, biodegradability, and high strength-to-weight and impact–resistance ratios [29,33,34,90]. Additionally, compared with synthetic composites, they are less expensive to manufacture [33].
Ensuring the consistent quality and performance of NFRCs is one of the key issues regarding these materials. Natural fibers can have different qualities depending on factors such as their moisture content and the harvesting conditions [89,91,92,93]. Nevertheless, recent studies have shown that high-quality natural fiber-reinforced composites may be fabricated to match the specifications for prosthetic designs with fiber treatment and a good composite composition [30,31,79,94,95].
Each material has its own unique advantages and disadvantages in prosthetic manufacturing. Conventional materials are durable but may be heavy or uncomfortable for users, and they offer excellent strength-to-weight ratios but may not be biodegradable and can be expensive, whereas natural fiber-reinforced composites offer a lightweight and biodegradable option with excellent mechanical properties but require careful quality control during production.
3. Natural Fiber-Reinforced Composites
3.1. Characteristics of Natural Fibers
The utilization of natural fibers as reinforcement materials in composite materials has garnered significant attention owing to their distinctive properties [73]. Derived from diverse sources (Figure 2), such as plants, animals, and minerals [69,90,96], natural fibers have become increasingly popular in recent years owing to their cost-effectiveness, biodegradability, and renewability [30,31,32].
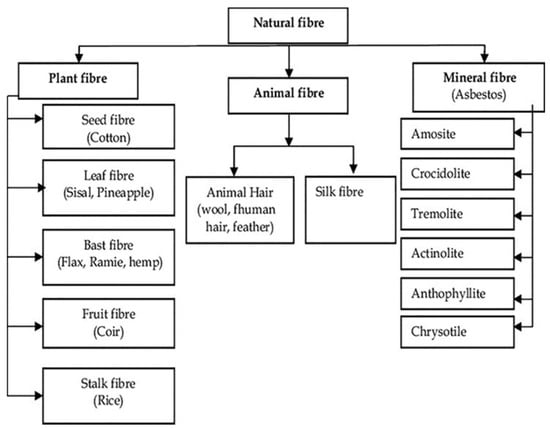
Figure 2.
Classification of natural fibers based on their origin: plant, animal, or mineral [29]. Reprinted from Materials Today: Proceedings, Vol. 50, Sandeep Kumar, Alakesh Manna, Rakesh Dang, A review on applications of natural fiber-reinforced composites (NFRCs), Pages 1632–1636, Copyright (2022), with permission from Elsevier.
The remarkable characteristic of natural fibers lies in their exceptional strength-to-weight ratio, particularly in jute, flax, and hemp fibers [38,79,90,97]. Owing to their robust tensile strength, natural fibers are highly suitable for integration into composite materials, particularly in applications where weight reduction is paramount, such as the development of lower-limb prosthetics. Furthermore, the low density of natural fibers presents an additional advantage, as they significantly contribute to reducing the overall weight in weight-sensitive applications [29,33,34]. The mechanical and physical properties of the most popular natural fibers are shown in Table 2.

Table 2.
Physical and mechanical properties of the most popular natural fibers [88,98,99,100].
Another noteworthy attribute of natural fibers is their biodegradability and renewability, rendering them an environmentally friendly alternative to synthetic fibers. By incorporating natural fibers into composite materials, the environmental impact of such materials can be reduced, thereby promoting sustainability [8,30,31,32].
Moisture absorption is a significant consideration in the utilization of natural fibers. Untreated natural fibers tend to exhibit higher moisture absorption than treated fibers [95]. This moisture absorption can cause dimensional changes and affect the mechanical properties of composites [33]. Techniques such as alkali treatment and the incorporation of hydrophobic additives or coatings can effectively mitigate moisture absorption [30,31,95].
Natural fibers possess distinctive characteristics that make them highly suitable for integration into composite materials, making them attractive substitutes for synthetic fibers. Incorporating natural fibers into composite materials not only offers the potential to reduce the environmental impact associated with these materials but also provides a sustainable solution for the design of lower-limb prosthetics.
3.2. Types and Properties of Natural Fiber-Reinforced Composites
Natural fiber-reinforced composites typically consist of natural fibers embedded within a polymer matrix [96]. The selection of the polymer matrix significantly influences the mechanical properties and overall performance of the composite [29,101,102,103,104,105,106]. The matrix materials commonly used in NFRCs include polypropylene (PP) [40], polyester (PET) [72,107,108], and epoxy [109,110,111,112,113], each offering distinct advantages in terms of their mechanical strength, durability, and compatibility with natural fibers [72,114,115].
While thermoplastic and thermosetting matrices are mostly used in NFRCs, bio-based epoxy resins derived from renewable sources such as vegetable oils offer a sustainable alternative for the matrix phase [116,117,118,119]. These bio-resins can potentially improve characteristics like the biodegradability and environmental impact of NFRCs when combined with natural-fiber reinforcements [118]. However, challenges related to the fiber–matrix compatibility, moisture sensitivity, and achieving the optimal mechanical performance still present difficulties that hinder their use in heavy-duty and long-lasting applications, such as in prosthetic devices.
The mechanical properties of NFRCs play a critical role in determining their suitability for lower-limb prosthetic designs. Parameters such as their tensile strength, flexural strength, impact resistance, and fatigue behavior are of utmost importance and must be carefully considered (Table 1).
Tensile strength represents the maximum stress that a material can withstand under tension before failure. NFRCs exhibit promising tensile strength owing to the reinforcing effect of their natural fibers. Several factors, including the fiber type, fiber content, fiber orientation, and fiber–matrix adhesion, influence the tensile properties of NFRCs [33,69,93,120,121]. Table 3 exhibits a summary of several NFRCs proposed and studied by different authors in detail.

Table 3.
Tensile and flexural strengths of some NFRCs [68].
Flexural strength characterizes a material’s ability to resist deformation when subjected to bending. NFRCs exhibit considerable flexural strength, which renders them suitable for load-bearing applications. The flexural properties of NFRCs are influenced by factors such as the fiber content, fiber length, fiber orientation, and matrix properties [33,74,93,141,142]. Attaining proper fiber–matrix interactions and optimal fiber dispersion within the matrix are crucial for achieving enhanced flexural strength.
The impact resistance of NFRCs is of utmost importance in prosthetic design because it determines the material’s capability to absorb and dissipate energy during dynamic loading [7,24,25]. As well as the flexural and tensile strength, the impact properties of NFRCs are influenced by the fiber selection, chemical treatment, and matrix properties [30,31,93]. Comprehensive assessments and optimization of impact resistance are essential to ensure the reliability and functionality of lower-limb prosthetics.
3.3. Manufacturing Methods for Natural Fiber-Reinforced Composites
The manufacturing process for natural fiber-reinforced composites (NFRCs) is similar to that of conventional composites, differing primarily in the utilization of natural fibers instead of synthetic fibers. Various manufacturing methods exist for producing NFRCs, each with its own set of advantages and disadvantages [29,33,88,121]. The selection of a specific method depends on its intended application and production requirements [120].
The hand-layup approach (Figure 3) is the most widely used manufacturing method. It entails manually inserting fibers into a mold, followed by applying resin to help the fibers join. This approach is well suited for small-scale production because it is simple and economical [121,143,144].
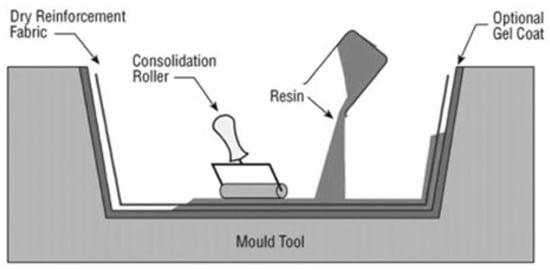
Figure 3.
Hand-layup method for manufacturing composite materials [145]. Reprinted from Comprehensive Composite Materials, Author(s): D. Cripps, T.J. Searle, J. Summerscales, Title of chapter: Comprehensive Composite Materials, Pages 737–761, Copyright (2000), with permission from Elsevier.
Compression molding is another process used in the production of NFRCs. Using this technique, the fibers are placed in a mold and compressed under pressure to release trapped air. The mold is then filled with resin, which is then heated to start the resin’s curing process. Compression molding permits the creation of intricately formed components, and is appropriate for high-volume production [33,89,121,146].
The resin transfer molding (RTM) method (Figure 4) is employed to produce composites with high strength and stiffness. In this approach, the fibers are positioned within a mold and resin is injected under pressure. The mold is then heated to promote the curing of the resin. RTM has widespread applications in the automotive and aerospace industries [71,147,148,149,150].
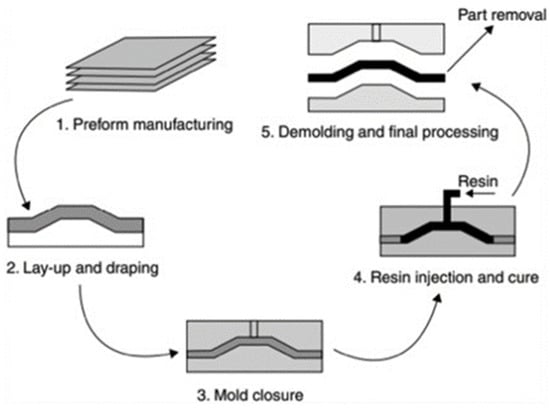
Figure 4.
Resin transfer molding (RTM) method for manufacturing composite materials [151]. Reprinted from Design for Sustainability, Author(s): Nadlene Razali, Muhd Ridzuan Mansor, Ghazali Omar, Syed Ahmad Faiz Syed Kamarulzaman, Mohd Hanafee Zin, Nadia Razali, Title of chapter: Design for Sustainability, Pages 395–413, Copyright (2021), with permission from Elsevier.
Pultrusion is a continuous manufacturing method that is extensively used for the production of fiber-reinforced composites. In this technique, the fibers are pulled through a resin bath and subsequently passed through a heated die, resulting in resin curing. Pultrusion is well suited for creating components with a consistent cross-section and is commonly employed in the construction sector [89,120,121,146,147].
Finally, the filament winding method is employed to manufacture cylindrical NFRC parts, including pipes and tanks. This process involves winding fibers around a mandrel in a specific pattern, followed by the application of a resin to facilitate fiber bonding. After curing, the mandrel is removed, leaving the final product [71,120,146,147,152].
4. Lower-Limb Prosthetic Design Using Natural Fiber-Reinforced Composites
4.1. Advantages and Drawbacks of Natural Composites in Prosthetic Design
NFRCs have garnered attention in the field of lower-limb prosthetic design owing to their unique properties and potential benefits. However, like other existing materials, they have their own advantages and drawbacks, which must be carefully considered and addressed in the design and manufacturing processes to fully exploit their potential in prosthetic applications.
Advantages:
- Low Weight and High Strength-to-Weight Ratio: As mentioned before, NFRCs have the remarkable ability to have both a minimal weight and a high strength-to-weight ratio [29,33,34,55]. This quality is very helpful for designing lower-limb prosthetics because it makes it possible to create lightweight, comfortable prosthetics without sacrificing strength and longevity [7,8,9,11,66].
- Energy Return and Shock Absorption: The mechanical properties of natural composites, including their ability to store and release energy, contribute to enhanced energy return and shock absorption [30,31,55,56]. This feature is crucial in lower-limb prosthetics, as it mimics the natural gait cycle and improves the overall walking efficiency [7,10,24,25,26,58].
- Sustainability and Environmental Friendliness: Natural fibers used as composite reinforcements, such as kenaf and flax, are renewable resources that provide a sustainable alternative to synthetic fibers [8,29,30,31,32,33,35,36,37,98,119]. The utilization of natural composites in prosthetic design aligns with the increasing demand for eco-friendly materials and reduces the reliance on non-renewable resources.
Drawbacks:
- Moisture Absorption: Natural fibers have a propensity to absorb moisture [89,93], which can lead to dimensional changes and diminished mechanical properties of the composites [33]. This drawback presents a challenge for prosthetic designs, as exposure to moisture can affect the long-term performance and durability of prosthetic devices [50]. Detailed data on different natural fibers are displayed in Table 1.
- Limited Durability: Compared to synthetic-fiber-reinforced composites, natural composites may exhibit lower durability and resistance to wear and tear [29,34,153]. The natural fibers used in reinforcement may degrade over time [94], affecting the overall lifespan of prosthetic devices.
- Variability in Mechanical Properties: Natural fibers, which are organic materials, inherently exhibit variability in their mechanical properties [89,93]. This variability can pose challenges in achieving consistent and predictable performance with natural fiber-reinforced composites in prosthetic designs. This necessitates careful selection and quality control of the natural fibers to ensure consistent mechanical properties and high performance of the prosthetic devices.
4.2. Cases of Natural Fiber-Reinforced Composites Used in Prosthetic Designs
Nurhanisah et al. [8] proposed the use of a kenaf-fiber-reinforced composite material for the fabrication of transtibial prosthetic sockets (Figure 5). Their proposed design exhibited favorable results in terms of mechanical properties and comfort, making it suitable for providing good strength and added aesthetic value. Additionally, the proposed design demonstrated environmental friendliness compared to fiberglass-based sockets.

Figure 5.
Prosthetic socket made from a kenaf-woven-fabric composite designed by Nurhanisah et al. Reprinted from ref. [8].
In a study by Irawan et al. [55], the manufacturing of lower-limb prosthetic sockets using ramie fibers and epoxy composites was suggested. Their results showed that such sockets had a significant impact on comfort because of their light weight, strength, and flexibility compared to fiberglass sockets. Furthermore, sockets fabricated with the ramie fibers exhibited a considerably lower weight than those made with fiberglass, with a difference of 186 g, representing a 46.26% reduction. As mentioned several times before, the strength-to-weight ratio exhibited by natural fibers is one of their key advantages over synthetic fibers [33,34], which is essential for maintaining the prosthetic weight within an appropriate range, and thus avoiding increased energy expenditure and excessive stress on the user’s residual limb [11,66].
Moreover, a study by Mankai et al. [56] showed that esparto fibers (Stipa tenacissima) are a promising alternative material for manufacturing prosthetic sockets. Their fatigue testing results revealed the viscoelastic behavior of the material and estimated its lifespan to be 2,325,000 cycles, satisfying 77.5% of the ISO 10328 objective.
These studies provide evidence for the potential of NFRCs in lower-limb prosthetic designs. The utilization of these composites can result in lightweight, strong, and biocompatible prostheses. Furthermore, their incorporation into prosthetic designs offers environmental benefits, as natural fibers are renewable resources with a lower carbon footprint than synthetic fibers. This makes them a more sustainable option for prosthetic designs. In addition to their mechanical properties and sustainability advantages, natural fiber-reinforced composites can also provide aesthetic benefits by providing prosthetics with a more natural and organic appearance, thus mitigating the stigma associated with prosthetic use.
5. Evaluation of Natural Fiber-Reinforced Composite Prosthetics
5.1. Standards and Guidelines for Evaluating Prosthetic Devices
The evaluation of prosthetic devices is an important step in the design process because it ensures that the functional, safety, and performance requirements are met. Adhering to accepted norms and criteria is essential for prostheses constructed of NFRCs to guarantee their safe and efficient use.
One widely recognized standard for evaluating prosthetic devices is ISO 10328, which provides comprehensive guidelines for the mechanical testing of lower-limb prostheses [154,155]. This standard defines the testing procedures for various mechanical properties, including static strength, fatigue strength, and impact resistance. Furthermore, ISO 22675 offers guidelines specifically for testing ankle/foot prostheses, encompassing durability, strength, and range-of-motion requirements [156]. Both ISO 10328 and 22675 establish frameworks for evaluating prosthetic devices, ensuring the adherence to safety and performance requirements. Widely recognized and employed by manufacturers, clinicians, and researchers in the field of prosthetics, these standards guarantee the safety, efficacy, and reliability of prosthetic devices for individuals with lower-limb amputations.
ISO 10328 outlines procedures for both the static and dynamic testing of lower-limb prostheses, encompassing mechanical properties such as static strength, fatigue strength, and impact resistance (Figure 6). Static strength testing involves subjecting the prosthetic device to increasing loads until failure, whereas fatigue strength testing simulates cyclic loading to mimic normal usage stresses. Impact resistance testing involves dropping a weight onto the device to simulate the impact of a fall.
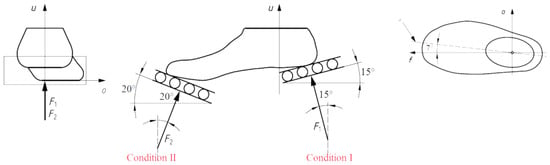
Figure 6.
Alignment and angles of test loads for a prosthetic foot, established by ISO 10328 [157]. Reprinted from Procedia Engineering, Vol. 10, C. Colombo, E.G. Marchesin, L. Vergani, E. Boccafogli, G. Verni, Study of an ankle prosthesis for children: adaptation of ISO 10328 and experimental tests, Pages 3510–3517, Copyright (2011), with permission from Elsevier.
ISO 22675 provides guidelines for testing ankle–foot prostheses, including the requirements for durability, strength, and range of motion (Figure 7). This standard presents testing procedures for both cyclic and static loading, aiming to replicate the load conditions experienced during the stance phase of an individual’s gait. Cyclic loading tests involve applying loads to the device cyclically to simulate typical usage stresses, whereas static loading tests apply loads at specific points in the gait cycle to simulate the maximum loads at those instances.
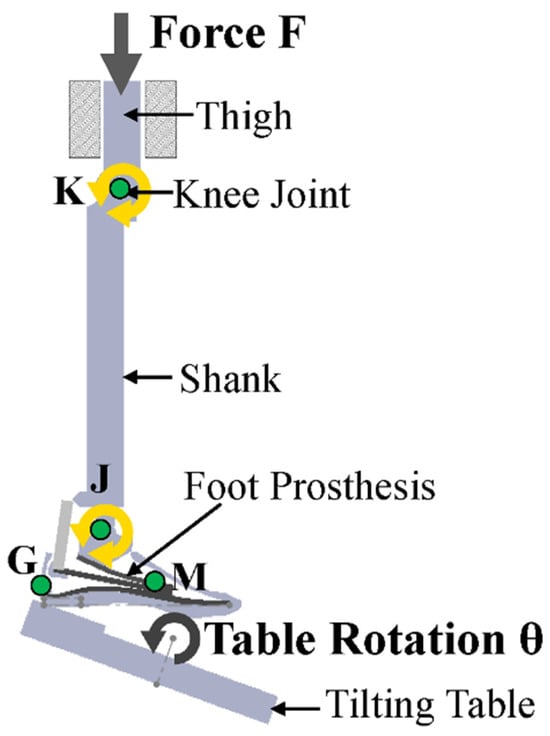
Figure 7.
Alignment and angles of test loads for a prosthetic foot established in ISO 22675. Reprinted from ref. [158].
Numerous other studies have also employed the ISO 10328 [10,56,154,159,160] and 22675 [160,161,162] standards to assess the mechanical properties of prosthetic devices. These standards offer a valuable framework for evaluating the safety and performance of such devices, enjoying broad recognition and adoption by researchers, clinicians, and manufacturers in the prosthetics field. Additionally, organizations such as the American Orthotic and Prosthetic Association (AOPA) (https://www.aopanet.org/, accessed on 1 August 2023) [160,162] and KS P 8403 [163,164] have established guidelines for prosthetic device design, fabrication, fitting, clinical evaluation, and follow-up care.
Although these criteria and recommendations offer a framework for assessing prosthetic devices, it is crucial to keep in mind that not all device types or materials necessarily fall under their purview. Additional testing and assessments may be required for NFRC prostheses to guarantee their compliance with appropriate safety and performance standards.
5.2. Using Computational Biomechanical Models to Assess Prosthetic Devices
Computational biomechanical models have become a prevalent tool for assessing the performance of prosthetic devices, enabling simulations of the interaction between the device and the residual limb, as well as the forces and stresses during walking. These models offer the opportunity to optimize prosthetic designs and evaluate device performance under diverse conditions [165,166,167] (Figure 8).
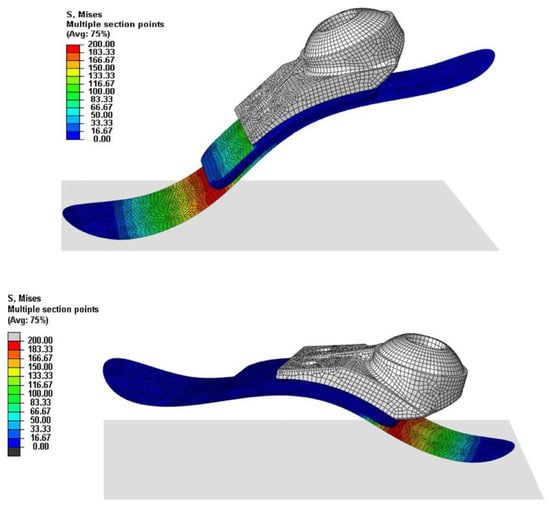
Figure 8.
Illustrative finite-element analysis of a prosthetic foot designed and studied by Song et al. [164] (Note: The data shown in this figure is for illustrative purposes only and is not relevant to the present discussion). Reproduced with permission from Youngnam Song et al., International Journal of Precision Engineering and Manufacturing; published by Springer Nature, 2019.
In the context of NFRC prosthetics, computational biomechanical models allow the assessment of the impact of various design parameters on device performance (Figure 9). Parameters such as the fiber orientation, number of layers, and composite laminate thickness can be evaluated using these models [168,169]. Additionally, these models facilitate assessments of the effects of different loading conditions on device performance, such as walking on different terrains or at varying speeds [165,166,167].
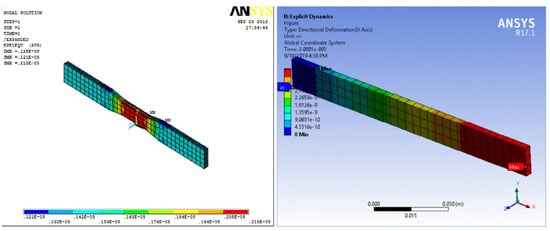
Figure 9.
Illustrative tensile and flexural finite-element analysis results for an NFRC studied by Balasubramanian et al. [170] (Note: The data shown in this figure is for illustrative purposes only and is not relevant to the present discussion). Reprinted from Materials Today: Proceedings, Vol. 28, K. Balasubramanian, N. Rajeswari, K. Vaidheeswaran, Analysis of mechanical properties of natural fiber composites by experimental with FEA, Pages 1149–1153, Copyright (2020), with permission from Elsevier.
An inherent challenge in using computational biomechanical models for prosthetic designs is the requirement of accurate input data. This includes information about the geometry and material properties of both the prosthetic device and the residual limb. However, advances in imaging technology and material characterization techniques have led to increasingly accurate data acquisition [166,171,172].
The application of computational biomechanical models is a potent tool for designing and evaluating NFRC prosthetics. By utilizing these models, the design of a device can be optimized, and its performance can be evaluated under diverse conditions, ultimately leading to improved prosthetic devices for individuals with lower-limb amputations [67,167,173].
Finite-element analysis (FEA) is a widely used computational biomechanical tool for the design and evaluation of prosthetic devices. FEA is a numerical method that can simulate complex mechanical systems, including prosthetic devices and the human body, by dividing them into simpler elements. The mathematical equations applied to these elements allow FEA to predict the system behavior under different loading conditions [166,174,175]. FEA enables the assessment of mechanical performance in the context of prosthetic designs and evaluation under different specific loading scenarios, including walking, running, and leaping. Additionally, this computational biomechanical tool makes it easier to optimize designs of devices by analyzing the effects of many design factors, such as the material qualities, shape, and thickness.
An advantage of FEA is its ability to assess the stress and strain distribution within the prosthetic device and residual limb. This information helps in identifying areas of high stress or strain that could lead to failure or discomfort, prompting design optimization to mitigate these concerns. FEA has been extensively used in the design and evaluation of NFRCs [120,143,144,162,168,169,170]. For instance, it has been employed to evaluate the impact of different fiber orientations and laminate configurations on the mechanical performance of devices.
Even though computational biomechanics possesses multiple advantages, such as evaluating prosthetic device performance under different loading conditions, there are limitations. The accuracy of the results depends on the accuracy of the input data and assumptions made in the model, which can introduce errors and uncertainties. Acquiring accurate input data, such as the geometry and material properties, may be experimentally challenging. Moreover, the complexity of the models used in computational biomechanics can make interpreting and understanding the underlying mechanisms difficult. Computational biomechanics can also be computationally expensive and time-consuming, which may restrict their use in certain applications. Finally, it is essential to recognize that computational biomechanics cannot fully replace experimental testing, and that the results of computational models should be validated experimentally.
6. Future Directions and Conclusions
The integration of NFRCs in lower-limb prosthetic designs has demonstrated significant promise in recent times. These materials have several advantages over conventional prosthetic materials, including enhanced strength, durability, and biocompatibility. Nevertheless, there remains considerable scope for further exploration to fully unlock the potential of these materials.
A compelling avenue for future research is the development of novel NFRC materials with improved properties. This may entail exploring new natural fibers, such as bamboo or hemp, or devising innovative processing techniques to enhance the mechanical properties of existing fibers. Furthermore, it is imperative to evaluate the performance of NFRC prostheses through both computational modeling and experimental testing. This comprehensive assessment is pivotal to ensure the safety and efficacy of these materials across a diverse range of applications.
In conclusion, the integration of NFRCs in lower-limb prosthetic designs holds promise for transformative advancements in the field. These materials exhibit numerous advantages over conventional prosthetic materials, including increased strength, durability, and biocompatibility. Furthermore, they have the potential to offer enhanced cost-effectiveness and eco-friendliness compared to traditional alternatives.
However, to achieve widespread adoption in prosthetic designs, several challenges must be resolved. The foremost task involves the development of new materials with improved properties. Additionally, it is imperative to develop innovative prosthetic devices that effectively capitalize on the distinctive attributes of these materials. Concurrently, ongoing assessments of their safety and efficacy through the combined use of computational models and experimental testing remain crucial.
Notwithstanding these challenges, the potential benefits of NFRCs engender a compelling domain for future research. Through sustained exploration and refinement, these materials could significantly enhance the quality of life of millions of individuals worldwide who rely on prosthetic devices to preserve their mobility and independence.
Author Contributions
Conceptualization, A.D.C.-F. and M.S.-H.; methodology, A.D.C.-F. and M.S.-H.; investigation: A.D.C.-F.; writing—original draft, A.D.C.-F., M.S.-H. and V.G.-A.; writing—review and editing, A.D.C.-F., M.S.-H., V.G.-A., I.M.-M., L.E.V.-O. and H.D.M.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
The authors would like to thank the National Council for Science and Technology of Mexico (CONACYT) for the Ph.D. Scholarship support given to Angel Daniel Castro Franco (CVU No. 983649). The authors are also greatly grateful to the Universidad Autónoma de Baja, California for facilitating the access and use of their facilities and equipment to carry out this research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ahmad, N.; Thomas, G.N.; Gill, P.; Chan, C.; Torella, F. Lower limb amputation in England: Prevalence, regional variation and relationship with revascularisation, deprivation and risk factors. A retrospective review of hospital data. J. R. Soc. Med. 2014, 107, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Imam, B.; Miller, W.C.; Finlayson, H.C.; Eng, J.J.; Jarus, T. Incidence of lower limb amputation in Canada. Can. J. Public Health 2017, 108, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Behrendt, C.A.; Sigvant, B.; Szeberin, Z.; Beiles, B.; Eldrup, N.; Thomson, I.; Venermo, M.; Altreuther, M.; Menyhei, G.; Nordanstig, J.; et al. International Variations in Amputation Practice: A VASCUNET Report. Eur. J. Vasc. Endovasc. Surg. 2018, 56, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Moini, M.; Rasouli, M.R.; Khaji, A.; Farshidfar; Heidari, P. Patterns of extremity traumas leading to amputation in Iran: Results of Iranian National Trauma Project. Chin. J. Traumatol. = Zhonghua Chuang Shang Za Zhi 2009, 12, 77–80. Available online: http://www.ncbi.nlm.nih.gov/pubmed/19321050 (accessed on 13 January 2022). [PubMed]
- Rouhani, A.; Mohajerzadeh, S. An epidemiological and etiological report on lower extremity amputation in northwest of Iran. Arch. Bone Jt. Surg. 2013, 1, 103–106. Available online: http://www.ncbi.nlm.nih.gov/pubmed/25207299 (accessed on 13 January 2022). [PubMed]
- Shaw, J.; Challa, S.; Conway, D.; Liu, M.; Haonga, B.; Eliezer, E.; Morshed, S.; Shearer, D. Quality of life and complications in lower limb amputees in Tanzania: Results from a pilot study. Lancet Glob. Health 2018, 6, S18. [Google Scholar] [CrossRef]
- Gard, S. Prosthetic Devices and Methods. In Wiley Encyclopedia of Biomedical Engineering; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2006; Volume 1960, no. 4; pp. 1–21. [Google Scholar] [CrossRef]
- Nurhanisah, M.H.; Hashemi, F.; Paridah, M.T.; Jawaid, M.; Naveen, J. Mechanical properties of laminated kenaf woven fabric composites for below-knee prosthesis socket application. IOP Conf. Ser. Mater. Sci. Eng. 2018, 368, 012050. [Google Scholar] [CrossRef]
- Strait, E.; McGimpsey, G.; Bradford, T. Limb Prosthetics Services and Devices. White Paper; January 2006; pp. 1–35. Available online: https://www.nist.gov/system/files/documents/2017/04/28/239_limb_prosthetics_services_devices.pdf (accessed on 13 January 2022).
- Lee, W.C.C.; Zhang, M.; Chan, P.P.Y.; Boone, D.A. Gait analysis of low-cost flexible-shank transtibial prostheses. IEEE Trans. Neural Syst. Rehabil. Eng. 2006, 14, 370–377. [Google Scholar] [CrossRef] [PubMed]
- DeWees, T. Transtibial prosthetics. In Orthotics and Prosthetics in Rehabilitation; Elsevier: Amsterdam, The Netherlands, 2020; pp. 605–634. [Google Scholar] [CrossRef]
- Boulton, A.J.; Vileikyte, L.; Ragnarson-Tennvall, G.; Apelqvist, J. The global burden of diabetic foot disease. Lancet 2005, 366, 1719–1724. [Google Scholar] [CrossRef] [PubMed]
- Vileikyte, L. Diabetic foot ulcers: A quality of life issue. Diabetes. Metab. Res. Rev. 2001, 17, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Renström, P.; Grimby, G.; Morelli, B.; Palmertz, B. Thigh muscle atrophy in below-knee amputees. Scand. J. Rehabil. Med. Suppl. 1983, 9, 150–162. [Google Scholar] [PubMed]
- Jaegers, S.M.; Arendzen, J.H.; de Jongh, H.J. Changes in hip muscles after above-knee amputation. Clin. Orthop. Relat. Res. 1995, 319, 276–284. Available online: http://www.ncbi.nlm.nih.gov/pubmed/7554640 (accessed on 3 February 2022). [CrossRef]
- Burger, H.; Valenčič, V.; Marinček, Č.; Kogovšek, N. Properties of musculus gluteus maximus in above-knee amputees. Clin. Biomech. 1996, 11, 35–38. [Google Scholar] [CrossRef]
- Schmalz, T.; Blumentritt, S.; Reimers, C.D. Selective thigh muscle atrophy in trans-tibial amputees: An ultrasonographic study. Arch. Orthop. Trauma Surg. 2001, 121, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Henson, D.P.; Edgar, C.; Ding, Z.; Sivapuratharasu, B.; Le Feuvre, P.; Finnegan, M.E.; Quest, R.; McGregor, A.H.; Bull, A.M. Understanding lower limb muscle volume adaptations to amputation. J. Biomech. 2021, 125, 110599. [Google Scholar] [CrossRef] [PubMed]
- Geurts, A.C.H.; Mulder, T.W. Reorganisation of Postural Control Following Lower Limb Amputation: Theoretical Considerations and Implications for Rehabilitation. Physiother. Theory Pract. 1992, 8, 145–157. [Google Scholar] [CrossRef]
- Silverman, A.K.; Fey, N.P.; Portillo, A.; Walden, J.G.; Bosker, G.; Neptune, R.R. Compensatory mechanisms in below-knee amputee gait in response to increasing steady-state walking speeds. Gait Posture 2008, 28, 602–609. [Google Scholar] [CrossRef] [PubMed]
- Clites, T.R.; Carty, M.J.; Ullauri, J.B.; Carney, M.E.; Mooney, L.M.; Duval, J.F.; Srinivasan, S.S.; Herr, H.M. Proprioception from a neurally controlled lower-extremity prosthesis. Sci. Transl. Med. 2018, 10, eaap8373. [Google Scholar] [CrossRef] [PubMed]
- Cummings, D. Prosthetics in the developing world. Prosthet. Orthot. Int. 1996, 20, 51–60. [Google Scholar] [CrossRef][Green Version]
- McDonald, C.L.; Kramer, P.A.; Morgan, S.J.; Halsne, E.G.; Cheever, S.M.; Hafner, B.J. Energy expenditure in people with transtibial amputation walking with crossover and energy storing prosthetic feet: A randomized within-subject study. Gait Posture 2018, 62, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Macfarlane, P.A.; Nielsen, D.H.; Shurr, D. Mechanical gait analysis of transfemoral amputees: SACH foot versus the Flex-Foot. J. Prosthet. Orthot. 1997, 9, 144–155. [Google Scholar] [CrossRef]
- Powers, C.M.; Torburn, L.; Perry, J.; Ayyappa, E. Influence of prosthetic foot design on sound limb loading in adults with unilateral below-knee amputations. Arch. Phys. Med. Rehabil. 1994, 75, 825–829. Available online: http://www.ncbi.nlm.nih.gov/pubmed/8024435 (accessed on 7 January 2022). [CrossRef] [PubMed]
- Klodd, E.; Hansen, A.; Fatone, S.; Edwards, M. Effects of prosthetic foot forefoot flexibility on gait of unilateral transtibial prosthesis users. J. Rehabil. Res. Dev. 2010, 47, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Joshi, S.; Drzal, L.; Mohanty, A.; Arora, S. Are natural fiber composites environmentally superior to glass fiber reinforced composites? Compos. Part A Appl. Sci. Manuf. 2004, 35, 371–376. [Google Scholar] [CrossRef]
- Etcheverry, M.; Barbosa, S.E. Glass Fiber Reinforced Polypropylene Mechanical Properties Enhancement by Adhesion Improvement. Materials 2012, 5, 1084–1113. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Manna, A.; Dang, R. A review on applications of natural Fiber-Reinforced composites (NFRCs). Mater. Today Proc. 2022, 50, 1632–1636. [Google Scholar] [CrossRef]
- Dixit, S.; Goel, R.; Dubey, A.; Shivhare, P.R.; Bhalavi, T. Natural Fibre Reinforced Polymer Composite Materials—A Review. Polym. Renew. Resour. 2017, 8, 71–78. [Google Scholar] [CrossRef]
- ArunKumar, D.; Kaushik, V.; Raghavedra, R.P. Tensile and Impact properties of jute/glass and jute/carbon fiber reinforced polypropylene. J. Polym. Compos. 2016, 4, 35–39. [Google Scholar]
- Mohammed, A.A.; Bachtiar, D.; Siregar, J.P.; Rejab, M.R.M.; Hasany, S.F. Physicochemical Study of Eco-Friendly Sugar Palm Fiber Thermoplastic Polyurethane Composites. BioResources 2016, 11, 9438–9454. [Google Scholar] [CrossRef]
- Zhao, X.; Copenhaver, K.; Wang, L.; Korey, M.; Gardner, D.J.; Li, K.; Lamm, M.E.; Kishore, V.; Bhagia, S.; Tajvidi, M.; et al. Recycling of natural fiber composites: Challenges and opportunities. Resour. Conserv. Recycl. 2022, 177, 105962. [Google Scholar] [CrossRef]
- Liu, C.; Luan, P.; Li, Q.; Cheng, Z.; Sun, X.; Cao, D.; Zhu, H. Biodegradable, Hygienic, and Compostable Tableware from Hybrid Sugarcane and Bamboo Fibers as Plastic Alternative. Matter 2020, 3, 2066–2079. [Google Scholar] [CrossRef]
- Saba, N.; Paridah, M.T.; Jawaid, M. Mechanical properties of kenaf fibre reinforced polymer composite: A review. Constr. Build. Mater. 2015, 76, 87–96. [Google Scholar] [CrossRef]
- Chen, Y.; Sun, L.; Chiparus, O.; Negulescu, I.; Yachmenev, V.; Warnock, M. Kenaf/Ramie Composite for Automotive Headliner. J. Polym. Environ. 2005, 13, 107–114. [Google Scholar] [CrossRef]
- Yuhazri, M.Y.; Phongsakorn, P.T.; Sihombing, H.; Jeefferie, A.R.; Perumal, P.; Kamarul, A.M.; Rassiah, K. Mechanical properties of kenaf/polyester composites. Int. J. Eng. Technol. 2011, 11, 127–131. [Google Scholar]
- Ku, H.; Wang, H.; Pattarachaiyakoop, N.; Trada, M. A review on the tensile properties of natural fiber reinforced polymer composites. Compos. Part B Eng. 2011, 42, 856–873. [Google Scholar] [CrossRef]
- Batu, T.; Lemu, H.; Sirhabizuh, B. Study of the Performance of Natural Fiber Reinforced Composites for Wind Turbine Blade Applications. Adv. Sci. Technol. Res. J. 2020, 14, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Sullins, T.; Pillay, S.; Komus, A.; Ning, H. Hemp fiber reinforced polypropylene composites: The effects of material treatments. Compos. Part B Eng. 2017, 114, 15–22. [Google Scholar] [CrossRef]
- Preece, R.A.; Dilaver, N.; Waldron, C.A.; Pallmann, P.; Thomas-Jones, E.; Gwilym, B.L.; Norvell, D.C.; Czerniecki, J.M.; Twine, C.P.; Bosanquet, D.C. A Systematic Review and Narrative Synthesis of Risk Prediction Tools Used to Estimate Mortality, Morbidity, and Other Outcomes Following Major Lower Limb Amputation. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Columbo, J.A.; Davies, L.; Kang, R.; Barnes, J.A.; Leinweber, K.A.; Suckow, B.D.; Goodney, P.P.; Stone, D.H. Patient Experience of Recovery After Major Leg Amputation for Arterial Disease. Vasc. Endovasc. Surg. 2018, 52, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Franklin, H.; Rajan, M.; Tseng, C.-L.; Pogach, L.; Sinha, A. Cost of lower-limb amputation in U.S. veterans with diabetes using health services data in fiscal years 2004 and 2010. J. Rehabil. Res. Dev. 2014, 51, 1325–1330. [Google Scholar] [CrossRef] [PubMed]
- McDonald, C.L.; Westcott-McCoy, S.; Weaver, M.R.; Haagsma, J.; Kartin, D. Global prevalence of traumatic non-fatal limb amputation. Prosthet. Orthot. Int. 2020, 45, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Dillingham, T.R.; Pezzin, L.E.; MacKenzie, E.J. Limb Amputation and Limb Deficiency: Epidemiology and Recent Trends in the United States. South. Med. J. 2002, 95, 875–883. [Google Scholar] [CrossRef] [PubMed]
- Calle-Pascual, A.L.; Redondo, M.J.; Ballesteros, M.; Martinez-Salinas, M.A.; Diaz, J.A.; De Matias, P.; Calle, J.R.; Gil, E.; Jimenez, M.; Serrano, F.J.; et al. Nontraumatic lower extremity amputations in diabetic and non-diabetic subjects in Madrid, Spain. Diabetes Metab. 1997, 23, 519–523. Available online: http://www.ncbi.nlm.nih.gov/pubmed/9496558 (accessed on 15 February 2022). [PubMed]
- Ebskov, B.; Ebskov, L. Major lower limb amputation in diabetic patients: Development during 1982 to 1993. Diabetologia 1996, 39, 1607–1610. [Google Scholar] [CrossRef] [PubMed]
- Tentolouris, N.; Al-Sabbagh, S.; Walker, M.G.; Boulton, A.J.M.; Jude, E.B. Mortality in Diabetic and Nondiabetic Patients After Amputations Performed From 1990 to 1995. Diabetes Care 2004, 27, 1598–1604. [Google Scholar] [CrossRef] [PubMed]
- Vázquez, E.; Wiecher, E. Los Amputados y su Rehabilitación; Academia Nacional de Medicina: Mexico City, Mexico, 2016. [Google Scholar]
- Carroll, K.; Rheinstein, J.; Pollard, E. Understanding and Selecting Prosthetic Feet, 4th ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2019. [Google Scholar] [CrossRef]
- Lawall Prosthetics & Orthotics. How Much Does a Prosthetic Leg Cost? The Cost of Prosthetic Legs. Available online: https://www.lawall.com/blog/how-much-does-a-prosthetic-leg-cost (accessed on 30 January 2023).
- Luxmed Protez. Prosthetic Leg Cost. Available online: https://luxmedprotez.com/en/prosthetic-leg-prices/ (accessed on 30 January 2023).
- Lavery, L.A.; van Houtum, W.H.; Armstrong, D.G.; Harkless, L.B.; Ashry, H.R.; Walker, S.C. Mortality following lower extremity amputation in minorities with diabetes mellitus. Diabetes Res. Clin. Pract. 1997, 37, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadística y Geografía. La Discapacidad en México, Datos al 2014. Versión 2017; INEGI Aguascalientes: Aguascalientes, Mexico, 2017. [Google Scholar]
- Irawan, A.P.; Soemardi, T.P.; Widjajalaksmi, K.; Reksoprodjo, A.H.S. Gait analysis of the prosthesis prototype made from the natural fiber reinforced composite. In Proceedings of the Apchi-Ergofuture 2010, Bali, Indonesia, 2–6 August 2010; pp. 37–43. [Google Scholar]
- Mankai, W.; Brahim, S.B.; Smida, B.B.; Cheikh, R.B.; Chafra, M. Mechanical behavior of a lower limb prosthetic socket made of natural fiber reinforced composite. J. Eng. Res. 2021, 9, 269–277. [Google Scholar] [CrossRef]
- Blatchford. Below Knee Prosthesis: Standard Features of a Below Knee Prosthesis. Available online: www.blatchford.co.uk/prosthetics/ (accessed on 3 February 2022).
- Abbod, E.A.; Resan, K.K. Review on the Interface Pressure Measurement for Below Knee Prosthetic Socket. IOP Conf. Ser. Mater. Sci. Eng. 2021, 1094, 012036. [Google Scholar] [CrossRef]
- Attwells, R.L.; Birrell, S.A.; Hooper, R.H.; Mansfield, N.J. Influence of carrying heavy loads on soldiers’ posture, movements and gait. Ergonomics 2006, 49, 1527–1537. [Google Scholar] [CrossRef]
- Birrell, S.A.; Haslam, R.A. The effect of military load carriage on 3-D lower limb kinematics and spatiotemporal parameters. Ergonomics 2009, 52, 1298–1304. [Google Scholar] [CrossRef]
- Hansen, A.H.; Childress, D.S. Effects of adding weight to the torso on roll-over characteristics of walking. J. Rehabil. Res. Dev. 2005, 42, 381. [Google Scholar] [CrossRef] [PubMed]
- Doyle, S.S.; Lemaire, E.D.; Besemann, M.; Dudek, N.L. Changes to level ground transtibial amputee gait with a weighted backpack. Clin. Biomech. 2014, 29, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Schnall, B.L.; Hendershot, B.D.; Bell, J.C.; Wolf, E.J. Kinematic analysis of males with transtibial amputation carrying military loads. J. Rehabil. Res. Dev. 2014, 51, 1505–1514. [Google Scholar] [CrossRef] [PubMed]
- Schnall, B.L.; Dearth, C.L.; Elrod, J.M.; Golyski, P.R.; Koehler-McNicholas, S.R.; Ray, S.F.; Hansen, A.H.; Hendershot, B.D. A more compliant prosthetic foot better accommodates added load while walking among Servicemembers with transtibial limb loss. J. Biomech. 2020, 98, 109395. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.C.; Ravji, K.; Key, J.J.; Mahler, D.B.; Blume, P.A.; Sumpio, B. Let Them Walk! Current Prosthesis Options for Leg and Foot Amputees. J. Am. Coll. Surg. 2008, 206, 548–560. [Google Scholar] [CrossRef] [PubMed]
- Gailey, R.S.; Nash, M.S.; Atchley, T.A.; Zilmer, R.M.; Moline-Little, G.R.; Morris-Cresswell, N.; Siebert, L.I. The effects of prosthesis mass on metabolic cost of ambulation in non-vascular trans-tibial amputees. Prosthet. Orthot. Int. 1997, 21, 9–16. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balaramakrishnan, T.M.; Natarajan, S.; Srinivasan, S. Roll-over shape of a prosthetic foot: A finite element evaluation and experimental validation. Med. Biol. Eng. Comput. 2020, 58, 2259–2270. [Google Scholar] [CrossRef] [PubMed]
- Malalli, C.S.; Ramji, B. Mechanical characterization of natural fiber reinforced polymer composites and their application in Prosthesis: A review. Mater. Today Proc. 2022, 62, 3435–3443. [Google Scholar] [CrossRef]
- Stokke, D.D.; Wu, Q.; Han, G. Wood and Natural Fiber Composites: An Overview. In Introduction to Wood and Natural Fiber Composites; Wiley: Hoboken, NJ, USA, 2013; pp. 1–17. [Google Scholar] [CrossRef]
- Callister, W.J. Fundamentals of Materials Science and Engineering: An Interactive eText, 5th ed.; John Wiley & Sons, Inc.: New York, NY, USA, 2001. [Google Scholar]
- Chung, D. Composite Materials. In Kirk-Othmer Encyclopedia of Chemical Technology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2015; Volume 82, no. 35; pp. 1–39. [Google Scholar] [CrossRef]
- Hsissou, R.; Seghiri, R.; Benzekri, Z.; Hilali, M.; Rafik, M.; Elharfi, A. Polymer composite materials: A comprehensive review. Compos. Struct. 2021, 262, 113640. [Google Scholar] [CrossRef]
- Tan, Q.; Wu, C.; Li, L.; Shao, W.; Luo, M. Nanomaterial-Based Prosthetic Limbs for Disability Mobility Assistance: A Review of Recent Advances. J. Nanomater. 2022, 2022, 3425297. [Google Scholar] [CrossRef]
- Yang, Y.; Boom, R.; Irion, B.; van Heerden, D.-J.; Kuiper, P.; de Wit, H. Recycling of composite materials. Chem. Eng. Process. Process. Intensif. 2012, 51, 53–68. [Google Scholar] [CrossRef]
- Otani, L.B.; Pereira, A.H.A.; Melo, J.D.D.; Amico, S.C. Elastic Moduli characterization of composites using the Impulse Excitation Technique. Mater. Sci. Eng. Phys. 2014, 36. [Google Scholar] [CrossRef]
- Ibrahim, I.D.; Jamiru, T.; E Sadiku, R.; Kupolati, W.K.; Agwuncha, S.C.; Ekundayo, G. The use of polypropylene in bamboo fibre composites and their mechanical properties—A review. J. Reinf. Plast. Compos. 2015, 34, 1347–1356. [Google Scholar] [CrossRef]
- Hale, D.K. The physical properties of composite materials. J. Mater. Sci. 1976, 11, 2105–2141. [Google Scholar] [CrossRef]
- Jones, R.M. Mechanics of Composite Materials; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- Yan, D.-X.; Ren, P.-G.; Pang, H.; Fu, Q.; Yang, M.-B.; Li, Z.-M. Efficient electromagnetic interference shielding of lightweight graphene/polystyrene composite. J. Mater. Chem. 2012, 22, 18772–18774. [Google Scholar] [CrossRef]
- Sahmaran, M.; Li, V.C.; Andrade, C. Corrosion Resistance Performance of Steel-Reinforced Engineered Cementitious Composite Beams. ACI Mater. J. 2008, 105, 243. [Google Scholar] [CrossRef] [PubMed]
- Budinski, K. Engineering Materials: Properties and Selection, 2nd ed.; Reston Publishing Company Inc.: Reston, VA, USA, 1983. [Google Scholar]
- Morton, J.; Ho, H.; Tsai, M.Y.; Farley, G.L. An Evaluation of The Iosipescu Specimen for Composite Materials Shear Property Measurement. Compos. Mater. 1992, 26, 708–750. [Google Scholar] [CrossRef]
- De Araújo, M. Natural and man-made fibres: Physical and mechanical properties. In Fibrous and Composite Materials for Civil Engineering Applications; Elsevier: Amsterdam, The Netherlands, 2011; pp. 3–28. [Google Scholar] [CrossRef]
- Husić, S.; Javni, I.; Petrović, Z.S. Thermal and mechanical properties of glass reinforced soy-based polyurethane composites. Compos. Sci. Technol. 2005, 65, 19–25. [Google Scholar] [CrossRef]
- Singh, T.J.; Samanta, S. Characterization of Kevlar Fiber and Its Composites: A Review. Mater. Today Proc. 2015, 2, 1381–1387. [Google Scholar] [CrossRef]
- Rezaei, F.; Yunus, R.; Ibrahim, N.A. Effect of fiber length on thermomechanical properties of short carbon fiber reinforced polypropylene composites. Mater. Des. 2009, 30, 260–263. [Google Scholar] [CrossRef]
- Davis, D.C.; Wilkerson, J.W.; Zhu, J.; Ayewah, D.O. Improvements in mechanical properties of a carbon fiber epoxy composite using nanotube science and technology. Compos. Struct. 2010, 92, 2653–2662. [Google Scholar] [CrossRef]
- Kozlowski, R.; Wladyka-Przybylak, M. Uses of Natural Fiber Reinforced Plastics. In Natural Fibers, Plastics and Composites; Springer: Boston, MA, USA, 2004; pp. 249–274. [Google Scholar] [CrossRef]
- Stokke, D.D.; Wu, Q.; Han, G. Natural Fiber and Plastic Composites. In Introduction to Wood and Natural Fiber Composites; Wiley: Hoboken, NJ, USA, 2013; pp. 237–285. [Google Scholar] [CrossRef]
- Thapliyal, D.; Verma, S.; Sen, P.; Kumar, R.; Thakur, A.; Tiwari, A.K.; Singh, D.; Verros, G.D.; Arya, R.K. Natural Fibers Composites: Origin, Importance, Consumption Pattern, and Challenges. J. Compos. Sci. 2023, 7, 506. [Google Scholar] [CrossRef]
- Tajvidi, M.; Takemura, A. Recycled Natural Fiber Polypropylene Composites: Water Absorption/Desorption Kinetics and Dimensional Stability. J. Polym. Environ. 2010, 18, 500–509. [Google Scholar] [CrossRef]
- Beg, M.; Pickering, K. Reprocessing of wood fibre reinforced polypropylene composites. Part II: Hygrothermal ageing and its effects. Compos. Part A Appl. Sci. Manuf. 2008, 39, 1565–1571. [Google Scholar] [CrossRef]
- Gogna, E.; Kumar, R.; Anurag; Sahoo, A.K.; Panda, A. A Comprehensive Review on Jute Fiber Reinforced Composites; Springer: Berlin/Heidelberg, Germany, 2019; pp. 459–467. [Google Scholar] [CrossRef]
- Wei, L.; McDonald, A.G.; Freitag, C.; Morrell, J.J. Effects of wood fiber esterification on properties, weatherability and biodurability of wood plastic composites. Polym. Degrad. Stab. 2013, 98, 1348–1361. [Google Scholar] [CrossRef]
- Kumar, A.P.; Singh, R.P.; Sarwade, B.D. Degradability of composites, prepared from ethylene–propylene copolymer and jute fiber under accelerated aging and biotic environments. Mater. Chem. Phys. 2005, 92, 458–469. [Google Scholar] [CrossRef]
- Bongarde, U.S.; Shinde, V.D. Review on natural fiber reinforcement polymer composites. Int. J. Eng. Sci. Innov. Technol. 2014, 3, 431–436. [Google Scholar]
- Chethan, N.; Nagesh, S.; Babu, L.S. Mechanical behaviour of Kenaf-Jute-E-glass reinforced hybrid polymer composites. Mater. Today Proc. 2020, 46, 4454–4459. [Google Scholar] [CrossRef]
- Lopresto, V.; Leone, C.; De Iorio, I. Mechanical characterisation of basalt fibre reinforced plastic. Compos. Part B Eng. 2011, 42, 717–723. [Google Scholar] [CrossRef]
- Bledzki, A.K.; Gassan, J. Composites reinforced with cellulose based fibres. Prog. Polym. Sci. 1999, 24, 221–274. [Google Scholar] [CrossRef]
- Vigneshwaran, S.; Sundarakannan, R.; John, K.; Johnson, R.D.J.; Prasath, K.A.; Ajith, S.; Arumugaprabu, V.; Uthayakumar, M. Recent advancement in the natural fiber polymer composites: A comprehensive review. J. Clean. Prod. 2020, 277, 124109. [Google Scholar] [CrossRef]
- Arabpour, A.; Shockravi, A.; Rezania, H.; Farahati, R. Investigation of anticorrosive properties of novel silane-functionalized polyamide/GO nanocomposite as steel coatings. Surf. Interfaces 2020, 18, 100453. [Google Scholar] [CrossRef]
- Zheng, S.; Bellido-Aguilar, D.A.; Hu, J.; Huang, Y.; Zhao, X.; Wang, Z.; Zeng, X.; Zhang, Q.; Chen, Z. Waterborne bio-based epoxy coatings for the corrosion protection of metallic substrates. Prog. Org. Coat. 2019, 136, 105265. [Google Scholar] [CrossRef]
- Ray, B. Temperature effect during humid ageing on interfaces of glass and carbon fibers reinforced epoxy composites. J. Colloid Interface Sci. 2006, 298, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Chung, D.; Mroz, C. Thermally conducting aluminum nitride polymer-matrix composites. Compos. Part A Appl. Sci. Manuf. 2001, 32, 1749–1757. [Google Scholar] [CrossRef]
- Davim, J.; Reis, P. Study of delamination in drilling carbon fiber reinforced plastics (CFRP) using design experiments. Compos. Struct. 2003, 59, 481–487. [Google Scholar] [CrossRef]
- Mukherjee, M.; Das, C.; Kharitonov, A. Fluorinated and oxyfluorinated short Kevlar fiber-reinforced ethylene propylene polymer. Polym. Compos. 2006, 27, 205–212. [Google Scholar] [CrossRef]
- Armstrong, D.P.; Chatterjee, K.; Ghosh, T.K.; Spontak, R.J. Form-stable phase-change elastomer gels derived from thermoplastic elastomer copolyesters swollen with fatty acids. Thermochim. Acta 2020, 686, 178566. [Google Scholar] [CrossRef]
- Senthilkumar, K.; Saba, N.; Chandrasekar, M.; Jawaid, M.; Rajini, N.; Alothman, O.Y.; Siengchin, S. Evaluation of mechanical and free vibration properties of the pineapple leaf fibre reinforced polyester composites. Constr. Build. Mater. 2018, 195, 423–431. [Google Scholar] [CrossRef]
- Hsissou, R.; Abbout, S.; Seghiri, R.; Rehioui, M.; Berisha, A.; Erramli, H.; Assouag, M.; Elharfi, A. Evaluation of corrosion inhibition performance of phosphorus polymer for carbon steel in [1 M] HCl: Computational studies (DFT, MC and MD simulations). J. Mater. Res. Technol. 2020, 9, 2691–2703. [Google Scholar] [CrossRef]
- Datsyuk, V.; Trotsenko, S.; Trakakis, G.; Boden, A.; Vyzas-Asimakopoulos, K.; Parthenios, J.; Galiotis, C.; Reich, S.; Papagelis, K. Thermal properties enhancement of epoxy resins by incorporating polybenzimidazole nanofibers filled with graphene and carbon nanotubes as reinforcing material. Polym. Test. 2019, 82, 106317. [Google Scholar] [CrossRef]
- Hsissou, R.; Elharfi, A. Rheological behavior of three polymers and their hybrid composites (TGEEBA/MDA/PN), (HGEMDA/MDA/PN) and (NGHPBAE/MDA/PN). J. King Saud Univ. Sci. 2020, 32, 235–244. [Google Scholar] [CrossRef]
- Parida, S.P.; Jena, P.C. Preparation of epoxy-glass composites with graphene and flyash filler. Mater. Today Proc. 2020, 26, 2328–2332. [Google Scholar] [CrossRef]
- Jin, X.; Guo, N.; You, Z.; Wang, L.; Wen, Y.; Tan, Y. Rheological properties and micro-characteristics of polyurethane composite modified asphalt. Constr. Build. Mater. 2019, 234, 117395. [Google Scholar] [CrossRef]
- Saba, N.; Jawaid, M. A review on thermomechanical properties of polymers and fibers reinforced polymer composites. J. Ind. Eng. Chem. 2018, 67, 1–11. [Google Scholar] [CrossRef]
- Dang, Z.-M.; Yuan, J.-K.; Zha, J.-W.; Zhou, T.; Li, S.-T.; Hu, G.-H. Fundamentals, processes and applications of high-permittivity polymer–matrix composites. Prog. Mater. Sci. 2012, 57, 660–723. [Google Scholar] [CrossRef]
- Pokharel, A.; Falua, K.J.; Babaei-Ghazvini, A.; Acharya, B. Biobased Polymer Composites: A Review. J. Compos. Sci. 2022, 6, 255. [Google Scholar] [CrossRef]
- Ortiz, P.; Wiekamp, M.; Vendamme, R.; Eevers, W. Bio-based epoxy resins from biorefinery by-products. BioResources 2019, 14, 3200–3209. [Google Scholar] [CrossRef]
- Thomas, J.; Patil, R. Enabling Green Manufacture of Polymer Products via Vegetable Oil Epoxides. Ind. Eng. Chem. Res. 2023, 62, 1725–1735. [Google Scholar] [CrossRef]
- Lascano, D.; Valcárcel, J.; Balart, R.; Quiles-Carrillo, L.; Boronat, T. Manufacturing of composite materials with high environmental efficiency using epoxy resin of renewable origin and permeable light cores for vacuum-assisted infusion molding. Ingenius 2020, 23, 62–73. [Google Scholar] [CrossRef]
- Sridhar, I.; Adie, P.; Ghista, D. Optimal design of customised hip prosthesis using fiber reinforced polymer composites. Mater. Des. 2010, 31, 2767–2775. [Google Scholar] [CrossRef]
- Guild, F.J.; Taylor, A.C.; Downes, J. Composite Materials. In Encyclopedia of Maritime and Offshore Engineering; John Wiley & Sons, Ltd.: Chichester, UK, 2017; Volume 82, no. 35; pp. 1–14. [Google Scholar] [CrossRef]
- Aslan, M.; Tufan, M.; Küçükömeroğlu, T. Tribological and mechanical performance of sisal-filled waste carbon and glass fibre hybrid composites. Compos. Part B Eng. 2018, 140, 241–249. [Google Scholar] [CrossRef]
- Assarar, M.; Zouari, W.; Sabhi, H.; Ayad, R.; Berthelot, J.-M. Evaluation of the damping of hybrid carbon–flax reinforced composites. Compos. Struct. 2015, 132, 148–154. [Google Scholar] [CrossRef]
- Campbell, A.I.; Sexton, S.; Schaschke, C.J.; Kinsman, H.; McLaughlin, B.; Boyle, M. Prosthetic limb sockets from plant-based composite materials. Prosthet. Orthot. Int. 2012, 36, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, V.; Bajpai, P.K.; Maheshwari, S. An Investigation on Wear and Dynamic Mechanical behavior of Jute/Hemp/Flax Reinforced Composites and Its Hybrids for Tribological Applications. Fibers Polym. 2018, 19, 403–415. [Google Scholar] [CrossRef]
- Essabir, H.; Bensalah, M.; Rodrigue, D.; Bouhfid, R.; Qaiss, A. Structural, mechanical and thermal properties of bio-based hybrid composites from waste coir residues: Fibers and shell particles. Mech. Mater. 2016, 93, 134–144. [Google Scholar] [CrossRef]
- Gu, Y.; Tan, X.; Yang, Z.; Li, M.; Zhang, Z. Hot compaction and mechanical properties of ramie fabric/epoxy composite fabricated using vacuum assisted resin infusion molding. Mater. Des. 2014, 56, 852–861. [Google Scholar] [CrossRef]
- Reddy, M.I.; Kumar, M.A.; Raju, C.R.B. Tensile and Flexural properties of Jute, Pineapple leaf and Glass Fiber Reinforced Polymer Matrix Hybrid Composites. Mater. Today Proc. 2018, 5, 458–462. [Google Scholar] [CrossRef]
- Jagannatha, T.D.; Harish, G. Mechanical properties of carbon/glass fiber reinforced epoxy hybrid polymer composites. Int. J. Mech. Eng. Robot. Res. 2015, 4, 131–137. [Google Scholar]
- Lee, B.-H.; Kim, H.-J.; Yu, W.-R. Fabrication of long and discontinuous natural fiber reinforced polypropylene biocomposites and their mechanical properties. Fibers Polym. 2009, 10, 83–90. [Google Scholar] [CrossRef]
- Rahman, A.; Rahman, M.Z.A.A.; Zaidi, A.M.A.; Rahman, I.A. Analysis of Comparison between Unconfined and Confined Condition of Foamed Concrete Under Uni-Axial Compressive Load. Am. J. Eng. Appl. Sci. 2010, 3, 68–72. [Google Scholar] [CrossRef][Green Version]
- Saba, N.; Paridah, M.; Abdan, K.; Ibrahim, N. Effect of oil palm nano filler on mechanical and morphological properties of kenaf reinforced epoxy composites. Constr. Build. Mater. 2016, 123, 15–26. [Google Scholar] [CrossRef]
- Sekaran, A.S.J.; Kumar, K.P.; Pitchandi, K. Evaluation on mechanical properties of woven aloevera and sisal fibre hybrid reinforced epoxy composites. Bull. Mater. Sci. 2015, 38, 1183–1193. [Google Scholar] [CrossRef]
- Shanmugam, D.; Thiruchitrambalam, M. Static and dynamic mechanical properties of alkali treated unidirectional continuous Palmyra Palm Leaf Stalk Fiber/jute fiber reinforced hybrid polyester composites. Mater. Des. 2013, 50, 533–542. [Google Scholar] [CrossRef]
- Shih, Y.-F.; Chang, W.-C.; Liu, W.-C.; Lee, C.-C.; Kuan, C.-S.; Yu, Y.-H. Pineapple leaf/recycled disposable chopstick hybrid fiber-reinforced biodegradable composites. J. Taiwan Inst. Chem. Eng. 2014, 45, 2039–2046. [Google Scholar] [CrossRef]
- Shrivastava, R.; Telang, A.; Rana, R.; Purohit, R. Mechanical Properties of Coir/G Lass Fiber Epoxy Resin Hybrid Composite. Mater. Today Proc. 2017, 4, 3477–3483. [Google Scholar] [CrossRef]
- Sreekumar, P.; Joseph, K.; Unnikrishnan, G.; Thomas, S. A comparative study on mechanical properties of sisal-leaf fibre-reinforced polyester composites prepared by resin transfer and compression moulding techniques. Compos. Sci. Technol. 2007, 67, 453–461. [Google Scholar] [CrossRef]
- Widhata, D.; Ismail, R.; Sulardjaka. Water Hyacinth (Eceng Gondok) As Fibre Reinforcement Composite for Prosthetics Socket. IOP Conf. Ser. Mater. Sci. Eng. 2019, 598, 012127. [Google Scholar] [CrossRef]
- Yan, L.; Chouw, N.; Yuan, X. Improving the mechanical properties of natural fibre fabric reinforced epoxy composites by alkali treatment. J. Reinf. Plast. Compos. 2012, 31, 425–437. [Google Scholar] [CrossRef]
- Yang, Z.; Peng, H.; Wang, W.; Liu, T. Crystallization behavior of poly(ε-caprolactone)/layered double hydroxide nanocomposites. J. Appl. Polym. Sci. 2010, 116, 2658–2667. [Google Scholar] [CrossRef]
- Ahmadijokani, F.; Shojaei, A.; Dordanihaghighi, S.; Jafarpour, E.; Mohammadi, S.; Arjmand, M. Effects of hybrid carbon-aramid fiber on performance of non-asbestos organic brake friction composites. Wear 2020, 452–453, 203280. [Google Scholar] [CrossRef]
- Yuan, H.; Zhang, S.; Lu, C.; He, S.; An, F. Improved interfacial adhesion in carbon fiber/polyether sulfone composites through an organic solvent-free polyamic acid sizing. Appl. Surf. Sci. 2013, 279, 279–284. [Google Scholar] [CrossRef]
- Hatti, P.S.; Somanakatti, A.B.; Rakshith, M. Investigation on tensile behavior of glass-fiber reinforced polymer matrix composite with varying orientations of fibers. Mater. Today Proc. 2021, 54, 137–140. [Google Scholar] [CrossRef]
- Puttaraju, D.; Hanumantharaju, H. Finite element analysis and validation of tensile properties of carbon fiber reinforced polymer matrix composites. Mater. Today Proc. 2022, 62, 2800–2807. [Google Scholar] [CrossRef]
- Cripps, D.; Searle, T.J.; Summerscales, J. Open Mold Techniques for Thermoset Composites. In Comprehensive Composite Materials Encyclopædia; Talreja, R., Månson, J.-A., Eds.; Polymer Matrix Composites; Elsevier Science: Oxford, UK, 2000; Volume 2, Chapter 21; pp. 737–761. [Google Scholar] [CrossRef]
- Barbero, E.J. Introduction to Composite Materials Design, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar]
- Rajak, D.K.; Pagar, D.D.; Kumar, R.; Pruncu, C.I. Recent progress of reinforcement materials: A comprehensive overview of composite materials. J. Mater. Res. Technol. 2019, 8, 6354–6374. [Google Scholar] [CrossRef]
- Oksman, K. High Quality Flax Fibre Composites Manufactured by the Resin Transfer Moulding Process. J. Reinf. Plast. Compos. 2001, 20, 621–627. [Google Scholar] [CrossRef]
- Rouison, D.; Sain, M.; Couturier, M. Resin transfer molding of natural fiber reinforced composites: Cure simulation. Compos. Sci. Technol. 2004, 64, 629–644. [Google Scholar] [CrossRef]
- Nawaz, A.; Islam, B.; Khattak, M.S.; Ali, L.; Saleem, U.; Ullah, A.; Ijaz, M.Z.; Mao, W.G. Polyester Usage in Manufacturing of Electrical and Mechanical Products and Assemblies. In Polyester—Production, Characterization and Innovative Applications; InTech Open: London, UK, 2018. [Google Scholar] [CrossRef]
- Razali, N.; Mansor, M.R.; Omar, G.; Kamarulzaman, S.A.F.S.; Zin, M.H.; Razali, N. Out-of-autoclave as a sustainable composites manufacturing process for aerospace applications. In Design for Sustainability; Elsevier: Amsterdam, The Netherlands, 2021; pp. 395–413. [Google Scholar] [CrossRef]
- Kassapoglou, C. Design and Analysis of Composite Structures; American Institute of Aeronautics and Astronautics (AIAA): Reston, VA, USA, 2010; ISBN 9781600867804. [Google Scholar]
- Zhao, X.; Li, K.; Wang, Y.; Tekinalp, H.; Richard, A.; Webb, E.; Ozcan, S. Bio-treatment of poplar via amino acid for interface control in biocomposites. Compos. Part B Eng. 2020, 199, 108276. [Google Scholar] [CrossRef]
- Taboga, P.; Grabowski, A.M. Axial and torsional stiffness of pediatric prosthetic feet. Clin. Biomech. 2017, 42, 47–54. [Google Scholar] [CrossRef] [PubMed]
- ISO 10328; Prosthethics—Structural Testing of Lower-Limb Prostheses—Requirements and Test Methods. ISO: Geneva, Switzerland, 2006.
- ISO 22675; Prosthetics—Testing of Ankle-Foot Devices and Foot Units—Requirements and Test Methods. ISO: Geneva, Switzerland, 2006.
- Colombo, C.; Marchesin, E.; Vergani, L.; Boccafogli, E.; Verni, G. Study of an ankle prosthesis for children: Adaptation of ISO 10328 and experimental tests. Procedia Eng. 2011, 10, 3510–3517. [Google Scholar] [CrossRef]
- Tabucol, J.; Brugo, T.M.; Povolo, M.; Leopaldi, M.; Oddsson, M.; Carloni, R.; Zucchelli, A. Structural FEA-Based Design and Functionality Verification Methodology of Energy-Storing-and-Releasing Prosthetic Feet. Appl. Sci. 2021, 12, 97. [Google Scholar] [CrossRef]
- Colombo, C.; Marchesin, E.; Vergani, L.; Boccafogli, E.; Verni, G. Design of an ankle prosthesis for swimming and walking. Procedia Eng. 2011, 10, 3503–3509. [Google Scholar] [CrossRef]
- Hamzah, M.; Gatta, A. Design of a Novel Carbon-Fiber Ankle-Foot Prosthetic using Finite Element Modeling. IOP Conf. Ser. Mater. Sci. Eng. 2018, 433, 012056. [Google Scholar] [CrossRef]
- Starker, F.; Blab, F.; Dennerlein, F.; Schneider, U. A Method for Sports Shoe Machinery Endurance Testing: Modification of ISO 22675 Prosthetic Foot Test Machine for Heel-to-toe Running Movement. Procedia Eng. 2014, 72, 405–410. [Google Scholar] [CrossRef]
- Santana, J.P.; Beltran, K.; Barocio, E.; Lopez-Avina, G.I.; Huegel, J.C. Development of a Low-Cost and Multi-Size Foot Prosthesis for Humanitarian Applications. In Proceedings of the 2018 IEEE Global Humanitarian Technology Conference (GHTC), Radnor, PA, USA, 12–15 October 2023; pp. 1–8. [Google Scholar]
- KS P 8403; Prosthetic Feet and Ankle Joints. Korean Industrial Standards: Seoul, Republic of Korea, 2017.
- Song, Y.; Choi, S.; Kim, S.; Roh, J.; Park, J.; Park, S.H.; Yoon, J. Performance Test for Laminated-Type Prosthetic Foot with Composite Plates. Int. J. Precis. Eng. Manuf. 2019, 20, 1777–1786. [Google Scholar] [CrossRef]
- Miller, K. Computational biomechanics for medicine. Int. J. Numer. Methods Biomed. Eng. 2011, 27, 345–346. [Google Scholar] [CrossRef]
- Simkins, D.C.C.; Alford, J.B.B. The Role of Computational Tools in Biomechanics. In Biomechanics of the Female Pelvic Floor; Elsevier: Amsterdam, The Netherlands, 2016; pp. 351–366. [Google Scholar] [CrossRef]
- Balaramakrishnan, T.M.; Natarajan, S.; Sujatha, S. Biomechanical design framework for prosthetic feet: Experimentally validated non-linear finite element procedure. Med. Eng. Phys. 2021, 92, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Parashar, S.; Chawla, V.K. Evaluation of fiber volume fraction of kenaf-coir-epoxy based green composite by finite element analysis. Mater. Today Proc. 2022, 50, 1265–1274. [Google Scholar] [CrossRef]
- Lian, W.; Yao, W. Fatigue life prediction of composite laminates by FEA simulation method. Int. J. Fatigue 2010, 32, 123–133. [Google Scholar] [CrossRef]
- Balasubramanian, K.; Rajeswari, N.; Vaidheeswaran, K. Analysis of mechanical properties of natural fibre composites by experimental with FEA. Mater. Today Proc. 2019, 28, 1149–1153. [Google Scholar] [CrossRef]
- Birrer, R.B.; Buzermanis, S.; DellaCorte, M.P.; Grisalfi, P.J. Biomechanics of Running; Medical Publishing Division: Oxford, UK, 2001. [Google Scholar]
- Rietman, H.S.; Postema, K.; Geertzen, J.H.B. Gait analysis in prosthetics: Opinions, ideas and conclusions. Prosthet. Orthot. Int. 2003, 27, 76–77. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balaramakrishnan, T.M.; Natarajan, S.; Sujatha, S. Design of a biomimetic sach foot: An experimentally verified finite element approach. J. Biomim. Biomater. Biomed. Eng. 2020, 45, 22–30. [Google Scholar] [CrossRef]
- Wittek, A.; Miller, K. Computational biomechanics for medical image analysis. In Handbook of Medical Image Computing and Computer Assisted Intervention; Elsevier: Amsterdam, The Netherlands, 2020; pp. 953–977. [Google Scholar] [CrossRef]
- Paknys, R. Finite Element Method. In Applied Frequency-Domain Electromagnetics; John Wiley & Sons, Ltd.: Chichester, UK, 2016; pp. 233–267. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).