The Effect of Morpholine on Composite-to-Composite Repair Strength Contaminated with Saliva
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of Aged Resin Composite
2.2. Surface Contamination and Surface Treatment Protocols
2.3. Saliva Contamination
2.4. Phosphoric Acid Etch
2.5. Morpholine Surface Treatment
2.6. Adhesive Agent Treatment
2.7. Bonding Procedures
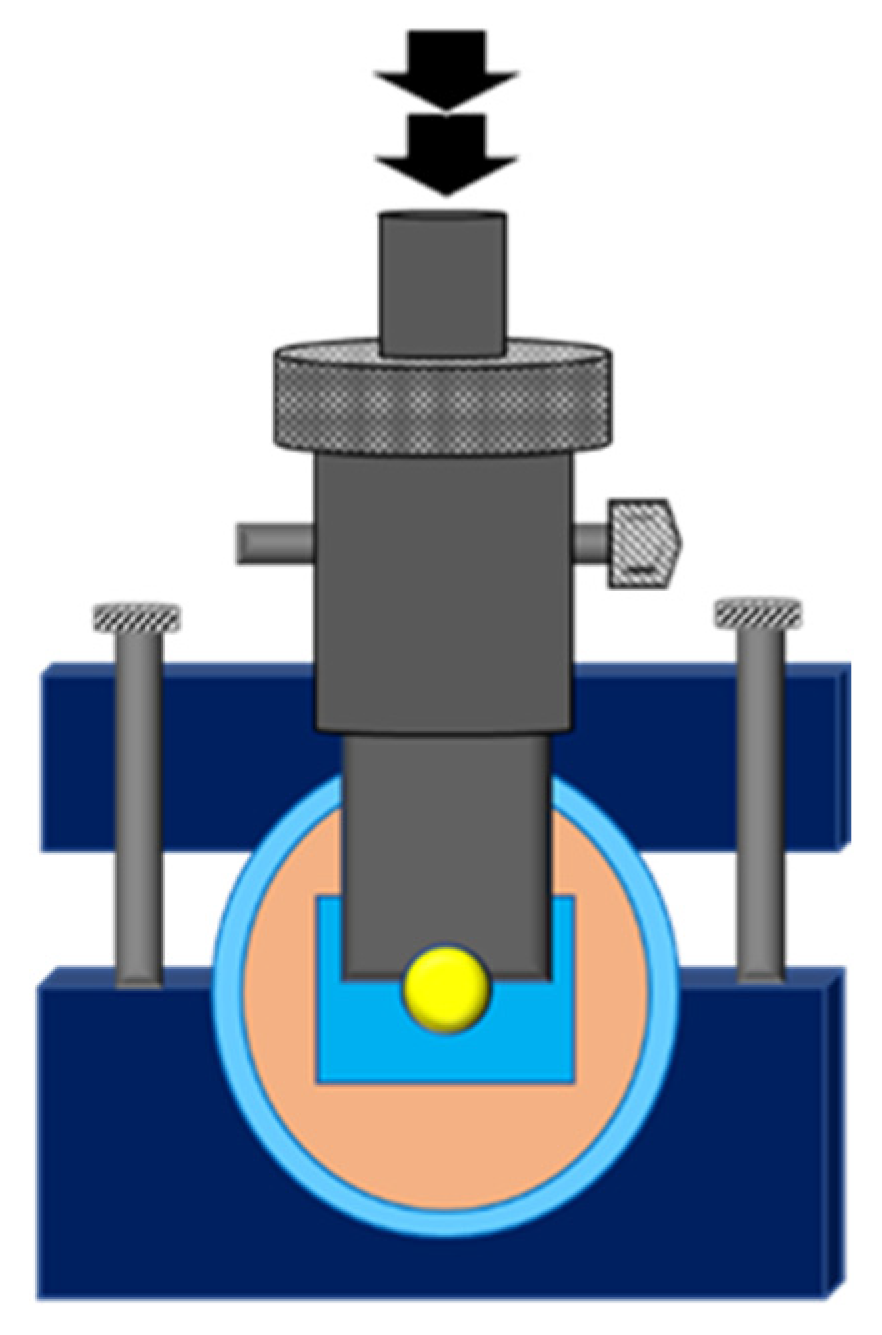
2.8. Shear Bond Strength (SBS) Test
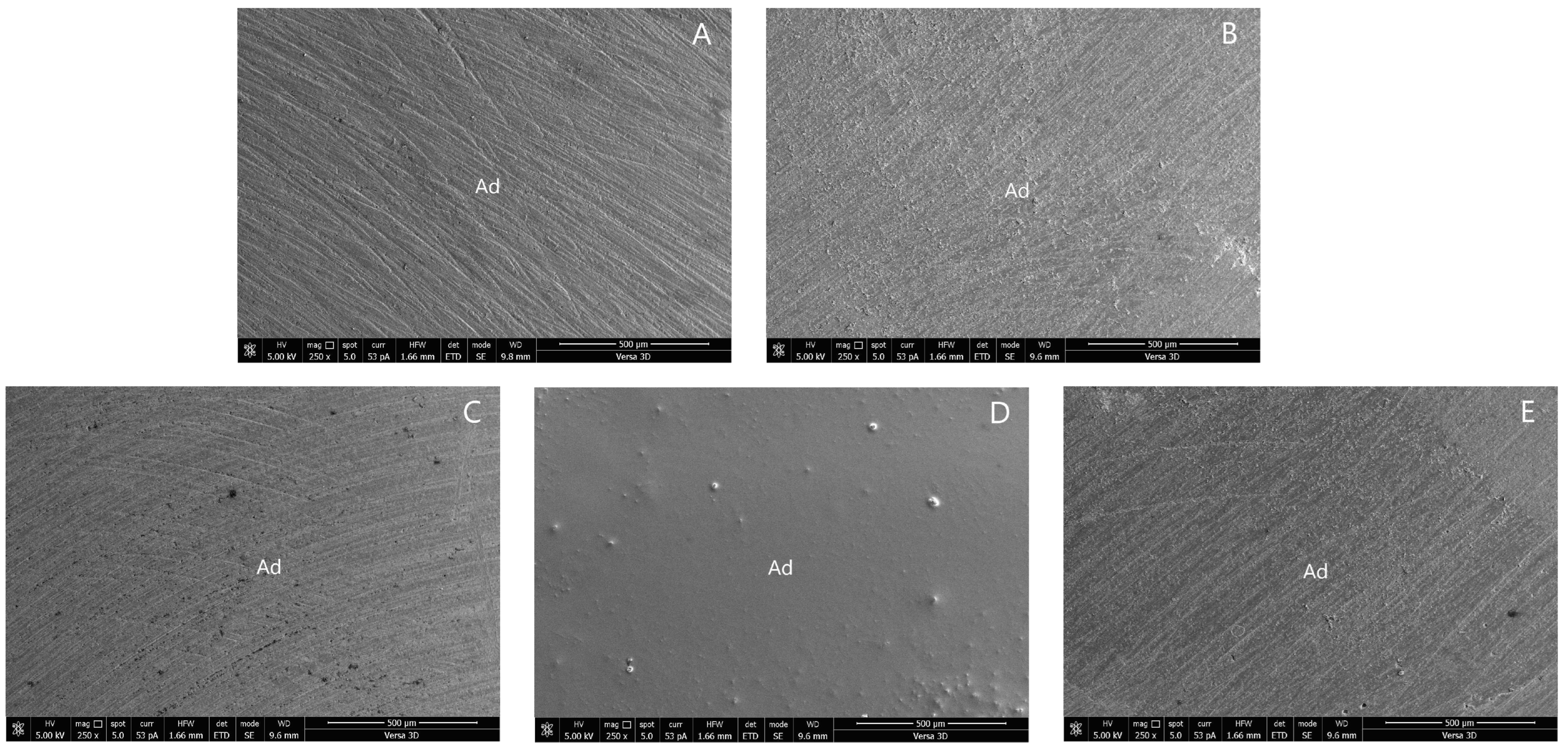
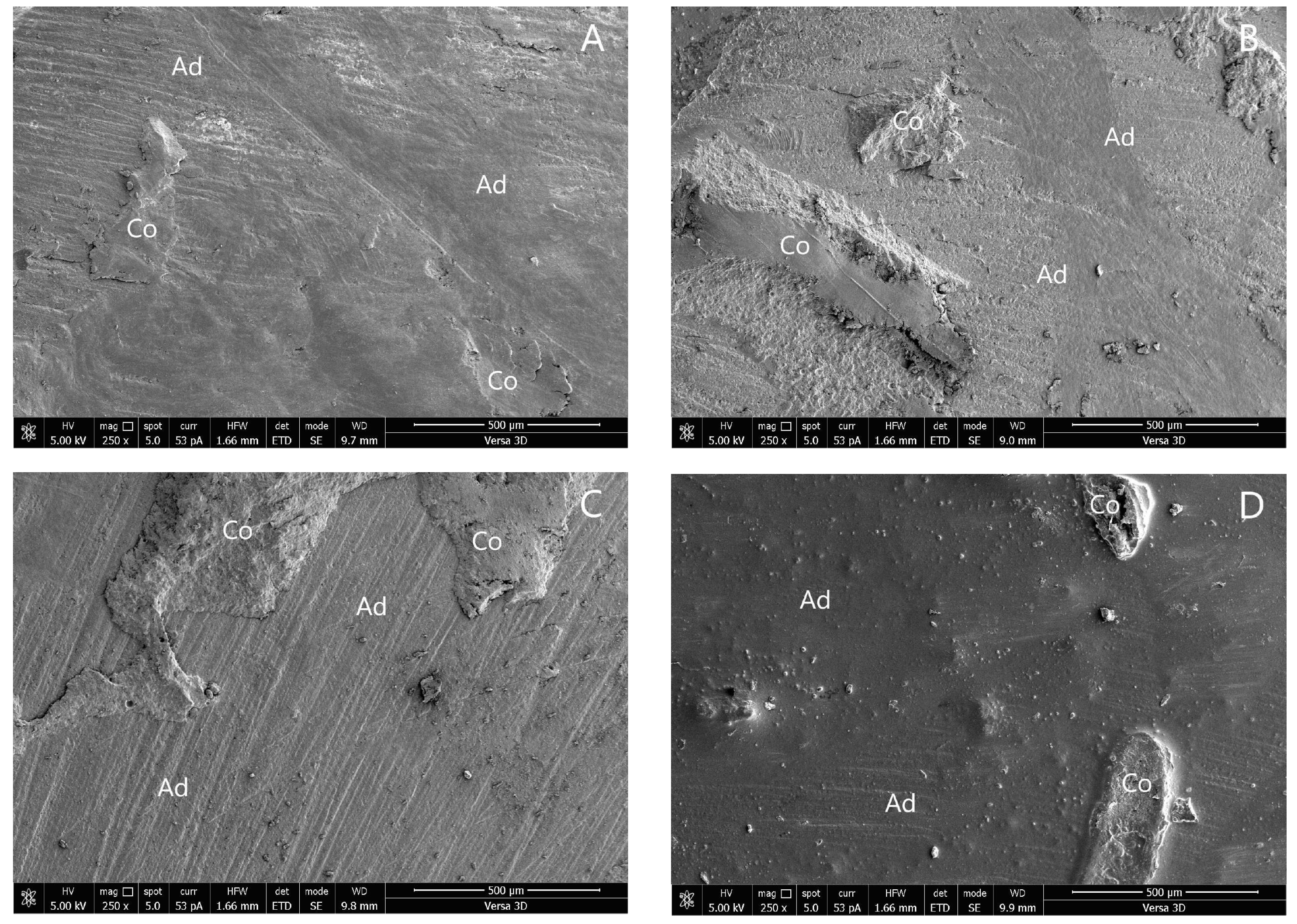
2.9. Failure Mode Analysis
2.10. Statistics Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferracane, J.L. Resin composite—State of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Fernández, E.; Martín, J.; Vildósola, P.; Junior, O.B.O.; Gordan, V.; Major, I.; Bersezio, C.; Estay, J.; de Andrade, M.F.; Moncada, G. Can repair increase the longevity of composite resins? Results of a 10-year clinical trial. J. Dent. 2015, 43, 279–286. [Google Scholar] [CrossRef]
- Momoi, Y.; Hayashi, M.; Fujitani, M.; Fukushima, M.; Imazato, S.; Kubo, S.; Nikaido, T.; Shimizu, A.; Unemori, M.; Yamaki, C. Clinical guidelines for treating caries in adults following a minimal intervention policy—Evidence and consensus based report. J. Dent. 2012, 40, 95–105. [Google Scholar] [CrossRef]
- Altinci, P.; Mutluay, M.; Tezvergil-Mutluay, A. Repair bond strength of nanohybrid composite resins with a universal adhesive. Acta Biomater. Odontol. Scand. 2017, 4, 10–19. [Google Scholar]
- Miletic, V.J.; Santini, A. Remaining unreacted methacrylate groups in resin-based composite with respect to sample preparation and storing conditions using micro-Raman spectroscopy. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 87, 468–474. [Google Scholar] [CrossRef]
- Wendler, M.; Belli, R.; Panzer, R.; Skibbe, D.; Petschelt, A.; Lohbauer, U. Repair bond strength of aged resin composite after different surface and bonding treatments. Materials. 2016, 9, 547. [Google Scholar] [CrossRef]
- Rodrigues, S.A., Jr.; Ferracane, J.L.; Della Bona, A. Influence of surface treatments on the bond strength of repaired resin composite restorative materials. Dent. Mater. 2009, 25, 442–451. [Google Scholar]
- Nassoohi, N.; Kazemi, H.; Sadaghiani, M.; Mansouri, M.; Rakhshan, V. Effects of three surface conditioning techniques on repair bond strength of nanohybrid and nanofilled composites. Dent. Res. J. 2015, 12, 554–561. [Google Scholar]
- Sismanoglu, S. Efficiency of self-adhering flowable resin composite and different surface treatments in composite repair using a universal adhesive. Niger. J. Clin. Pract. 2019, 22, 1675–1679. [Google Scholar]
- Arshad, F.; Khan, M.F.; Akhtar, W.; Alam, M.M.; Nainwal, L.M.; Kaushik, S.K.; Akhter, M.; Parvez, S.; Hasan, S.M.; Shaquiquzzaman, M. Revealing quinquennial anticancer journey of morpholine: A SAR based review. Eur. J. Med. Chem. 2019, 167, 324–356. [Google Scholar]
- Kourounakis, A.P.; Xanthopoulos, D.; Tzara, A. Morpholine as a privileged structure: A review on the medicinal chemistry and pharmacological activity of morpholine containing bioactive molecules. Med. Res. Rev. 2020, 40, 709–752. [Google Scholar] [PubMed]
- Staxrud, F.; Dahl, J.E. Role of bonding agents in the repair of composite resin restorations. Eur. J. Oral. Sci. 2011, 119, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Eliasson, S.T.; Tibballs, J.; Dahl, J.E. Effect of different surface treatments and adhesives on repair bond strength of resin composites after one and 12 months of storage using an improved microtensile test method. Oper. Dent. 2014, 39, E206–E216. [Google Scholar] [CrossRef] [PubMed]
- Loomans, B.A.; Cardoso, M.V.; Roeters, F.J.; Opdam, N.J.M.; de Munck, J.; Huysmans, M.C.D.N.J.M.; van Meerbeek, B. Is there one optimal repair technique for all composites? Dent. Mater. 2011, 27, 701–709. [Google Scholar] [PubMed]
- Klaisiri, A.; Krajangta, N.; Phumpatrakom, P.; Sriamporn, T.; Thamrongananskul, N. The effect of curing mode in universal adhesive on zirconia and resin cement shear bond strength. J. Int. Dent. Med. Res. 2021, 14, 896–900. [Google Scholar]
- Klaisiri, A.; Krajangta, N.; Thamrongananskul, N. The durability of zirconia/resin composite shear bond strength using different functional monomer of universal adhesives. Eur. J. Dent. 2021; online ahead of print. [Google Scholar] [CrossRef]
- Sriamporn, T.; Thamrongananskul, N.; Klaisiri, A. The effectiveness of various functional monomers in self-adhesive resin cements on prosthetic materials. J. Int. Soc. Prevent. Communit. Dent. 2022, 12, 332–335. [Google Scholar]
- Matinlinna, J.P.; Lassila, L.V. Enhanced resin-composite bonding to zirconia framework after pretreatment with selected silane monomers. Dent. Mater. 2011, 27, 273–280. [Google Scholar]
- Klaisiri, A.; Maneenacarith, A.; Jirathawornkul, N.; Suthamprajak, P.; Sriamporn, T.; Thamrongananskul, N. The effect of multiple applications of phosphate-containing primer on shear bond strength between zirconia and resin composite. Polymers 2022, 14, 4174. [Google Scholar]
- Sideridou, I.D.; Karabela, M.M.; Bikiaris, D.N. Aging studies of light cured dimethacrylate-based dental resins and a resin composite in water or ethanol/water. Dent. Mater. 2007, 23, 1142–1149. [Google Scholar] [CrossRef]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Barbosa, S.H.; Melo, R.M.; Galhano, G.A.; Bottino, M.A. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent. Mater. 2007, 23, 1276–1282. [Google Scholar] [PubMed]
- Rinastiti, M.; Özcan, M.; Siswomihardjo, W.; Busscher, H.J. Effects of surface conditioning on repair bond strengths of non-aged and aged microhybrid, nanohybrid, and nanofilled composite resins. Clin. Oral. Investig. 2011, 15, 625–633. [Google Scholar] [CrossRef] [PubMed]
- Jafarzadeh Kashi, T.S.; Erfan, M.; Rakhshan, V.; Aghabaigi, N.; Tabatabaei, F.S. An in vitro assessment of the effects of three surface treatments on repair bond strength of aged composites. Oper. Dent. 2011, 36, 608–617. [Google Scholar] [CrossRef]
- Eiriksson, S.O.; Pereira, P.N.; Swift, E.J., Jr.; Heymann, H.O.; Sigurdsson, A. Effects of saliva contamination on resin-resin bond strength. Dent. Mater. 2004, 20, 37–44. [Google Scholar] [CrossRef]
- Furuse, Y.; da Cunha, L.F.; Benetti, A.R.; Mondelli, J. Bond strength of resin-resin interfaces contaminated with saliva and submitted to different surface treatments. J. Appl. Oral. Sci. 2007, 15, 501–505. [Google Scholar] [CrossRef]
- Oztoprak, M.O.; Isik, F.; Sayinsu, K.; Arun, T.; Aydemir, B. Effect of blood and saliva contamination on shear bond strength of brackets bonded with 4 adhesives. Am. J. Orthod. Dentofacial. Orthop. 2007, 131, 238–242. [Google Scholar] [CrossRef]
- Cao, P.; Chen, D.-W.; Liang, J.; Wu, P.-G.; Wen, S.; Wei, J.; Liu, S.-J.; Wu, X.-M.; Zhao, Y.-F.; Xu, H.-B. Concentration of morpholine residues in major fruits and juices and its dietary exposure in China. Food Addit. Contam. Part A 2019, 36, 26–34. [Google Scholar]
- Yin, H.; Kwon, S.; Chung, S.H.; Kim, R.J.Y. Performance of universal adhesives in composite resin repair. Biomed. Res. Int. 2022, 2022, 7663490. [Google Scholar] [CrossRef]
- Klaisiri, A.; Phumpatrakom, P.; Thamrongananskul, N. Chemical surface modification methods of resin composite repaired with resin-modified glass-ionomer cement. Eur. J. Dent. 2022; online ahead of print. [Google Scholar] [CrossRef]
| Type | Material | Composition |
|---|---|---|
| Filling material | Resin composite (Filtex Z350 XT (A1E, A4B), 3M ESPE, St. Paul, MN, USA) | Bis-GMA, Bis-EMA-6, TEGDMA, UDMA, PEGDMA, silane-treated ceramic, silane-treated silica, silane-treated zirconia |
| Adhesive agent | Scotchbond multipurpose adhesive (3M ESPE, St. Paul, MN, USA) | Bis-GMA, HEMA, peroxide component of catalyst resin, amine |
| Surface treatment agent | Morpholine (Loba Chemie PVT Ltd., Mumbai, India) | 98% Extra pure O(CH2CH2)2NH |
| Group | Mean SBS ± SD | Failure Mode | Cohesive | |
|---|---|---|---|---|
| Adhesive | Mixed | |||
| 1. No surface treatment | 9.83 ± 1.13 a | 100 | 0 | 0 |
| 2. No saliva + SB | 16.41 ± 1.22 b | 80 | 20 | 0 |
| 3. No saliva + MOR + SB | 23.66 ± 1.35 c | 60 | 40 | 0 |
| 4. No saliva + MOR | 10.71 ± 0.81 a | 100 | 0 | 0 |
| 5. Saliva | 3.31 ± 0.95 d | 100 | 0 | 0 |
| 6. Saliva + SB | 4.05 ± 0.93 d | 100 | 0 | 0 |
| 7. Saliva + MOR + SB | 22.88 ± 1.96 c | 70 | 30 | 0 |
| 8. Saliva + MOR | 10.36 ± 1.53 a | 100 | 0 | 0 |
| 9. Saliva + PHOS + SB | 17.31 ± 1.48 b | 80 | 20 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klaisiri, A.; Suebnukarn, S.; Krajangta, N.; Rakmanee, T.; Sriamporn, T.; Thamrongananskul, N. The Effect of Morpholine on Composite-to-Composite Repair Strength Contaminated with Saliva. Polymers 2022, 14, 4718. https://doi.org/10.3390/polym14214718
Klaisiri A, Suebnukarn S, Krajangta N, Rakmanee T, Sriamporn T, Thamrongananskul N. The Effect of Morpholine on Composite-to-Composite Repair Strength Contaminated with Saliva. Polymers. 2022; 14(21):4718. https://doi.org/10.3390/polym14214718
Chicago/Turabian StyleKlaisiri, Awiruth, Siriwan Suebnukarn, Nantawan Krajangta, Thanasak Rakmanee, Tool Sriamporn, and Niyom Thamrongananskul. 2022. "The Effect of Morpholine on Composite-to-Composite Repair Strength Contaminated with Saliva" Polymers 14, no. 21: 4718. https://doi.org/10.3390/polym14214718
APA StyleKlaisiri, A., Suebnukarn, S., Krajangta, N., Rakmanee, T., Sriamporn, T., & Thamrongananskul, N. (2022). The Effect of Morpholine on Composite-to-Composite Repair Strength Contaminated with Saliva. Polymers, 14(21), 4718. https://doi.org/10.3390/polym14214718








