Evaluation of Effect of Different Insertion Speeds and Torques on Implant Placement Condition and Removal Torque in Polyurethane Dense D1 Bone Model
Abstract
1. Introduction
2. Materials and Methods
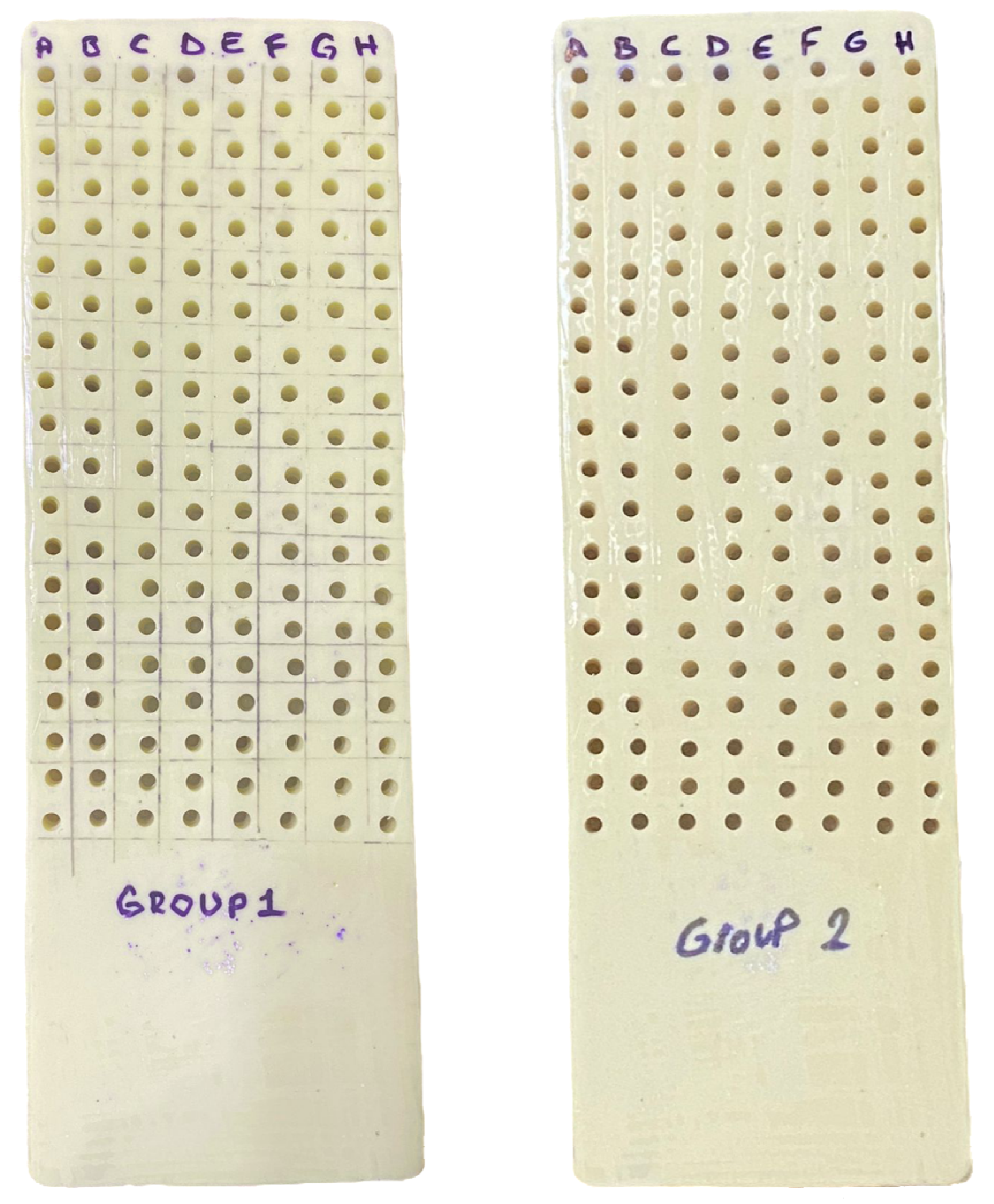
2.1. Study Groups
2.2. Implant Socket Preparation Protocol
2.3. Statistical Analyses
3. Results
3.1. Intra-Group Implant Removal Torque Assessments
3.2. Inter-Group Implant Removal Torque Assessments
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Jenny, G.; Jauernik, J.; Bierbaum, S.; Bigler, M.; Grätz, K.W.; Rücker, M.; Stadlinger, B. A Systematic Review and Meta-Analysis on the Influence of Biological Implant Surface Coatings on Periimplant Bone Formation. J. Biomed. Mater. Res. Part A 2016, 104, 2898–2910. [Google Scholar] [CrossRef] [PubMed]
- Leong, D.; Yap, A.; Tay, J.; Tan, W. A Patient’s Guide to Dental Implants, 1st ed.; Implantdontics Pte Ltd.; The Oral Maxillofacial Practice Pte Ltd.; MyoHealth Asia Pte Ltd.: Singapore, 2006. [Google Scholar]
- Mathieu, V.; Vayron, R.; Richard, G.; Lambert, G.; Naili, S.; Meningaud, J.-P.; Haiat, G. Biomechanical Determinants of the Stability of Dental Implants: Influence of the Bone–Implant Interface Properties. J. Biomech. 2014, 47, 3–13. [Google Scholar] [CrossRef]
- Zohrabian, V.M.; Sonick, M.; Hwang, D.; Abrahams, J.J. Dental Implants; Elsevier: Amsterdam, The Netherlands, 2015; Volume 36, pp. 415–426. [Google Scholar]
- Diz, P.; Scully, C.; Sanz, M. Dental Implants in the Medically Compromised Patient. J. Dent. 2013, 41, 195–206. [Google Scholar] [CrossRef]
- Paquette, D.W.; Brodala, N.; Williams, R.C. Risk Factors for Endosseous Dental Implant Failure. Dent. Clin. 2006, 50, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Berglundh, T.; Abrahamsson, I.; Albouy, J.; Lindhe, J. Bone Healing at Implants with a Fluoride-modified Surface: An Experimental Study in Dogs. Clin. Oral Implants Res. 2007, 18, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Seth, S.; Kalra, P. Effect of Dental Implant Parameters on Stress Distribution at Bone-Implant Interface. Int. J. Sci. Res. 2013, 2, 121–124. [Google Scholar]
- Sullivan, R.M. Implant Dentistry and the Concept of Osseointegration: A Historical Perspective. J. Calif. Dent. Assoc. 2001, 29, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Gulsahi, A. Bone Quality Assessment for Dental Implants; InTech: Rijeka, Croatia, 2011; pp. 437–452. [Google Scholar]
- Tinsley, D.; Watson, C.; Ogden, A. A Survey of UK Centres on Implant Failures. J. Oral Rehabil. 1999, 26, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Turkyilmaz, I.; Tözüm, T.; Tumer, C. Bone Density Assessments of Oral Implant Sites Using Computerized Tomography. J. Oral Rehabil. 2007, 34, 267–272. [Google Scholar] [CrossRef]
- Farré-Pagès, N.; Augé-Castro, M.L.; Alaejos-Algarra, F.; Mareque-Bueno, J.; Ferrés-Padró, E.; Hernández-Alfaro, F. Relation between Bone Density and Primary Implant Stability. Med. Oral Patol. Oral Cir. Bucal. 2011, 16, e62–e67. [Google Scholar] [CrossRef]
- Shalabi, M.M.; Wolke, J.G.; Jansen, J.A. The Effects of Implant Surface Roughness and Surgical Technique on Implant Fixation in an In Vitro Model. Clin. Oral Implants Res. 2006, 17, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Stimmelmayr, M.; Beuer, F.; Edelhoff, D.; Güth, J. Implant Impression Techniques for the Edentulous Jaw: A Summary of Three Studies. J. Prosthodont. 2016, 25, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Seifert, L.B.; Schnurr, B.; Herrera-Vizcaino, C.; Begic, A.; Thieringer, F.; Schwarz, F.; Sader, R. 3D-printed Patient Individualised Models vs Cadaveric Models in an Undergraduate Oral and Maxillofacial Surgery Curriculum: Comparison of Student’s Perceptions. Eur. J. Dent. Educ. 2020, 24, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Gao, Y.; Zhao, J.; Yuan, L.; Li, C.; Liu, Z.; Hou, Z. A Mild Method for Surface-Grafting PEG onto Segmented Poly (Ester-Urethane) Film with High Grafting Density for Biomedical Purpose. Polymers 2018, 10, 1125. [Google Scholar] [CrossRef]
- Xu, W.; Xiao, M.; Yuan, L.; Zhang, J.; Hou, Z. Preparation, Physicochemical Properties and Hemocompatibility of Biodegradable Chitooligosaccharide-Based Polyurethane. Polymers 2018, 10, 580. [Google Scholar] [CrossRef]
- Szperlich, P.; Toroń, B. An Ultrasonic Fabrication Method for Epoxy Resin/SbSI Nanowire Composites, and Their Application in Nanosensors and Nanogenerators. Polymers 2019, 11, 479. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Guirado, J.L.C.; Bettach, R.; Fabbro, M.D.; Martínez, C.P.; Shibli, J.A. Evaluation of the Insertion Torque, Implant Stability Quotient and Drilled Hole Quality for Different Drill Design: An In Vitro Investigation. Clin. Oral Implants Res. 2018, 29, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Delgado-Ruiz, R.A.; Sacks, D.; Calvo-Guirado, J.L. Influence of the Implant Diameter and Bone Quality on the Primary Stability of Porous Tantalum Trabecular Metal Dental Implants: An In Vitro Biomechanical Study. Clin. Oral Implants Res. 2018, 29, 649–655. [Google Scholar] [CrossRef]
- Comuzzi, L.; Iezzi, G.; Piattelli, A.; Tumedei, M. An in Vitro Evaluation, on Polyurethane Foam Sheets, of the Insertion Torque (IT) Values, Pull-out Torque Values, and Resonance Frequency Analysis (RFA) of Nanoshort Dental Implants. Polymers 2019, 11, 1020. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The Insertion Torque-Depth Curve Integral as a Measure of Implant Primary Stability: An in Vitro Study on Polyurethane Foam Blocks. J. Prosthet. Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef]
- Glauser, R.; Sennerby, L.; Meredith, N.; Rée, A.; Lundgren, A.; Gottlow, J.; Hämmerle, C.H. Resonance Frequency Analysis of Implants Subjected to Immediate or Early Functional Occlusal Loading: Successful vs. Failing Implants. Clin. Oral Implants Res. 2004, 15, 428–434. [Google Scholar] [CrossRef]
- Kittur, N.; Oak, R.; Dekate, D.; Jadhav, S.; Dhatrak, P. Dental Implant Stability and Its Measurements to Improve Osseointegration at the Bone-Implant Interface: A Review. Mater. Today Proc. 2021, 43, 1064–1070. [Google Scholar] [CrossRef]
- Ikumi, N.; Tsutsumi, S. Assessment of Correlation between Computerized Tomography Values of the Bone and Cutting Torque Values at Implant Placement: A Clinical Study. Int. J. Oral Maxillofac. Implants 2005, 20, 253. [Google Scholar]
- Atsumi, M.; Park, S.-H.; Wang, H.-L. Methods Used to Assess Implant Stability: Current Status. Int. J. Oral Maxillofac. Implants 2007, 22, 743. [Google Scholar]
- Campos, F.E.; Gomes, J.B.; Marin, C.; Teixeira, H.S.; Suzuki, M.; Witek, L.; Zanetta-Barbosa, D.; Coelho, P.G. Effect of Drilling Dimension on Implant Placement Torque and Early Osseointegration Stages: An Experimental Study in Dogs. J. Oral Maxillofac. Surg. 2012, 70, e43–e50. [Google Scholar] [CrossRef]
- Goswami, M.; Kumar, M.; Vats, A.; Bansal, A. Evaluation of Dental Implant Insertion Torque Using a Manual Ratchet. Med. J. Armed Forces India 2015, 71, S327–S332. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yang, B.; Irastorza-Landa, A.; Heuberger, P.; Ploeg, H.-L. Effect of Insertion Factors on Dental Implant Insertion Torque/Energy-Experimental Results. J. Mech. Behav. Biomed. Mater. 2020, 112, 103995. [Google Scholar] [CrossRef]
- Farronato, D.; Manfredini, M.; Stocchero, M.; Caccia, M.; Azzi, L.; Farronato, M. Influence of Bone Quality, Drilling Protocol, Implant Diameter/Length on Primary Stability: An In Vitro Comparative Study on Insertion Torque and Resonance Frequency Analysis. J. Oral Implantol. 2020, 46, 182–189. [Google Scholar] [CrossRef]
- Bassi, M.A.; Arosio, P.; Alessio Di Stefano, D. Evaluation of Peri-Implant Bone Stress on D1 Bone Using a Computerized Torque-Measuring Implant Motor: A Study on Photoelastic Resin Blocks. Int. J. Oral Maxillofac. Implants 2018, 33, 770. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.-T.; Jin, J.; Mangal, U.; Lee, K.-J.; Kim, K.-M.; Choi, S.-H.; Kwon, J.-S. Primary Stability of Orthodontic Titanium Miniscrews due to Cortical Bone Density and Re-Insertion. Materials 2020, 13, 4433. [Google Scholar] [CrossRef]
- Fanali, S.; Tumedei, M.; Pignatelli, P.; Inchingolo, F.; Pennacchietti, P.; Pace, G.; Piattelli, A. Implant Primary Stability with an Osteocondensation Drilling Protocol in Different Density Polyurethane Blocks. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; Pontes, A.E.; Piattelli, A.; Iezzi, G. Primary Stability of Dental Implants in Low-Density (10 and 20 Pcf) Polyurethane Foam Blocks: Conical vs Cylindrical Implants. Int. J. Environ. Res. Public Health 2020, 17, 2617. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.E. Bone Density: A Key Determinant for Clinical Success. Contemp. Implant Dent. 1999, 109–118. [Google Scholar]
- Puisys, A.; Schlee, M.; Linkevicius, T.; Petrakakis, P.; Tjaden, A. Photo-Activated Implants: A Triple-Blinded, Split-Mouth, Randomized Controlled Clinical Trial on the Resistance to Removal Torque at Various Healing Intervals. Clin. Oral Investig. 2020, 24, 1789–1799. [Google Scholar] [CrossRef]
- Nary Filho, H.; Calvo Guirado, J.L.; Matsumoto, M.A.; Bresaola, M.D.; Aur, R. Biomechanical Evaluation of Resistance to Insertion Torque of Different Implant Systems and Insertion Driver Types. Implant Dent. 2015, 24, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Baldi, D.; Lombardi, T.; Colombo, J.; Cervino, G.; Perinetti, G.; Di Lenarda, R.; Stacchi, C. Correlation between Insertion Torque and Implant Stability Quotient in Tapered Implants with Knife-Edge Thread Design. BioMed Res. Int. 2018, 2018, 7201093. [Google Scholar] [CrossRef] [PubMed]
- Khayat, P.G.; Milliez, S.N. Prospective Clinical Evaluation of 835 Multithreaded Tapered Screw-Vent Implants: Results after Two Years of Functional Loading. J. Oral Implantol. 2007, 33, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Aspenberg, P.; Goodman, S.; Toksvig-Larsen, S.; Ryd, L.; Albrektsson, T. Intermittent Micromotion Inhibits Bone Ingrowth: Titanium Implants in Rabbits. Acta Orthop. Scand. 1992, 63, 141–145. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-L.; Hsu, J.-T.; Fuh, L.-J.; Tu, M.-G.; Ko, C.-C.; Shen, Y.-W. Bone Stress and Interfacial Sliding Analysis of Implant Designs on an Immediately Loaded Maxillary Implant: A Non-Linear Finite Element Study. J. Dent. 2008, 36, 409–417. [Google Scholar] [CrossRef]
- Brink, J.; Meraw, S.J.; Sarment, D.P. Influence of Implant Diameter on Surrounding Bone. Clin. Oral Implants Res. 2007, 18, 563–568. [Google Scholar] [CrossRef]
- Chun, H.; Cheong, S.; Han, J.; Heo, S.; Chung, J.; Rhyu, I.; Choi, Y.; Baik, H.; Ku, Y.; Kim, M. Evaluation of Design Parameters of Osseointegrated Dental Implants Using Finite Element Analysis. J. Oral Rehabil. 2002, 29, 565–574. [Google Scholar] [CrossRef] [PubMed]
- McCullough, J.J.; Klokkevold, P.R. The Effect of Implant Macro-thread Design on Implant Stability in the Early Post-operative Period: A Randomized, Controlled Pilot Study. Clin. Oral Implants Res. 2017, 28, 1218–1226. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T., Jr.; Miller, R.; Trushkowsky, R.; Dard, M. Tapered Implants in Dentistry: Revitalizing Concepts with Technology: A Review. Adv. Dent. Res. 2016, 28, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Rokn, A.; Ghahroudi, A.R.; Mesgarzadeh, A.; Miremadi, A.; Yaghoobi, S. Evaluation of Stability Changes in Tapered and Parallel Wall Implants: A Human Clinical Trial. J. Dent. 2011, 8, 186. [Google Scholar]
- Lozano-Carrascal, N.; Salomó-Coll, O.; Gilabert-Cerdà, M.; Farré-Pagés, N.; Gargallo-Albiol, J.; Hernández-Alfaro, F. Effect of Implant Macro-Design on Primary Stability: A Prospective Clinical Study. Med. Oral Patol. Oral Cir. Bucal. 2016, 21, e214. [Google Scholar] [CrossRef] [PubMed]
- Da Cunha, H.A.; Francischone, C.E.; Fliho, H.N.; de Oliveira, R.C.G. A Comparison between Cutting Torque and Resonance Frequency in the Assessment of Primary Stability and Final Torque Capacity of Standard and TiUnite Single-Tooth Implants under Immediate Loading. Int. J. Oral Maxillofac. Implants 2004, 19, 578. [Google Scholar]
- Darriba, I.; Seidel, A.; Moreno, F.; Botelho, J.; Machado, V.; Mendes, J.J.; Leira, Y.; Blanco, J. Influence of Low Insertion Torque Values on Survival Rate of Immediately Loaded Dental Implants: A Systematic Review and Meta-Analysis. J. Clin. Periodontol. 2023, 50, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Barone, A.; Alfonsi, F.; Derchi, G.; Tonelli, P.; Toti, P.; Marchionni, S.; Covani, U. The Effect of Insertion Torque on the Clinical Outcome of Single Implants: A Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2016, 18, 588–600. [Google Scholar] [CrossRef] [PubMed]
- Hsu, Y.-Y.; Huang, H.-L.; Fuh, L.-J.; Tsai, M.-T.; Hsu, J.-T. The Effects of Insertion Approach on the Stability of Dental Implants. Appl. Bionics Biomech. 2022, 2022, 7188240. [Google Scholar] [CrossRef]
- Chugh, T.; Jain, A.K.; Jaiswal, R.K.; Mehrotra, P.; Mehrotra, R. Bone Density and Its Importance in Orthodontics. J. Oral Biol. Craniofacial Res. 2013, 3, 92–97. [Google Scholar] [CrossRef]
| n (%) | ||
|---|---|---|
| Implant placement condition | Bone level | 182 (56.9) |
| Not fully inserted | 138 (43.1) | |
| Implant removal torque | Mean ± Sd | 80.81 ± 19.22 |
| (Min − Max) | (40–100) | |
| Group | 30 rpm | 160 (50.0) |
| 50 rpm | 160 (50.0) | |
| Torque subgroup | 25 torque | 40 (12.5) |
| 30 torque | 40 (12.5) | |
| 35 torque | 40 (12.5) | |
| 40 torque | 40 (12.5) | |
| 45 torque | 40 (12.5) | |
| 50 torque | 40 (12.5) | |
| 55 torque | 40 (12.5) | |
| 60 torque | 40 (12.5) |
| 30 rpm (n = 160) | 50 rpm (n = 160) | a p | ||
|---|---|---|---|---|
| Total | Bone level | 66 (41.3) | 116 (72.5) | a 0.001 * |
| Not fully inserted | 94 (58.8) | 44 (27.5) | ||
| 25 torque | Bone level | - | - | - |
| Not fully inserted | 20 (100) | 20 (100) | ||
| 30 torque | Bone level | - | - | - |
| Not fully inserted | 20 (100) | 20 (100) | ||
| 35 torque | Bone level | 0 (0) | 16 (80.0) | a 0.001 * |
| Not fully inserted | 20 (100) | 4 (20.0) | ||
| 40 torque | Bone level | 2 (10) | 20 (100) | a 0.001 * |
| Not fully inserted | 18 (90) | 0 (0) | ||
| 45 torque | Bone level | 4 (20) | 20 (100) | a 0.001 * |
| Not fully inserted | 16 (80) | 0 (0) | ||
| 50 torque | Bone level | 20 (100) | 20 (100) | - |
| Not fully inserted | - | - | ||
| 55 torque | Bone level | 20 (100) | 20 (100) | - |
| Not fully inserted | - | - | ||
| 60 torque | Bone level | 20 (100) | 20 (100) | - |
| Not fully inserted | - | - | ||
| Implant removal torque | Mean ± Sd | 75.31 ± 21.49 | 86.31 ± 14.75 | b 0.001 * |
| (Min-Max) | (40–100) | (50–100) | ||
| Torque Subgroup | Mean ± Sd | (Min − Max) | a p | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 320) | 25 torque | 56.00 ± 9.14 | (40–70) | a 0.001 * | |||||
| 30 torque | 61.50 ± 11.67 | (40–80) | |||||||
| 35 torque | 70.50 ± 12.50 | (45–100) | |||||||
| 40 torque | 76.00 ± 17.44 | (45–100) | |||||||
| 45 torque | 92.00 ± 10.55 | (75–100) | |||||||
| 50 torque | 95.00 ± 8.77 | (80–100) | |||||||
| 55 torque | 96.00 ± 8.10 | (80–100) | |||||||
| 60 torque | 99.50 ± 3.16 | (80–100) | |||||||
| 30 rpm (n = 160) | 25 torque | 49.25 ± 6.13 | (40–60) | a 0.001 * | |||||
| 30 torque | 52.50 ± 10.07 | (40–80) | |||||||
| 35 torque | 61.00 ± 10.08 | (45–80) | |||||||
| 40 torque | 65.25 ± 15.85 | (45–100) | |||||||
| 45 torque | 92.50 ± 10.58 | (75–100) | |||||||
| 50 torque | 90.00 ± 10.26 | (80–100) | |||||||
| 55 torque | 93.00 ± 9.79 | (80–100) | |||||||
| 60 torque | 99.00 ± 4.47 | (80–100) | |||||||
| 50 rpm (n = 160) | 25 torque | 62.75 ± 6.17 | (50–70) | a 0.001 * | |||||
| 30 torque | 70.50 ± 2.76 | (65–75) | |||||||
| 35 torque | 80.00 ± 5.38 | (70–100) | |||||||
| 40 torque | 86.75 ± 11.39 | (70–100) | |||||||
| 45 torque | 91.50 ± 10.77 | (75–100) | |||||||
| 50 torque | 100.00 ± 0.00 | (100–100) | |||||||
| 55 torque | 99.00 ± 4.47 | (80–100) | |||||||
| 60 torque | 100.00 ± 0.00 | (100–100) | |||||||
| Post hoc | 25 torque | 30 torque | 35 torque | 40 torque | 45 torque | 50 torque | 55 torque | 60 torque | |
| Total | 25 torque | ||||||||
| 30 torque | 1.000 | ||||||||
| 35 torque | 0.001 * | 1.000 | |||||||
| 40 torque | 0.001 * | 0.007 * | 0.678 | ||||||
| 45 torque | 0.001 * | 0.001 * | 0.001 * | 0.004 * | |||||
| 50 torque | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 1.000 | ||||
| 55 torque | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 1.000 | 1.000 | |||
| 60 torque | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 1.000 | 1.000 | 1.000 | ||
| 30 rpm | 25 torque | ||||||||
| 30 torque | 1.000 | ||||||||
| 35 torque | 1.000 | 1.000 | |||||||
| 40 torque | 0.372 | 1.000 | 1.000 | ||||||
| 45 torque | 0.001 * | 0.001 * | 0.001 * | 0.004 * | |||||
| 50 torque | 0.001 * | 0.001 * | 0.001 * | 0.012 * | 1.000 | ||||
| 55 torque | 0.001 * | 0.001 * | 0.001 * | 0.002 * | 1.000 | 1.000 | |||
| 60 torque | 0.001 * | 0.001 * | 0.001 * | 0.001 * | 1.000 | 1.000 | 1.000 | ||
| 50 rpm | 25 torque | ||||||||
| 30 torque | 1.000 | ||||||||
| 35 torque | 0.006 * | 0.347 | |||||||
| 40 torque | 0.001 * | 0.003 * | 1.000 | ||||||
| 45 torque | 0.001 * | 0.001 * | 0.490 | 1.000 | |||||
| 50 torque | 0.001 * | 0.001 * | 0.001 * | 0.138 | 1.000 | ||||
| 55 torque | 0.001 * | 0.001 * | 0.002 * | 0.256 | 1.000 | 1.000 | |||
| 60 torque | 0.001 * | 0.001 * | 0.001 * | 0.138 | 1.000 | 1.000 | 1.000 | ||
| Torque Subgroup | 30 rpm (n = 160) Mean ± Sd (Min − Max) | 50 rpm (n = 160) Mean ± Sd (Min − Max) | a p |
|---|---|---|---|
| 25 torque | 49.25 ± 6.13 | 62.75 ± 6.17 | 0.001 * |
| (40–60) | (50–70) | ||
| 30 torque | 52.50 ± 10.07 | 70.50 ± 2.76 | 0.001 * |
| (40–80) | (65–75) | ||
| 35 torque | 61.00 ± 10.08 | 80.00 ± 5.38 | 0.001 * |
| (45–80) | (70–100) | ||
| 40 torque | 65.25 ± 15.85 | 86.75 ± 11.39 | 0.001 * |
| (45–100) | (70–100) | ||
| 45 torque | 92.50 ± 10.58 | 91.5 ± 10.77 | 0.769 |
| (75–100) | (75–100) | ||
| 50 torque | 90.00 ± 10.26 | 100.00 ± 0.00 | 0.001 * |
| (80–100) | (100–100) | ||
| 55 torque | 93.00 ± 9.79 | 99.00 ± 4.47 | 0.017 * |
| (80–100) | (80–100) | ||
| 60 torque | 99.00 ± 4.47 | 100.00 ± 0.00 | 0.329 |
| (80–100) | (100–100) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orhan, Z.D.; Ciğerim, L. Evaluation of Effect of Different Insertion Speeds and Torques on Implant Placement Condition and Removal Torque in Polyurethane Dense D1 Bone Model. Polymers 2024, 16, 1361. https://doi.org/10.3390/polym16101361
Orhan ZD, Ciğerim L. Evaluation of Effect of Different Insertion Speeds and Torques on Implant Placement Condition and Removal Torque in Polyurethane Dense D1 Bone Model. Polymers. 2024; 16(10):1361. https://doi.org/10.3390/polym16101361
Chicago/Turabian StyleOrhan, Zeynep Dilan, and Levent Ciğerim. 2024. "Evaluation of Effect of Different Insertion Speeds and Torques on Implant Placement Condition and Removal Torque in Polyurethane Dense D1 Bone Model" Polymers 16, no. 10: 1361. https://doi.org/10.3390/polym16101361
APA StyleOrhan, Z. D., & Ciğerim, L. (2024). Evaluation of Effect of Different Insertion Speeds and Torques on Implant Placement Condition and Removal Torque in Polyurethane Dense D1 Bone Model. Polymers, 16(10), 1361. https://doi.org/10.3390/polym16101361






