Assessment of Microhardness of Conventional and Bulk-Fill Resin Composites Using Different Light-Curing Intensity
Abstract
1. Introduction
2. Materials and Methods
2.1. Tested Materials and Light-Curing Protocols
2.2. Specimen Preparation
2.3. Microhardness Measurement Protocol
2.4. Statistical Analysis
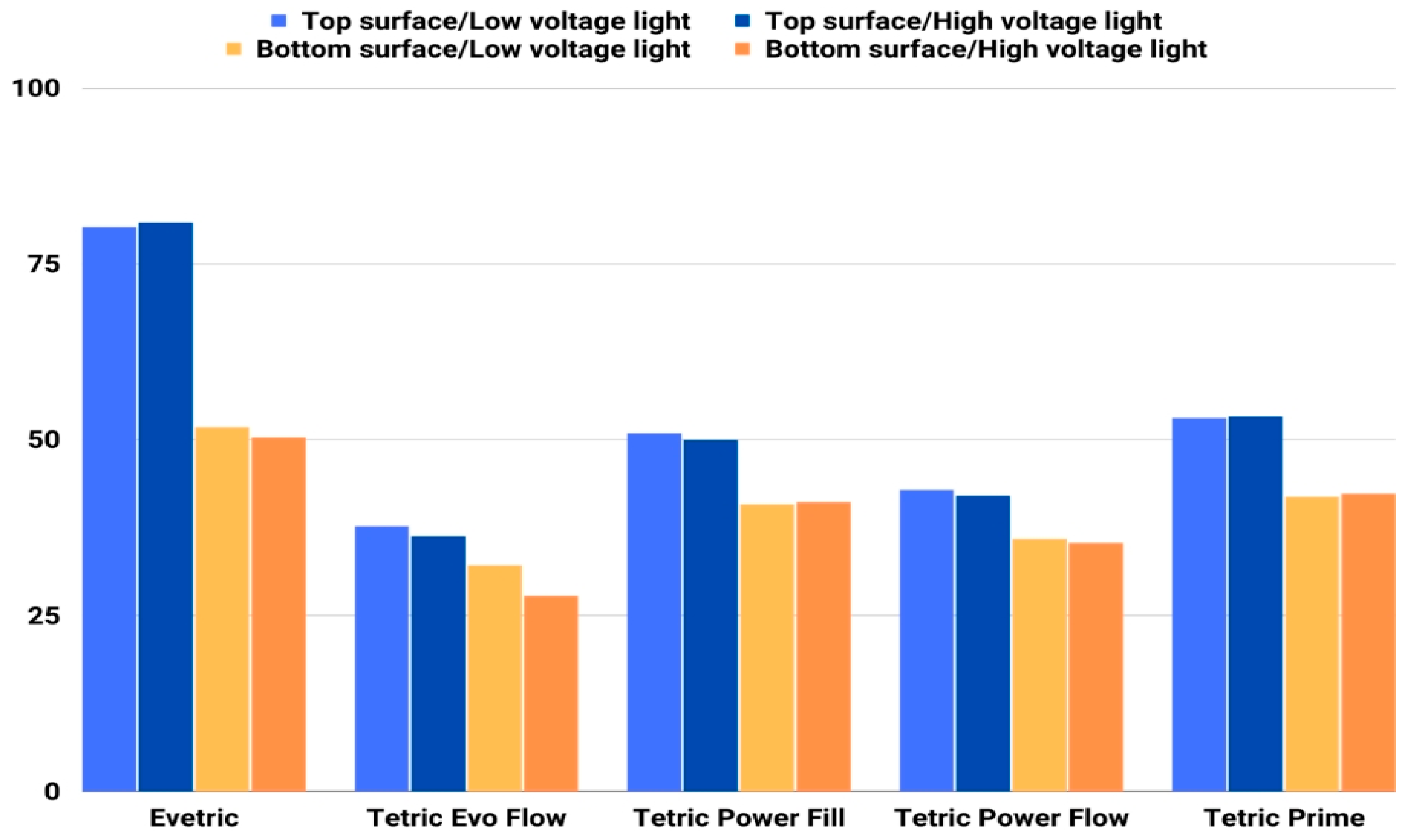
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yeşil Acar, Z.; Tunç Koçyiğit, M.; Asiltürk, M. Investigation of the Effect of Matrix-Interface Formed with Silane-Based Coupling Agents on Physico-Chemical Behavior and Flow Distance of Dental Composites. J. Mol. Liq. 2023, 378, 121600. [Google Scholar] [CrossRef]
- Cho, K.; Rajan, G.; Farrar, P.; Prentice, L.; Prusty, B.G. Dental Resin Composites: A Review on Materials to Product Realizations. Compos. Part B Eng. 2022, 230, 109495. [Google Scholar] [CrossRef]
- Georgiev, G.; Dikova, T. Hardness Investigation of Conventional, Bulk Fill and Flowable Dental Composites. J. Achiev. Mater. Manuf. Eng. 2021, 109, 68–77. [Google Scholar] [CrossRef]
- Anusavice, K. Chapter 18—Dental Ceramics. In Phillips’ Science of Dental Materials; Anusavice, K.J., Shen, C., Rawls, H.R., Eds.; Saunders: St. Louis, MO, USA, 2013; pp. 418–473. [Google Scholar]
- Sherwood, I. Introduction to Dental Materials. In Materials in Restorative Dentistry; Jaypee Brothers: New Delhi, India, 2010. [Google Scholar]
- Zhou, X.; Huang, X.; Li, M.; Peng, X.; Wang, S.; Zhou, X.; Cheng, L. Development and Status of Resin Composite as Dental Restorative Materials. J. Appl. Polym. Sci. 2019, 136, 48180. [Google Scholar] [CrossRef]
- Rodríguez, H.A.; Kriven, W.M.; Casanova, H. Development of Mechanical Properties in Dental Resin Composite: Effect of Filler Size and Filler Aggregation State. Mater. Sci. Eng. C 2019, 101, 274–282. [Google Scholar] [CrossRef]
- Yang, D.L.; Sun, Q.; Niu, H.; Wang, R.L.; Wang, D.; Wang, J.X. The Properties of Dental Resin Composites Reinforced with Silica Colloidal Nanoparticle Clusters: Effects of Heat Treatment and Filler Composition. Compos. Part B Eng. 2020, 186, 107791. [Google Scholar] [CrossRef]
- Cho, K.; Sul, J.H.; Stenzel, M.H.; Farrar, P.; Prusty, B.G. Experimental Cum Computational Investigation on Interfacial and Mechanical Behavior of Short Glass Fiber Reinforced Dental Composites. Compos. Part B Eng. 2020, 200, 108294. [Google Scholar] [CrossRef]
- Aminoroaya, A.; Neisiany, R.E.; Khorasani, S.N.; Panahi, P.; Das, O.; Madry, H.; Cucchiarini, M.; Ramakrishna, S. A Review of Dental Composites: Challenges, chemistry aspects, filler influences, and future insights. Compos. Part B. 2021, 216, 108852. [Google Scholar] [CrossRef]
- Behl, S.; Farahani, A.D.; Raju; Rajan, G.; Ellakwa, A.; Farrar, P.; Thordarson, P.; Prusty, B.G. Evaluation of rheological behaviour of flowable dental composites reinforced with low aspect ratio micro-sized glass fibres. Dent Mater. 2021, 37, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Raju, R.; Rajan, G.; Farrar, P.; Prusty, B.G. Dimensional Stability of Short Fibre Reinforced Flowable Dental Composites. Sci. Rep. 2021, 11, 4697. [Google Scholar] [CrossRef]
- Buelvas, D.D.A.; Besegato, J.F.; Vicentin, B.L.S.; Jussiani, E.I.; Hoeppner, M.G.; Andrello, A.C.; Di Mauro, E. Impact of light-cure protocols on the porosity and shrinkage of commercial bulk fill dental resin composites with different flowability. J. Polym. Res. 2020, 27, 292. [Google Scholar] [CrossRef]
- Kobayashi, S.; Nakajima, M.; Furusawa, K.; Tichy, A.; Hosaka, K.; Tagami, J. Color Adjustment Potential of Single-Shade Resin Composite to Various-Shade Human Teeth: Effect of Structural Color Phenomenon. Dent. Mater. J. 2021, 40, 1033–1040. [Google Scholar] [CrossRef]
- Salas, M.; Lucena, C.; Herrera, L.J.; Yebra, A.; Della Bona, A.; Pérez, M.M. Translucency Thresholds for Dental Materials. Dent. Mater. 2018, 34, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Cândea Ciurea, A.; Şurlin, P.; Stratul, Ş.I.; Soancă, A.; Roman, A.; Moldovan, M.; Tudoran, B.L.; Pall, E. Evaluation of the biocompatibility of resin composite-based dental materials with gingival mesenchymal stromal cells. Microsc. Res. Tech. 2019, 82, 1768–1778. [Google Scholar] [CrossRef] [PubMed]
- Shahi, S.; Özcan, M.; Maleki Dizaj, S.; Sharifi, S.; Al-Haj Husain, N.; Eftekhari, A.; Ahmadian, E. A Review on Potential Toxicity of Dental Material and Screening Their Biocompatibility. Toxicol. Mech. Methods 2019, 29, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Dikova, T.; Maximov, J.; Todorov, V.; Georgiev, G.; Panov, V. Optimization of Photopolymerization Process of Dental Composites. Processes 2021, 9, 779. [Google Scholar] [CrossRef]
- Baloš, S.; Pilić, B.; Petronijević, B.; Marković, D.; Mirković, S.; Šarčev, I. Improving mechanical properties of flowable dental composite resin by adding silica nanoparticles. Vojnosanit. Pregl. 2013, 70, 477–483. [Google Scholar] [CrossRef]
- Chen, H.; Wang, R.; Qian, L.; Liu, H.; Wang, J.; Zhu, M. Surface Modification of Urchin-like Serried Hydroxyapatite with Sol-Gel Method and Its Application in Dental Composites. Compos. Part B Eng. 2020, 182, 107621. [Google Scholar] [CrossRef]
- Wang, Y.; Hua, H.; Liu, H.; Zhu, M.; Zhu, X.X. Surface Modification of ZrO2Nanoparticles and Its Effects on the Properties of Dental Resin Composites. ACS Appl. Bio. Mater. 2020, 3, 5300–5309. [Google Scholar] [CrossRef]
- Shah, P.K.; Stansbury, J.W. Photopolymerization Shrinkage-Stress Reduction in Polymer-Based Dental Restoratives by Surface Modification of Fillers. Dent. Mater. 2021, 37, 578–587. [Google Scholar] [CrossRef]
- Cho, K.; Wang, G.; Raju; Fang, J.; Rajan, G.; Stenzel, M.H.; Farrar, P.; Prusty, B.G. Selective Atomic-Level Etching on Short S-Glass Fibres to Control Interfacial Properties for Restorative Dental Composites. Sci. Rep. 2019, 9, 3851. [Google Scholar] [CrossRef] [PubMed]
- Tian, K.V.; Nagy, P.M.; Chass, G.A.; Fejerdy, P.; Nicholson, J.W.; Csizmadia, I.G.; Dobó-Nagy, C. Qualitative Assessment of Microstructure and Hertzian Indentation Failure in Biocompatible Glass Ionomer Cements. J. Mater. Sci. Mater. Med. 2012, 23, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Araújo, J.L.N.; de Melo Alencar, C.; Barbosa, G.M.; Silva, C.M.; Turbino, M.L. Effect of LEDs with Different Wavelengths on the Microhardness and Nanohardness of Nanohybrid Composite Resins. J. Contemp. Dent. Pract. 2021, 22, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Miletic, V.; Pongprueksa, P.; De Munck, J.; Brooks, N.R.; Van Meerbeek, B. Curing Characteristics of Flowable and Sculptable Bulk-Fill Composites. Clin. Oral Investig. 2017, 21, 1201–1212. [Google Scholar] [CrossRef]
- Son, S.A.; Park, J.K.; Seo, D.G.; Ko, C.C.; Kwon, Y.H. How Light Attenuation and Filler Content Affect the Microhardness and Polymerization Shrinkage and Translucency of Bulk-Fill Composites? Clin. Oral Investig. 2017, 21, 559–565. [Google Scholar] [CrossRef]
- Tomaszewska, I.M.; Kearns, J.O.; Ilie, N.; Fleming, G.J.P. Bulk Fill Restoratives: To Cap or Not to Cap—That Is the Question? J. Dent. 2015, 43, 309–316. [Google Scholar] [CrossRef]
- Rosatto, C.M.P.; Bicalho, A.A.; Veríssimo, C.; Bragança, G.F.; Rodrigues, M.P.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Mechanical Properties, Shrinkage Stress, Cuspal Strain and Fracture Resistance of Molars Restored with Bulk-Fill Composites and Incremental Filling Technique. J. Dent. 2015, 43, 1519–1528. [Google Scholar] [CrossRef]
- Van Ende, A.; De Munck, J.; Van Landuyt, K.L.; Poitevin, A.; Peumans, M.; Van Meerbeek, B. Bulk-Filling of High C-Factor Posterior Cavities: Effect on Adhesion to Cavity-Bottom Dentin. Dent. Mater. 2013, 29, 269–277. [Google Scholar] [CrossRef]
- Van Ende, A.; Lise, D.P.; De Munck, J.; Vanhulst, J.; Wevers, M.; Van Meerbeek, B. Strain Development in Bulk-Filled Cavities of Different Depths Characterized Using a Non-Destructive Acoustic Emission Approach. Dent. Mater. 2017, 33, e165–e177. [Google Scholar] [CrossRef]
- Fronza, B.M.; Rueggeberg, F.A.; Braga, R.R.; Mogilevych, B.; Soares, L.E.S.; Martin, A.A.; Ambrosano, G.; Giannini, M. Monomer Conversion, Microhardness, Internal Marginal Adaptation, and Shrinkage Stress of Bulk-Fill Resin Composites. Dent. Mater. 2015, 31, 1542–1551. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Jäger, F.; Attin, T. Polymerization Shrinkage and Shrinkage Force Kinetics of High- and Low-Viscosity Dimethacrylate- and Ormocer-Based Bulk-Fill Resin Composites. Odontology 2019, 107, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Clinical performance and chemical-physical properties of bulk fill composites resin—A systematic review and meta-analysis. Dent. Mater. 2019, 35, e249–e264. [CrossRef] [PubMed]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Marcos, A.; Salazar-Correa, G.; Castro-Ramirez, L.; Ladera-Castañeda, M.; López-Gurreonero, C.; Cachay-Criado, H.; Aliaga-Mariñas, A.; Cornejo-Pinto, A.; Cervantes-Ganoza, L.; Cayo-Rojas, C.F. The Microhardness and Surface Roughness Assessment of Bulk-Fill Resin Composites Treated with and without the Application of an Oxygen-Inhibited Layer and a Polishing System: An In Vitro Study. Polymers 2022, 14, 3053. [Google Scholar] [CrossRef]
- Vivadent Ivoclar Tetric EvoCeram Bulk Fill. Instructions for Use. Available online: http://www.ivoclarvivadent.com/en-us/composites/restorative-materials/tetricevocerambulk-fill (accessed on 21 November 2022).
- Cayo, C.; Llancari, L.; Mendoza, R.; Cervantes, L. Marginal filling and adhesive resistance of bulk fill resin applying 18% edta gel compared with 37% phosphoric acid gel in vitro dental conditioning. J. Oral Res. 2019, 8, 228–235. [Google Scholar] [CrossRef]
- Marovic, D.; Panduric, V.; Tarle, Z.; Ristic, M.; Sariri, K.; Demoli, N.; Klaric, E.; Jankovic, B.; Prskalo, K. Degree of Conversion and Microhardness of Dental Composite Resin Materials. J. Mol. Struct. 2013, 1044, 299–302. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin Composite—State of the Art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Rencz, A.; Hickel, R.; Ilie, N. Curing efficiency of modern LED units. Clin. Oral Investig. 2012, 16, 173–179. [Google Scholar] [CrossRef]
- Aguiar, F.H.; Lazzari, C.R.; Lima, D.A.; Ambrosano, G.M.; Lovadino, J.R. Effect of light curing tip distance and resin shade on microhardness of a hybrid resin composite. Braz. Oral Res. 2005, 19, 302–306. [Google Scholar] [CrossRef]
- Cekic-Nagas, I.; Egilmez, F.; Ergun, G. The effect of irradiation distance on microhardness of resin composites cured with different light curing units. Eur. J. Dent. 2010, 4, 440–446. [Google Scholar] [CrossRef]
- Ilie, N.; Watts, D.C. Outcomes of ultra-fast (3 s) photo-cure in a RAFT-modified resin-composite. Dent. Mater. 2020, 36, 570–579. [Google Scholar] [CrossRef] [PubMed]
- Tauböck, T.T.; Feilzer, A.J.; Buchalla, W.; Kleverlaan, C.J.; Krejci, I.; Attin, T. Effect of modulated photo-activation on polymerization shrinkage behavior of dental restorative resin composites. Eur. J. Oral Sci. 2014, 122, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Santini, A.; Miletic, V.; Swift, M.D.; Bradley, M. Degree of Conversion and Microhardness of TPO-Containing Resin-Based Composites Cured by Polywave and Monowave LED Units. J. Dent. 2012, 40, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Porto, I.C.; Soares, L.E.; Martin, A.A.; Cavalli, V.; Liporoni, P.C. Influence of the photoinitiator system and light photoactivation units on the degree of conversion of dental composites. Braz. Oral Res. 2012, 24, 475–481. [Google Scholar] [CrossRef]
- Mousavinasab, S.M.; Meyers, I. Comparison of Depth of Cure, Hardness and Heat Generation of LED and High Intensity QTH Light Sources. Eur. J. Dent. 2011, 5, 299–304. [Google Scholar] [CrossRef]
- Ceballos, L.; Fuentes, M.V.; Tafalla, H.; Martínez, A.; Flores, J.; Rodríguez, J. Curing effectiveness of resin composites at different exposure times using LED and halogen units. Med. Oral Patol. Oral Cir. Buccal 2009, 14, E51–E56. [Google Scholar]
- Alpöz, A.R.; Ertugrul, F.; Cogulu, D.; Ak, A.T.; Tanoglu, M.; Kaya, E. Effects of light curing method and exposure time on mechanical properties of resin based dental materials. Eur. J. Dent. 2008, 2, 37–42. [Google Scholar] [CrossRef]
- Hosseinalipour, M.; Javadpour, J.; Rezaie, H.; Dadras, T.; Hayati, A.N. Investigation of mechanical properties of experimental Bis-GMA/TEGDMA dental composite resins containing various mass fractions of silica nanoparticles. J. Prosthodont. 2010, 19, 112–117. [Google Scholar] [CrossRef]
- Gladwin, M.A.; Bagby, M.D. Chapter 5: Direct Polymeric Restorative Materials. In Clinical Aspects of Dental Materials: Theory, Practice and Cases, 3rd ed.; Wolters Kluwer—Lippincott Williams & Wilkins: Baltimore, MD, USA, 2009. [Google Scholar]
- Colombo, M.; Gallo, S.; Poggio, C.; Ricaldone, V.; Arciola, C.R.; Scribante, A. New Resin-Based Bulk-Fill Composites: In vitro Evaluation of Micro-Hardness and Depth of Cure as Infection Risk Indexes. Materials 2020, 13, 1308. [Google Scholar] [CrossRef]
- Available online: https://pdf.medicalexpo.com/pdf/ivoclar-vivadent-72878.html (accessed on 21 November 2022).
- Par, M.; Marovic, D.; Attin, T.; Tarle, Z.; Tauböck, T.T. The effect of rapid high-intensity light-curing on micromechanical properties of bulk-fill and conventional resin composites. Sci. Rep. 2020, 10, 10560. [Google Scholar] [CrossRef]
- Gurbuz, O.; Cilingir, A.; Dikmen, B.; Ozsoy, A.; Mert, M. Effect of surface sealant on the surface roughness of different composites and evaluation of their microhardness. Eur. Oral Res. 2020, 54, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gantz, L.; Fauxpoint, G.; Arntz, Y.; Pelletier, H.; Etienne, O. In vitro comparison of the surface roughness of polymethyl methacrylate and bis-acrylic resins for interim restorations before and after polishing. J. Prosthet. Dent. 2021, 125, 833.e1–833.e10. [Google Scholar] [CrossRef]
- Aydın, N.; Topçu, F.T.; Karaoğlanoğlu, S.; Oktay, E.; Erdemir, U. Effect of finishing and polishing systems on the surface roughness and color change of composite resins. J. Clin. Exp. Dent. 2021, 13, e446–e454. [Google Scholar] [CrossRef]
- Asmussen, E.; Peutzfeldt, A. Influence of pulse-delay curing on softening of polymer structures. J. Dent. Res. 2001, 80, 1570–1573. [Google Scholar] [CrossRef] [PubMed]
- Benetti, A.R.; Asmussen, E.; Munksgaard, E.C.; Dewaele, M.; Peutzfeldt, A.; Leloup, G.; Devaux, J. Softening and elution of monomers in ethanol. Dent. Mater. 2009, 25, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Brandt, W.C.; de Moraes, R.R.; Correr-Sobrinho, L.; Sinhoreti, M.A.; Consani, S. Effect of different photo-activation methods on push out force, hardness and cross-link density of resin composite restorations. Dent. Mater. 2008, 24, 846–850. [Google Scholar] [CrossRef]
- Dewaele, M.; Asmussen, E.; Peutzfeldt, A.; Munksgaard, E.C.; Benetti, A.R.; Finné, G.; Leloup, G.; Devaux, J. Influence of curing protocol on selected properties of light-curing polymers: Degree of conversion, volume contraction, elastic modulus, and glass transition temperature. Dent. Mater. 2009, 25, 1576–1584. [Google Scholar] [CrossRef]
- Cavalcante, L.M.; Schneider, L.F.; Silikas, N.; Watts, D.C. Surface integrity of solvent-challenged ormocer-matrix composite. Dent. Mater. 2011, 27, 173–179. [Google Scholar] [CrossRef]
- Lovell, L.G.; Lu, H.; Elliott, J.E.; Stansbury, J.W.; Bowman, C.N. The effect of cure rate on the mechanical properties of dental resins. Dent. Mater. 2001, 17, 504–511. [Google Scholar] [CrossRef]
- Par, M.; Repusic, I.; Skenderovic, H.; Milat, O.; Spajic, J.; Tarle, Z. The effects of extended curing time and radiant energy on microhardness and temperature rise of conventional and bulk-fill resin composites. Clin. Oral Investig. 2019, 23, 3777–3788. [Google Scholar] [CrossRef]
- Hadis, M.; Leprince, J.G.; Shortall, A.C.; Devaux, J.; Leloup, G.; Palin, W.M. High irradiance curing and anomalies of exposure reciprocity law in resin-based materials. J. Dent. 2011, 39, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.K.; Platt, J.A.; Borges, G.; Chu, T.M.; Katsilieri, I. Depth of cure of dental resin composites: ISO 4049 depth and microhardness of types of materials and shades. Oper. Dent. 2008, 33, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Fujita, K.; Ikemi, T.; Nishiyama, N. Effects of particle size of silica filler on polymerization conversion in a light-curing resin composite. Dent. Mater. 2011, 27, 1079–1085. [Google Scholar] [CrossRef] [PubMed]


| Composite Viscosity | Composite Type | Composite Name | Resin Matrix | Filler Content (wt%/vol%) | Manufacturer |
|---|---|---|---|---|---|
| Sculptable | Conventional | Evetric (EVT) | UDMA, Bis-GMA, Bis-EMA | 80/56 | Ivoclar Vivadent, Schaan, Liechtenstein |
| Tetric Prime (TP) | Bis-GMA, UDMA, Bis-EMA, D3MA | 77/56 | |||
| Bulk-fill | Tetric Power Fill (PFL) | Bis-GMA, Bis-EMA, UDMA, propoxylated bisphenol A dimethacrylate, DCP, β-allyl sulfone AFCT agent | 77/54 | ||
| Flowable | Conventional | Tetric Evo Flow (TEF) | Bis-GMA, UDMA, decandioldimethacrylate | 58/31 | |
| Bulk-fill | Tetric Power Flow (PFW) | Bis-GMA, Bis-EMA, UDMA | 68/46 |
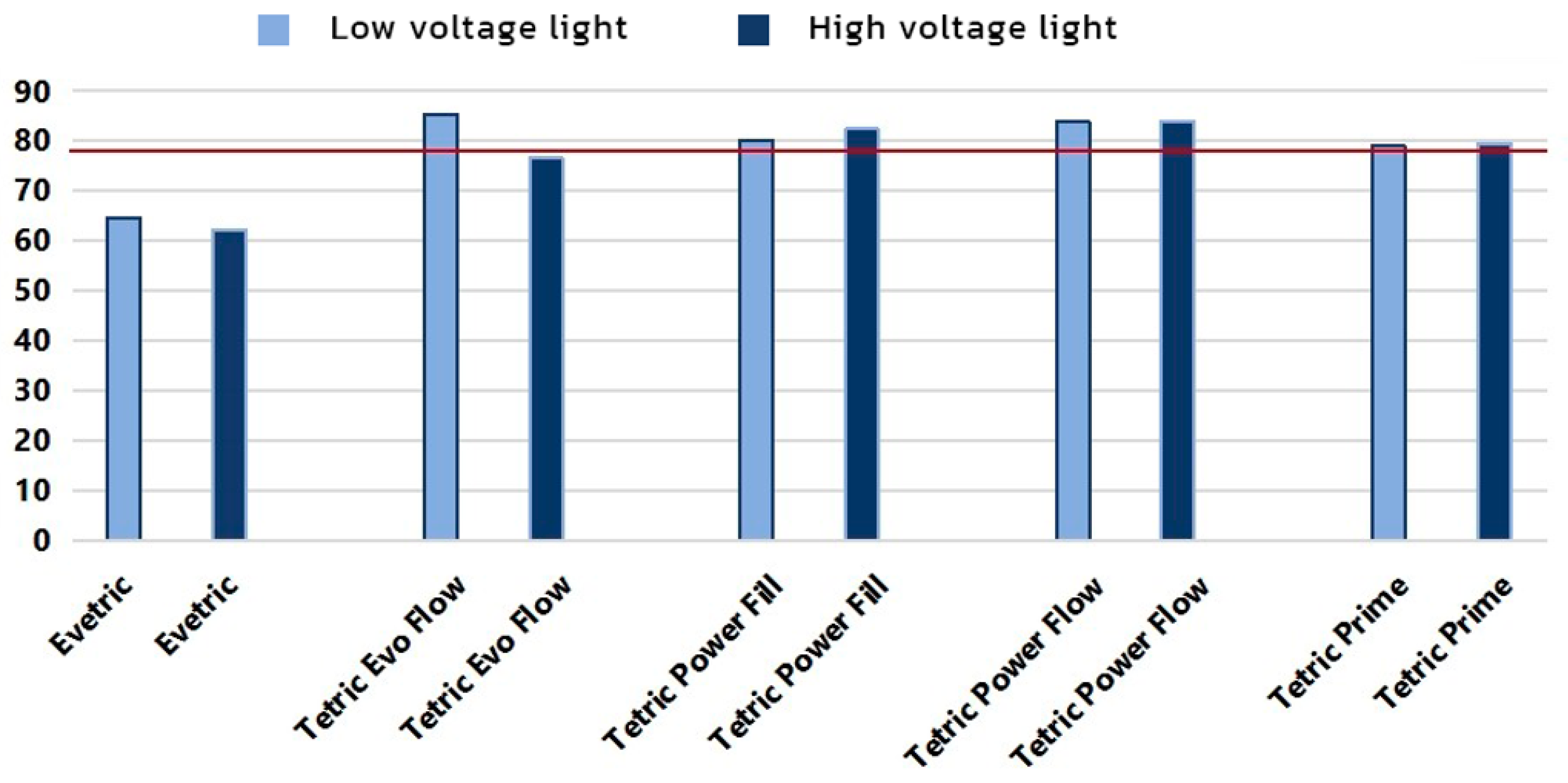
| Variable | Average | Standard Deviation | Min | Max |
|---|---|---|---|---|
| Evetric | 65.73 | 15.15 | 49.10 | 81.70 |
| Tetric Evo Flow | 33.42 | 4.01 | 26.80 | 38.70 |
| Tetric Power Fill | 45.64 | 4.88 | 40.20 | 51.60 |
| Tetric Power Flow | 38.99 | 3.57 | 34.60 | 43.80 |
| Tetric Prime | 47.60 | 5.80 | 40.90 | 55.00 |
| 3 s curing | 46.67 | 13.12 | 31.10 | 81.30 |
| Conventional curing | 45.88 | 13.94 | 26.80 | 81.70 |
| Top surface | 52.65 | 15.21 | 35.60 | 81.70 |
| Bottom surface | 39.90 | 7.25 | 26.80 | 53.60 |
| Top Surface | Bottom Surface | |||
|---|---|---|---|---|
| p | Partial η2 | p | Partial η2 | |
| Material | <0.000 | 0.998 | <0.000 | 0.991 |
| Curing protocol | <0.039 | 0.195 | <0.000 | 0.515 |
| Material × curing protocol | <0.011 | 0.463 | <0.000 | 0.714 |
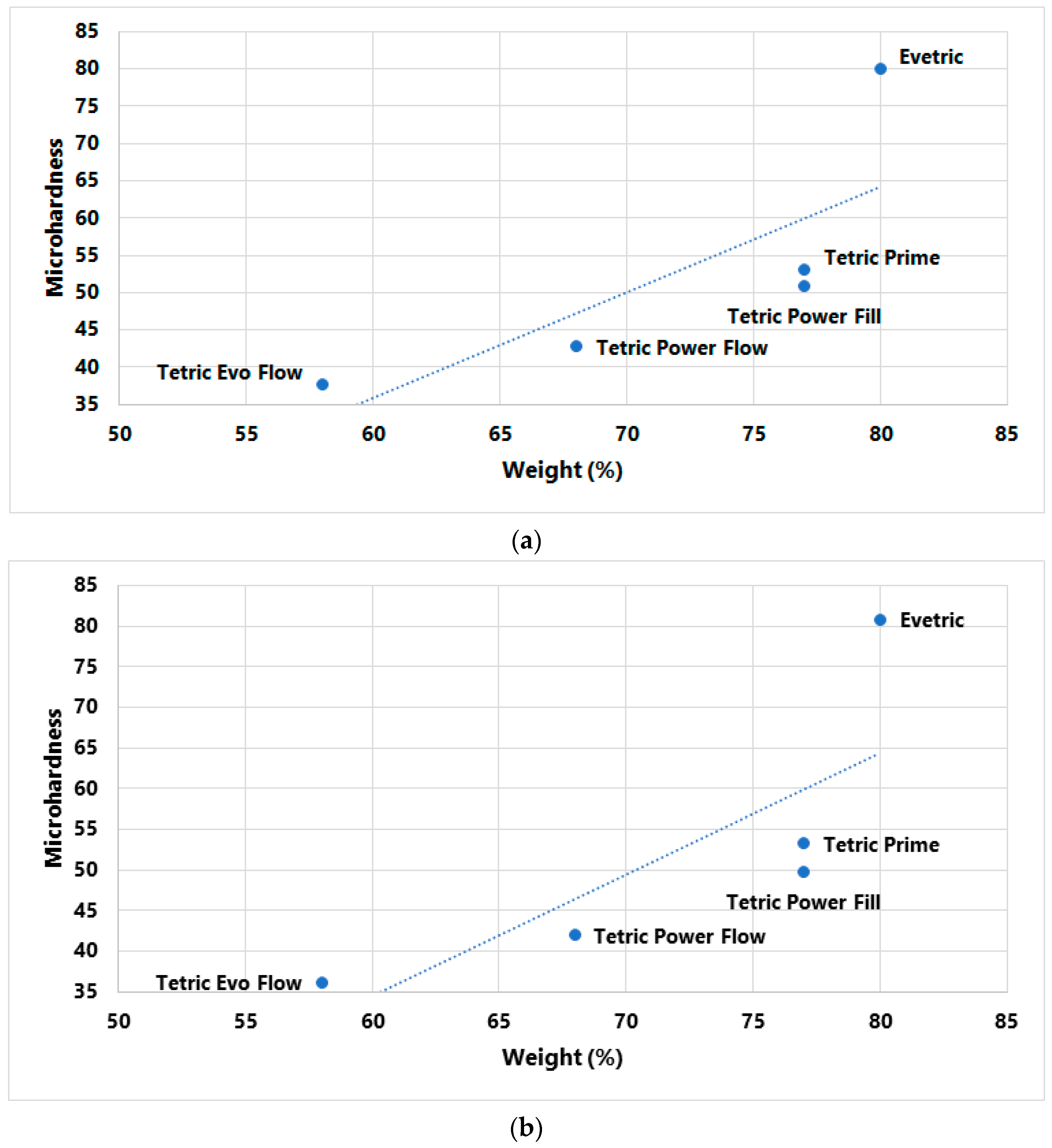
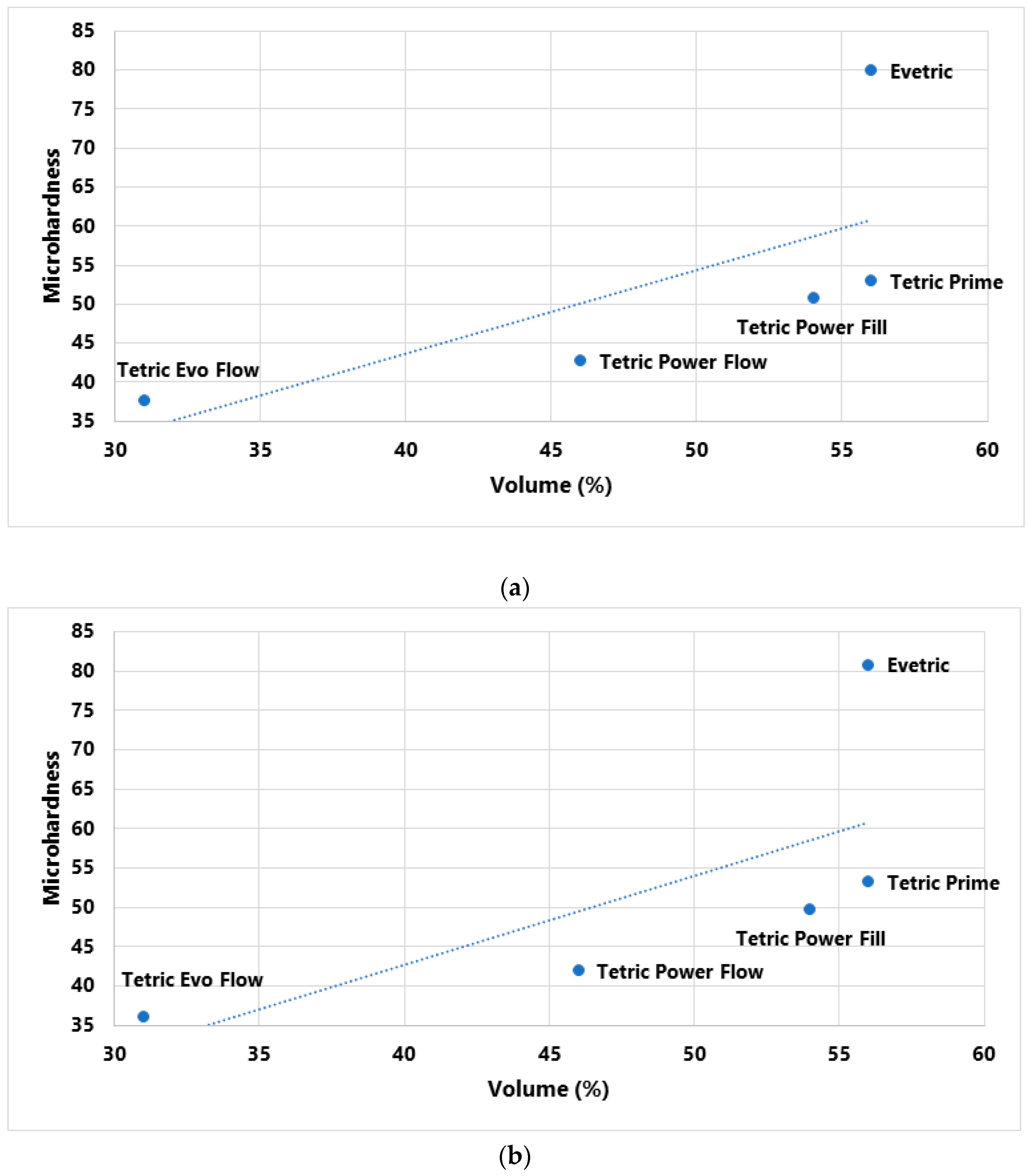
| Filler Content and LV/HV Curing Protocol | p-Value | Correlation Coefficient (R) |
|---|---|---|
| wt% LV protocol | 0.120 | 0.780 |
| wt% HV protocol | 0.117 | 0.783 |
| vol% LV protocol | 0.194 | 0.694 |
| vol% HV protocol | 0.188 | 0.701 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakupović, S.; Pervan, N.; Mešić, E.; Gavranović-Glamoč, A.; Bajsman, A.; Muratović, E.; Kazazić, L.; Kantardžić-Kovačević, A. Assessment of Microhardness of Conventional and Bulk-Fill Resin Composites Using Different Light-Curing Intensity. Polymers 2023, 15, 2250. https://doi.org/10.3390/polym15102250
Jakupović S, Pervan N, Mešić E, Gavranović-Glamoč A, Bajsman A, Muratović E, Kazazić L, Kantardžić-Kovačević A. Assessment of Microhardness of Conventional and Bulk-Fill Resin Composites Using Different Light-Curing Intensity. Polymers. 2023; 15(10):2250. https://doi.org/10.3390/polym15102250
Chicago/Turabian StyleJakupović, Selma, Nedim Pervan, Elmedin Mešić, Alma Gavranović-Glamoč, Anita Bajsman, Enis Muratović, Lejla Kazazić, and Alma Kantardžić-Kovačević. 2023. "Assessment of Microhardness of Conventional and Bulk-Fill Resin Composites Using Different Light-Curing Intensity" Polymers 15, no. 10: 2250. https://doi.org/10.3390/polym15102250
APA StyleJakupović, S., Pervan, N., Mešić, E., Gavranović-Glamoč, A., Bajsman, A., Muratović, E., Kazazić, L., & Kantardžić-Kovačević, A. (2023). Assessment of Microhardness of Conventional and Bulk-Fill Resin Composites Using Different Light-Curing Intensity. Polymers, 15(10), 2250. https://doi.org/10.3390/polym15102250






