Effect of Long Glass Fiber Orientations or a Short-Fiber-Reinforced Composite on the Fracture Resistance of Endodontically Treated Premolars
Abstract
1. Introduction
2. Materials and Methods
2.1. Tooth Selection
2.2. Access Cavity Preparations and Endodontic Treatment
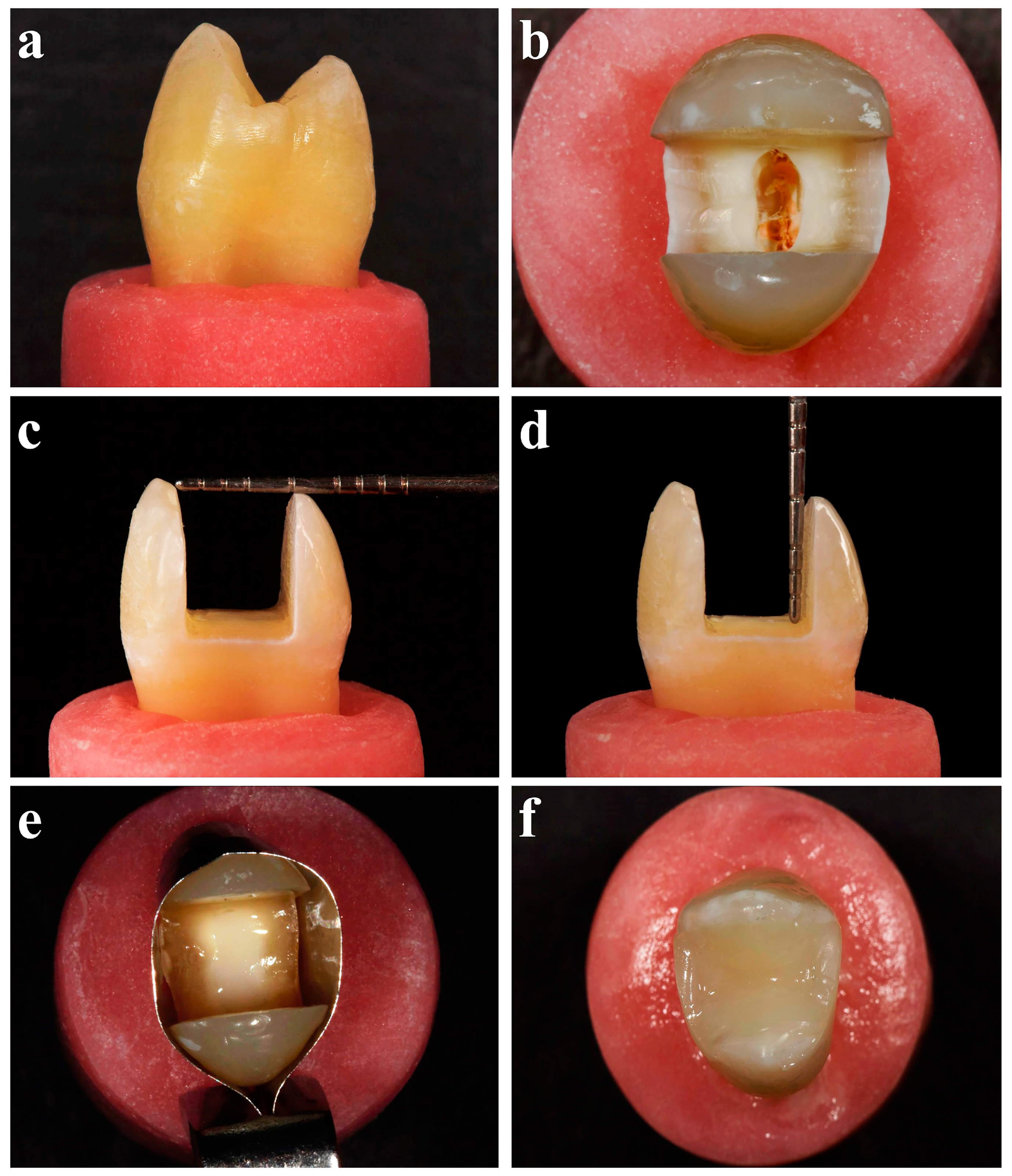
2.3. MOD Cavity Preparations
2.4. Adhesive Application
2.5. Resin Composite Group
2.6. Modified Transfixed Technique + Resin Composite Group
2.7. Circumferential Technique + Resin Composite Group
2.8. Cavity Floor Technique + Resin Composite Group
2.9. everX Flow™ (SFRC) + Resin Composite Group
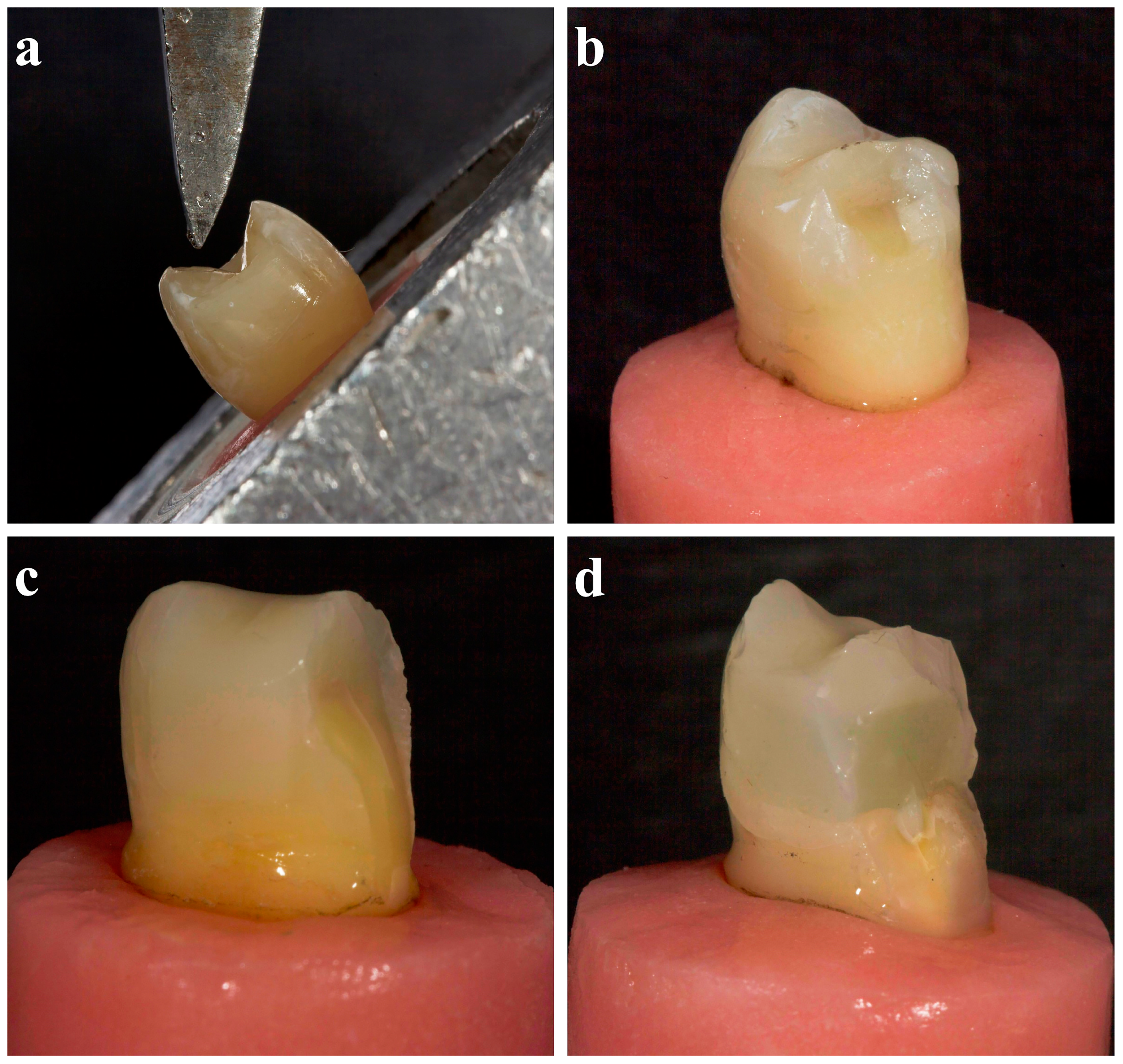
2.10. Fracture Strength Test
2.11. Statistical Analyses
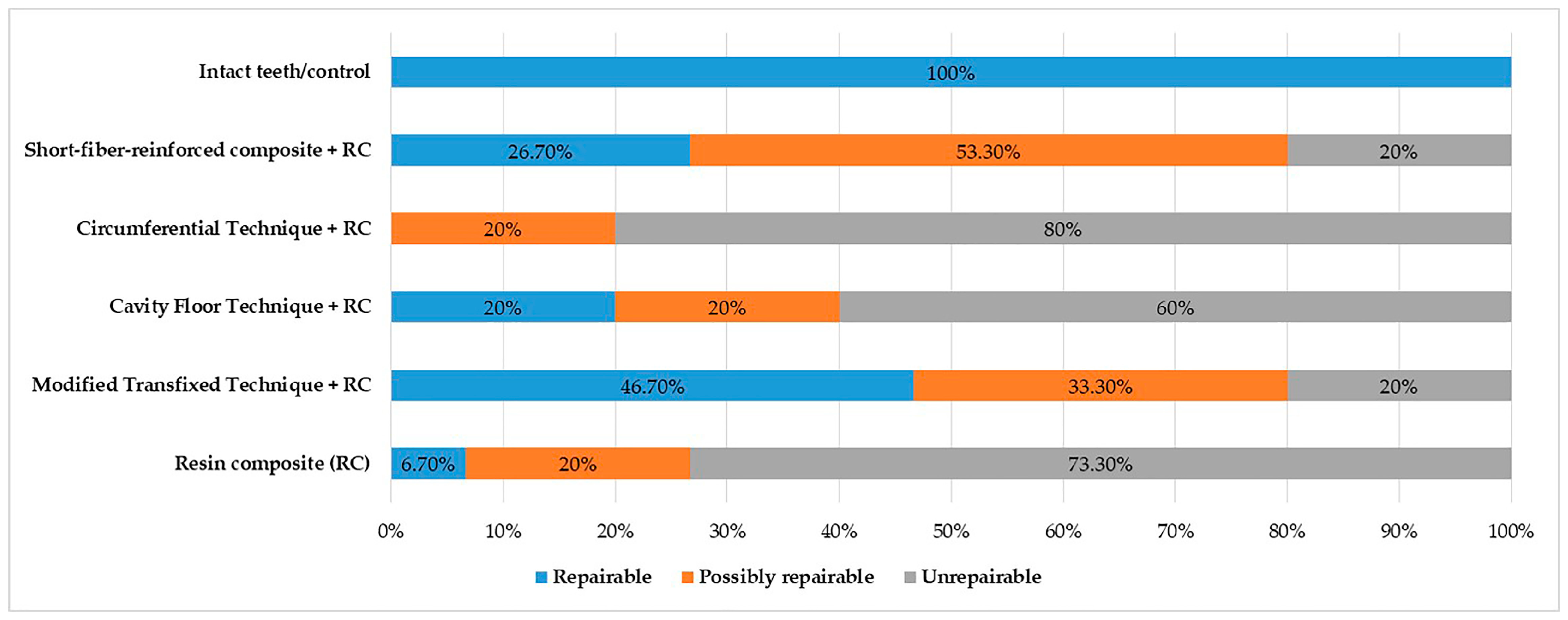
3. Results
4. Discussion
5. Conclusions
- Direct restorations using unidirectional long fibers with modified transfixed technique or flowable SFRCs increase the fracture strength of ETPs.
- In the resin composite restorations of endodontic, treated posterior teeth, bonding everStick®C&B between the buccal and palatal cusps with the modified transfixed technique could be a conservative treatment option to improve the decreasing fracture strength.
- From a clinical perspective, using flowable SFRCs was easier and less time-consuming compared with applying long fiber orientations.
- everStick®C&B bonded between cusps horizontally or everX Flow™ applied as a dentin replacement material improves the fracture pattern of direct resin composite restorations.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ElAyouti, A.; Serry, M.I.; Geis-Gerstorfer, J.; Löst, C. Influence of cusp coverage on the fracture resistance of premolars with endodontic access cavities. Int. Endod. J. 2011, 44, 543–549. [Google Scholar] [CrossRef]
- Kishen, A. Biomechanics of fractures in endodontically treated teeth. Endod. Top. 2015, 33, 3–13. [Google Scholar] [CrossRef]
- Tang, W.; Wu, Y.; Smales, R.J. Identifying and reducing risks for potential fractures in endodontically treated teeth. J. Endod. 2010, 36, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Eapen, A.M.; Amirtharaj, L.V.; Sanjeev, K.; Mahalaxmi, S. Fracture resistance of endodontically treated teeth restored with 2 different fiber-reinforced composite and 2 conventional composite resin core buildup materials: An in vitro study. J. Endod. 2017, 43, 1499–1504. [Google Scholar] [CrossRef]
- Plotino, G.; Buono, L.; Grande, N.M.; Lamorgese, V.; Somma, F. Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J. Prosthet. Dent. 2008, 99, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.; Xavier, T.; Noritomi, P.; Saavedra, G.; Borges, A. The influence of elastic modulus of inlay materials on stress distribution and fracture of premolars. Oper. Dent. 2014, 39, E160–E170. [Google Scholar] [CrossRef][Green Version]
- Al-Omiri, M.K.; Mahmoud, A.A.; Rayyan, M.R.; Abu-Hammad, O. Fracture resistance of teeth restored with post-retained restorations: An overview. J. Endod. 2010, 36, 1439–1449. [Google Scholar] [CrossRef] [PubMed]
- Karzoun, W.; Abdulkarim, A.; Samran, A.; Kern, M. Fracture strength of endodontically treated maxillary premolars supported by a horizontal glass fiber post: An in vitro study. J. Endod. 2015, 41, 907–912. [Google Scholar] [CrossRef]
- Peroz, I.; Blankenstein, F.; Lange, K.P.; Naumann, M. Restoring endodontically treated teeth with posts and cores—A review. Quintessence Int. 2005, 36, 737–746. [Google Scholar]
- Capriotti, L.; Greco, K.; Paolone, G.; Sberna, M.T.; Cantatore, G. Removal of fiber posts during endodontic retreatments using ultrasonic tips: A comparison between two different endodontic fiber posts. G. Ital. Endod. 2018, 32, 47–50. [Google Scholar] [CrossRef]
- Hofsteenge, J.W.; Scholtanus, J.D.; Özcan, M.; Nolte, I.M.; Cune, M.S.; Gresnigt, M.M.M. Clinical longevity of extensive direct resin composite restorations after amalgam replacement with a mean follow-up of 15 years. J. Dent. 2023, 130, 104409. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, Q.; Meng, X.; Ye, Y.; Feng, D.; Xue, J.; Wang, H.; Huang, H.; Wang, M.; Wang, J. Rheological and Mechanical Properties of Resin-Based Materials Applied in Dental Restorations. Polymers 2021, 13, 2975. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, I.; Otsuki, M.; Sadr, A.; Nomura, T.; Kishikawa, R.; Tagami, J. Effect of filler content of flowable composites on resin-cavity interface. Dent. Mater. J. 2009, 28, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, P.H.; Catelan, A.; Albuquerque Guedes, A.P.; Umeda Suzuki, T.Y.; de Lima Godas, A.G.; Fraga Briso, A.L.; Bedran-Russo, A.K. Effect of thermocycling on roughness of nanofill, microfill and microhybrid composites. Acta Odontol. Scand. 2015, 73, 176–181. [Google Scholar] [CrossRef]
- Jang, J.; Han, S. Mechanical properties of glass-fibre mat/PMMA functionally gradient composite. Compos. A Appl. Sci. Manuf. 1999, 30, 1045–1053. [Google Scholar] [CrossRef]
- Szabó, V.T.; Szabó, B.; Barcsayné-Tátrai, N.; Mészáros, C.; Braunitzer, G.; Szabó, B.P.; Lassila, L.; Garoushi, S.; Fráter, M. Fatigue Resistance of Dissected Lower First Molars Restored with Direct Fiber-Reinforced Bridges—An In Vitro Pilot Study. Polymers 2023, 15, 1343. [Google Scholar] [CrossRef] [PubMed]
- Sáry, T.; Garoushi, S.; Braunitzer, G.; Alleman, D.; Volom, A.; Fráter, M. Fracture behaviour of MOD restorations reinforced by various fibre-reinforced techniques—An in vitro study. J. Mech. Behav. Biomed. Mater. 2019, 98, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Mergulhão, V.A.; de Mendonça, L.S.; de Albuquerque, M.S.; Braz, R. Fracture Resistance of Endodontically Treated Maxillary Premolars Restored With Different Methods. Oper. Dent. 2019, 44, 1–11. [Google Scholar] [CrossRef]
- Deliperi, S.; Alleman, D.; Rudo, D. Stress-reduced Direct Composites for the Restoration of Structurally Compromised Teeth: Fiber Design According to the “Wallpapering” Technique. Oper. Dent. 2017, 42, 233–243. [Google Scholar] [CrossRef]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of large MOD restorations: Composite resin inlays vs. short fiber-reinforced direct restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef]
- Huang, Q.; Qin, W.; Garoushi, S.; He, J.; Lin, Z.; Liu, F.; Vallittu, P.K.; Lassila, L.V.J. Physicochemical properties of discontinuous S2-glass fiber reinforced resin composite. Dent. Mater. J. 2018, 37, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K. High-aspect ratio fillers: Fiber-reinforced composites and their anisotropic properties. Dent. Mater. 2015, 31, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Milani, T. Short-fiber Reinforced MOD Restorations of Molars with Severely Undermined Cusps. J. Adhes. Dent. 2023, 25, 99–106. [Google Scholar] [PubMed]
- Soto-Cadena, S.L.; Zavala-Alonso, N.V.; Cerda-Cristerna, B.I.; Ortiz-Magdaleno, M. Effect of short fiber-reinforced composite combined with polyethylene fibers on fracture resistance of endodontically treated premolars. J. Prosthet. Dent. 2023, 129, 598.e1–598.e10. [Google Scholar] [CrossRef] [PubMed]
- Akman, S.; Akman, M.; Eskitascioglu, G.; Belli, S. Influence of several fibre-reinforced composite restoration techniques on cusp movement and fracture strength of molar teeth. Int. Endod. J. 2011, 44, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Gómez, J.F.; Ortiz-Magdaleno, M.; Zavala-Alonso, N.V. Effect of polyethylene fiber orientation on fracture resistance of endodontically treated premolars. J. Prosthet. Dent. 2024, 131, 92.e1–92.e8. [Google Scholar] [CrossRef] [PubMed]
- Ellakwa, A.E.; Shortall, A.C.; Marquis, P.M. Influence of fiber type and wetting agent on the flexural properties of an indirect fiber reinforced composite. J. Prosthet. Dent. 2002, 88, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Arhun, N.; Arman, A. Fiber-reinforced technology in multidisciplinary chairside approaches. Indian J. Dent. Res. 2008, 19, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Kolbeck, C.; Rosentritt, M.; Behr, M.; Lang, R.; Handel, G. In vitro study of fracture strength and marginal adaptation of polyethylene fibre-reinforced composite versus glass fibre-reinforced composite fixed partial dentures. J. Oral. Rehabil. 2002, 29, 668–674. [Google Scholar] [CrossRef]
- de Mesquita, C.B.; Melara, R.; Luisi, S.B.; Burnett, L.H., Jr.; de Melo, T.A.F. Influence of dental crown topography on fracture resistance of premolars with MOD preparation and subjected to different restorative protocols. Aust. Endod. J. 2021, 47, 493–498. [Google Scholar] [CrossRef]
- Abdulrab, S.; Geerts, G.; Al-Maweri, S.A.; Alhajj, M.N.; Alhadainy, H.; Ba-Hattab, R. The influence of horizontal glass fiber posts on fracture strength and fracture pattern of endodontically treated teeth: A systematic review and meta-analysis of in vitro studies. J. Prosthodont. 2023, 32, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Naik, A.; de Ataide, I.N.; Fernandes, M. Fracture Resistance of Endodontically Treated Premolars Using Nanohybrid Composite, Fiber-Reinforced Composite, Horizontal Glass Fiber Posts, and Ceramic Inlays: An In Vitro Study. J. Endod. 2023, 49, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Burke, F.J. Tooth fracture in vivo and in vitro. J. Dent. 1992, 20, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Patil, D.B.; Reddy, E.R.; Rani, S.T.; Kadge, S.S.; Patil, S.D.; Madki, P. Evaluation of stress in three different fiber posts with two-dimensional finite element analysis. J. Indian Soc. Pedod. Prev. Dent. 2021, 39, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, V.S.; Shah, A.; Kapoor, S. Effect of fiber orientation and placement on fracture resistance of large class II mesio-occluso-distal cavities in maxillary premolars: An in vitro study. J. Conserv. Dent. 2022, 25, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Abdulamir, S.W.; Majeed, M.A. Fracture Resistance of Endodontically Treated Maxillary Premolar Teeth Restored with Wallpapering Technique: A Comparative In Vitro Study. Int. J. Dent. 2023, 2023, 6159338. [Google Scholar] [CrossRef] [PubMed]
- Fildisi, M.A.; Eliguzeloglu Dalkilic, E. The effect of fiber insertion on fracture strength and fracture modes in endocrown and overlay restorations. Microsc. Res. Tech. 2022, 85, 1799–1807. [Google Scholar] [CrossRef]
- Jafari Navimipour, E.; Ebrahimi Chaharom, M.E.; Alizadeh Oskoee, P.; Mohammadi, N.; Bahari, M.; Firouzmandi, M. Fracture Resistance of Endodontically-treated Maxillary Premolars Restored with Composite Resin along with Glass Fiber Insertion in Different Positions. J. Dent. Res. Dent. Clin. Dent. Prospect. 2012, 6, 125–130. [Google Scholar]
- Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Fracture resistance of short, randomly oriented, glass fiber-reinforced composite premolar crowns. Acta Biomater. 2007, 3, 779–784. [Google Scholar] [CrossRef]
- Fráter, M.; Sáry, T.; Vincze-Bandi, E.; Volom, A.; Braunitzer, G.; Szabó, P.B.; Garoushi, S.; Forster, A. Fracture Behavior of Short Fiber-Reinforced Direct Restorations in Large MOD Cavities. Polymers 2021, 13, 2040. [Google Scholar] [CrossRef]
- Garoushi, S.; Akbaşak-Sungur, A.Ö.; Erkut, S.; Vallittu, P.K.; Uctasli, S.; Lassila, L. Evaluation of fracture behavior in short fiber-reinforced direct and indirect overlay restorations. Clin. Oral. Investig. 2023, 27, 5449–5458. [Google Scholar] [CrossRef] [PubMed]
- ElAziz, R.H.A.; ElAziz, S.A.A.; ElAziz, P.M.A.; Frater, M.; Vallittu, P.K.; Lassila, L.; Garoushi, S. Clinical evaluation of posterior flowable short fiber-reinforced composite restorations without proximal surface coverage. Odontology, 2024; epub ahead of print. [Google Scholar]

| Material | Manufacturer | Fillers | Matrix |
|---|---|---|---|
| G-aenial Universal Injectable, flowable composite | GC Corporation, Tokyo, Japan (Lot number: 2103192) | Silicon dioxide (SiO2), barium glass, 69 wt%, 50 vol% | UDMA, Bis-MEPP, TEGDMA, |
| everX Flow™, short-fiber-reinforced composite | GC Corporation, Tokyo, Japan (Lot number: 2106221) | Micrometer scale glass fiber filler, barium glass, 70 wt%, 46 vol% | Bis-EMA, TEGDMA, UDMA, |
| Scotchbond Universal Plus Adhesive | 3M Deutschland GmbH, Neuss, Germany (Lot number: 7730432) | Bis-GMA, 10-MDP, 2-HEMA, Vitrebond copolymer, ethanol, water, initiators, fillers methacrylate, water | |
| everStick®C&B fibers | GC Corporation, Tokyo, Japan (Lot number: 2210201) | Silanated unidirectional glass fibers | PMMA, Bis-GMA |
| Groups | Mean ± sd (N) | Test Statistic | p |
|---|---|---|---|
| Resin composite (RC) | 443.511 ± 19.17 a | 135.383 | <0.001 |
| Modified transfixed technique + RC | 496.58 ± 19.67 b | ||
| Cavity floor technique + RC | 404.623 ± 19.21 c | ||
| Circumferential technique + RC | 442.835 ± 31.89 a | ||
| Short-fiber-reinforced composite + RC | 469.62 ± 19.56 d | ||
| Intact teeth/control | 599.336 ± 22.9 e | ||
| Total | 476.084 ± 65.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hazar, E.; Hazar, A. Effect of Long Glass Fiber Orientations or a Short-Fiber-Reinforced Composite on the Fracture Resistance of Endodontically Treated Premolars. Polymers 2024, 16, 1289. https://doi.org/10.3390/polym16091289
Hazar E, Hazar A. Effect of Long Glass Fiber Orientations or a Short-Fiber-Reinforced Composite on the Fracture Resistance of Endodontically Treated Premolars. Polymers. 2024; 16(9):1289. https://doi.org/10.3390/polym16091289
Chicago/Turabian StyleHazar, Ecehan, and Ahmet Hazar. 2024. "Effect of Long Glass Fiber Orientations or a Short-Fiber-Reinforced Composite on the Fracture Resistance of Endodontically Treated Premolars" Polymers 16, no. 9: 1289. https://doi.org/10.3390/polym16091289
APA StyleHazar, E., & Hazar, A. (2024). Effect of Long Glass Fiber Orientations or a Short-Fiber-Reinforced Composite on the Fracture Resistance of Endodontically Treated Premolars. Polymers, 16(9), 1289. https://doi.org/10.3390/polym16091289






