Abstract
The thinking about metallic replacement has begun in a global context of reducing metallic alloys’ use in odontology. Among the materials proposed for their replacement, poly(etheretherketone) may present interesting properties, especially in removable dentures’ frames. The purpose of this study is to evaluate fracture resistance of PEEK posts-and-cores compared to non-metallic CAD/CAM materials and fiber glass posts. Forty extracted maxillary central incisors were prepared to receive posts. Samples were divided into four groups depending on whether they had been reconstructed with LuxaCam® PEEK, Enamic®, Numerys GF® or LuxaPost®. Samples were submitted to an oblique compressive test and results were statistically analyzed with ANOVA and Student’s tests (or non-parametric tests depending on the conditions). Glass fiber posts and Numerys GF® reveal a significantly higher fracture resistance than LuxaCam® PEEK and Enamic®. No exclusively dental fracture has been noted for the Enamic group, which significantly distinguishes these samples from the three other groups. In our study, it appears that the conception of posts and cores with hybrid ceramic never conducts to a unique tooth fracture. By weighting the results according to the materials used, our data, obtained for the first time on this type of PEEK block, cannot confirm the possibility of using PEEK for inlay-core conception, excepted for specific cases when the material is considered in a patient presenting allergies or systemic disease contraindicating resin or metal.
1. Introduction
There is no consensus in dentistry regarding the restoration of a severely injured tooth, with 0 or 1 healthy wall remaining on the crown after endodontic treatment. The key factor seems to be the possibility to create a ferrule effect under the crown []. The design of a root post is theoretically indicated in order to reinforce the tooth; however, those who oppose the use of posts consider them to be a deleterious factor [] as a vector of intra-radicular stresses, potentiating the risk of irreversible tooth fracture.
Furthermore, the choice of the material to perform the post creates another debate because there is no consensus on this issue either []. Several parameters must be considered such as the need for retention (the number of posts on the same tooth and their length), the risk of material fracture and the risk of tooth fracture. In the anterior sector, the aesthetic properties of the restoration must also be taken into account []. It mainly exists as metal [], fiber [] and ceramic posts [].
Metallic posts, also known as inlay-cores, are constituted of Cobalt–Chromium (CoCr) alloys or more rarely of Nickel–Chromium (NiCr) or Titanium alloys because of a high elasticity modulus []. This property allows one to increase the fracture resistance of the material, but the differences between the elasticity modulus of the post and those of the tooth may complicate the stress transmission inside the root during chewing cycles []. The residual tissues are thus weakened and may break [].
The solution of using fiber posts, whose elasticity modulus is closer to the dentin [], would improve the stress repartition inside the root []. They are constituted of a prefabricated post, made of a resin matrix reinforced with longitudinal fibers (of glass, carbon or quartz) and bonded to the intra-radicular dentin []. A strict protocol is required for their successful implementation since they imply the execution of a bonding procedure. However, with the resistance of the biomaterial being lower, more important is the risk of post fracture []. The main cause of failure of this approach is the dislodgment, but, with the tooth being less exposed to a fracture, its life expectancy on the arch is potentially increased [].
A meta-analysis has recently shown that both metallic and fiber posts could be considered as valuable therapeutic solutions; the choice being driven by the practitioner’s preferences []. The thinking about metallic replacement has begun in a global context of reducing metallic alloys’ use in odontology, especially because of the evolution of the regulatory frameworks all over the world concerning these metals’ security of use [].
The progress of digital dentistry and CAD/CAM devices has been accompanied by the development of new materials, available as blocks or discs and shaped by machining after computer design of the piece to be manufactured. A block supposed to reproduce a fiber-reinforced post (Numerys GF, Itena Clinical, France), for example, was launched in 2019. According to the manufacturer’s data, it is composed of 20% to 25% of epoxy resin and 75% to 80% of unidirectionally oriented glass fibers, and it presents a modulus of elasticity of approximatively 25 GPa. Earlier, in 2013, there have appeared the new Polymer-Infiltrated Ceramic Networks (PICN) composed of 86% ceramic and 14% polymers for the first generation (Enamic, Vita Zahnfabrik, Germany). Mainly intended for use in coronal reconstruction, their modulus of elasticity, close to 30 GPa, has led to imagining their use as root posts [,].
Poly(EtherEtherKetone) (PEEK) is a semi-crystalline polyaromatic thermoplastic polymer which has been marketed in the industry since the early 1980s []. Its first biomedical application was developed in the late 1990s [] as an alternative to metallic or ceramic medical devices in orthopedics or craniofacial reconstructive surgery. It began to be used in the field of odontology more than 10 years ago to create removable partial denture’s basis, several elements in implantology (fixtures abutments, healing screws) [] or even occlusal splints []. This material is free of corrosion and radiolucent [,] which offers an interesting comparison with metals. It is biocompatible, non-toxic, stable over time [] and hypo-allergenic in the absence of monomers in its structure [,]. Even if the applications for PEEK in dentistry are numerous in prosthodontics [], only a few publications have already studied the potential for this biomaterial to serve for post conception.
The objective of our study will thus be to evaluate the mechanical strength of PEEK posts in comparison with three other non-metallic biomaterials. The null hypothesis is that the type of material does not influence the fracture resistance of the tooth-restoration assembly.
2. Materials and Methods
An in vitro study has been performed in Toulouse Health Faculty (Département Odontologie, Université Toulouse III, Toulouse, France).
2.1. Teeth Collection
Forty human upper incisors, extracted for periodontal reasons, have been collected in Toulouse Hospital (Service d’Odontologie, Hôpitaux de Toulouse, Toulouse, France) in compliance with the Hospital’s rules for tissue collection. Before the beginning of the study, the teeth were conserved in a 1% chloramine solution in order to decontaminate them as well as maintain their hydration and their integrity before mechanical tests []. To be suitable for use in the study, the teeth had to present healthy crown and root—i.e., those who present a decay, a crack, a fracture, an incomplete root formation, a resorption, endodontic calcification (evaluated on an X-ray) or a root curvature higher than 20° have been excluded.
2.2. Teeth Preparation
The crowns of the teeth were sectioned perpendicularly to their longitudinal axis, 2 mm above the buccal cement-enamel junction, with a low-speed diamond disc under irrigation (IsoMet 2000, Buehler, Evanston III, Leinfelden-Echterdingen, Germany) (Figure 1a). This cut allowed us to access the endodontic canal whose preparation was performed with a constant rotation system (ProTaper Next, Dentsply-Sirona, Bensheim, Germany). The X2 final file had a 025 diameter and a 6% conicity. Each instrument passage was followed by a 3% sodium hypochlorite rinse, completed for final irrigation with a 17% ethylenediaminetetraacetic acid (EDTA) rinse. The endodontic obturation (Figure 1b) had been performed following the thermocompacted monocone technique with an adequate gutta-percha cone and a eugenol-free cement (AH Plus, Dentsply-Sirola, Bensheim, Germany) to anticipate the need for bonding procedures with the future posts. Then, the endodontic treatment was removed for the first 10 mm of the canal (Gates #3, Dentsply-Sirona, Germany) (Figure 1c) and the endodontium was flared with the smaller file of the fiber post kit (LuxaPost, DMG, Hambourg, Germany). The endodontic preparation ended with a final rinse and drying. A 1 mm wide corono-peripheral reduction was made for each tooth, defining a 2 mm high dentinal cerclage (Figure 1d) in accordance with the minimum ferrule height of 1.5 to 2 mm recommended in the literature [,].
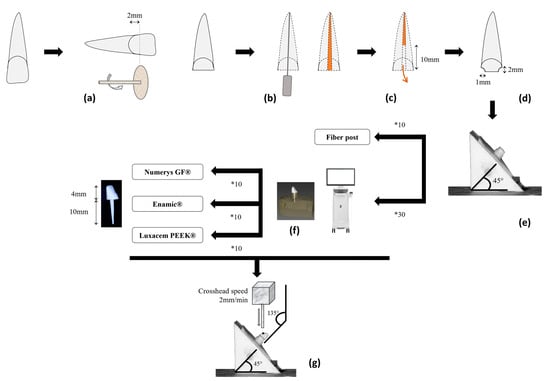
Figure 1.
Schematic representation of the different steps of the experimental procedure. Briefly, each incisor’s crown was cut (a) and the tooth treated endodontically (b). Next, 10 mm of the endodontic filling was removed (c), a corono-peripheral preparation was performed (d) and each tooth was embedded in standardized resin mold (e). Among the 40 teeth, 10 received a fiber post, and the 30 others were scanned with an intra-oral scanner to design and produce posts and cores (f) (10 in fiber-reinforced resin, 10 in hybrid ceramic, 10 in PEEK). Once all the restorations were bonded to the endodontic dentin, the samples were submitted to a universal testing machine in a compression mode at a crosshead speed of 2 mm/min (g).
The prepared roots have been included in a self-curing acrylic resin (SR Ivolen, Ivoclar Vivadent, Saint-Jorioz, France) inside a pyramid-shaped mold that produces a 135° angle between the probe of the future fracture test and the tooth (Figure 1e). This angle simulates the natural inter-incisal angle formed by the longitudinal axes of the maxillary and mandibular central incisors and has already been reproduced many times in mechanical studies [,,,,,,,,].
2.3. Samples Design and Assembly
The 40 prepared teeth were randomly assigned to one of the four groups (n = 10), characterized individually by a different biomaterial to conceive the post: the LuxaCam PEEK (DMG, Hambourg, Germany), the Enamic (Vita Zahnfabrik, Bad Säckingen, Germany), the Numerys GF (Itena Clinical, Villepinte, France) and the LuxaTemp fiber post (DMG, Hambourg, Germany). Their main characteristics are summarized in Table 1.

Table 1.
Main characteristics of the four biomaterials used to conceive the posts in this study (data extracted from [] and manufacturers’ brochures).
For the control group (fiber post LuxaPost small, DMG, Hambourg, Germany), the intra-root canal preparations were etched with 35% orthophosphoric acid (Vococid, VOCO, Cuxhaven, Germany) for 20 s and then rinsed and dried again. A universal adhesive (PermaBond Universel, DMG, Hambourg, Germany) was applied inside the preparations and dried before a 20 s light-curing sequence. The fiber post contained in the kit is already coated with a silane, so the adhesive was directly applied on the post, dried and light-cured for 20 s. A dual-cure restorative composite resin (LuxaCore, DMG, Hambourg, Germany) was injected into the endodontic canals before the fiber post insertion. A 40 s photopolymerization was performed. Then the same composite resin was applied again to build-up the core, and a final light-curing sequence of 20 s was launched. According to the manufacturers’ recommendations, the biomaterial’s curing is complete 5 min after the end of this whole protocol. The design of the occlusal core was thought to measure 4 mm high, the same dimension as the machined posts in the other groups.
For the three other groups, the endodontic preparations have been registered with an intra-oral scanner (Cerec Primescan, Dentsply-Sirona, Bensheim, Germany) whose depth of field of 20 mm was able to access the more apical part of the cavity. The various posts and cores had been designed on Inlab software (Inlab 18.1, Dentsply-Sirona, Bensheim, Germany) before launching the drilling machine (MCXL, Dentsply-Sirona, Bensheim, Germany) with the three types of CAD/CAM blocks (Figure 1f).
The inlay-cores made of PEEK-based material have been sandblasted (50 µm Alumine, 2 bar) and air-dried. A coupling agent (LuxaTemp Glaze & Bond, DMG, Hambourg, Germany) was then slightly applied and light-cured for 20 s. For the hybrid-ceramics restorations, a 5% fluorhydric acid gel (Adiva Cera Etch, Vita-Zahnfabrik, Bad Säckingen, Germany) was applied for 60 s; then the pieces were rinsed, and a silane (Adive C-Prime, Vita-Zahnfabrik, Bad Säckingen, Germany) was coated on their surface. The inlay-cores made of Numerys GF were coated with a specific silane (Silane-it, Itena Clinical, Villepinte, France) only. All these restorations have been bonded on dental tissues with a self-adhesive resin (Permacem 2.0, DMG, Hambourg, Germany) following a principle of double application: one on the post and one inside the tooth. Once the posts were inserted into the roots, the resin excesses were cleaned with a microbrush during the chemopolymerization’s waiting period (30 s under digital pressure and 7 min with no pressure). The final step of the protocol consisted of light-curing buccal and lingual faces of the teeth
2.4. Fracture Tests
The samples, included in their acrylic bases, were submitted to a constant oblique compressive stress at a crosshead speed of 2 mm/min (TA.XT Plus Texture Analyzer, Stable MicroSystems, Godalming, UK) (Figure 1g). The point of impact of the load was located at 2 mm from the incisal edge, in the middle of the lingual surface. The cylindrical probe was positioned to form a 135° angle with the longitudinal axis of the tooth (Figure 1g). Fracture was defined as the point at which the stress reached its maximum value by fracturing the material, the tooth or both. The strength and tenacity values were calculated.
2.5. Fracture Mode
The fracture mode of each tooth has been analyzed after the mechanical tests and classified into one of the three possibilities: dental (only the tooth was broken, the post being intact), material (only the post was broken, the tooth-integrity being respected) or mixed (both the tooth and the post were broken).
2.6. Statistical Analyses
All the data have been collected on an Excel sheet (Microsoft Excel 2019, Microsoft, Redmond, WA, USA). Then the analyses and figures were designed on Stata (Stata v.13, StataCorp, College Station, TX, USA) and Prism (Prism 5, GraphPad, Boston, MA, USA) software. Comparisons between the groups have been performed with ANOVA (global p-value) or Student’s tests (bivariate analyses) after verification of the values’ normal distribution and variance equality. If Shapiro–Wilk tests (for normality) and/or Levene’s tests (for variance equality) were significant, non-parametric Mann–Whitney tests were preferred for bivariate analyses. The fracture mode being presented as a classification, Fisher tests have been used to compare groups. The significance level was fixed at 5%.
3. Results
3.1. Fracture Tests
Posts made of PEEK-based biomaterial present a lower resistance (9.48 ± 6.65 MPa) than fiber posts (15.88 ± 4.37 MPa, p = 0.005) and Numerys GF posts (15.35 ± 6.65 MPa, p = 0.03) (Table 2). The Enamic biomaterial is the option for which the lower strength is necessary to reach the fracture (6.05 ± 4.14 MPa; p = 0.0001 and 0.002 in comparison respectively with fiber posts and Numerys GF posts).

Table 2.
Results of the fracture tests performed on the four materials. Values are presented as Mean ± Standard Deviation. A different letter a,b,c in the same line indicates that the difference between the two biomaterials presents a p-value lower than 0.05. Each group contains 10 samples.
Tenacity, that can be interpreted as the energy stored until failure, is highest for the fiber posts (12.58 ± 5.46 Pa/m²), and these are significantly more elevated than those of PEEK (6.43 ± 4.22 Pa/m², p = 0.01) and Enamic posts (3.18 ± 2.92 Pa/m², p = 0.0005). For the Numerys GF posts, tenacity is only significantly different than those of the Enamic group (9.69 ± 5.92 Pa/m², p = 0.002).
3.2. Fracture Mode
No exclusively dental fracture was noted for the Enamic group (Figure 2), which significantly distinguishes the proportions of fracture patterns of these samples from the three other groups (60% of dental fracture in PEEK group (p = 0.02), 80% in fiber posts group (p = 0.001) and 70% in Numerys GF group (p = 0.001)). All the modes of fracture are summarized in Table 3.
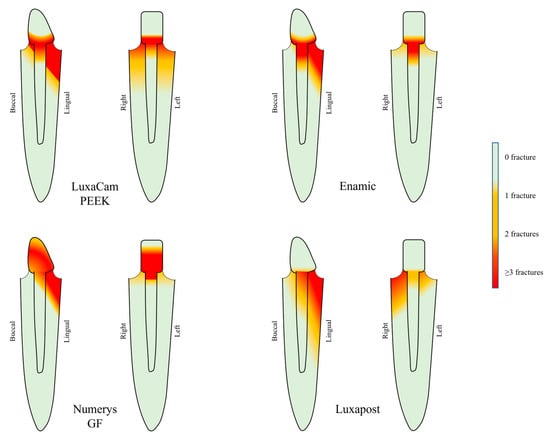
Figure 2.
Distribution of the fracture lines retrieved among the samples of each of the four groups. For each material, side (left) and front (right) diagrams are shown. Each group brings 10 samples.

Table 3.
Proportion of each fracture mode observed in the four groups. A different letter a,b,c,d indicates that the difference between the two biomaterials presents a p-value lower than 0.05. Each group contains 10 samples.
As shown in Figure 2, the fracture feature profiles on the material are mainly located at the post-core junction for the PEEK and Enamic samples. In the Numerys GF® group, fractures are more widespread on the core.
4. Discussion
The results of our study highlight the excellent mechanical behavior of fiber-reinforced materials (fiber posts and Numerys GF) in comparison with PEEK-based material and hybrid ceramic for the conception of post and core reconstitutions. The null hypothesis initially formulated concerning the absence of influence of the material type on the fracture resistance is rejected.
These results are consistent with the real indications for each one of these materials. PEEK and hybrid ceramic are sold for a use, respectively, in removable dentures and fixed prosthesis (inlays and crowns). The key element to explain the values obtained is the biomaterials’ elasticity modulus because the results are better for the LuxaPost and the Numerys GF, which are the two materials for which the Young modulus is close to those of the dentin []. Dietschi et al. have concluded, in their systematic review more than 15 years ago, that the strength experienced by a tooth would be better distributed along the root with a material whose elasticity modulus is closer to natural tissues [].
In our study, it appears that the conception of posts and cores with hybrid ceramic never conducts to the tooth fracture. This characteristic makes one question the possibility of using this material in this way. On the one hand, it is difficult to consider a restoration with a very low tenacity when milled as a post. On the other hand, its poor mechanical resistance may be interesting for the root survival, as a biomaterial that breaks with no injury on dental tissues would improve the “life expectancy” of the tooth and make the new therapeutic intervention easier. Our results must be balanced with regard to the existing literature, especially previously published results that have shown the absence of a significant difference in the fracture resistance of hybrid ceramic, zirconium and metallic inlay-cores []. However, the authors have also noted fewer root fractures in the hybrid ceramic group [].
An important number of studies have already compared the in vitro and clinical behaviors of fiber posts and metallic posts [,,,,,,,,,]. Among them, two randomized clinical trials have concluded in the absence of significant difference between the two types of tenons [,]. Their survival after a follow-up period of 17 years is comparable []. Our study was focused on upper incisors with aesthetic considerations and with a metal-free thinking; that is why no metallic inlay-core was included here, even if they present an excellent fracture resistance [].
The material that is still relatively new and, therefore, lacks such clinical feedback is the milled fiber-reinforced post (Numerys GF). In contrast with the conventional fiber post, it is especially adapted to the dentin walls; thus, the adhesive thickness is lower, and the risks for air bubbles and gaps are reduced []. Our results, which show the similar resistance of the two types of restorations, confirm the existing data obtained by Eid et al. on a standardized fiber post and a milled one []. However, we have chosen to concentrate purely on mechanical behavior with no intervention of fatigue in our tests, on which others have conducted research, such as Falcão Spina et al. in 2017 []. Their results slightly differ since they showed no difference between several milled esthetic biomaterials used as posts including hybrid ceramic []. The greatest proximity of values in their observations may be explained by the lower tolerance of fiber-reinforced resins to fatigue in comparison with those of Enamic to fatigue, which probably smoothed their results in contrast to those we have obtained. The interest of fatigue simulation is to apply a dynamic repeated stress that reproduces the real occlusal strength in humans and, thus, to accelerate the material wear []. It is interesting to highlight that one study, published in 2019, shows an important fracture resistance for hybrid ceramic posts and cores (793.8 ± 55.6 N in Enamic group vs. 607.7 ± 54.8 N in fiber posts group) on samples that were submitted to thermocycling aging and entirely restored since the authors had added metallic crowns on the cores []. The presence of a crown obviously improves the clinical relevance of the mechanical test, but its shape, its thickness and its composition add a new resistance to the whole restoration and may hide the specific properties of the post [].
Previously published works on PEEK used for post design are relatively recent even if the biomaterial has been of interest in dentistry for approximatively two decades. Thanks to new technologies, Sammany et al. in 2019 [], Yu et al. in 2022 [] and Gontijo et al. more recently [] have performed finite elements tri-dimensional analyses to evaluate the behavior of PEEK inlay-cores, and their studies have shown that the tooth survival was not compromised when it was reconstituted with such a post [,]. Interestingly, the results of Sammany et al. show that under physiological forces, the stress distribution all along the root was similar to those of a safe tooth []. In 2020, Teixeira et al. have compared the fracture resistance of several biomaterials designed as posts and cores with interesting results concerning Poly(EtherEtherKetone) []. Indeed, they found no significant difference between this material, fiber posts and milled composite resin. Among the failures observed in the PEEK group, 83.3% were a loss of bonding and could thus be considered as favorable for tooth survival []. Recently, in 2023, M.O. Lima et al. have published results showing that PEEK posts and cores were slightly similar to those of glass-fiber posts in tooth resistance preservation provided that a ferrule effect is respected during tissue preparation []. The main characteristics of the protocols already published that have evaluated the resistance and feasibility of PEEK posts and cores are presented in Table 4.
Some of our results may be contradictory in comparison with others studies, especially one published this year. The study used other types of PEEK CAD/CAM blocks and showed material deformation only for PEEK whereas posts made of Enamic® critically broke in 20% of the cases []. As presented in Table 4, the PEEK CAD/CAM blocks used in our study have never been tested previously. Thus, our results, that highlight that PEEK posts and cores seem less resistant than fiber-reinforced posts (pre-fabricated or milled) and that 80% present tooth fracture, should be weighted by limiting their external validity to these blocks in particular. Moreover, our protocol slightly differs with those retrieved in previous publications, as we chose to perform a tissue preparation before sealing the posts in order to create a ferule effect on the tooth. This parameter was also designed in only 5 publications of the 22 published since 2020 [,,,,]. It may also be worth highlighting one of the parameters that varies greatly between the different studies, namely the type of support on which the tests have been carried out. Without taking into account numerical simulation analyses, in vitro tests have been carried out on natural human teeth [,,], bovine teeth [,,] or artificial supports [,], which can significantly change the results obtained. Finally, the last parameters that may influence the differences observed between the studies concern the nature of the assembling biomaterial or the post’s size. Here, a self-adhesive resin containing mainly metacrylic esters (Permacem 2.0, DMG, Hambourg, Germany) has been chosen for three reasons: its compatibility with the three types of milled posts, its easy-handling and, thus, the reduction of bias in its manipulation between several samples. In the majority of studies, a self-adhesive resin with tri-ethylene glycol dimethacrylate (TEGDMA) monomer is used (RelyX Unicem, 3 M ESPE, St Paul, MN, USA) [,,,,,]. The height of the tenons is directly correlated to the thickness of the residual tissues, whatever the type of post, the health of these tissues, or the therapeutic’s success rate [,,,,]. Over the root, the presence of a ferrule effect may be decisive in the prosthetic survival [,,,,,]. It is efficient when there is a dentin wall perpendicular to the cervical limit on the whole circumference of the tooth. Its objective is to reduce the intra-canal stress and consequently increase its resistance to fracture []. There are conflicting data in the literature concerning its exact dimensions, but it seems to be recognized that the ferrule effect should have a minimal size of 1 mm height [,], a 0.5 mm thickness [] and a presence on at least 75% of the tooth’s circumference []. According to Naumann et al., the presence of the ferrule is more important than the choice of the post []. Pascal Magne et al. have even suggested that a tenon would no longer be necessary if the ferrule were higher than 2 mm in height and 1 mm in thickness []. If a post is chosen, its length should not be considered a decisive factor in the bonding protocol applied [] as the number of dentinal tubules decreases from the coronal to the apical part of the root. Apically, the tissues are less accessible to instrumentation and photopolymerization light [], so it appears not to be necessary to increase the tenon dimensions just to improve the quality of the bonding procedure.
Our data thus cannot confirm the possibility of using PEEK for inlay-core conception, but it is possible to mention specific cases in which it can be of high interest when the material is considered in a patient presenting allergies or systemic disease contraindicating resin or metal [].

Table 4.
Experimental conditions applied in the studies published since 2020 in which the authors have evaluated the mechanical properties of PEEK posts and cores.
Table 4.
Experimental conditions applied in the studies published since 2020 in which the authors have evaluated the mechanical properties of PEEK posts and cores.
| Year of Pub. | Authors | PEEK Manufacturer | Main Characteristics of the Protocol | Main Conclusions on PEEK |
|---|---|---|---|---|
| 2023 | Our study | DMG | Oblique compressive stress (2 mm/min) on PEEK posts and cores bonded to natural teeth (with tissue preparation and ferule effect). | Resistance of PEEK is lower than those of fiber posts. |
| 2023 | Ahmad et al. [] | Juvora | Oblique compressive stress (1 mm/min) on PEEK posts and cores bonded to natural teeth (with tissue preparation and ferule effect) and pull-out tests. | Higher resistance for prefabricated PEEK posts with composite core than PEEK full posts and cores. Similar results for pull-out tests. |
| 2023 | Gontijo et al. [] | Juvora | Oblique compressive stress (0.5 mm/min) on PEEK posts and cores bonded to bovine teeth (with tissue preparation and ferule effect). Moreover, simulation with finite element analysis. | Weakened roots restored with PEEK posts and cores are more resistant than those treated with prefabricated glass fiber posts. |
| 2023 | Kole et al. [] | Juvora | Push-out stress on slices of PEEK posts and cores bonded to natural teeth (no ferule effect). | Zirconia post-cores appear to be a promising material. |
| 2023 | Lima et al. [] | Juvora | Oblique compressive stress (1 mm/min) on PEEK posts and cores bonded to bovine teeth (with tissue preparation and ferule effect). Moreover, simulation with finite element analysis. | Fracture resistance of the tooth is not different with PEEK posts and cores. |
| 2023 | Saisho et al. [] | Amann Girrbach | Oblique compressive stress (1 mm/min) on PEEK posts and cores bonded to natural teeth (no ferule effect) and pull-out tests. | No difference between the materials for compressive load. PEEK posts and cores showed lower bond strength to intracanal dentin. |
| 2023 | Zhao et al. [] | Unspecified | Shear bond strength of PEEK-glass fibers composites cores on artificial molds. No posts; no use of natural teeth. | The mechanical properties of the composites were greatly improved. |
| 2022 | Attia et al. [] | Bredent | Pull-out tests on PEEK posts and cores bonded to natural teeth (no ferule effect). | Precisions on bonding protocol, not on material choice for post and core (no control group). |
| 2022 | Gontijo et al. [] | Juvora | Oblique compressive stress (0.5 mm/min) on PEEK posts and cores bonded to bovine teeth (with tissue preparation and ferule effect). | In presence of good bone condition, roots restored with PEEK posts and cores provide more reparable fractures and more resistant roots than those treated with prefabricated and anatomic glass fiber posts. |
| 2022 | Hallak et al. [] | Informatic simulation | Simulation of masticatory forces with finite element analysis software on upper central incisors restored with PEEK posts. | Similar stress intensity and distribution between PEEK and glass fiber posts. |
| 2022 | Monteiro et al. [] | Bredent | Pull-out tests on PEEK posts and cores bonded to bovine teeth (no ferule effect). | Good clinical options, but with a need for improvement. |
| 2022 | Pourkhalili et al. [] | Bredent | Oblique compressive stress (0.5 mm/min) on PEEK posts and cores bonded to natural teeth (ferule effect not specified). | Mode of failure mostly repairable in the PEEK group. Resistance is lower than Ni-Cr alloys and greater than fiberglass posts. |
| 2022 | Yu et al. [] | Informatic simulation | Simulation of mechanical load with finite element analysis software on upper central incisors restored with PEEK and Carbone-reinforced-PEEK posts. | Biomechanical behavior of the CFR-PEEK posts and cores was the closest to dentin. |
| 2021 | Haralur SB. [] | Unspecified | Oblique compressive stress (0.5 mm/min) on PEEK posts and cores bonded to natural teeth (with tissue preparation). | Resistance of PEEK is higher than those of fiber posts. |
| 2021 | Ibrahim et al. [] | Informatic simulation | Simulation of mechanical and thermal load with finite element analysis software on upper central incisors restored with PEEK posts. | Good resistance to masticatory forces for teeth restored with PEEK posts and favorable intra-radicular stress distribution. |
| 2021 | Özarslan et al. [] | Juvora | Oblique compressive stress (1 mm/min) on PEEK posts and cores bonded to natural teeth (no ferule effect). | No superior features for PEEK in comparison with zirconia and glass-fiber. |
| 2020 | Benli et al. [] | Juvora | Pull-out tests on PEEK posts bonded on natural teeth. No cores. | PEEK is a reliable option for dental posts. |
| 2020 | Çulhaoglu et al. [] | Bredent | Shear bond strength of PEEK cores on resin. No posts; no use of natural teeth. | Acceptable resistance of resin bonding on PEEK surface. |
| 2020 | Li et al. [] | Bredent | Pull-out tests of PEEK post and core restorations combined with polyvinylsiloxane attachments. No use of natural teeth. | The new post and core system showed favorable retention forces. |
| 2020 | Nahar et al. [] | Informatic simulation | Simulation of mechanical load with finite element analysis software on upper central incisors restored with several PEEK posts (carbon fibers-reinforced (CFR), glass fibers-reinforced (GFR), PEKK). | CFR-PEEK is a good material for the fabrication of endodontic post. GFR-PEEK and PEKK materials can also be used. |
| 2020 | Sugano et al. [] | Yasojima | Oblique compressive stress (1 mm/min) on PEEK posts and resin cores bonded to bovine teeth with flared canals (with ferule effect). | Higher stability is obtained with PEEK posts and glass fiber sleeves. |
| 2020 | Teixeira et al. [] | DEGOS | Oblique compressive stress (0.5 mm/min) on PEEK posts and cores bonded to natural teeth (no ferule effect). | Resistance of PEEK is comparable to those of fiber posts. |
| 2020 | Tekin et al. [] | Informatic simulation | Simulation of mechanical load and stress distribution with finite element analysis software on upper central incisors restored with PEEK posts and cores. | No difference in the stress value between PEEK and fiber posts. |
5. Conclusions
This study has highlighted the fracture resistance of several biomaterials used to build-up bonded posts and cores on natural human teeth. Within the limitations of this study, the following conclusions could be drawn:
- Under oblique compressive tests, posts and cores designed from CAD/CAM blocks made of PEEK (80%) and TiO2 (20%) present a lower resistance in comparison to fiber posts.
- Prefabricated fiber posts and milled fiber posts present a similar behavior under oblique compressive tests.
- The Enamic material, used to design posts and cores, seems to be the most protective concerning root fracture.
The results of this study need to be weighted according to block manufacturers, particularly in the case of PEEK.
Author Contributions
Conceptualization, T.C. and K.N.; methodology, T.C. and K.N.; software, K.R.; validation, T.C., K.R. and K.N.; formal analysis, T.C., P.P. and J.D.; investigation, K.R. and P.P.; resources, K.N. and T.V.; data curation, K.R. and P.P.; writing—original draft preparation, K.R., T.V. and T.C.; writing—review and editing, J.D., P.P. and K.N.; visualization, T.C.; supervision, T.C. and K.N.; project administration, T.C. and K.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Data are available on reasonable demand addressed to the authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Naumann, M.; Schmitter, M.; Frankenberger, R.; Krastl, G. “Ferrule Comes First. Post Is Second!” Fake News and Alternative Facts? A Systematic Review. J. Endod. 2018, 44, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Mamoun, J. Post and Core Build-Ups in Crown and Bridge Abutments: Bio-Mechanical Advantages and Disadvantages. J. Adv. Prosthodont. 2017, 9, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Balevi, B. Metal or Fibre Posts and Root Fractures. Evid.-Based Dent. 2015, 16, 80–81. [Google Scholar] [CrossRef]
- Kumar, L.; Pal, B.; Pujari, P. An Assessment of Fracture Resistance of Three Composite Resin Core Build-up Materials on Three Prefabricated Non-Metallic Posts, Cemented in Endodontically Treated Teeth: An in Vitro Study. PeerJ 2015, 3, e795. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Polo, M.; Llidó, B.; Rivero, A.; Del Río, J.; Celemín, A. A 10-Year Retrospective Study of the Survival Rate of Teeth Restored with Metal Prefabricated Posts versus Cast Metal Posts and Cores. J. Dent. 2010, 38, 916–920. [Google Scholar] [CrossRef] [PubMed]
- Başaran, G.; Göncü Başaran, E.; Ayna, E.; Değer, Y.; Ayna, B.; Tuncer, M.C. Microtensile Bond Strength of Root Canal Dentin Treated with Adhesive and Fiber-Reinforced Post Systems. Braz. Oral Res. 2019, 33, e027. [Google Scholar] [CrossRef]
- Martins, M.D.; Junqueira, R.B.; de Carvalho, R.F.; Lacerda, M.F.L.S.; Faé, D.S.; Lemos, C.A.A. Is a Fiber Post Better than a Metal Post for the Restoration of Endodontically Treated Teeth? A Systematic Review and Meta-Analysis. J. Dent. 2021, 112, 103750. [Google Scholar] [CrossRef]
- Dietschi, D.; Duc, O.; Krejci, I.; Sadan, A. Biomechanical Considerations for the Restoration of Endodontically Treated Teeth: A Systematic Review of the Literature—Part 1. Composition and Micro- and Macrostructure Alterations. Quintessence Int. 2007, 38, 11. [Google Scholar]
- Kurthukoti, A.J.; Paul, J.; Gandhi, K.; Rao, D.B.J. Fracture Resistance of Endodontically Treated Permanent Anterior Teeth Restored with Three Different Esthetic Post Systems: An in Vitro Study. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 296. [Google Scholar] [CrossRef]
- Ambica, K.; Mahendran, K.; Talwar, S.; Verma, M.; Padmini, G.; Periasamy, R. Comparative Evaluation of Fracture Resistance under Static and Fatigue Loading of Endodontically Treated Teeth Restored with Carbon Fiber Posts, Glass Fiber Posts, and an Experimental Dentin Post System: An In Vitro Study. J. Endod. 2013, 39, 96–100. [Google Scholar] [CrossRef]
- Verri, F.R.; Okumura, M.H.T.; Lemos, C.A.A.; de Faria Almeida, D.A.; de Souza Batista, V.E.; Cruz, R.S.; Oliveira, H.F.F.; Pellizzer, E.P. Three-Dimensional Finite Element Analysis of Glass Fiber and Cast Metal Posts with Different Alloys for Reconstruction of Teeth without Ferrule. J. Med. Eng. Technol. 2017, 41, 644–651. [Google Scholar] [CrossRef]
- King, P.A.; Setchell, D.J.; Rees, J.S. Clinical Evaluation of a Carbon Fibre Reinforced Carbon Endodontic Post. J. Oral Rehabil. 2003, 30, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Wang, Q. Comparison of Fracture Resistance between Cast Posts and Fiber Posts: A Meta-Analysis of Literature. J. Endod. 2013, 39, 11–15. [Google Scholar] [CrossRef]
- Marchionatti, A.M.E.; Wandscher, V.F.; Rippe, M.P.; Kaizer, O.B.; Valandro, L.F.; Marchionatti, A.M.E.; Wandscher, V.F.; Rippe, M.P.; Kaizer, O.B.; Valandro, L.F. Clinical Performance and Failure Modes of Pulpless Teeth Restored with Posts: A Systematic Review. Braz. Oral Res. 2017, 31, e64. [Google Scholar] [CrossRef] [PubMed]
- Vaicelyte, A.; Janssen, C.; Le Borgne, M.; Grosgogeat, B. Cobalt–Chromium Dental Alloys: Metal Exposures, Toxicological Risks, CMR Classification, and EU Regulatory Framework. Crystals 2020, 10, 1151. [Google Scholar] [CrossRef]
- Alkhatri, R.; Saleh, A.R.M.; Kheder, W. Impact of Post and Core Materials on the Apical Extension of Root Fracture in Root Canal Treated Teeth. J. Mater. Res. Technol. 2021, 10, 730–737. [Google Scholar] [CrossRef]
- Falcão Spina, D.R.; Goulart da Costa, R.; Farias, I.C.; da Cunha, L.G.; Ritter, A.V.; Gonzaga, C.C.; Correr, G.M. CAD/CAM Post-and-Core Using Different Esthetic Materials: Fracture Resistance and Bond Strengths. Am. J. Dent. 2017, 30, 299–304. [Google Scholar]
- Skirbutis, G.; Dzingutė, A.; Masiliūnaitė, V.; Šulcaitė, G.; Žilinskas, J. PEEK Polymer’s Properties and Its Use in Prosthodontics. A Review. Stomatologija 2018, 20, 54–58. [Google Scholar]
- Papathanasiou, I.; Kamposiora, P.; Papavasiliou, G.; Ferrari, M. The Use of PEEK in Digital Prosthodontics: A Narrative Review. BMC Oral Health 2020, 20, 217. [Google Scholar] [CrossRef] [PubMed]
- Najeeb, S.; Zafar, M.S.; Khurshid, Z.; Siddiqui, F. Applications of Polyetheretherketone (PEEK) in Oral Implantology and Prosthodontics. J. Prosthodont. Res. 2016, 60, 12–19. [Google Scholar] [CrossRef]
- Delrieu, J.; Joniot, S.; Vergé, T.; Destruhaut, F.; Nasr, K.; Canceill, T. The Use of PEEK as an Occlusal Splint in a Patient with Histaminosis: A Case Report: Case Report of a PEEK Occlusal Splint. Spec. Care Dent. 2022, 42, 646–650. [Google Scholar] [CrossRef]
- Hahnel, S.; Wieser, A.; Lang, R.; Rosentritt, M. Biofilm Formation on the Surface of Modern Implant Abutment Materials. Clin. Oral Implant. Res. 2015, 26, 1297–1301. [Google Scholar] [CrossRef]
- Sobieraj, M.C.; Kurtz, S.M.; Rimnac, C.M. Notch Sensitivity of PEEK in Monotonic Tension. Biomaterials 2009, 30, 6485–6494. [Google Scholar] [CrossRef]
- Skirbutis, G. A Review of PEEK Polymer’s Properties and Its Use in Prosthodontics. Stomatologija 2017, 19, 19–23. [Google Scholar] [PubMed]
- Zoidis, P.; Papathanasiou, I.; Polyzois, G. The Use of a Modified Poly-Ether-Ether-Ketone (PEEK) as an Alternative Framework Material for Removable Dental Prostheses. A Clinical Report. J. Prosthodont. 2016, 25, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Vaezi, M.; Yang, S. A Novel Bioactive PEEK/HA Composite with Controlled 3D Interconnected HA Network. Int. J. Bioprinting 2015, 1, 66–76. [Google Scholar] [CrossRef]
- Mobarak, E.H.; El-Badrawy, W.; Pashley, D.H.; Jamjoom, H. Effect of Pretest Storage Conditions of Extracted Teeth on Their Dentin Bond Strengths. J. Prosthet. Dent. 2010, 104, 92–97. [Google Scholar] [CrossRef]
- Al-Omiri, M.K.; Mahmoud, A.A.; Rayyan, M.R.; Abu-Hammad, O. Fracture Resistance of Teeth Restored with Post-Retained Restorations: An Overview. J. Endod. 2010, 36, 1439–1449. [Google Scholar] [CrossRef]
- Calabro, D.E.; Kojima, A.N.; Gallego Arias Pecorari, V.; Helena Coury Saraceni, C.; Blatz, M.B.; Özcan, M.; Mikail Melo Mesquita, A. A 10-Year Follow-Up of Different Intra-Radicular Retainers in Teeth Restored with Zirconia Crowns. Clin. Cosmet. Investig. Dent. 2019, 11, 409–417. [Google Scholar] [CrossRef]
- Makade, C.S.; Meshram, G.K.; Warhadpande, M.; Patil, P.G. A Comparative Evaluation of Fracture Resistance of Endodontically Treated Teeth Restored with Different Post Core Systems—An in-Vitro Study. J. Adv. Prosthodont. 2011, 3, 90–95. [Google Scholar] [CrossRef]
- Doshi, P.; Kanaparthy, A.; Kanaparthy, R.; Parikh, D.S. A Comparative Analysis of Fracture Resistance and Mode of Failure of Endodontically Treated Teeth Restored Using Different Fiber Posts: An In Vitro Study. J. Contemp. Dent. Pract. 2019, 20, 1195–1199. [Google Scholar] [CrossRef]
- Mehrvarzfar, P.; Rezvani, Y.; Jalalian, E. Comparison of Resilon and Gutta-Percha Filling Materials on Root Canal Fracture Resistance Following Restoring with Quartz Fiber Posts. J. Dent. 2012, 9, 156. [Google Scholar]
- Chauhan, N.; Saraswat, N.; Parashar, A.; Sandu, K.; Jhajharia, K.; Rabadiya, N. Comparison of the Effect for Fracture Resistance of Different Coronally Extended Post Length with Two Different Post Materials. J. Int. Soc. Prev. Community Dent. 2019, 9, 144. [Google Scholar] [CrossRef]
- Khaledi, A.A.R.; Sheykhian, S.; Khodaei, A. Evaluation of Retention of Two Different Cast Post-Core Systems and Fracture Resistance of the Restored Teeth. J. Dent. 2015, 16, 121–128. [Google Scholar]
- Mergulhão, V.; de Mendonça, L.; de Albuquerque, M.; Braz, R. Fracture Resistance of Endodontically Treated Maxillary Premolars Restored With Different Methods. Oper. Dent. 2019, 44, E1–E11. [Google Scholar] [CrossRef]
- Steiner, M.; Mitsias, M.E.; Ludwig, K.; Kern, M. In Vitro Evaluation of a Mechanical Testing Chewing Simulator. Dent. Mater. 2009, 25, 494–499. [Google Scholar] [CrossRef]
- Kumagae, N.; Komada, W.; Fukui, Y.; Okada, D.; Takahashi, H.; Yoshida, K.; Miura, H. Influence of the Flexural Modulus of Prefabricated and Experimental Posts on the Fracture Strength and Failure Mode of Composite Resin Cores. Dent. Mater. J. 2012, 31, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Vafaee, F.; Khoshhal, M.; Rezaei, A.; Sooltani, F.; Jalalzadeh, M.; Yalpaniyan, A.; Firooz, F.; Izady, A.R.; Yarmohamadi, E. Multiple In Vitro Analyses of Fracture Resistance in Maxillary Central Incisors Restored with Fiber Posts. Iran. Endod. J. 2010, 5, 125–130. [Google Scholar]
- Kathuria, A.; Kavitha, M.; Khetarpal, S. Ex Vivo Fracture Resistance of Endodontically Treated Maxillary Central Incisors Restored with Fiber-Reinforced Composite Posts and Experimental Dentin Posts. J. Conserv. Dent. 2011, 14, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Sammany, F.; Sultan, M.; Ide, N.A.-D. Stress and Strain Distribution in a Single Root Canal Post Made of Polyether Ether Ketone Using Three-Dimensional Finite Elements Method. Acad. J. Oral Dent. Med. 2019, 8, 1–7. [Google Scholar]
- Sarkis-Onofre, R.; de Castilho Jacinto, R.; Boscato, N.; Cenci, M.S.; Pereira-Cenci, T. Cast Metal vs. Glass Fibre Posts: A Randomized Controlled Trial with up to 3 Years of Follow Up. J. Dent. 2014, 42, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Juloski, J.; Fadda, G.M.; Monticelli, F.; Fajó-Pascual, M.; Goracci, C.; Ferrari, M. Four-Year Survival of Endodontically Treated Premolars Restored with Fiber Posts. J. Dent. Res. 2014, 93, 52S–58S. [Google Scholar] [CrossRef]
- Fokkinga, W.A.; Kreulen, C.M.; Bronkhorst, E.M.; Creugers, N.H.J. Up to 17-Year Controlled Clinical Study on Post-and-Cores and Covering Crowns. J. Dent. 2007, 35, 778–786. [Google Scholar] [CrossRef]
- Wang, X.; Shu, X.; Zhang, Y.; Yang, B.; Jian, Y.; Zhao, K. Evaluation of Fiber Posts vs Metal Posts for Restoring Severely Damaged Endodontically Treated Teeth: A Systematic Review and Meta-Analysis. Quintessence Int. 2018, 50, 8–20. [Google Scholar] [CrossRef]
- Garcia, P.P.; Wambier, L.M.; de Geus, J.L.; da Cunha, L.F.; Correr, G.M.; Gonzaga, C.C. Do Anterior and Posterior Teeth Treated with Post-and-Core Restorations Have Similar Failure Rates? A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2019, 121, 887–894.e4. [Google Scholar] [CrossRef]
- De Souza Batista, V.E.; Bitencourt, S.B.; Bastos, N.A.; Pellizzer, E.P.; Goiato, M.C.; dos Santos, D.M. Influence of the Ferrule Effect on the Failure of Fiber-Reinforced Composite Post-and-Core Restorations: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2020, 123, 239–245. [Google Scholar] [CrossRef]
- Naumann, M.; Koelpin, M.; Beuer, F.; Meyer-Lueckel, H. 10-Year Survival Evaluation for Glass-Fiber–Supported Postendodontic Restoration: A Prospective Observational Clinical Study. J. Endod. 2012, 38, 432–435. [Google Scholar] [CrossRef] [PubMed]
- Martino, N.; Truong, C.; Clark, A.E.; O’Neill, E.; Hsu, S.-M.; Neal, D.; Esquivel-Upshaw, J.F. Retrospective Analysis of Survival Rates of Post-and-Cores in a Dental School Setting. J. Prosthet. Dent. 2020, 123, 434–441. [Google Scholar] [CrossRef]
- Eid, R.; Juloski, J.; Ounsi, H.; Silwaidi, M.; Ferrari, M.; Salameh, Z. Fracture Resistance and Failure Pattern of Endodontically Treated Teeth Restored with Computer-Aided Design/ Computer-Aided Manufacturing Post and Cores: A Pilot Study. J. Contemp. Dent. Pract. 2019, 20, 56–63. [Google Scholar] [CrossRef]
- Borzangy, S.S.; Saker, S.; Al-Zordk, W.A.E.-G. Effect of Restauration Technique on Resistance to Fracture of Endodontically Treated Anterior Teeth with Flared Root Canals. J. Biomed. Res. 2019, 33, 131. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, R.; Gupta, S.; Tandan, A.; Gupta, N.K.; Dwivedi, R.; Aggarwal, R. Comparative Evaluation of Fracture Resistance of Various Post Systems Using Different Luting Agents under Tangential Loading. J. Oral Biol. Craniofacial Res. 2013, 3, 63–67. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yu, H.; Feng, Z.; Wang, L.; Mihcin, S.; Kang, J.; Bai, S.; Zhao, Y. Finite Element Study of PEEK Materials Applied in Post-Retained Restorations. Polymers 2022, 14, 3422. [Google Scholar] [CrossRef] [PubMed]
- Gontijo, I.G.; Ferretti, M.A.; Caldas, R.A.; Pecorari, V.G.A.; França, F.M.G.; Oliveira, L.K.N.; Aguiar, F.H.B. Biomechanical Behavior of Weakened Roots Restored with Custom-Made Post-and-Cores of Glass Fiber and Polyetheretherketone. J. Prosthodont. 2022, 1–8. [Google Scholar] [CrossRef]
- Teixeira, K.; Duque, T.; Maia, H.; Gonçalves, T. Fracture Resistance and Failure Mode of Custom-Made Post-and-Cores of Polyetheretherketone and Nano-Ceramic Composite. Oper. Dent. 2020, 45, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Lima, M.O.; Ferretti, M.A.; Caldas, R.A.; Barão, V.A.R.; França, F.M.G.; Lima, D.A.N.L.; Martins, L.R.; Aguiar, F.H.B. Application of Polyetheretherketone (PEEK) Posts: Evaluation of Fracture Resistance and Stress Distribution in the Root: In Vitro and Finite Element Analyses. Braz. Oral Res. 2023, 37, e047. [Google Scholar] [CrossRef]
- Saisho, H.; Marcolina, G.; Perucelli, F.; Goulart da Costa, R.; Machado de Souza, E.; Rached, R.N. Fracture Strength, Pull-out Bond Strength, and Volume of Luting Agent of Tooth-Colored CAD-CAM Post-and-Cores. J. Prosthet. Dent. 2023, 129, 599–606. [Google Scholar] [CrossRef]
- Gontijo, I.G.; Ferretti, M.A.; Monteiro, L.C.; Caldas, R.A.; Pecorari, V.G.A.; França, F.M.G.; Aguiar, F.H.B. Influence of Alveolar Bone Height on the Biomechanical Behavior of Roots Restored with Custom-Made Posts-and-Cores. J. Esthet. Restor. Dent. 2023, 35, 677–686. [Google Scholar] [CrossRef] [PubMed]
- Sugano, K.; Komada, W.; Okada, D.; Miura, H. Evaluation of Composite Resin Core with Prefabricated Polyetheretherketone Post on Fracture Resistance in the Case of Flared Root Canals. Dent. Mater. J. 2020, 39, 924–932. [Google Scholar] [CrossRef]
- Ahmad, S.M.; Dawood, S.N.; Dalloo, G.A.M.; Al-Barazanchi, T.R.H. Evaluation of Mechanical Properties of Different Polyetheretherketone Endodontic Post Systems: An in Vitro Study. BMC Oral Health 2023, 23, 537. [Google Scholar] [CrossRef]
- Kole, S.; Ergun, G. Bond Strength of Various Post-Core Restorations with Different Lengths and Diameters Following Cycle Loading. J. Mech. Behav. Biomed. Mater. 2023, 142, 105804. [Google Scholar] [CrossRef]
- Monteiro, L.C.; Pecorari, V.G.A.; Gontijo, I.G.; Marchi, G.M.; Lima, D.A.N.L.; Aguiar, F.H.B. PEEK and Fiberglass Intra-Radicular Posts: Influence of Resin Cement and Mechanical Cycling on Push-out Bond Strength. Clin. Oral Investig. 2022, 26, 6907–6916. [Google Scholar] [CrossRef]
- Zhao, T.; Jiang, Z.; Ge, Y.; Yin, H.; Yang, Q.; Li, R.; Chen, Z.; Zhang, H.; Liu, X. Mechanical Properties, Biosafety, and Shearing Bonding Strength of Glass Fiber-Reinforced PEEK Composites Used as Post-Core Materials. J. Mech. Behav. Biomed. Mater. 2023, 145, 106047. [Google Scholar] [CrossRef] [PubMed]
- Çulhaoğlu, A.K.; Özkır, S.E.; Şahin, V.; Yılmaz, B.; Kılıçarslan, M.A. Effect of Various Treatment Modalities on Surface Characteristics and Shear Bond Strengths of Polyetheretherketone-Based Core Materials. J. Prosthodont. 2020, 29, 136–141. [Google Scholar] [CrossRef]
- Chen, Z.; Li, Y.; Deng, X.; Wang, X. A Novel Computer-Aided Method to Fabricate a Custom One-Piece Glass Fiber Dowel-and-Core Based on Digitized Impression and Crown Preparation Data: CAD/CAM of Custom One-Piece Glass Fiber Dowel-and-Core. J. Prosthodont. 2014, 23, 276–283. [Google Scholar] [CrossRef]
- Eid, R.Y.; Koken, S.; Baba, N.Z.; Ounsi, H.; Ferrari, M.; Salameh, Z. Effect of Fabrication Technique and Thermal Cycling on the Bond Strength of CAD/CAM Milled Custom Fit Anatomical Post and Cores: An In Vitro Study. J. Prosthodont. 2019, 28, 898–905. [Google Scholar] [CrossRef] [PubMed]
- Salameh, Z.; Ferrari, M.; Skienhe, H.; Ounsi, H.; Eid, R.; Azzam, K. Influence of Adaptation and Adhesion on the Retention of Computer-Aided Design/Computer-Aided Manufacturing Glass Fiber Posts to Root Canal. J. Contemp. Dent. Pract. 2019, 20, 1003–1008. [Google Scholar] [CrossRef]
- Santos Pantaleón, D.; Valenzuela, F.M.; Morrow, B.R.; Pameijer, C.H.; García-Godoy, F. Effect of Ferrule Location with Varying Heights on Fracture Resistance and Failure Mode of Restored Endodontically Treated Maxillary Incisors. J. Prosthodont. 2019, 28, 677–683. [Google Scholar] [CrossRef]
- Fontana, P.; Bohrer, T.; Wandscher, V.; Valandro, L.; Limberger, I.; Kaizer, O. Effect of Ferrule Thickness on Fracture Resistance of Teeth Restored With a Glass Fiber Post or Cast Post. Oper. Dent. 2019, 44, E299–E308. [Google Scholar] [CrossRef]
- Magne, P.; Lazari, P.C.; Carvalho, M.A.; Johnson, T.; Del Bel Cury, A.A. Ferrule-Effect Dominates Over Use of a Fiber Post When Restoring Endodontically Treated Incisors: An In Vitro Study. Oper. Dent. 2017, 42, 396–406. [Google Scholar] [CrossRef] [PubMed]
- Stavridakis, M.; Brokos, Y.; Krejci, I. Is the Glass Half Empty or Half Full? A Novel “Philosophical” Approach to the “Mystery” of the so-Called Ferrule Effect. Med. Hypotheses 2018, 115, 35–41. [Google Scholar] [CrossRef]
- Mishra, L.; Khan, A.S.; Velo, M.M.d.A.C.; Panda, S.; Zavattini, A.; Rizzante, F.A.P.; Arbildo Vega, H.I.; Sauro, S.; Lukomska-Szymanska, M. Effects of Surface Treatments of Glass Fiber-Reinforced Post on Bond Strength to Root Dentine: A Systematic Review. Materials 2020, 13, 1967. [Google Scholar] [CrossRef]
- Attia, M.A.; Shokry, T.E.; Abdel-Aziz, M. Effect of Different Surface Treatments on the Bond Strength of Milled Polyetheretherketone Posts. J. Prosthet. Dent. 2022, 127, 866–874. [Google Scholar] [CrossRef] [PubMed]
- Hallak, A.G.; Caldas, R.A.; Silva, I.D.; Miranda, M.E.; Brandt, W.C.; Vitti, R.P. Stress Distribution in Restorations with Glass Fiber and Polyetheretherketone Intraradicular Posts: An in Silico Analysis. Dent. Mater. J. 2022, 41, 376–381. [Google Scholar] [CrossRef]
- Pourkhalili, H.; Maleki, D. Fracture Resistance of Polyetheretherketone, Ni-Cr, and Fiberglass Postcore Systems: An in Vitro Study. Dent. Res. J. 2022, 19, 20. [Google Scholar] [CrossRef]
- Haralur, S.B. Fracture Resistance of Endodontically Treated Teeth Restored with Various Esthetic Posts. Technol. Health Care 2021, 29, 243–252. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, R.O.; Al-Zahawi, A.R.; Sabri, L.A. Mechanical and Thermal Stress Evaluation of PEEK Prefabricated Post with Different Head Design in Endodontically Treated Tooth: 3D-Finite Element Analysis. Dent. Mater. J. 2021, 40, 508–518. [Google Scholar] [CrossRef] [PubMed]
- Özarslan, M.; Büyükkaplan, U.Ş.; Özarslan, M.M. Comparison of the Fracture Strength of Endodontically Treated Teeth Restored with Polyether Ether Ketone, Zirconia and Glass-Fibre Post-Core Systems. Int. J. Clin. Pract. 2021, 75, e14440. [Google Scholar] [CrossRef] [PubMed]
- Benli, M.; Eker Gümüş, B.; Kahraman, Y.; Huck, O.; Özcan, M. Surface Characterization and Bonding Properties of Milled Polyetheretherketone Dental Posts. Odontology 2020, 108, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Hasselbeck, D.; Unkovskiy, A.; Sharghi, F.; Spintzyk, S. Retentive Characteristics of a Polyetheretherketone Post-Core Restoration with Polyvinylsiloxane Attachments. Polymers 2020, 12, 2005. [Google Scholar] [CrossRef]
- Nahar, R.; Mishra, S.K.; Chowdhary, R. Evaluation of Stress Distribution in an Endodontically Treated Tooth Restored with Four Different Post Systems and Two Different Crowns—A Finite Element Analysis. J. Oral Biol. Craniofacial Res. 2020, 10, 719–726. [Google Scholar] [CrossRef]
- Tekin, S.; Adiguzel, O.; Cangul, S.; Atas, O.; Erpacal, B. Evaluation of the Use of PEEK Material in Post-Core and Crown Restorations Using Finite Element Analysis. Am. J. Dent. 2020, 33, 251–257. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).